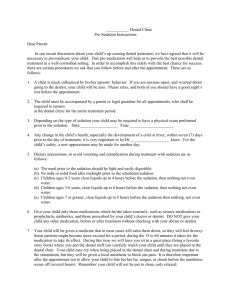
oral diagnosis
advertisement

Oral Surgery Oral Diagnosis 11 (1998) Vol 11: 1-368 ORAL SURGERY ORAL DIAGNOSIS Published by Osfix Research Centre in co-operation with FREO r.y. and the Institute of Oral and Maxillo-Facial Surgery, University of Kuopio, Finland MONITORED INTRAVENOUS SEDATION WITH LOCAL ANAESTHESIA FOR DENTAL OUTPATIENTS. Clinical Observations by Kari Luotio, DDS Eight studies and clinical guidelines AUTHOR’S ADDRESS: OSFIX OY/LTD P.O.BOX 14, FIN-47200 ELIMÄKI OSFIX@SCI.FI Elimäki 1998 To Kirsti, Johanna, Eero, Lauri and Juha without whom this book would have been accomplished many years earlier. Life is based on rhythms. From the basic rhythm of the earth around the sun to the complex rhythms of music. Thus we are living in the middle of an endless interplay of countless rhythms. This book is inspired by the continuos rhythm of the monitored heart . 5 Monitored intravenous sedation with local anaesthesia for dental outpatients CONTENTS FOREWORD .......................................................................................................................... 14 PREFACE ............................................................................................................................... 17 ACKNOWLEDGEMENTS..................................................................................................... 19 ABBREVIATIONS ................................................................................................................. 21 PART I: 1 GENERAL INTRODUCTION AND REVIEW OF THE LITERATURE .................. .23 1.1 GENERAL DESCRIPTION OF THE STUDY ................................................... 25 1.2 ABSTRACT......................................................................................................... 27 1.2.1 Part II (Monitoring...): .......................................................................... 27 1.2.2 Part III (Experiences...): ...................................................................... 28 1.2.3 Part IV (Challenges): ........................................................................... 29 1.3 INTRODUCTION TO OXYGEN DELIVERY SYSTEM .................................. 31 1.4 THE STATE OF ART IN THE BEGINNING THE WORK IN THE YEARS 1992-1993: REVIEW OF THE LITERATURE................. .................................................... 35 1.4.1 SEDATION WITH LOCAL ANAESTHESIA OR GENERAL ANAESTHESIA? ........................................................................................... 35 1.4.1.1 Midazolam ............................................................................ 35 1.4.1.2 Midazolam compared to diazepam ....................................... 35 1.4.2 PATIENT MANAGEMENT WITH INTRAVENOUS SEDATION ... 36 1.4.2.1 Dentist’s sight ....................................................................... 36 1.4.2.2 Patient’s opinion ................................................................... 36 1.4.2.3 Antagonist to benzodiazepines.............................................. 36 1.4.3 BENZODIAZEPINES COMBINED WITH OPIATES ...................... 38 1.4.3.1 Healthy patients .................................................................... 38 1.4.3.2 Medically compromised patients .......................................... 38 1.4.4 THE COMPARISON OF ORAL AND INTRAVENOUS ADMINISTRATION ............................................................................................ 40 1.4.5 THE NECESSITY OF OXIMETRY DURING INTRAVENOUS SEDATION ....................................................................... 41 1.4.5.1 Hypoxia................................................................................. 41 1.4.5.2 Pulse oximetry ...................................................................... 41 1.4.6 SEVERE COMPLICATIONS DURING PROCEDURE ..................... 44 1.4.6.1 Psychological complications ................................................. 44 1.4.6.2 Other complications .............................................................. 44 7 Contents 1.5 AIMS OF THE STUDY ...................................................................................... 46 1.5.1 MORE DETAILED DESCRIPTION OF THE BACKGROUNDS AND AIMS OF THE SEPARATE STUDIES ............................................... 48 1.5.1.1 Part II (Monitoring...) ........................................................... 48 1.5.1.2 Part III (Experiences...) ......................................................... 48 1.5.1.3 Part IV (Challenges) ............................................................. 49 1.6 PATIENTS AND METHODS ............................................................................. 50 1.6.1 STUDY DESIGN ................................................................................. 50 1.6.1.1 Patients.................................................................................. 51 1.6.1.1.1 Patients in Part II (Monitoring...) .......................... 51 1.6.1.1.2 Patients in Part III (Experiences...) ........................ 51 1.6.1.1.3 Patients in Part IV (Challenges) ............................ 52 1.6.2 PRE- AND POSTOPERATIVE PATIENT PREPARATION ............. 54 1.6.3 MEDICATION ..................................................................................... 56 1.6.3.1 Medication in Part II (Monitoring...) .................................... 56 1.6.3.1.1 Sedation ................................................................. 56 1.6.3.1.2 Local anaesthesia ................................................... 56 1.6.3.2 Medication in Part III (Experiences...) .................................. 57 1.6.3.3 Medication in Part IV (Challenges) ...................................... 57 1.6.4 MONITORING AND DATA REVIEW............................................... 58 1.6.5 THE WORKING PRINCIPLE OF THE PULSE OXIMETRIC EQUIPMENT................................................................................................. 59 1.6.5.1 Different equipment philosophies ......................................... 59 PART II: MONITORING PATIENTS WITH THREE PULSE OXIMETER EQUIPMENTS ...................................................................................................................... 61 2.1 SURVEY 1: DETECTION OF OXYGEN SATURATION UNDER INTRAVENOUS SEDATION WITH OHMEDA PULSE OXIMETER AND REGISTRATION OF OTHER CARDIOVASCULAR PARAMETERS ............ 