HIS Outpatient Services Literature
advertisement

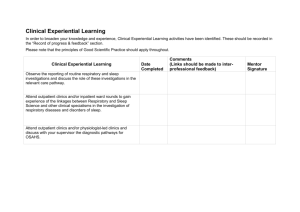
Outpatient Services: literature review summary Question Reference 1. What can be done in the primary care or community setting to reduce pressure on outpatient clinics? 1, 9, 14 2. What can be done to decrease the numbers of new and return appointments to the outpatient clinics? 7, 12, 16 3. How can outpatient appointments be used more effectively? 3 - 6, 8, 13, 15 & 17 - 24 4. How can efficiency be improved by reducing variation and overall demand and what are the resultant effects on savings and cost containment? 2, 10, 11, 13 25 - 35 The tables in this report are an overview of the evidence base presented in two separate reports on the UK and international evidence on interventions to improve delivery of outpatient care, produced by Healthcare Improvement Scotland in February and December 2012. Table 1 lists the references for each type of study found, Table 2 shows potentially successful interventions and in which study they appear, Table 3 shows the interventions which were shown to be ineffective and Table 4 shows the interventions for which there was inconclusive findings (and which therefore may warrant further study). Although not essential, it may be beneficial to read this document in conjunction with the more detailed presentation of the evidence contained in the original reports. Only 4 studies included in the reports contained costing or economic data and these are highlighted at the bottom of Table 1. What is striking is the lack of crossover between UK and international studies with the exception of appointment reminders, alternative patient booking systems and outreach clinics. The reasons for this are due to the possibility of differing terminology which is masking the cross over in the type of interventions described as well as variations in the types of health care systems. One US study, for example, was carried out in order to determine if profits could be increased in a private clinic 17. One international systematic review also included studies from the UK 4 which is why it appears in both reference columns. Table 1: Evidence breakdown by study type Publication Type UK evidence Health Technology Assessment 2 Systematic review 3 Comprehensive scoping report 1 Structured review International evidence 14 24 Primary studies 4-13 15-23, 25-35 Studies which also included economic information 3 15, 17, 18 Outpatient Services: literature review summary Table 2: Potentially effective interventions UK evidence Intervention Discharge of patients to no follow up or patient-initiated follow-up or GP follow-up instead of routine outpatient follow-up. 1 Direct access for GPs to hospital-based tests or investigations or treatments, without approval of outpatient specialist. 1 Structured referral sheets prompting GPs to conduct necessary prereferral tests or treatments 1 GP and/or nurse education 1, 4 Triaging by pre-assessment and pre-specifying management plans 2, 11 Paper clinics (treatment plans based on medical records after outpatient appointment rather than further follow-up) International evidence 10, 13. Close monitoring of unnecessary visits based on pre-attendance test or investigation results 16 Waiting list validation 4 Text message surveillance of patients 13 Text message and paper based appointment reminders 3 22, 23 12, 7 33 Patient booking systems where patients can choose their appointment time and date, or variations Group medical appointments 17, 18, 19 Quick diagnostic clinics to reduce inpatient numbers by treating in outpatient services 15 Six Sigma modelling 26, 27, 28 Capacity modelling 30 Lean Management 31, 32 Supply and demand matching 35 Patient Letters in improving patient satisfaction or non-attendance rates. Nurse or service worker role extension 4, 5, 6, 8 4 Table 3: Ineffective Interventions Intervention UK evidence Relocation of specialists to primary care settings 1 Joint working between primary and secondary clinicians 1 Outreach clinics 14 Nurse led telephone service 4 Referral proformas 4 International evidence 14 Outpatient Services: literature review summary Table 4: Inconclusive Interventions Intervention UK evidence GPs with special interest acting as substitute outpatient specialists. 