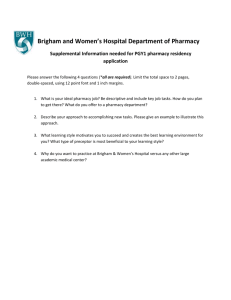
Queen`s Online: Programme Specification
advertisement

Programme Code: S132100DG 08/09 Programme Title: Pharmacy Awarding Institution Queen's University Belfast Teaching Institution QUB, School of Pharmacy Programme Accredited By Pharmaceutical Society of Northern Ireland, Royal Pharmaceutical Society of Great Britain Final Award M.Pharm. Honours UCAS Code PHARMACY [B230] QAA Benchmarking Group Pharmacy (Hons) Educational Aims Of Programme Provide a quality education programme for pharmacy students that meets the requirements of the Pharmaceutical Society of Northern Ireland and the Royal Pharmaceutical Society of Great Britain; provide an educational environment within which students will have the opportunity to develop their interest in pharmacy; prepare students for independent life-long learning by encouraging directed self-study; provide a strong knowledge base in pharmaceutical and related clinical sciences and in professional aspects of pharmacy; provide training in those practical skills related to the science and practice of pharmacy; help students develop a range of key and employability skills; foster development of research skills; develop awareness of professional and ethical issues; facilitate students in developing their full potential. For current general University entry requirements for this pathway go to http://www.qub.ac.uk/ado Criteria For Admission (Subject Specific Requirements) To Programme Target grades are for 2006 entry & may be amended for those entering in 2007 HOME & EU APPLICANTS A-Levels AAB including Chemistry & at least one from Biology, Mathematics & Physics OR ABB including Chemistry & at least one from Biology, Mathematics & Physics plus A in a fourth AS level subject. One Applied/VCE A-level or Applied/VCE AS level subject is acceptable in fulfillment of the three A-level plus one AS level offer. However, it may not be offered as part of a three A-level combination Only one Mathematics subject will be counted at A-level. General Studies is not acceptable. GCSE English, Mathematics & either Biology or Double Award Science at Grade C or better are required if not offered at AS level or A-level. Both GCSE & AS level performance are taken into account. Where offers are made to repeat applicants, the standard required is AAA at A-level or AAB at A-level plus A in a fourth AS level. Irish Leaving Certificate AAAB2B2B2 (including Biology) at Higher Level plus B in A-level Chemistry. English & Mathematics are required at Ordinary Level, if not taken at Higher Level. Scottish Highers AAAAB (including at least one from Biology, Mathematics & Physics) plus B in Advanced Higher Chemistry. Standard Grade (3 or better) in English, Mathematics & Biology required if not taken at Higher Level. International Baccalaureate Diploma A total of 34 points including 6,6,6 or 6,6,5 in Higher Level subjects, including Chemistry & at least one from Biology, Mathematics & Physics. Standard Level Biology, English & Mathematics or equivalent are required if not taken at Higher Level. Graduate Entry A minimum of an Upper Second Class Honours degree, preferably in a relevant subject, normally completed within five years of the intended date of entry to the Pharmacy degree. Those with an Upper Second Class Honours degree in a non-relevant subject may be considered if they have the appropriate science background at GCSE & A-level. Mature Students The same requirements as listed above apply. Other Qualifications Contact the Admissions Office for advice. INTERNATIONAL APPLICANTS Apply through the Universities & Colleges Admissions Service (www.ucas.com). Slightly different requirements apply. Check the School web site for details. (http://www.qub.ac.uk/pha/) Canadian & Australian High School qualifications are also welcomed. International applicants must have an acceptable English Language qualification eg IELTS 6.5 or TOEFL 580. Additional Relevant Information None For Further Information Refer To Advisors of Studies Tel: 028 9097 5800 Programme Structure, Levels, Modules and Credits Stage 1 Status Code Title Pre-Requisites CATS STATUS compulsory PMY1014 Introduction to Pharmacy Practice Skills Must be accepted onto the Pharmacy MPharm course. 