63 2.1.1 ABSTRACT ......................................................................................... 63 2.1.2 INTRODUCTION ................................................................................ 64 2.1.3 PATIENTS AND METHODS ............................................................. 66 2.1.3.1 Study design .......................................................................... 66 2.1.3.2 Patients.................................................................................. 66 2.1.3.3 Sedation ................................................................................ 67 2.1.3.4 Monitoring and data review .................................................. 68 2.1.3.5 Statistical methods ................................................................ 69 2.1.4 RESULTS ............................................................................................ 70 2.1.4.1 Oxygen saturation of blood .................................................. 70 2.1.4.2 Other remarks........................................................................ 70 2.1.5 DISCUSSION ...................................................................................... 73 2.1.5.1 Desaturation .......................................................................... 73 2.1.5.2 Monitoring ............................................................................ 74 2.1.6 CLINICAL CONCLUSION ................................................................. 77 8 Monitored intravenous sedation with local anaesthesia for dental outpatients 2.2 SURVEY 2: DETECTION OF CARDIOVASCULAR RESPONSES TO LOCAL ANAESTHESIA WITH A DATEX CARDIOCAP MULTIPARAMETER MONITOR ........................................................................ 79 2.2.1 ABSTRACT ......................................................................................... 79 2.2.2 INTRODUCTION ................................................................................ 79 2.2.3 PATIENTS AND METHODS ............................................................. 82 2.2.3.1 Study design .......................................................................... 82 2.2.3.2 Subjects ................................................................................. 82 2.2.3.3 Local anaesthesia .................................................................. 82 2.2.3.4 Timing of the procedure ........................................................ 83 2.2.3.5 Monitoring ............................................................................ 85 2.2.3.6 Statistical methods ............................................................... 85 2.2.4 RESULTS ............................................................................................ 87 2.2.4.1 Pulse .................................................................................... 87 2.2.4.2 Amplitude of pulse wave ..................................................... 87 2.2.4.3 Blood pressure ..................................................................... 88 2.2.4.4 Oxygen saturation of blood (SaO2) ..................................... 88 2.2.5 DISCUSSION ...................................................................................... 93 2.2.5.1 Amplitude of pulse wave and the measuring equipment ....... 93 2.2.5.2 Oxygen saturation of blood during dental treatment ............ 93 2.2.5.3 Toxic reactions ...................................................................... 94 2.2.5.4 Pulse and blood pressure after local anaesthesia ................... 94 2.2.6 CLINICAL CONCLUSIONS ............................................................... 97 2.3 SURVEY 3: DETECTION OF MAXIMAL PULSE AND PERIPHERAL BLOOD FLOW UNDER INTRAVENOUS SEDATION WITH A DATEX SATTLITE TRANS PULSE OXIMETER ............................................................. 99 2.3.1 ABSTRACT ......................................................................................... 99 2.3.2 INTRODUCTION .............................................................................. 100 2.3.2 1 Monitored sedation ............................................................. 100 2.3.2.2 Local anaesthesia ................................................................ 100 2.3.2.3 Amplitude of pulse wave (A.P.W.) ..................................... 101 2.3.2.4 Aim of the study.................................................................. 101 2.3.3 PATIENTS AND METHODS ........................................................... 102 2.3.3.1 Study design ........................................................................ 102 2.3.3.2 Monitoring .......................................................................... 102 2.3.3.3 The working principle of the pulse oximetric equipment .... 102 2.3.3.4 Patients................................................................................ 103 2.3.3.5 Sedation .............................................................................. 103 2.3.3.6 Statistical methods .............................................................. 104 2.3.4 RESULTS .......................................................................................... 106 2.3.4.1 Maximal pulse rate .............................................................. 106 2.3.4.2 Amplitude of pulse wave (A.P.W.) .................................... 106 2.3.4.3 Other observations .............................................................. 107 2.3.5 DISCUSSION .................................................................................... 114 2.3.5.1 False alarms ........................................................................ 114 2.3.5.2 Reactions to local anaesthesia ............................................. 114 2.3.5.3 Clinical monitoring ............................................................. 115 2.3.6 CLINICAL CONCLUSIONS ............................................................. 117 9 Contents PART III: PATIENTS’ EXPERIENCES DURING AND AFTER SURGERY UNDER INTRAVENOUS SEDATION ............................................................................................ 119 3.1 STUDY 4: PEROPERATIVE EXPERIENCES ........................................... 121 3.1.1 INTRODUCTION .............................................................................. 