MS2 HEENT Stroke
advertisement
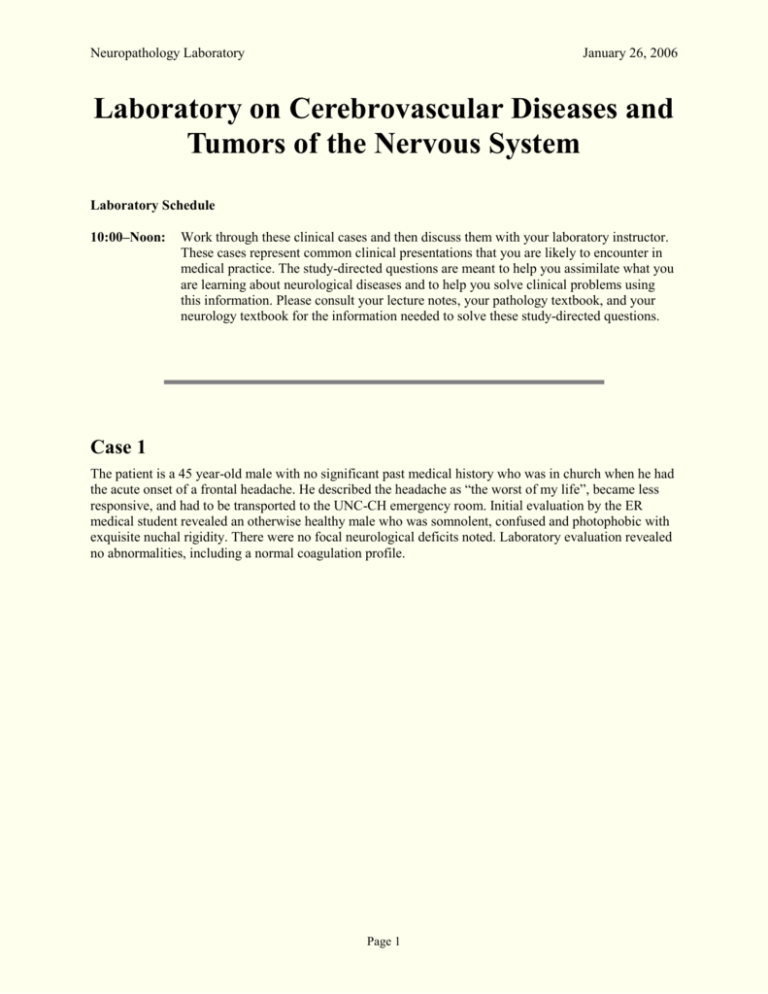
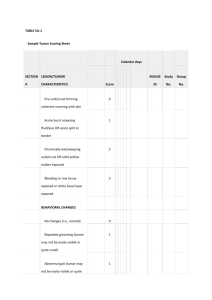
Neuropathology Laboratory January 26, 2006 Laboratory on Cerebrovascular Diseases and Tumors of the Nervous System Laboratory Schedule 10:00–Noon: Work through these clinical cases and then discuss them with your laboratory instructor. These cases represent common clinical presentations that you are likely to encounter in medical practice. The study-directed questions are meant to help you assimilate what you are learning about neurological diseases and to help you solve clinical problems using this information. Please consult your lecture notes, your pathology textbook, and your neurology textbook for the information needed to solve these study-directed questions. Case 1 The patient is a 45 year-old male with no significant past medical history who was in church when he had the acute onset of a frontal headache. He described the headache as “the worst of my life”, became less responsive, and had to be transported to the UNC-CH emergency room. Initial evaluation by the ER medical student revealed an otherwise healthy male who was somnolent, confused and photophobic with exquisite nuchal rigidity. There were no focal neurological deficits noted. Laboratory evaluation revealed no abnormalities, including a normal coagulation profile. Page 1 Neuropathology Laboratory January 26, 2006 He was transported to the CT scanner, and the unenhanced scan is shown below: See lots of diffuse white stuff (blood) – speaks to being subarachnoid – this is the place we can bleed and have diffuse pattern of blood Question 1: With respect to the surrounding brain parenchyma, the appearance of acute hemorrhage on CT scan is described as… a) hyperdense b) hypodense c) invisible d) isodense Question 2: The most likely diagnosis in the above patient is… a) acute epidural hematoma b) acute subdural hematoma c) intracerebral hematoma d) subarachnoid hemorrhage Question 3: The most common cause of subarachnoid hemorrhage in a man with this clinical history is… a) aneurysmal rupture b) arteriovenous malformation hemorrhage c) hemorrhage from tumor d) trauma Question 4: The most common cause of subarachnoid hemorrhage is… a) aneurysmal rupture b) arteriovenous malformation hemorrhage c) hemorrhage from tumor d) trauma – often it’s minor and doesn’t cause as many symptoms Page 2 Neuropathology Laboratory January 26, 2006 The patient subsequently deteriorated neurologically and was transported to the ICU (intensive care unit) for further management. Angiography of the left internal carotid artery (arrow identifies carotid siphon) revealed the following lesion (arrowhead): He continued to deteriorate and eventually died. Postmortem examination revealed acute subarachnoid hemorrhage and a ruptured berry aneurysm. Question 5: All of the statements about the locations of saccular (berry) aneurysms are true except… a) 5-15% occur in the posterior circulation b) they occur at arterial bifurcations c) commonest sites are anterior and posterior communicating and middle cerebral arteries d) 85-95% occur in the anterior circulation e) all aneurysms eventually rupture YOU ARE BORN WITH THE INTIMAL CHANGES BUT ANEURYSM DOESN’T COME ABOUT UNTIL LATER IN LIFE!!! See atherosclerosis in some walls and other walls are thin – don’t have much MEDIA. (Slide E92—Berry aneurysm). This section from the circle of Willis and has been stained with the Verhoeff-van Gieson method. The cerebral arteries show a thin intima, black-staining internal elastica, green-staining media, and red-staining adventitia. Note the absence of an external elastica, a normal feature of intracranial arteries. The wall of the aneurysm shows absence of internal elastica and media. Also note that there is considerable atherosclerosis, which is a secondary change. Question 6: Berry aneurysms are… a) a consequence of atherosclerosis b) associated with polycystic kidney disease c) congenitally present d) most often on the vertebrobasilar system e) usually multiple Page 3 Neuropathology Laboratory January 26, 2006 Question 7: All of the following statements about berry aneurysms are true except… a) they are often associated with aneurysms of the aorta b) aneurysmal rupture is associated with a high rate of morbidity and mortality c) they are likely to cause increased intracranial pressure after rupture d) they