10 LIVE compulsory PMY1011 Physiology for Pharmacy Must be accepted onto the Pharmacy MPharm course 20 LIVE compulsory PMY1001 Pharmaceutics Must be accepted onto the Pharmacy degree course 20 LIVE compulsory CHM1004 Structure, Reactivity and Mechanism in Organic and Biorganic Chemistry A Chemistry C or at least one of CHM0011/CHM0002 20 LIVE compulsory PLY1002 Physiology 2 Must be accepted onto the Pharmacy MPharm course 20 LIVE compulsory PMY1005 Physicochemical Principles for Pharmacy Must be accepted onto the Pharmacy MPharm course 30 LIVE Stage 2 Status Code Title Pre-Requisites CATS STATUS compulsory PMY2001 Medicinal Substances: Characterisation and Quantification PMY1001, CHM1004, PMY1011, PLY1002, PMY1005, PMY1014. 20 LIVE compulsory PMY2004 Principles of Drug Action (1) PMY1001, CHM1004, PMY1011, PLY1002, PMY1005, PMY1014. 20 LIVE compulsory PMY2002 Medicinal Substances: Structure and Function PMY1001, CHM1004, PMY1011, PLY1002, PMY1005, PMY1014. 20 LIVE compulsory PMY2005 Principles of Drug Action (2) PMY1001, CHM1004, PMY1011, PLY1002, PMY1005, PMY1014. 20 LIVE compulsory PMY2006 Pharmaceutical Technology PMY1001, CHM1004, PMY1011, PLY1002, PMY1005, PMY1014. 40 LIVE Status Code Title Pre-Requisites compulsory PMY3069 Legislation PMY2001, PMY2004, PMY2002, PMY2005, PMY2006 10 LIVE compulsory PMY3081 Drug Delivery PMY2001, PMY2004, PMY2002, PMY2005, PMY2006 20 LIVE compulsory PMY3064 Pharmacy Practice 1 PMY2001, PMY2004, PMY2002, PMY2005, PMY2006. 20 LIVE compulsory PMY3075 Pharmacotherapy 2 PMY2001, PMY2004, PMY2002, PMY2005, PMY2006. 20 LIVE compulsory PMY3082 Drug design/Pharmaceutical analysis PMY2001, PMY2004, PMY2002, PMY2005, PMY2006 20 LIVE compulsory PMY3072 Pharmaceutical Biotechnology PMY2001, PMY2004, PMY2002, PMY2005, PMY2006 10 LIVE compulsory PMY3073 Applied Clinical Pharmacy 1 PMY2001, PMY2004, PMY2002, PMY2005, PMY2006 10 LIVE compulsory PMY3074 Pharmacotherapy 1 PMY2001, PMY2004, PMY2002, PMY2005, PMY2006 10 LIVE Status Code Title Pre-Requisites compulsory PMY4071 Pharmacist Prescribing PMY3064, PMY3069, PMY3072, PMY3073, PMY3074, PMY3075, PMY3081, PMY3082. 10 LIVE Compulsory PMY4072 Social and Behavioural Aspects of Pharmacy 1 PMY3064, PMY3069, PMY3072, PMY3073, PMY3074, PMY3075, PMY3081, PMY3082. 10 LIVE compulsory PMY4002 Business Government and Industry PMY3064, PMY3069, PMY3072, PMY3073, PMY3074, PMY3075, PMY3081, PMY3082. 10 LIVE compulsory PMY4070 Social and Behavioural Aspects of Pharmacy 2 PMY3064, PMY3069, PMY3072, PMY3073, PMY3074, PMY3075, PMY3081, PMY3082. 10 LIVE Compulsory PMY4073 Infectious Diseases PMY3064, PMY3069, PMY3072, PMY3073, PMY3074, PMY3075, PMY3081, PMY3082. 10 LIVE compulsory PMY4007 Pharmacotherapy 3 PMY3064, PMY3069, PMY3072, PMY3073, PMY3074, PMY3075, PMY3081, PMY3082. 20 LIVE compulsory PMY4003 Pharmacy Practice; Responding To Symptoms PMY3064, PMY3069, PMY3072, PMY3073, PMY3074, PMY3075, PMY3081, PMY3082. 20 LIVE compulsory PMY4005 Project PMY3064, PMY3069, PMY3072, PMY3073, PMY3074, PMY3075, PMY3081, PMY3082. 30 LIVE Stage 3 CATS STATUS Stage 4 CATS STATUS Awards, Credits and Progression of Learning Outcomes Examinations On successful completion of Stage 4 candidates qualify for the award of an MPharm honours degree on the basis of performance in the written examinations, coursework and project. The degree classification is based on the performance at Stage 2 (10%) and equally on the performance at Stage 3 (45%) and Stage 4 (45%). Stage 1 Due to strict requirements of professional accreditation, the regulations for the MPharm differ in important ways from those for other degree courses. Entry into the Pharmacy degree course is only possible on acceptance via an UCAS application. It is not normally possible for a registered student to change degree course into Pharmacy. The MPharm in Pharmacy may only be taken full-time and as a degree with Honours. In order to proceed to Stage 2 students must normally have passed all Level 1 modules. No compensation between modules is permitted. No substitution of modules is allowed Stages 2, 3 & 4 Students must pass all modules in each Stage. No compensation between modules is permitted. No substitution of modules is allowed. No student may proceed to Stage 3 unless passes have been obtained in all the prescribed Level 1 and Level 2 modules. Students who fail not more than the equivalent of two modules at Stage 3, are