122 3.1.1.1 Fear ..................................................................................... 122 3.1.1.2 Sedation ............................................................................. 122 3.1.1.3 Aims of the study ................................................................ 124 3.1.2 PATIENTS AND METHODS ........................................................... 125 3.1.2.1 Patients................................................................................ 125 3.1.2.2 Questionnaire ...................................................................... 127 3.1.2.3 Medication .......................................................................... 128 3.1.2.4 Statistical methods .............................................................. 130 3.1.3 RESULTS .......................................................................................... 131 3.1.3.1 All patients (n=108) ............................................................ 131 3.1.3.2 Phobia group (n=53) ........................................................... 131 3.1.3.3 Operation group (n=38) ...................................................... 132 3.1.3.4 Differences .......................................................................... 132 3.2 STUDY 5: POSTOPERATIVE EXPERIENCES ......................................... 141 3.2.1 INTRODUCTION .............................................................................. 141 3.2.1.1 Postoperative recovery ........................................................ 141 3.2.1.2 Aim of the study.................................................................. 142 3.2.2 PATIENTS AND METHODS ........................................................... 143 3.2.2.1 Statistical methods .............................................................. 143 3.2.3 RESULTS .......................................................................................... 144 3.2.3.1 All patients (n=108) ............................................................ 144 3.2.3.2 Phobia group (n=53) ........................................................... 145 3.2.3.3 Operation group (n=37) ...................................................... 146 3.2.3.4 Differences ............................................................... 147 3.3 GENERAL DISCUSSION OF PART III ....................................................... 155 3.3.1 The anxious patient ................................................................. 155 3.3.2 Amnesia .................................................................................. 156 3.3.3 Sedation and confusion ........................................................... 156 3.3.4 Postoperative pain ................................................................... 157 3.4 CLINICAL CONCLUSIONS ......................................................................... 160 10 Monitored intravenous sedation with local anaesthesia for dental outpatients PART IV: CHALLENGES ................................................................................................................... 163 4.1 SURVEY 6: ADVANCED MONITORING: HOLTER ECG AND ANALYSIS OF THE STATUS OF THE AUTONOMIC NERVOUS SYSTEM ............................................................................................. 165 4.1.1 ABSTRACT ....................................................................................... 165 4.1.2 INTRODUCTION .............................................................................. 165 4.1.2.1 Autonomic nervous system and fear ................................... 165 4.1.2.2 Aim of the study.................................................................. 167 4.1.3 PATIENTS AND METHODS ........................................................... 168 4.1.3.1 Patient: preparation, sedation and local anaesthesia ........... 168 4.1.3.1.1 1. Study group: ................................................... 168 4.1.3.1.2 2. Reference group............................................... 169 4.1.3.2 Monitoring .......................................................................... 170 4.1.3.3 Statistical methods .............................................................. 171 4.1.4 RESULTS .......................................................................................... 172 4.1.5 DISCUSSION .................................................................................... 180 4.1.5.1 Cardiac occurrences ............................................................ 180 4.1.5.2 Pulse ................................................................................... 180 4.1.5.3 Heart rate variability ........................................................... 181 4.1.6 CLINICAL CONCLUSIONS ............................................................. 183 4.2 STUDY 7: STRESS INDEX ........................................................................... 185 4.2.1 ABSTRACT ....................................................................................... 185 4.2.2 INTRODUCTION .............................................................................. 185 4.2.3 PATIENTS AND METHODS ........................................................... 187 4.2.3.1 Study design........................................................................ 187 4.2.3.2 Monitoring .......................................................................... 187 4.2.3.3 Patients................................................................................ 188 4.2.3.4 Sedation .............................................................................. 189 4.2.3.5 Local anaesthesia ................................................................ 189 4.2.3.6 Timing of the procedure ...................................................... 190 4.2.3.7 Statistical methods .............................................................. 190 4.2.4 OBSERVATIONS.............................................................................. 192 4.2.5 DISCUSSION .................................................................................... 200 4.2.5.1 Stress during treatment ....................................................... 200 4.2.5.2 Amplitude of pulse wave (A.P.W.) ..................................... 200 4.2.5.3 Amplitude of pulse wave and the measuring equipment ..... 