are likely to cause vasospasm after rupture e) they are likely to rebleed after initial rupture Case 2 The patient, a 50 year-old black man, collapsed at work after complaining of the sudden onset of a severe headache. Upon arrival at the ER, his vital signs were temperature 36.7°C, pulse 110 bpm, respirations 28/min, and blood pressure 220/110 mmHg. He was awake but drowsy, complained of a right-sided headache, and was noted to have a left hemiparesis. His family reported that he had been in good health. His chest radiograph showed cardiomegaly. A CT scan of his head is shown below: -- should be dealing with motor cortex which is frontal Question 1: The CT scan reveals… a) acute contusions b) acute ischemic infarct c) intracerebral hematoma –bleed and get mass effect with edema also pouring in – so the right uncus is going to herniate d) subarachnoid hemorrahge e) subdural hemorrhage The patient’s blood pressure remained highly elevated, and he sequentially developed dilatation of his right pupil (nerve compression from uncal herniation and cranial nerve 3 messed up), then left pupil (because cranial nerve 3 on the left side gets squished), and finally fixed and dilated pupils. As he became progressively more obtunded and eventually comatose, he developed right-sided hemiplegia (now everything in the midbrain is getting squished). He died two days later. Page 4 Neuropathology Laboratory January 26, 2006 An autopsy was performed, and a coronal section of the brain is illustrated below. Question 2: The lesion is… a) epidural b) extra-axial c) intra-axial d) subarachnoid e) subdural Question 3: The specimen clearly shows all of the following except… a) blood extending into the ventricular system b) local destruction of brain tissue c) mass effect d) right-to-left shift e) secondary brainstem (Duret) hemorrhages Question 4: The most likely underlying cause of the lesion shown is… a) atherosclerotic plaque b) bleeding disorder c) congenital malformation of blood vessels d) embolus e) hypertension – which vessel bled? Lenticulo-striate arteries bled!!!! His motor deficit is coming from IC being messed up!! Question 5: A significant complication of lumbar puncture (LP) in this patient would be… a) excessive CSF leakage from the LP site b) herniation – whenever there’s mass effect never do an LP because could cause a herniation c) infarction d) infection e) sympathetic discharge and elevation in blood pressure Page 5 Neuropathology Laboratory January 26, 2006 Question 6: What is the etiology of the patient’s new right-sided hemiplegia? a) increasing size of hematoma b) compression of right side of brainstem by herniating uncus and parahippocampal gyrus c) compression of left side of brainstem by edge of the tentorial incisure d) subfalcine herniation Page 6 Neuropathology Laboratory January 26, 2006 Case 3 A 64 year-old white male presents to the ER at 9 am. His son states that his father is “confused”. This state came on abruptly while watching television around 11 pm last night. There has been no subsequent change in his condition. He has a history of smoking 1.5 packs per day, hypertension, type II diabetes, and angina. On exam, his vital signs are temperature 37.6°C, heart rate 76 bpm, respirations 15, and blood pressure 154/93 mmHg. The patient appears awake, alert and in no distress. His speech is nonsensical, but he has no difficulty producing words. He has difficulty comprehending both spoken and written commands. Strength and sensation appear intact. He has a right visual field cut. His MR scan is below: T2-weighted MRI FLAIR image (to highlight brain edema) Question 1: The above MRI scans reveal… a) acute brain infarct b) chronic infarct c) contusion d) metastatic lung carcinoma e) subarachnoid hemorrhage Question 2: The lesion is located in… a) Broca’s area b) Hecht’s area c) Motor cortex d) Visual cortex e) Wernicke’s area Question 3: This lesion most likely resulted from… a) embolus from right ventricle (paradoxical embolus) b) loss of blood flow in right middle cerebral artery c) loss of blood flow in left middle cerebral artery d) loss of blood flow in left posterior cerebral artery e) loss of blood flow in left vertebral artery Page 7 Neuropathology Laboratory January 26, 2006 (Slide E69—Acute Infarct). This H&E-stained section of temporal lobe includes the hippocampus. There is widespread acute ischemic neuronal necrosis in