Aesthetic Posters
advertisement

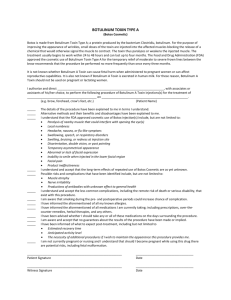
POSTER SECTION AESTHETIC Effect of Botulinum toxin type A on tear production following treatment of lateral canthal rhytides Yonca O. Arat, MD, Micheal T. Yen, MD. Baylor College of Medicine, Houston, TX. Introductory Sentence: The literature regarding tear production after botulinum toxin type A injections is inconclusive with several studies reporting increase 1, decrease 2,3 or no change 4 in tear production after botulinum toxin injections. Only one case of symptomatic dry eye has been reported after botulinum toxin injection for lateral canthal rhytides 5. Our purpose is to evaluate the incidence of temporary dry eye following treatment of lateral canthal rhytides with botulinum toxin and the effects of lateral periorbital injections on lacrimal gland tear production. Methods: Twenty-six crow’s feet areas were injected with botulinum toxin in 13 females with an age range of 31-58 years. Botulinum toxin was diluted with unpreserved saline yielding a concentration of 2.5 units/0.1 cc. A total of 5 units of botulinum toxin was injected per side with two separate injections. Schirmer 1 testing was performed before, at 1 week, and at 1 month after the injections. Statistical significance was evaluated with paired t-test analysis. Results: None of the patients developed dry eye symptoms 1 week and 1 month after botulinum toxin injection. No statistical difference was found in Schirmer test results from baseline at 1 week (p=0.23) or 1 month (p=0.32) after the injection. Five eyes of 3 patients had significant decrease in Schirmer test results in the range of 24-72% decrease from baseline at 1 week and 11- 60% at 1 month after the injection. Conclusions: Botulinum toxin for lateral canthal rhytides, when properly administered, usually does not suppress tear production but decreased tear production after botulinum toxin for crow's feet is a possible complication and patients should be advised of the small but definite risk of a temporary dry eye. Bibliography: 1. Spiera H, Asbell PA, Simpson DM. Botulinum toxin increases tearing in patients with Sjogren's syndrome: a preliminary report. J Rheumatol. 1997; 24(9):1842-3. 2. Horwath-Winter J, Bergloeff J, Floegel I, et al. Botulinum toxin A treatment in patients suffering from blepharospasm and dry eye. Br J Ophthalmol. 2003;87(1):54-6. 3. Dutton JJ, Buckley EG. Long-term results and complications of botulinum A toxin in the treatment of blepharospasm. Ophthalmology.1988; 95(11):1529-34. 4. Price J, O'Day J. A comparative study of tear secretion in blepharospasm and hemifacial spasm patients treated with botulinum toxin. J Clin Neuroophthalmol. 1993; 13(1):67-71. 5. Matarasso SL. Decreased tear expression with an abnormal Schirmer's test following botulinum toxin type A for the treatment of lateral canthal rhytides. Dermatol Surg. 2002; 28(2):149-52. Author Disclosure Block: Y.O. Arat, None; M.T. Yen, None. Soft Tissue Necrosis And Inflammation As A Complication Of Hyaluronic Acid Injection Brian Biesman, M.D.. Nashville, TN. Introductory Sentence: Cross-linked hyaluronic acid (HA) compounds are well recognized for their usefullness in soft tissue augmentation. Restylane (Medicis, Inc) is a cross-linked HA product produced via a bacterial fermentation process. HA is not species specific and thus skin testing is not required. Serious complications to HA injection are rare. I report a case of serious local tissue inflammation, necrosis, and infection following HA injection. Methods: A 52 year old female underwent injection of 2.0 cc of HA to the nasolabial folds and submental region. Approximately 0.9 cc was placed in each NL fold. Approximately 2 weeks after injection the patient began to experience moderate inflammation in the left nasolabial fold. Despite the use of topical and systemic steroids, this inflammation progressed and an abscess developed. This was drained in the office and oral antibiotic therapy was initiated. Despite completion of a 10-day course of oral antibiotics, the inflammation progressed and another abscess developed. The patient ultimately required inpatient hospitalization for IV antibiotic therapy. Results: The facial inflammation eventually resolved. Mild soft tissue changes remain but additional intervention has not been required. Once hospitalized, the patient reported a remote medical history of nonspecific autoimmune disease. Conclusions: Serious complications of HA injections are rare but can occur. The proposed etiology and management of this condition will be discussed. Bibliography: 1. Lowe NJ, Maxwell CA, Lowe P, ,Duick MG, Shah K. Haluronic acid skin fillers: adverse reactions and skin testing. J Am Acad Dermatol. 