Orthopaedics, Autumn Term 2013 - Ping-Pong
advertisement

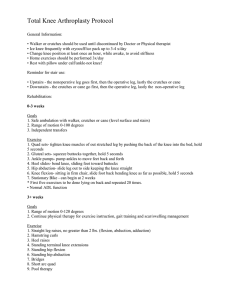
Orthopaedics, Autumn Term 2013 Question 1. At the Primary Health Care Centre, you meet a man with a recently diagnosed gonarthrosis. As pain relief, he takes diclophenac 50 mg x 3 which helps him quite well but he can “feel it” in his stomach. He would like you to prescribe sleeping tablets as he has difficulties falling asleep due to his knee ache. Once he has fallen asleep, he sleeps well. 1A. Which changes should be made to the patient’s medication? (1.5p) The patient’s problem is pain. He must thus receive adequate pain relief, not sleeping pills. Prescribe paracetamol 3-4 g daily, possibly additional mild opioids, and NSAID if he gets treatment with omeprazol or misoprostol at the same time. 1B. There are other general measures, apart from medication, which can mitigate the symptoms of gonarthrosis. Name three such measures! (3 correct 1 p, 2 correct 0.5 p) Strain relief e.g. by using a cane, physiotherapy, weight loss, orthosis. 1C. The patient wonders why he has developed arthrosis in his knee and what will happen in the future. Describe what information you should give the patient! (3p) It is of course not possible to give an exact template for the answer, but for receiving a full score, the answer must contain an adequate discussion on the aetiology and the natural course of the condition, and its treatment: The cause of primary arthrosis is often unknown. Factors that increase the risk for arthrosis are age, gender (higher risk for women), heredity and probably mechanical factors, but in the individual case it is most often impossible to say why this patient in particular has been affected. Sometimes a previous trauma may be identified (e.g. a fracture or infection) causing arthrosis, which then is regarded as secondary to the previous injury. The condition develops slowly, and it often takes many years until the first symptoms appear. The most common symptom is pain and the treatment is focused on pain relief. There is no curative treatment. The joint will slowly but surely deteriorate with increasing movement limitation and pain. The treatment is conservative with analgesia, physiotherapy and strain relief of the affected joint, but when treatment no longer suffices in keeping pain and ache on an acceptable level, surgery may be necessary. If the patient is young, different surgical methods may be chosen depending on whether the whole joint or only parts of it are affected; older patients are operated by total knee arthroplasty. Question 2. A 65-year-old woman with diabetes and hypertension comes to the emergency unit on Monday morning. She has fully recovered from a minor stroke she had some years ago. She stumbled over the edge of the pavement during the weekend and injured her foot and ankle. She has a limp but can move reasonably well. Her foot is discoloured blue on its lateral aspect from the malleolus down to the sole and forward until the MTP joints. The foot is swollen within the same area but also on the back of the foot and its medial aspect. She wonders whether this is something “serious” or if she can “limp home and wait for it to get fine again”. 2A. Only by looking at the foot you can think of several orthopaedic differential diagnoses, which is why you recommend her to stay for examination and treatment. Name three plausible orthopaedic differential diagnoses! (3 correct give 1 p, 2 correct 0.5 p) Fractured ankle (lateral malleolus), ankle distorsion, avulsion fracture MT5, fractured metatarsal, peroneus brevis tendon rupture… 2B. Choose two of these differential diagnoses and describe, for each one of them, both the acute management and the subsequent treatment and follow-up. If there are alternative treatments, your answer must state clearly which factors to consider in order to choose respective treatments. (3 p per diagnosis = max 6 p) It is of course impossible to give an exact template of an answer, but to obtain full score the answer must contain an adequate discussion on the acute management and the subsequent treatment and follow-up for each one of the two diagnoses. Example: Fractured ankle (lateral malleolus): Detailed examination and X-rays confirm the diagnosis. As the fracture is some days old and the patient has been able to walk relatively well it is most probably an A or B injury without dislocation or rupture of the syndesmosis. In this case, the patient can be treated by plaster boot/orthosis for six weeks. Crutches, information on elevated positioning and movement training. Pain relief. Follow-up visit after two weeks for control (possibly X-rays). Removal of plaster and mobilisation with a physiotherapist after six weeks. If it is a dislocated B or C injury, this is a case for surgery