the hippocampal neurons, as evidenced by neurons with pink cytoplasm (red neurons) and pyknotic nuclei. Note the paucity of ischemic cell change in the white matter, despite the widespread acute ischemic neuronal injury in the gray matter. A few inflammatory cells are in the leptomeninges. This infarct appears histologically to be about one day old. Acute infarct. The tissue is discolored, swollen, very soft and necrotic and is becoming demarcated (arrow) from the adjacent viable brain. The infarct is 2–3 days old. By comparison, the remote infarct in the right panel is many months or years old Remote infarct. The necrotic tissue has been completely resorbed, so that the infarct is now only a cavity. The residual tissue in the infracted area is collapsed leptomeninges and blood vessels. The brain tissue around the edge of the infarct would show atrophy and gliosis microscopically. Question 4: The acute infarct in the illustration is… a) a global infarct b) a hemorrhagic infarct c) a lacunar infarct d) a watershed infarct e) capable of having a mass effect Question 5: Infarcts often… a) involve the crowns of gyri (contusions) more than perisulcal cortex b) involve the perisulcal cortex more than the crowns of gyri c) involve white matter more than gray matter – it’s the opposite of this!! d) predispose to primary intracerebral hemorrhage Page 8 Neuropathology Laboratory January 26, 2006 Case 4 The patient is a 65-year-old male who presents to the UNC emergency room with new onset seizures(new onset anything could be stroke). His wife explains that he has been complaining of headaches for two weeks (so it’s probably not acute) and has been increasingly forgetful. Examination reveals a thin male in no acute distress. He is alert but confused. He has no focal weakness or numbness (ascending and descending tracts and cortical regions). Past medical history reveals no other medical problems. An enhanced CT scan of the patient’s head is shown below. What you’re seeing here is a butterfly ring-enhancing lesion (blood-brain barrier is broken down) – see ventricles too! Where would it actually be? The CC – white matter – this is suggesting a glioma (Astrocytes). The arrows are pointing to dark areas of edema, if it’s the same color as ventricular fluid then it’s ventricular fluid. No one was able to elicit focal signs and symptoms! Why the headaches? Increased intra-cranial pressure – this is because of the mass effect because more material has been pushed into the vault Question 1: The lesion in the scan has all of the following features except… a) extra-axial lesion b) intra-axial lesion c) involves both hemispheres d) ring enhancing lesion Question 2: The most common type of primary brain tumor is… note that mets to the brain are more common a) glioma b) meningioma c) metastasis d) pituitary adenoma e) schwannoma Page 9 Neuropathology Laboratory January 26, 2006 Question 3: The most common type of glioma is… a) anaplastic astrocytoma b) ependymoma c) glioblastoma –GBM – these are high grade, bad that the worst of the options is what we’re getting! – this is a TUMOR OF JUST THE ASTROCYTES (NOT OF ALL GLIAL CELLS) d) oligodendroglioma Question 4: All of the following are common in the posterior fossa (cerebellum and brainstem) of children except… why is this even a discussion? Most childhood CNS tumors are in the posterior fossa whereas adults have tumors anteriorly -a) ependymoma – ependyma – cells lining vetricles -- YES b) glioblastoma (GBM) – it could happen in the white matter – this is the worst version; adults get it c) medulloblastoma – “blast” means undifferentiated – “small round blue cell tumors of childhood” d) pilocytic astrocytoma – belongs in the glioma, of the astrocytes, it’s the best differentiated (grade I) – this is the best version; kids get it adults: glioblastoma (GBM), mets, meningioma – are most common of CNS Question 5: The most common type of astrocytoma is… a) anaplastic astrocytoma (grade 3) b) astrocytoma (grade 2) c) glioblastoma (grade 4) d) pilocytic astrocytoma (grade 1) Question 6: The most common location and age for glioblastoma is… a) brainstem, adult b) cerebrum, adult c) cerebrum, child d) cerebellum, child The patient underwent biopsy of the above lesion. The biopsy tissue is available for your diagnosis. (Slide 5301). This section of the cerebrum, including cortex, white matter and leptomeninges, has