2001;45(6):930-3. 1. Fernandez-Acenero MJ, Zamora E, Borbujo J. Granulomatous foreign body reaction against hyaluronic acid: report of a case after lip augmentation. Dermatologic Surgery. 2003;29(12):1225-6. Author Disclosure Block: B. Biesman, Medicis, Inc. S. Midfacial Surgery: Surgical Precision Through Anatomic Restoration Karim Punja, MD, Don O. Kikkawa, MD, Nonette Y. Pasco, MD, Bobby S. Korn, MD, PhD. University of California, San Diego, La Jolla, CA. Introductory Sentence: Surgical restoration of the lower eyelid and midface can be challenging to even seasoned surgeons. It requires an intimate understanding of surgical anatomy and age-related changes. Particular attention should be paid to the orbitomalar ligament, SMAS, muscles of facial expression, and topographical changes. The goal of this presentation is to highlight three useful techniques for functional and aesthetic restoration of the midface. Methods: In this video, anatomic and structural landmarks will be emphasized. Surgical rejuvenation and reconstructive techniques will be demonstrated using three principle approaches: 1) Transconjunctival fat redraping; 2) Restoration of the orbitomalar ligament with SOOF lift; and 3) Subperiosteal midface lifting. Results: Restoration of midfacial contour is achievable by observing sound surgical principles and respect of anatomic tissue planes. Depending upon the degree of age-related change, each of the three techniques offer graded restoration. These techniques can be used for both reconstructive and aesthetic indications. Conclusion: With adherence to sound anatomic and surgical principles, both functional and aesthetic restoration of the midface can be obtained. Bibliography: 1. Hamra ST. Arcus marginalis release and orbital fat preservation in midface rejuvenation. Plast Reconstr Surg. 1995 Aug;96(2):354-62. 2. Hester TR Jr, Codner MA, McCord CD, Nahai F, Giannopoulos A. Evolution of technique of the direct transblepharoplasty approach for the correction of lower lid and midfacial aging: maximizing results and minimizing complications in a 5-year experience. Plast Reconstr Surg. 2000 Jan;105(1):393-406. 3. Patipa M. Transblepharoplasty lower eyelid and midface rejuvenation: part I. Avoiding complications by utilizing lessons learned from the treatment of complications. Plast Reconstr Surg. 2004 Apr 15;113(5):1459-68. Author Disclosure Block: K. Punja , None; D.O. Kikkawa , None; N.Y. Pasco , None; B.S. Korn , None. Suture Suspension Technique for Facial Rejuvenation Alan B. Brackup, MD. Langhorne, PA. Abstract Body: Introductory Sentence: The purpose of this paper is to present techniques the author has found useful in achieving facial rejuvenation with suture suspension over the past year. Utilizing techniques derived from the Threadlift protocol and subsequently modified, subjects underwent facial soft-tissue suspension with both barbed and smooth prolene sutures. The areas treated included the brows, midface, cheek/jowls, and neck. Methods: This does not represent a controlled study, but rather a presentation of techniques proven useful to achieve facial rejuvenation in a non-incisional manner. Patients were counseled preoperatively regarding the risks, benefits and especially limitations of these techniques as compared to open procedures. Unless combined with other, incisional surgery, all cases were performed under local anesthesia. Depending upon the area treated, either smooth prolene, APTOS barbed prolene, or Woffles barbed prolene sutures were placed in the subdermal tissue to elevate the desired region. Results: All patients to date have expressed satisfaction with their results. Midface elevation has proven particularly striking, approaching or even exceeding results achieved with open procedures. All patients have been able to return to public, daily acitivities within 2 days of their procedure. Complications have been limited to one case of suture migration following breakage. Conclusions: Suture suspension techniques can be used successfully to achieve significant facial rejuvenation. Patient selection is critical, as certain facial types respond less well to these procedures than others. Patient satisfaction is dependent upon an understanding of the limitations of suture suspension as compared to traditional incisional surgery, as well as proper patient selection and surgical technique. Bibliography: References can be provided if desired. Author Disclosure Block: A.B. Brackup, None. Aesthetic Comparison of the Results of Combined Browlift and Blepharoplasty versus Blepharoplasty Alone Benson Chen, MD1, John A. Burns, MD1, Kenneth V. Cahill, MD1, Julian D. Perry, MD2, David E.E. Holck, MD3, Allan E. Wulc, MD4, Spencer Ludlow, BS1, Deb Grzybowski, PhD1, Edward E. Herderick, BS1, Jill A. Foster, MD1. 