permitted to take resit examinations for those modules in August/September. No student may proceed to Stage 4 unless passes have been obtained in all the prescribed Level 3 modules. Students who fail not more than the equivalent of two modules at Stage 4, are permitted to take resit examinations for those modules in August/September. Learning Outcomes: Knowledge and Understanding On successful completion of the M.Pharm. degree, the student will be able to demonstrate pharmaceutical knowledge and understanding of the following: 1. the physical, chemical and biological principles relevant to the pharmaceutical sciences 2. the design, development and delivery of drugs 3. the clinical sciences relevant to the practice of pharmacy 4. the organisation of healthcare provision and the social, legal, ethical and economic issues relating to pharmacy practice Teaching and Assessment Methods: Knowledge and Understanding Learning & Teaching: Students acquisition of core knowledge is achieved primarily through independent study supported by lectures, directed reading, laboratory classes, workshops, tutorials, clinical and community based placements and project work. Assessment: 1. Written examinations and coursework 2. Clinical and community based placements are assessed from Levels 2 through 4 using multiple choice questions, work books, mini-projects and case based presentations. Learning Outcomes: Subject-specific Skills 1. Demonstration of knowledge and critical understanding of essential facts, concepts, principles and theories relating to the subject areas identified above. 2. Ability to apply in practice settings the knowledge and understanding required to meet the needs of other health care professionals. 3. Application of clinical skills in practice settings to the provision of pharmaceutical care to patients. 4. Recognition and analysis of problems and planning of strategies for their solution. 5. Critical evaluation, interpretation and synthesis of pharmaceutical information and data. 6. Production of pharmacy-specific scientific documentation. 7. Presentation of pharmaceutical science material and arguments clearly and correctly, in writing and orally, to both specialist and lay audiences. 8. Calculation of medicine doses and dosage regimens. 9. Interpretation of patient and clinical data, including patient records held within practice settings. 10. Ability to contribute to the development of healthcare through reflective practice, enquiry and innovation. 11. Interpretation of prescriptions and other orders for medicines. 12. Ability to prescribe appropriately using patient based case notes and scenarios. 13. Monitor and assess patients’ response to drug treatment using basic physical examination skills relevant to certain disease states. Teaching and Assessment Methods: Subject-specific Skills Learning & Teaching: Subject-specific skills are developed through a range of teaching methods such as lectures, directed reading, laboratory classes, workshops, tutorials, hospital based teaching and project work; feedback on submitted coursework plays an important role in this process. Assessment: Subject-specific skills are assessed through written examinations, laboratory reports, critical literature reviews, OSCEs (objective, structured, clinical examinations), poster presentations (e.g. group projects), oral presentations (e.g. patient case studies), role play, practical examinations (e.g. extemporaneous dispensing and pharmacy practice) and an extended individual research project during final year. Learning Outcomes: Cognitive Skills 1. The safe handling of chemical and pharmaceutical materials, taking into account their physical and chemical properties, including any specific hazards associated with their use. 2. The ability to undertake risk assessments concerning pharmaceutical procedures and practices. 3. Skills required for the conduct of standard pharmaceutical laboratory procedures. 4. The planning, design and execution of self-directed and original research investigations, from the problem-recognition stage through to the evaluation and appraisal of results and findings; this to include the ability to select appropriate techniques and procedures. 5. The operation of standard pharmaceutical instrumentation. 