1, 4 Transfer of care for common chronic conditions from secondary to primary care 1, 4 In-house second opinion prior to referral 1 One-stop clinic 9 Electronic Medical/Health Records 20, 21 Electronic Consultation (as augmentation to face to face consultations) 24 Flow modelling 25, 29 Risk assessment coupled with streaming into short or longer appointment times GP telephone access to consultants and specialist nurses International evidence 34 4 References UK Evidence 1. National Primary Care Research and Development Centre: University of Manchester. Outpatient services and primary care : a scoping review of research into strategies for improving outpatient effectiveness and efficiency [online]. 2005 Available from: http://www.medicine.manchester.ac.uk/primarycare/npcrdcarchive/Publications/Studyinghealthcare_Roland_finalreport.pdf. 2. NHS Quality Improvement Scotland. Service delivery organisation for acute low back pain. 2008. Available from: http://www.healthcareimprovementscotland.org/previous_resources/hta_report/hta_syste matic_review_1.aspx 3. Hasvold PE, Wootton R. Use of telephone and SMS reminders to improve attendance at hospital appointments: a systematic review. Journal of Telemedicine & Telecare. 2011;17(7):358-64. 4. Appleby A, Lawrence C. From blacklist to beacon, a case study in reducing dermatology outpatient waiting times. Clinical & Experimental Dermatology. 2001;26(6):548-55. 5. Hardy KJ, O'Brien SV, Furlong NJ. Quality improvement report: information given to patients before appointments and its effect on non-attendance rate. British Medical Journal. 2001;323(7324):1298-300. 6. Saunders NC, Georgalas C, Blaney SP, Dixon H, Topham JH. Does receiving a copy of correspondence improve patients' satisfaction with their out-patient consultation? Journal of Laryngology & Otology. 2003;117(2):126-9. 7. Lloyd J, Dillon D, Hariharan K. Outpatient clinics. Down the line. Health Service Journal. 2003;113(5837):22-3. 8. Fox AT, Palmer RD, Crossley JG, Sekaran D, Trewavas ES, Davies HA. Improving the quality of outpatient clinic letters using the Sheffield Assessment Instrument for Letters (SAIL). Medical Education. 2004;38(8):852-8. Outpatient Services: literature review summary 9. Sulaiman S, Wei CK, Gaudoin M. One-stop postmenopausal bleeding clinics reduce patient waiting times and theatre costs. Scottish Medical Journal. 2004;(4):152-4. 10. Rao GN, Basnyat P, Taffinder N, Hudson C, Insall R. Reducing surgical outpatient waiting is not the solution to meeting the 2005 colorectal cancer target. Colorectal Disease. 2006;8(2):1359. 11. Phillips SA, Ross PD, Chalmers K, MacDougall G. Can we improve dysphagia referrals? Journal of Laryngology & Otology. 2007;121(6):584-7. 12. Parmar V, Large A, Madden C, Das V. The online outpatient booking system 'Choose and Book' improves attendance rates at an audiology clinic: a comparative audit. Informatics in Primary Care. 2009;17(3):183-6. 13. Corrigan MA, McHugh SM, Murphy RK, Dhillon P, Shah A, Hennessy I, et al. Improving surgical outpatient efficiency through mobile phone text messaging. Surgical Innovation. 2011;18(4):354-7. International evidence 14. Gruen RL, Weeremanthri TS, Knight SS, Bailie RS. Specialist outreach clinics in primary care and rural hospital settings. 2012 [cited 20112 Jan 13];Available from: URL: http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD003798.pub2/pdf 15. Bosch X, Foix A, Jordan A, Coca A, Lopez-Soto A. Outpatient Quick Diagnosis Units for the evaluation of suspected severe diseases: an observational, descriptive study. Clinics 2011;66(5):737-41. 