File - Stephanie Hickey Nutrition Portfolio
advertisement

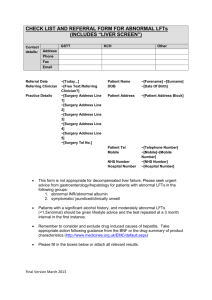
Nutrition 445 Case Study 1 Due September 18, 2013 Case: A 36-year old man was admitted to a hospital following episodes of nausea, vomiting, and general malaise. His urine was darker than usual. Upon examination it was discovered that his liver was enlarged and tender to palpation. Liver function tests were abnormal; plasma ALT was 1500 IU/L; AST was 400 IU/L. During the next 24 hours the man developed jaundice, and his plasma total bilirubin was 9.0 mg/dL (154 mmol/L). A diagnosis of hepatitis was made. The UL of the normal ranges in this lab are LD 300 IU/L, ALT, and AST 40 IU/L Questions: 1) Define hepatitis and discuss the major causes of hepatitis. Hepatitis is a disease of the liver where the liver becomes inflamed preventing proper function of the organ; and, there are five types of hepatitis, with the most common forms being Hepatitis A, B, and C. Hepatitis A is spread through contaminated food through the oral-fecal rout, by someone who prepared your food who has the virus, or by drinking contaminated water in parts of the world with poor sanitation. Hepatitis B and C are both spread by contact with an infected person’s blood, semen or bodily fluid. 2) What reactions are catalyzed by AST and ALT? and what coenzyme is required? Aspartate aminotransferase (AST) and alanine aminotransferase (ALT) become elevated when the hepatitis virus has affected the liver since the liver is the main site for the catabolism of amino acids (the transfer or removal of amino acids). This process occurs through transamination reactions, which involve the transfer of an amino group from one amino acid to an amino acid carbon skeleton, which are catalyzed by aminotransferases. (See written reaction below) (Smith, Grooper, 2013) AST, found in higher concentrations in the heart, and ALT, found in higher concentrations of the liver, catalyze the two most important aminotransferases reactions, which are both revisable reactions. ALT catalyzes the transfer of the amino group alanine to an –ketogluterate, producing pyruvate and glutamate, while AST transfers amino groups from aspartate to an –ketogluterate, producing oxaloacetate and glutamate. (See Figures 1 and 2 below) (Advanced Nutrition and Human Metabolism, 2013) Figure 1 Figure 2 3) What conditions are important to maintain in performing the enzyme assays? Enzyme assays are laboratory methods used for measuring enzymatic activity and measuring the loss of a substrate that should be measured under steady-state conditions and should also be tested under steady-state conditions. Problems that arise are due to lack of attention to detail, so it is crucial to ensure that the enzymes, substrates, buffers, etc. have been fully evaluated and characterized. The addition of an acidic solution to a basic solution, or vice versa, otherwise known as a titration, is the way to determine the concentration of an active site in the assay; likewise, multiple concentrations of the substrate should be tested in order to distinguish noncompetitive inhibition from uncompetitive inhibition. To distinguish a competitive inhibitor from a noncompetitive inhibitor or uncompetitive inhibitor is increased at concentrations of substrate above its own Km value, the velocity should be measured and it is recommended that less than 10% of the substrate should be converted into the product. Measuring the rate of the product formation should be liner to time, meaning, measuring the rate of product formation at the concentration of the substrate using the assay and equipment that will be used in the final assay and the linear part should be evaluated from the data. High and low controls of the substrate should be included in the final assay with the high control having the maximum enzyme activity at each substrate showing the substrate titration without the inhibitor and the low control has the substrate titration with the enzyme, substrate, or the inhibitor, which reflects the signal expected for there to be no enzyme activity at each substrate concentration. (Mechanism of Action Assays for Enzymes, 2008) 4) Which other enzymes might have been elevated in the plasma? Excluding aspartate aninotransferase and alanine aminotransferases, other