1 The Ohio State University, Columbus, OH, 2The Cleveland Clinic Foundation, Cleveland, OH, 3Wilford Hall Medical Center, San Antonio, TX, 4Wills Eye Hospital, Philadelphia, PA. Introductory Sentence: The aesthetic results of browlift with blepharoplasty were compared to blepharoplasty alone using digital imaging and comparison to a virtual ideal of beauty, "Virtual Miss Germany".1 Methods: Digital images of pre and post-operative results of three categories of surgical patients were collected: endoscopic browlift and blepharoplasty, direct browlift and blepharoplasty, and blepharoplasty alone. Using Adobe Photoshop V7.0( Adobe Systems, Inc ) eyebrow and eyelid positions of preoperative and postoperative patient photographs were analyzed in comparison to a computer rendered template of idealized beauty, "Virtual Miss Germany" (Figure 1)1. These were defined by Vertical Standard Lines intersecting the pupils, medial and lateral canthi and limbi, and an Oblique Standard Line intersecting the ala and lateral canthus of the template. Aesthetic Scores were defined as the difference in area between the patient and the idealized template for lidfold and eyebrow positions (Figure 2). Relative Surgical Success was defined as the natural log of the ratio of postoperative Aesthetic Score to preoperative Aesthetic Score. Relative Surgical Success was then compared between each category of surgery for both eyelid and eyebrow positions. Results: 30 Caucasian female patients (60 eyes) were included in this study: 11 patients had blepharoplasty surgery alone (Age 53-74, Mean 65.5 ). 12 patients had blepharoplasty and endoscopic browlifting (Age 43-78, Mean 60.2 ) and 7 received blepharoplasty with direct browlifting (Age 71-88, Mean 75.7 ). Each category of surgery was successful in moving the lidfold closer to the ideal position (p<0.01), and there was no significant difference in their Relative Surgical Success. When compared to blepharoplasty alone, both browlifting surgeries were significantly more successful at moving the eyebrows towards the idealized position (p<0.05). The category of patients who had blepharoplasty without browlifting surgery had no significant change to their eyebrow positions (p>0.8). There was also no significant difference between the two browlifting techniques. Conclusions: As compared to "Virtual Miss Germany", an idealized concept of beauty, eyebrow repositioning in conjunction with blepharoplasty resulted in a more aesthetically desireable result compared to blepharoplasty alone. Bibliography: 1. Gruendl M, Scherber C, Marberger C, Braun C. “Virtual Miss Germany”, Beautycheck.com, 2003. University of Regensburg, Regensburg, Germany. 2. Freund RM, Nolan WB III. Correlation between brow lift outcomes and aesthetic ideals for eyebrow height and shape in females. Plast Reconstr Surg 1996; 97:1343-8. 3. Gunter JP, Antrobus SD. Aesthetic analysis of the eyebrows. Plast Reconstr Surg 1997; 99:1808-16. Author Disclosure Block: B. Chen, None; J.A. Burns, None; K.V. Cahill, None; J.D. Perry, None; D.E. Holck, None; A.E. Wulc, None; S. Ludlow, None; D. Grzybowski, None; E.E. Herderick, None; J.A. Foster, None. Current Practice Trends In Browlifting: A Survey of Oculofacial Plastic Surgeons Chad L. Betts, M.D., David B. Lyon, M.D.. UMKC Department of Ophthalmology, Kansas City, MO. Introductory Sentence: To evaluate current trends in browlifting techniques used by oculofacial plastic surgeons. Methods: ASOPRS members who participate in the ASOPRS list serve (230 members) were surveyed regarding browlift procedures performed in 2004. The three-page email questionnaire inquired about the variety of browlift techniques performed, anesthesia preferences, utilization of the endoscopic technique, fixation methods, pre-operative and postoperative medication usage, and procedural expectations for 2005. Results: A total