6. The ability to evaluate critically and to interpret purposefully data derived from laboratory and clinical observations and measurements, in terms of their significance and the theory underlying them. 7. Preparation and presentation of medicines, by manufacture and extemporaneous dispensing, including sterile products. 8. Skills in the analysis of medicines. 9. The ability to advise patients and others on the safe and effective use of medicines. Teaching and Assessment Methods: Cognitive Skills Learning & Teaching: Student’s cognitive skills are developed through a range of teaching methods such as laboratory classes, workshops, tutorials, clinical and community based placements and project work. 1&2: Instruction in COSSH legislation and its application to work carried out by students within the laboratories; lectures in toxicology 3,5&8: Live demonstrations and the use of videos in a range of practical classes followed by the opportunity to develop the skills 4: group projects and individual research project (final year), critical literature reviews 6: analysis and presentation of clinical case studies 7: students develop these skills through relevant laboratory-based practical exercises 9: Role play in advising patients when dispensing medication and when responding to patients presenting with symptoms of minor ailments Assessment: Cognitive skills are assessed through, laboratory reports including presentation of products/materials produced, critical literature reviews, OSCEs (objective, structured, clinical examinations), poster presentations (e.g. group projects), oral presentations (e.g. patient case studies), role play, practical examinations (e.g. extemporaneous dispensing and pharmacy practice) and an extended individual research project during final year. Learning Outcomes: Transferable Skills 1. Interpersonal skills; the ability to interact effectively with patients, the public and healthcare professionals; including communication, both written and oral. 2. Team-working. 3. Problem-solving, relating to qualitative and quantitative information, extending to situations where evaluations have to be made on the basis of limited information. 4. Numeracy and computation, including such aspects as error analysis, order-of-magnitude estimations, correct use of units and modes of data presentation. 5. Acquisition, transformation, interpretation and critical evaluation of data. 6. Information retrieval in relation to primary and secondary information sources, including information retrieval through online computer searches. 7. Information technology skills, including word processing, spreadsheet use, database use, archiving data and information, and internet communication. 8. Time-management and organisation, as evidenced by the ability to plan and implement efficient and effective modes of working. 9. Independent study skills as preparation for continuing professional development. 10. Personal Development Planning and CV writing 11. A professional and ethical attitude and approach. 12. Analysis and critical appraisal of published literature. 13. Application of general, biological and medical statistics. 14. The ability to operate within a quality management framework. 15. Recognition of the need to work within personal limitations. Teaching and Assessment Methods: Transferable Skills Teaching & Learning Consistent with the benchmark statement for Pharmacy, the acquisition and development of key skills are integral to the delivery of the M.Pharm. degree pathway. The half module ‘Introduction to Pharmacy Practice Skills’, which gives students a basic grounding in IT skills, communication skills (verbal and written), numeracy and statistics, is delivered in first year over both semesters. Assessment 1,2,3,4,5,6,7,8,11&12: Students are required to submit word-processed individual and group assignments, case studies, workbooks & research dissertation according to fixed deadlines. 2: Students must attend a workshop which involves addressing an ethical dilemma with students from other healthcare disciplines. 1: Students give 2 oral case report presentations to clinical practitioners and their peers. 1,9,10,11,13&14: Oral presentations, written reports, role play, OSCEs, practical and written examinations are used to assess these skills in a professional context. Date of Last Revision: 17/11/2008