enzymes that may be elevated in the plasma is alkaline phosphate, gamma-glutamyl transferase (GGT), and bilirubin. Elevations of these enzymes can be detected by doing a liver panel, which is a way to screen for damage; these results do not detect a specific condition but instead they indicate that there may be a liver dysfunction. Alkaline phosphatase (ALP) is a source of the bone and liver and when ALP is elevated you want to check GGT to help locate the source because high levels can indicate cholestasis or hepatocellular injury. Both ALP and GGT will be elevated within the bile duct if the damage to the liver was caused by alcohol, GGT is not a source of the bone and is the most sensitive enzyme to detect liver damage. Bilirubin is elevated within the blood when too much of the enzyme is being produced which indicated less is being removed due to obstructions within the bile duct or issues processing bilirubin, levels of bilirubin are variable depending on the severity of jaundice or alcohol consumption. (Hepatitis, 2003) (Hepatic Function Panel, 2013) 5) How does “total” bilirubin relate to “direct” and “indirect” bilirubin? The result of the breakdown of Haemoglobin is bilirubin, and bilirubin is the principle pigment in bile, which then gets excreted from the body via feces. Bilirubin circulates throughout the blood stream in two forms, direct and indirect. Indirect bilirubin is insoluble and travels through the bloodstream to the liver where is it then changed to the soluble direct form. Direct bilirubin is soluble and is made by the liver from indirect bilirubin. Total bilirubin is the sum of direct bilirubin and indirect bilirubin and total bilirubin levels, along with direct bilirubin levels, are measured in the blood while indirect bilirubin levels are derived from the total and direct bilirubin measurements by subtracting the direct bilirubin value from the total value. We can measure the amount of bilirubin by collecting a blood sample and this test is used for liver moderation by checking if the liver is functioning properly as well as watching for any signs of liver dysfunction/disease such as hepatitis. Blood samples are also a way to find out if the bile ducts are blocked, and to monitor the presence and progression of jaundice. (Total and Direct Bilirubin) 6) What other diagnostic tests need to be done for this patient before a treatment plan can be recommended? The patient has hepatitis symptoms and was diagnosed with hepatitis, so his doctor should perform a blood test to check for the presence of the antibody to determine the type of hepatitis and possibly perform a liver biopsy to determine the extent of the liver damage. Other diagnostic tests that need to be done for this patient before a treatment plan can be recommended would be narrowing the hepatitis down to an acute or chronic form, then decide which one of the five forms of hepatitis, so the patient can be properly treated. Hepatitis A, B, and C are viral forms of hepatitis and can be diagnosed by a physical exam, blood tests, liver biopsy, and imaging studies like a CAT scan or a sonogram. No matter what type of hepatitis this man has he should avoid alcohol consumption because that can further damage the liver. Works Cited Alter, HJ: Hepatitis. Semin Liver Dis. 6:1, 1986. Cassidy, WM, Reynolds, TB: Serum lactate dehydrogenase in the differential diagnosis of acute hepatocellular injury. J Clin Gastroenterol. 19(2); 118, 1994. Chames, Frances. "Hepatitis." Presented at the E. Lansing CHM Campus. 14 Feb. 2003. Lecture. Jacobson, IM, Dienstag, JL.: The delta hepatitis agent: viral hepatitis, type D. Gastroenterology. 86: 1614, 1985. Liver Function Tests; LFTs." Hepatic Function Panel (n.d.): n. pag. Lab Tests Online. 6 Mar. 2013. Web. 15 Sept. 2013. National Digestive Diseases Information Clearinghouse 2007, NIH publication, Volume no. 07-6190 Smith, Grooper: Advanced Nutrition and Human Metabolism. 6: 2005, 2009, 2013 Strelow, John, Walthere Dewe, Phillip W. Iversen, Harold B. Brooks, Jeffrey A. Radding, James McGee, and Jeffrey Weidner: Mechanism of Action Assays for Enzymes. Assay Guidance Manual. National Center for BioTechnology Information, 1 May 2008. Web. 12 Sept. 2013. Total and Direct Bilirubin: Clinical Chemistry Lab Manual. F113-122.