of 1621 procedures were performed by the 48 respondents (response rate of 21%). All performed browlifts. The most widespread used techniques were: direct method (89.6% of surgeons), endoscopic (79.2%), and transblepharoplasty (60.4%). Of the total procedures performed, the endoscopic approach was performed the most (40.7%) followed by transblepharoplasty (26.2%) and direct (23.6%). For those performing small incision procedures, 95.2% used the endoscope during the procedure, and greater than 95% used the standard two paramedian and two temporal incisions. Temporal scalp elevation was most commonly done by suture fixation (63.2%), using 3-0 PDS most frequently, followed by scalp excision (15.8%). For paramedian fixation, the endotine alone( 32.5%), or in combination with another fixation method ( 47.5%), was most commonly used. Weakening of the corrugators and procerus muscles was done (87.5%) of the time, using mainly myotomy (37.5%) or a myotomy/botox combination (27.1%). For nausea control, Zofran ( 62.8%), IV fluids ( 93.0%), and Decadron (86.0 %) or some combination thereof were used intraoperatively. There were no clear preferences on post-operative nausea management. Most surgeons used a combination of a codeine derivative and acetaminophen for analgesia. The majority (79.2%) of all surveyed said they expected to increase the number of browlifts performed using an endoscope in 2005. Conclusions: Among oculofacial surgeons, the direct browlift approach was used by the greatest number of respondents, followed by the endoscopic and transblepharoplasty techniques. However, significantly more total procedures were done using an endoscopic approach than any other technique. The majority of respondents expect to increase the number of browlifts they will perform in 2005. Enthusiasm for the endoscopic technique remains high. Bibliography: 1. Chiu ES, Baker DC. Endoscopic Brow Lift: A retrospective review of 628 consecutive cases over 5 years. Plast Reconstr Surg. 2003;112(2):628-633. 2. Kikkawa DO. Small incision nonendoscopic browlift. Ophthal Plast Reconstr Surg. 2000;16(1):28-33. 3. Vasconez LO, Core GB, Gamboa-Bobadilla M, Guzman G, Askren C, Yamamoto Y. Endoscopic techniques in coronal browlifting. Plast Reconstr Surg. 1994;94(6):788-793. Author Disclosure Block: C.L. Betts, None; D.B. Lyon, None. Non-Bone Fixation During Subperiosteal Brow Lift Surgery Ioannis Mavrikakis, MD, PhD, Eleni Tsesmetzoglou E, Raman Malhotra. Corneo Plastic Unit, Queen Victoria Hospital, East Grinstead. Introductory Sentence: To report the efficacy of non-bone soft tissue fixation, during small incision subperiosteal forehead and brow lift. Methods: This is a retrospective case series of 19 patients over 12 months. 16 patients underwent bilateral and 3 unilateral surgery. Unilateral surgery was performed in patients with facial palsy and was augmented with cable suspension. 11 patients underwent associated blepharoplasty. In all cases, forehead fixation was achieved using Y-V scalp incisions with periosteal sutures and skin clips. Results: All patients achieved a desirable brow lift and contour. Follow up ranged from 2-11 months. One patient developed brief postoperative bleeding from one of the small incision sites. No alopecia was noted in any case. Sensory loss posterior to a scalp incision occurred in one patient and recovered by 4 months. Conclusions: Our results suggest that Y-V scalp incisions with periosteal sutures are safe and achieve a desirable height during small incision brow lift. They take significantly less time than bone fixation but may occasionally produce a less predictable browlift. Bibliography: Troilius C. Subperiosteal brow lifts without fixation. Plast Reconstr Surg 2004;114(6):1595-603 De Cordier BC, de la Torre JI, Al-Hakeem MS, et al. Endoscopic forehead lift: review of technique, cases, and complications. Plast Reconstr Surg 2002;110(6):1558-68 Holck DE, Ng JD, Wiseman JB, Foster JA. The endoscopic browlift for forehead rejuvenation. Semin Ophthalmol 1998;13(3):149-57. Author Disclosure Block: I. Mavrikakis, None; E. Tsesmetzoglou E, None; R. Malhotra, None. Brow Lifting: Operative Techniques Using Transblepharoplasty Approach with Internal Fixation Device Sterling S. Baker, MD1, David E. Holck, MD2, Erin L. Holloman, MD1. 