Patient Controlled Analgesia (PCA)
advertisement

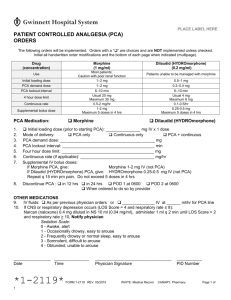
Patient Controlled Analgesia (PCA) Created By: esiddel 06/27/2005 - 11:34 AM CONNECTICUT CHILDREN’S MEDICAL CENTER [Clinical Care Manual] Title: Patient Controlled Analgesia (PCA) Date of Origination: April 1996 Approved By: Leonard Comeau, MD Signature(s): Document Name: pca.doc Date Last Revised: June 2005 Approval Date: September 2005 I. Policy: It is the policy of Connecticut Children’s Medical Center (CCMC) that Patient Controlled Analgesia (PCA) should be used for the administration of analgesics to minimize pain. A physician/licensed independent practitioner is responsible for ordering and adjusting the medications as well as determining the set limits through a PCA infusion. A registered nurse (RN) is responsible for monitoring and maintaining a PCA infusion. II. II. Purpose: To state the requirements of care and provide dosing and assessment recommendations for the child who is receiving PCA. PCA analgesia is used to allow the patient to control the analgesic medication to minimize pain, within physician determined pre-set limits. III. III. Protocol: A. A. Criteria/Standards: 1. 1. The physician and nursing staff providing care will determine patient appropriateness for PCA. Such criteria shall include, but is not limited to: a. a. Age/cognitive ability (recommended minimum age for use 7 years old) b. b. Alertness c. c. Physical ability (must be able to hold and push the button) d. d. Moderate to severe pain level with an expected minimum duration of pain for 24-36 hours. 2. 2. Nurse-Controlled Analgesia may be used as an alternative to PCA in patients whose age, clinical condition, and/or motor or cognitive ability preclude use of standard PCA. Refer to the “Nurse-Controlled Analgesia” guidelines for specific instructions. 3. 3. Parent-Controlled Analgesia is inappropriate except when the patient is receiving palliative care and is experiencing rapidly escalating, severe pain. ParentControlled Analgesia will not be used at CCMC under any other circumstances. 4. 4. Patients receiving continuous mode of IV opioids must be on continuous monitoring for heart rate, respiratory rate, and SaO2. a. a. Patients > one year of age may come off monitor when the dose of the continuous mode medication is unchanged for 24 hours. b. b. Patients receiving PCA mode-only do not require this type of monitoring. B. B. Nursing Responsibilities: 1. 1. The RN is responsible for pump set-up and programming as ordered by the MD, as well as the tubing changes and medication cartridge changes. 2. 2. When setting up pump, clear the prior patient’s history. Do not clear history for subsequent syringe changes for the same patient. 3. 3. Pain scores will be assessed after initiation, after any change in pump setting, and ongoing using a standardized pain rating scale to assess pain relief response to the PCA medication at least every 8 hours. 4. 4. Assess vital signs and other parameters per unit standard (at least every 4 hours), or as ordered by the physician. 5. 5. When using PCA mode only, the infusion should be “piggy-backed” into another IV fluid source to infuse at a minimum rate of 3 ml/hour. C. C. Initiation of PCA: 1. 1. PCA requires a physician order. 2. 2. The patient should be made comfortable before the PCA pump is initiated. This may require several intermittent analgesic doses at standard doses (morphine 0.05 to 0.1 mg/kg or equivalent) before the PCA pump is set. The PCA pump allows for only a single loading dose to be given at the start. PCA is most effective in maintaining pain control. D. D. Recommended Starting Doses (see Table): 1. 1. Due to limits of the PCA pump, round doses to nearest 0.1 mg or nearest 1 mcg. 2. 2. Four hour maximum cannot exceed 30 times drug concentration (1 PCA cartridge). Medication Morphine (1mg/ml) Loading Dose Continuous Dose PCA Dose Lockout Interval 4 Hour Maximum (initial) Hydromorphone (Dilaudid) (0.2 mg/ml) Loading Dose Continuous Dose PCA Dose Lockout Interval 4 Hour Maximum Opioid Naïve Patients Sickle Cell Crisis or Chronic Opioid Use Patients 0.05 – 0.1 mg/kg 0.015 – 0.025 mg/kg/hr 0.03 mg/kg 6-12 minutes 0.3 – 0.35 mg/kg 0.1 mg/kg 0.04-0.06 mg/kg/hr 0.02-0.03 mg/kg 6-8 minutes 0.48 – 0.72 mg/kg 0.01– 0.02 mg/kg 0.003– 0.005 mg/kg/hr 0.006 mg/kg 6-12 minutes 0.06 – 0.07 mg/kg 0.02 mg/kg 0.008-0.012 mg/kg/hr 0.004 – 0.006 mg/kg 6-8 minutes 0.1 – 0.14 mg/kg **Consult with Department of Pharmacy for use of other opioids by PCA modality. E. Assessment and Monitoring: 1. 