been stained with H&E. Within the white matter is an area of increased cellularity. The pleomorphic cells in this area have indistinct cytoplasm and hyperchromatic nuclei that vary from small to occasionally very large. Note that the neoplastic cells infiltrate the white matter, and that there is no sharp border between normal white matter and tumor. Normally white matter looks like pink strands with the occasional nucleus of a glial cell – grade 4 is GBM (have necrosis and mitotic figures) This is too cellular so we’re looking for necrosis but we DO see hemorrhage Pleomorhpic nuclei Page 10 Neuropathology Laboratory January 26, 2006 Question 7: What is your diagnosis of this brain biopsy, based on the above histology? a) infiltrating glioma b) meningioma c) lymphoma d) metastasis Examination of other histologic sections from this neoplasm revealed the histological findings illustrated below. An area of tumor necrosis is starred. NECROSIS IS THE TIPOFF FOR GBM Question 8: What is your diagnosis, given this additional finding? a) anaplastic astrocytoma b) ependymoma c) glioblastoma d) oligodendroglioma Question 9: The hypodense regions (white arrows) in the frontal white matter on the CT scan represent… a) cytotoxic edema b) ischemic infarction c) necrosis d) vasogenic edema – why? Because it’s in the white matter! Vasogenic is the type you get in white matter because cytotoxic involves cells which are in grey matter. Page 11 Neuropathology Laboratory January 26, 2006 While seeing patients in clinic the following day, a 67 year-old gentleman presents with a similar history of new-onset seizures and an additional history of lung cancer. His MRI scan with gadolinium is below. See multi-focal well circumscribed lesions Question 10: The most likely diagnosis is… a) brain abscesses b) metastatic lung cancer c) multicentric glioblastoma d) pilocytic astrocytoma This 67-year-old man subsequently died, and an autopsy was performed. A section from a brain lesion is submitted for your diagnosis. (Slide E73). This H&E-stained section of cerebrum shows a sharply circumscribed metastasis. The neoplastic cells form sheets and cords within a fibrous stroma. Foci of tumor necrosis are also present. The neural tissue surrounding the metastasis shows a mild reactive astrocytic proliferation (gliosis). Page 12 Neuropathology Laboratory January 26, 2006 Representative gross photographs of a glioblastoma and a brain metastasis are presented below for correlation with the radiographic scans from cases in the laboratory today. Can see normal grey, white, and meninges – see a sulcus too! See the white matter is getting filled up with tumor – mets like to occur at the grey-white jxn and we’re there! The tumor’s been spreading into the white matter Pink areas are necrosis – know that lung cancer can be adeno, squamous, Glioblastoma multiforme CAT scan with contrast Metastatic carcinoma MRI with contrast Page 13 Neuropathology Laboratory January 26, 2006 Case 5 The patient is a 70-year-old white male who presents with right frontal headaches and new onset seizures (we don’t really know if this is acute or chronic). Neurological examination revealed mild left-sided weakness (R side brain, pre-cenral so frontal lobe) and no sensory deficits. A CT scan of the head and an MRI of the brain were obtained and are shown below. CT Scan with contrast; Horizontal plane Sagittal, T1-weighted MR with gadolinium Coronal, T1-weighted MR with gadolinium Question 1: In the above CT and MR scans, the mass may be described as… a) contrast-enhancing b) dural-based c) extra-axial d) all of the above e) none of the above Question 2: Most common locations of intracranial meningiomas include all of the following except… a) convexity b) olfactory groove c) parasagittal/falcine region d) posterior fossa e) sphenoid ridge Question 3: All of the following statements about meningiomas are true except that they… a) frequently arise near the dural sinuses b) may involve surrounding bone c) are more common in adults than children – remember one of the adult “M’s” d) are more common in women than men e) are commonly malignant Question 4: Other than meningioma, which of the following tumors tends to involve the dura mater? a) choroid plexus papilloma – this is really far away -- ventricles b) ependymoma -- ventricles c) glioma –white matter d) metastatic carcinoma – they can go anywhere anyways!! Page 