1 Oklahoma city, OK, 2Wilford Hall Medical Center, San Antonio, TX. Introductory Sentence: Brow elevation is addressed by many surgical efforts, including a transblepharoplasty approach. Techniques for brow fixation through an upper eyelid incision using the Endotine TransBlephTM device (Coapt Systems, Inc) are presented. Methods: As a new approach for a modified fixation device, the surgical techniques and subsequent refinements developed over the course of treatment of the authors' first 100 consecutive patients are examined. Management of intraoperative and postoperative complications will be discussed. Results: Satisfactory results with rapid placement of devices, minimal additional surgical manuevers and instrumentation, and no major complications were obtained with this technique. Conclusions: Endotine fixation to treat brow ptosis can be safely, effectively, and reproducibly incorporated into current upper eyelid blepharoplasty surgery. The advantages of this technique include minimal modification of current skills, short operative time, familar approach and anatomy, and no requirement for endoscopy. Bibliography: none Author Disclosure Block: S.S. Baker, Coapt Systems Inc P, I, C, S, C, T; D.E. Holck, None; E.L. Holloman, None. Brow Lifting using the Transbleph Endotine Fixation System William P. Mack, MD1, John G. Rose, Jr., MD2, Mark J. Lucarelli, MD2, Cat N. Burkat, MD2. 1 University of South Florida, Tampa, FL, 2University of Wisconsin, Madison, WI. Introductory Statement: Fixation of the brow through an internal browpexy approach has included various techniques and methods of fixation. The authors describe a recently FDA approved device, the Endotine transbleph fixation system, which is inserted through a conventional blepharoplasty incision. The bioabsorbable Endotine implant allows subperiosteal multipoint soft tissue fixation via a three tined (3.0 mm or 3.5 mm) design. This technique allows an alternative, less invasive brow lift procedure for patients with mild to moderate brow ptosis. Methods: Twenty-one consecutive patients who were undergoing internal browpexy in combination with an upper eyelid blepharoplasty elected to receive the Endotine transbleph device. All patients received the device containing the 3 mm tines. The patients were subsequently evaluated at 1 and 3 months post operatively. The degree of brow elevation and patient satisfaction were noted. Results: All patients were satisfied with the obtained surgical results. No patients in the study had any significant complications. Five patients could feel the tines upon palpation. One had temporary discomfort. The degree of brow elevation and patient satisfaction were noted. Conclusions: The Transbleph Endotine fixation system allows the surgeon to achieve satisfactory brow elevation. Long term results as compared to other methods of fixation are not yet known. There was no evidence of any significant complications. Potential side effects may include extrusion or poor absorption of the implant. A learning curve is associated with the drilling of the fixation hole and placement of the multipoint fixation device in the subperiosteal plane. Author Disclosure: W Mack, None; J Rose, None; M Lucarelli, None, C Burkat, None. Author Disclosure Block: W.P. Mack, None; J.G. Rose, None; M.J. Lucarelli, None; C.N. Burkat, None. Lasing The Posterior Surface Of Orbicularis Muscle To Tighten The Lower Eyelid Skin During Lower Blepharoplasty Joseph A. Mauriello, Jr., MD. Cosmetic Eyelid and Facial Rejuvenation Center, Summit, NJ. Introductory Sentence: Lasing the posterior surface of the orbicularis oculi muscle during lower blepharoplasty serves to tighten the eyelid skin and when combined with orbicularis muscle resuspension effectively elevates the upper cheek during lower blepharoplasty. Methods: This technique has been modified over the past 7 years. A subciliary skin incision is made 5 mm medial to the lateral canthus and is extended 5 mm beyond the lateral commissure. A skin-muscle flap is developed across the lower eyelid and into the cheek over the inferolateral orbital rim with a carbon dioxide laser as an incisional device (4 to 5 watts). In patients judged to have significant anterior lamellar redundancy, the posterior orbicularis muscle flap is then treated in a defocused mode to effect additional immediate (and delayed) contraction. Minimal skin excision is necessary due to tissue tightening. The skin-orbicularis muscle flap is resuspended to the lateral orbital periosteum with a single 50 Vicryl suture (1). Horizontal eyelid tightening is accomplished by a single horizontal mattress “V” 5-0 