1. Pressing the history button on the PCA pump allows the viewer to check how much the patient has used the pump. It summarizes demands and injections for the previous 1 and 24 hours. It also allows the clinician to view each hour of use in reverse chronological order. a. a. Demands are the number of times the patient requests a dose but does not receive one. b. b. Injections are the number of times the patient requests a PCA dose and receives one. 2. 2. Pain scores and pump history should be assessed frequently after initiation of PCA and following any change in pump settings. 3. 3. Document changes in pain intensity/pain score and actions taken in nursing flowsheet and/or progress notes. 4. 4. If any of the following “triggers” are present reassess the situation and consider the need for action: a. a. Pain score greater than or equal to 4 out of 10 b. b. Verbal complaint of pain c. c. Patient having more demands than injections in a 4 hour period d. d. Patient reaches 4 hour maximum and locks out e. e. Anticipation that lock out will be reached f. f. Adverse effects present. 5. 5. Consider whether adjunctive therapies (acetaminophen, nonsteroidal antiinflammatory agents, antispasmodics) are ordered and appropriate. F. Dose Titration: 1. 1. If patient is in acute pain, give a separate bolus dose (approximately 0.05 mg/kg/dose morphine or equivalent) per physician order. 2. 2. If no relief in 30 minutes, repeat a bolus one time per physician order. 3. 3. Reassess reason for increase in pain (e.g. ambulation, got behind due to long period of sleep.) 4. 4. Make adjustments in dosing (listed in order of preference): a. a. If lock out period is long (10-12 minutes) consider shortening interval (6-8 minutes). b. b. Increase PCA dose by 10-20% (4 a and 4 b may be done simultaneously). c. c. Adjustments to basal infusion should be made with caution since it may result in drug accumulation and oversedation. Consider an increase of 20-40% in basal rate. Changes to the basal infusion rate should not be made more frequently than every 6 hours. d. d. If the basal rate is increased, increase the 4-hour maximum dose by the same percentage. G. Transition off PCA Modality: 1. Before transition off PCA consider the following: a. a. Patient’s anticipated level of activity b. b. PCA doses required in last 12-24 hours c. c. Current level of pain control. 2. Steps to transition off PCA: a. a. Step 1 – Discontinue continuous infusion mode or consider converting it to a long acting dosage form at approximate equianalgesic doses if pain is expected to persist. Leave all other PCA parameters the same. b. b. Step 2 – Evaluate PCA only needs over the next 12-24 hours. c. c. Transition PCA only needs to equianalgesic doses of intermittent opiate. H. Patient and Family Education: 1. 1. Patient and family teaching should be provided prior to the painful event whenever possible, e.g., peroperatively. 2. 2. Teaching should include discussion of the risks of over-sedation and respiratory depression associated with use of PCA, and that only the patient will be allowed to administer bolus doses using the PCA pump. 3. 3. Provide the patient and family with any appropriate teaching tools. III. Documentation: A. A. Medications: 1. 1. Record medication doses on MAR in the PRN section and on the Proof-of-Use Pharmacy Sheet (as appropriate). 2. 2. Record as milligrams or micrograms received every 4 hours. 3. 3. Record medication fluids on the flowsheet. B. B. Patient teaching: 1. 1. Record initial and ongoing teaching on the patient’s Care Plan. 2. 2. Record distribution of written teaching materials on the patient’s Care Plan. C. C. Assessment: 1. 1. Record vital signs and other assessments on the flowsheet. 2. 2. Record pain scale scores (including reassessment scores) and actions taken on the flowsheet. 3. 3. Describe details of the patient’s response to pain medication and actions taken in the Progress Notes. IV. IV. Resources for Assistance with PCA Management PCA pump manual (technical questions) Department of Pharmacy 5-9935 ACUTE PAIN TEAM CONSULT V. V. Cross-referenced Documents: Assessment and Reassessment of Patients Intravenous Fluid Administration Medication Administration Medication Control Monitoring Equipment: Medical/Surgical Units Nurse-Controlled Analgesia Pain Assessment and Management

![See our handout on Classroom Access Personnel [doc]](http://s3.studylib.net/store/data/007033314_1-354ad15753436b5c05a8b4105c194a96-300x300.png)