14 Neuropathology Laboratory January 26, 2006 The above patient was subsequently taken to surgery where a craniotomy and excision of the lesion were performed. The biopsy tissue is submitted for your diagnosis. (Slide 5300). The slide is a section of a meningeal-based neoplasm and contiguous cerebral cortex and has been stained with H&E. The benign-appearing neoplastic cells have oval nuclei and moderate amounts of pale staining cytoplasm. In a few areas the cells cluster to form small cellular whorls. Another characteristic feature found in some of these neoplasms is the presence of psammoma bodies. Note that the tumor compresses, but does not infiltrate, the surprisingly well-preserved underlying cerebral cortex. Notice how cellular it looks – when you get the slide though, note that the tumors can all look similar but work on the location! Psomomma bodies – calcium and junk together – these Ca++ would definitely show up on X-ray Question 5: The cell of origin of the meningioma is the… a) arachnoid cap cell b) astrocyte c) ependymal cell d) fibroblast A representative gross photograph of a parasagittal meningioma is presented below for correlation with the radiographic scans from this case. LOOK AND SEE THAT MENINGIOMA IS RIGHT IN THE MIDDLE Page 15 Neuropathology Laboratory January 26, 2006 Case 6 The patient is a 55-year-old female who presents with a 6-month history (CHRONIC – WE’RE THINKING TUMOR) of progressive left-sided hearing loss. Upon further questioning, she also reports tinnitus and dysequilibrium. Neurological examination reveals hearing loss in the left ear. Audiometry revealed a sensorineural hearing loss in the left ear. The patient had the MRI scan shown below. The abnormality on the scan is marked with an arrow. Axial (horizontal), T1-weighted MRI Coronal, T1-weighted MRI with contrast Note that this has to be outside the CNS because once auditory information enters the CNS it becomes bilateral – This is a schwannoma Question 1: The cranial nerve involved by this tumor (arrows) is most likely… a) III b) IV c) VIII d) X e) XI Question 2: Tumors that usually involve the cerebellopontine angle (in the CT on the left) include all of the following except… a) meningioma b) metastasis c) neurofibroma – you can’t just take these tumors off because they’re infiltrating the axons!!! These grow more peripherally d) schwannoma This patient had the lesion excised. The tissue is submitted for your diagnosis. (Slide E99). This section of a tumor arising within the eighth cranial nerve and has been stained with H&E. The tumor is composed of spindle-shaped cells (spindle cell tumor). Note that this tumor shows a Page 16 Neuropathology Laboratory January 26, 2006 biphasic histologic pattern, with compact areas (Antoni A pattern) of tumor and loose, edematous areas (Antoni B pattern) of tumor. Antoni A pattern predominates in this section. Note the tendency for the spindle shaped nuclei to palisade, i.e., align, parallel to their long axis. These palisades are called Verocay bodies. These schwann cells are spindle shaped (AREA A) nuclei that head off in different directionsat low power – Also see areas that are edematous (AREAS B) Question 3: Based on the histology of the tumor, the diagnosis is… a) meningioma b) neurofibroma c) neuroma d) schwannoma e) none of the above Question 4: All of the following are true for both schwannoma and neurofibroma except… a) both are comprised primarily of Schwann cells b) both are usually associated with an inherited disease – neurofibroma is associated with an inherited disease (neurofibromatosis) c) both may arise on spinal nerve roots d) only neurofibroma has a significant potential for malignant degeneration to sarcoma – schwannoma is truly a benign tumor whereas neurofibroma is sometimes an “oma” and sometimes becomes “sarcoma” e) the “acoustic neuroma” is almost always a schwannoma Gross photograph of a vestibular schwannoma for correlation with the radiographic scan from this case. The scan below (coronal T1 MRI with contrast) shows bilateral eighth-nerve schwannomas (arrowheads). Page 17 Neuropathology Laboratory January 26, 2006 Question 5: The diagnosis in the above patient, based on this coronal MR scan with gadolinium, is… a) neurofibromatosis type 1 (NF-1) b) neurofibromatosis type 2 (NF-2) c) Osler-Weber-Rendu syndrome d) Tuberous sclerosis e) Von Hippel-Lindau syndrome Page 18