polydiaxanone suture that engages partial thickness tarsus at its lateral aspect (1). Results: Data were available from 32 patients. The mean distance of elevation of the eyelid-cheek skin interface was 3.49 mm. The mean followup period was 4.25 months after surgery. Complications were minimal but included prolonged, but self-limited skin erythema in one patient and mild lower eyelid retraction in a second patient. Conclusions: Tissue tightening of the posterior orbicularis surface with a carbon dioxide laser combined with resuspension of the orbicularis flap is an effective method of elevating the eyelid-cheek skin interface (2). The tissue tightening forms a contracted template of the lower eyelid anterior lamella and avoids the necessity to excise excessive lower eyelid skin. Concomitant horizontal eyelid tightening supports the lateral canthus and the resuspended skin muscle flap. Bibliography: 1. Mauriello JA. Upper and lower blepharoplasty with combined blepharoptosis repair pp. 28-66 in Techniques of Cosmetic eyelid surgery. A Case Study Approach edited by Mauriello, JA, Lippincott Williams & Wilkins. Baltimore, Maryland, 2004. 2. Seckel BR, Kovanda CJ, Cetrulo CL Jr, Passmore AK, Meneses PG, White T. Laser blepharoplasty with transconjunctival orbicularis muscle/septum tightening and periocular skin resurfacing: a safe and advantageous technique. Plast Reconstr Surg. 2000;106(5):1127-41. Author Disclosure Block: J.A. Mauriello, Williams and Wilkins, Baltimore, Maryland, author of textbook, Techniques of Cosmetic Eyeld Surgery: A case study approach P. Symmetry in Healing After Bilateral Eyelid Surgery Mark P. Hatton, M.D.1, John M. Kelley, Ph.D2, Peter A.D. Rubin, M.D.1. 1 Massachusetts Eye and Ear Infirmary, Boston, MA, 2Massachusetts General Hospital, Boston, MA. Introductory Sentence: Ptosis repair and blepharoplasty typically result in post-operative ecchymosis and edema. When performed bilaterally there is usually little, if any, variation in the procedure between each side. However, many patients experience different rates of healing on each side despite having undergone identical surgeries. Methods: Seventeen patients undergoing symmetric bilateral upper eyelid surgery (ptosis repair and or blepharoplasty) were provided with a questionnaire at the day of surgery. They were asked on post-operative days 1, 3, 5, and 7 to document whether one eye was more swollen, whether one eye was more bruised, and whether one eye was more uncomfortable. Each question was written with multiple choice answers allowing them to choose “right eye”, “left eye”, or “both equal”. A digital camera was used to photograph a different cohort of 10 patients at the 1 week post-operative visit. Identical photographic techniques were used for each patient, including camera, lighting source and position, focal length, aperture settings, and head position. Digital photographs were analyzed with NIH ImageJ 1.27 software. Visible bruising was traced and the resulting area calculated. Results: Asymmetry in bruising and swelling was reported by the majority of patients at each time point (Table). Seven days after surgery, 71% of patients reported asymmetry in the amount of bruising present. Quantitatively, at the 1 week visit 50% of patients had more bruising on the right and 50% had more bruising on the left. The measured area of bruising per side ranged from 473 mm2 to 2339mm2 . The average area of bruising was 1523.9 mm2 for the right eye and 1454.5 mm2 for the left eye. On average, the mean difference in area of bruising between sides in each patient was 10% (median 6%), and 8 of 10 patients had less than 10% difference in area of bruising between sides. A paired t-test comparing right to left bruising showed that differences were not statistically significant (t(9)=.98,p=.35). Percent of Patients Reporting Asymmetry in Symptoms Symptom Day 1 Day 3 Day 5 Day 7 Bruising Swelling Discomfort 65 82 41 88 88 53 85 65 47 71 41 41 Conclusions: Despite undergoing identical surgery, many patients perceive asymmetry in bruising, swelling, and discomfort at all time points in the 1st post-operative week. However, at 1 week visit objective measurements of bruising demonstrated that asymmetry was minor. These findings will allow surgeons to reassure patients that perceived asymmetry during the 1st post-operative week is to be expected. Bibliography: n/a Author Disclosure Block: M.P. Hatton, None; J.M. Kelley, None; P.A. Rubin, None.