and the patient must thus be admitted to hospital. After surgery, plaster cast for six weeks and same follow-up as above. Question 3. A 31-year-old man comes to the primary health care centre and describes back ache that he has had intermittently for several years; however, he now additionally suffers from numbness and a tingling sensation in one leg for some days. He fills in a pain chart which looks like this: 3A. With the guidance of the medical history taken and the pain chart, which diagnosis is plausible to be suspected and where in the back is the problem located? Justify your answers! (3p) Herniated disc. Medical history of previous back ache and now additional symptoms radiating into one leg. The symptoms radiating into the leg suggest pressure on the nerve, the pain chart shows that the symptoms follow the dermatome of S1, hinting at the nerve root of S1 being affected. It is thus most likely that the herniated disc is located at the level of L5/S1. See pages 124 and 491 in the textbook. . 3B. Assuming that the clinical examination confirms the suspected diagnosis, what information should the patient receive? (2p) The symptoms he describes suggest a herniated disc; however, they are not alarming. He does not need any specific treatment at this time, but in case of leg pain he should take paracetamol and a NSAID. He is allowed to move as much as his symptoms admit him to. Normally, pain lasts for about 6 weeks. The prognosis is good; the vast majority (80-90%) recovers spontaneously. If any alarming symptoms occur (loss of perianal sensation, incontinence, urinary retention) he must seek urgent medical attention. See pages 493-494 in the textbook. 3C. In the way the medical problem is now described in this patient, there is most likely no need to operate. Name two facts from medical history taking and/or clinical findings that pose a strong indication for surgery. (1p) Insufferable pain, loss of perianal sensation, lack of sphincter tone, urinary retention. See page 494 in the textbook. Question 4. When you start your call at the emergency unit, you take over a patient who has been seen for swelling and pain in one knee. The colleague in charge before you has performed a knee joint puncture, suspecting an infection, and the patient has waited for the test results which are now available: CRP (blood) Blood glucose White blood cell count (joint) Glucose (joint) Lactate (joint) 67 6.7 55 4.9 4.5 (< 1) (< 0.2) (< 2.3) You do not find these results too unambiguous. 4A. Describe two situations in which a septic arthritis could give these test results (2p). The patient presents in the early phase of the infection, therefore the results have not yet become representative. The patient has an immunosuppressive treatment or suffers from some illness impairing the immune defence. 4B. Name two other afflictions (not septic arthritis) which could give these test results (1p). Gout, flare-up of rheumatoid arthritis, reactive arthritis, psoriatic arthritis. Apart from the joint fluid samples that have been analysed as shown above, a bacterial culture of the joint fluid has been sent. There is some millilitre of joint fluid left over in a test tube. 4C. Which test should you now order for additional diagnostic guidance? (0.5p) Direct microscopy 4D. Which two results from this test should strengthen the suspicion of an infection? (1p) Presence of bacteria Absence of crystals Question 5. Indicate whether the statements below are true or false! (4 correct = 1 p, 3 correct = 0.5 p) 5A. Knee □ True □ False □ True □ False When operating a chip fracture of the tibial condyle it is more important to get the joint surface in place than to adjust the leg length to the unaffected leg. □ True □ False In patellar fractures, it is contraindicated to perform a knee joint puncture as the proximal fragment then is dislocated inwards, towards the joint. □ True □ False □ True □ False □ True □ False □ True □ False □ True □ False An anterior cruciate ligament injury is caused by a varus force to the knee but posterior cruciate ligament injuries are caused by valgus force. A patellar luxation is repositioned by careful stretching of the patient’s leg while moving the patella into its position with one hand. 5B. Shoulder In a shoulder luxation, it is more common for the humeral head to dislocate forwards than backwards. Fractures of the surgical neck of the humerus most often affect elderly osteopenic individuals. An important diagnostic sign in shoulder impingement is the radiological appearance of a calcification in the supraspinatus tendon. In a shoulder luxation, the axillary nerve may be injured, which results in a reduced function of the deltoid muscle and impaired sensation on the proximal lateral aspect of the upper arm. Answers: 5A: F T T F 5B: T T F T