Meropenem – beta lactam (carapenem group)
advertisement

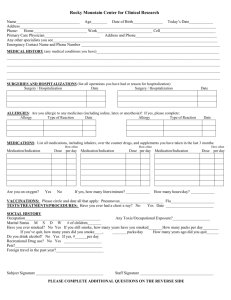
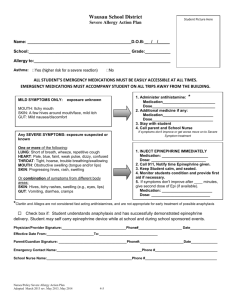
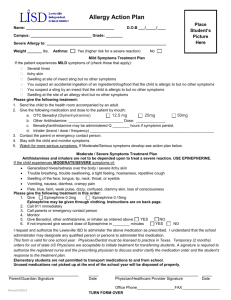
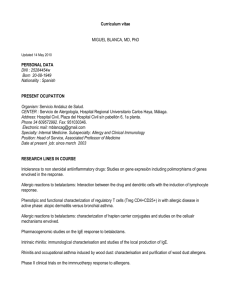
Antibiotic skin testing and challenge Patient XXXXX Intensive Care unit Skin testing SPT 1:1 IDT 1:100, 1:10, 1:1 Penicillin V & G Benzyl Penicillin Ambisome Meropenem IV challenge Meropenem – beta lactam (carbapenem group) IV challenge Issues to note: Renal impairment *Use normal dose every 12 hours if eGFR 26–50 mL/minute/1.73 m2; use half normal dose every 12 hours if eGFR 10–25 mL/minute/1.73 m2; use half normal dose every 24 hours if eGFR less than 10 mL/minute/1.73 m2 IV Challenge As symptoms were reported to be limited to generalised rash the incremental doses can be minimised to a few steps. 1% of total dose 4% of total dose 10% of total dose 20% of total dose 30% of total dose 35% of total dose An observation period of 15 minutes between steps is appropriate. Delayed reactions are possible. Notes Carbapenems differ from penicillins in that they are unsaturated and contain a carbon atom instead of sulphur in the thiazolidine ring. Incidence Penicillin allergy is reported in up to 10% of patients. At the same time, more than 90% of them are found to lack penicillin-specific IgE and can tolerate the antibiotic safely. Anaphylaxis: 0.015-0.04% (1.5-4/10,000) of treated patients; 1.23/10,000 injections in children and young adults population; 2.17/10,000 in prophylactic treatment in healthy military recruits. Incidence of anaphylaxis to cephalosporins and other beta-lactams has not been studied in largescale surveys but it is lower than with penicillin. Studies suggest that anaphylactic reactions to cephalosporin are rare, 0.0001 to 0.1%. However, death has been reported. The incidence of cutaneous reactions range from 1% to 3%. Risk factors A previous life-threatening reaction, such as anaphylactic shock with penicillin Concomitant illness, such as cardiovascular disease, respiratory or oncologic problems Patients who are taking certain drugs, such as beta-blockers. Clinical manifestations Immediate (< 1 h): anaphylactic shock, urticaria, angioedema, laryngospasm, bronchospasm. Cutaneous manifestations: Delayed reactions (>1 h): Maculopapular rash (ampicillin and amoxycillin with or without Epstein-Barr virus infection), urticaria, angioedema, erythroderma Acute generalized exanthematous pustulosis (amoxycillin or amoxycillin with clavulanate) Baboon syndrome and SDRIFE (Symmetrical Drug-Related Intertriginous and Flexural Exanthema): appears within a few hours or days after administration (amoxycillin) Erythema multiforme, Stevens-Johnson syndrome and toxic epidermal necrolysis Serum sickness (cefaclor +++, children; amoxycillin) Fixed drug eruption (amoxycillin) Childhood linear IgA bullous disease (amoxycillin) *eBNF accessed 14/02/2012 Padial A, Antunez C, Blanca-Lopez N, et al. Non-immediate reactions to beta-lactams: diagnostic value of skin testing and drug provocation test. Clin Exp Allergy 2008;38:822-8. Torres MJ, Blanca M, Fernandez J, et al. Diagnosis of immediate allergic reactions to beta-lactam antibiotics. Allergy 2003 ;58:961-72. Romano A, Blanca M, Torres MJ, et al. Diagnosis of non-immediate reactions to beta-lactam antibiotics. Allergy 2004;59:1153-60. Torres MJ, Blanca M, and the European Network for Drug Allergy and the EAACI interest group on drug hypersensitivity. Importance of skin testing with major and minor determinants of benzylpenicillin in the diagnistic of allergy to betalactams. Statement from European Network for Drug Allergy concerning Allergopen withdrawal. Allergy 2006;61:910-1. Andrew Williams 14.02.2012