16. Donnellan F, Hussain T, Aftab AR, McGurk C. Reducing unnecessary outpatient attendances. International Journal of Health Care Quality Assurance 2010;(5):527-31. 17. Sidorsky T, Huang Z, Dinulos JG. A business case for shared medical appointments in dermatology: improving access and the bottom line. Archives of Dermatology 2010 Apr;146(4):374-81. 18. Davies S, Quintner J, Parsons R, Parkitny L, Knight P, Forrester E, et al. Preclinic group education sessions reduce waiting times and costs at public pain medicine units. Pain Medicine 2011 Jan;12(1):59-71. 19. De VB, rling-Fisher C, Thomas AC, Belanger-Shugart EB. Implementation and outcomes of group medical appointments in an outpatient specialty care clinic. Journal of the American Academy of Nurse Practitioners 2008 Mar;20(3):163-9. 20. Furukawa M. Electronic Medical Records and Efficiency and Productivity During Office Visits. AM J MANAGE CARE 2011;17(4):296-303. 21. McAlearney AS, Robbins J, Hirsch A, Jorina M, Harrop JP. Perceived efficiency impacts following electronic health record implementation: An exploratory study of an urban community health center network. Int J Med Inf 2010;79(12):807-16. 22. Kitcheman J, Adams CE, Pervais A. Timely encouraging letters increase attendance at first consultations at outpatient psychiatric clinics. 2008 [cited 2012 Jan 13];Available from: URL: http://ebmh.bmj.com/content/11/4/122.full.pdf+html?ath_user=efscsleith001&ath_ttok=%3 CTxBKYaNErN8EIL3n1g%3E 23. Downer SR, Meara JG, Da Costa AC. Use of SMS text messaging to improve outpatient attendance. MJA 2005;183(7):366-8. Outpatient Services: literature review summary 24. Caffery LJ, Smith AC. A literature review of email-based telemedicine. Studies in Health Technology & Informatics 2010;161:20-34, 2010.:20-34. 25. Zonderland ME, Boer F, Boucherie RJ, de RA, van Kleef JW. Redesign of a university hospital preanesthesia evaluation clinic using a queuing theory approach. Anesthesia & Analgesia 2009 Nov;109(5):1612-21. 26. Patrick J, Puterman ML. Improving resource utilization for diagnostic services through flexible inpatient scheduling: A method for improving resource utilization. J Oper Res Soc 2007;58(2):235-45. 27. Bush SH, Lao MR, Simmons KL, Goode JH, Cunningham SA, Calhoun BC. Patient access and clinical efficiency improvement in a resident hospital-based women's medicine center clinic. AM J MANAGE CARE 2007 Dec;13(12):686-90. 28. Daggy J, Lawley M, Willis D, Thayer D, Suelzer C, DeLaurentis PC, et al. Using no-show modeling to improve clinic performance. Health Informatics Journal 2010;16(4):246-59. 29. Parks JK, Engblom P, Hamrock E, Satjapot S, Levin S. Designed to Fail: How Computer Simulation Can Detect Fundamental Flaws in Clinic Flow. Journal of Healthcare Management 2011;56(2):135-44. 30. Elkhuizen SG, Das SF, Bakker PJM, Hontelez JAM. Using computer simulation to reduce access time for outpatient departments. Quality & Safety in Health Care 2007;16(5):382-6. 31. Casey JT, Brinton TS, Gonzalez CM. Utilization of lean management principles in the ambulatory clinic setting. Nature Clinical Practice Urology 2009 Mar;6(3):146-53. 32. Smith C, Wood S, Beauvais B. Thinking lean: implementing DMAIC methods to improve efficiency within a cystic fibrosis clinic. Journal for healthcare quality : official publication of the National Association for Healthcare Quality 2011;(2):37-46. 33. Price RS, Balcer LJ, Galetta SL. Education research: a new system for reducing patient nonattendance in residents' clinic. Neurology 2010 Mar 9;74(10):e34-e36. 34. Heijman TLJ, van der Bij AK, de Vries HJC, van Leent EJM, Thiesbrummel HFJ, Fennema HSA. Effectiveness of a risk-based visitor-prioritizing system at a sexually transmitted infection outpatient clinic. Sex Transm Dis 2007;34(7):508-12. 35. Rouppe van der Voort MM, van Merode FG, Berden BH. Making sense of delays in outpatient specialty care: a system perspective. Health Policy 2010 Sep;97(1):44-52.