201 4.2.5.4 Stress index ......................................................................... 202 4.2.6 CLINICAL CONCLUSIONS ............................................................. 205 11 Contents 4.3 STUDY 8: COMPLICATED CASES............................................................ 207 4.3.1 ABSTRACT ....................................................................................... 207 4.3.2 INTRODUCTION .............................................................................. 208 4.3.3 PATIENT MANAGEMENT AND METHODS ................................ 209 4.3.4 OBSERVATIONS.............................................................................. 210 4.3.4.1 CASE 1. FIG. 1 ................................................................... 210 4.3.4.2 CASE 2. FIG. 2 ................................................................... 211 4.3.4.3 CASE 3. FIG. 3 ................................................................... 212 4.3.4.4 CASE 4. FIG. 4 ................................................................... 213 4.3.4.5 CASE 5. FIG. 5 ................................................................... 214 4.3.5 DISCUSSION .................................................................................... 218 4.3.5.1 Respiratory problems and oxygen ....................................... 218 4.3.5.2 Antidote for correction of hypoxia ...................................... 219 4.3.5.3 Wrong detection of hypoxia ................................................ 219 4.3.6 CLINICAL CONCLUSION ............................................................... 223 PART V: 5 GENERAL DISCUSSION AND CONCLUSIONS ...................................................... 227 5.1 DETECTION OF ADVERSE REACTIONS .................................................... 227 5.2 EFFECTS OF LOCAL ANAESTHETIC PREPARATIONS ........................... 228 5.3 THE USE OF TWO LOCAL ANAESTHETIC PREPARATIONS IN COMBINATION .......................................................................................... 229 5.4 EFFECTS OF BENZODIAZEPINES VS. LOCAL ANAESTHETICS ............ 229 5.5 PATIENTS' REACTIONS TO TREATMENT UNDER INTRAVENOUS SEDATION WITH LOCAL ANAESTHESIA .................................................. 230 5.6 THE PATIENT’S CONDITION AFTER TREATMENT UNDER INTRAVENOUS SEDATION WITH LOCAL ANAESTHESIA. .................... 231 5.7 ARRHYTHMIAS AND THE STATUS OF AUTONOMIC NERVOUS SYSTEM ........................................................................................ 231 5.8 FALSE ALARMS IN PULSE OXIMETRY ..................................................... 232 5.9 COMPLICATED CASES ................................................................................. 233 5.10 STATISTICAL VIEW VS. CLINICAL VIEW ............................................... 234 5.11 CONCLUSIONS ............................................................................................. 235 PART VI: 6 CLINICAL GUIDELINES .............................................................................................. 237 INTRAVENOUS SEDATION PROTOCOL............................................................ 239 6.1 Introduction ....................................................................................................... 243 6.2 The Patient for Sedation .................................................................................... 245 6.2.1 Examining the Patient ........................................................................ 245 6.2.2 Clinical Anatomy ............................................................................... 245 6.3 Benzodiazepines ................................................................................................ 247 6.3.1 Operating mechanism ......................................................................... 247 6.3.2 Half-life .............................................................................................. 247 6.3.3 Pharmacodynamics ............................................................................. 248 6.3.4 Pharmacokinetic anomalies ................................................................ 248 6.4 The Commercial Drugs ...................................................................................... 249 6.4.1 Selecting a suitable drug..................................................................... 249 6.4.2 Diazepam ............................................................................................ 249 6.4.3 Midazolam .......................................................................................... 250 6.4.4 Administration equipment .................................................................. 251 6.4.5 First aid equipment ............................................................................. 252 12 Monitored intravenous sedation with local anaesthesia for dental outpatients 6.5 Monitoring the Patient ....................................................................................... 254 6.5.1 Blood pressure monitors ..................................................................... 254 6.5.2 Pulse oximetry .................................................................................... 254 6.5.2.1 The monitoring principle and equipment ........................................ 255 6.5.2.2 Monitoring during sedation ............................................................. 256 6.5.2.3 Emergency situation ....................................................................... 256 6.5.2.4 Sources for defaults ......................................................................... 257 6.5.3 Pulse wave oximetry........................................................................... 257 6.6 Intravenous Sedation in Practice ........................................................................ 259 6.6.1 Cannulating the vein in the crook of the arm ..................................... 259 6.6.2 Administering the drug and observing the effects .............................. 260 6.6.3 Recovery from sedation ...................................................................... 261 6.6.3.1 Oxygen saturation............................................................................ 261 6.6.3.2 Flumazenil ....................................................................................... 261 6.7 Complications ..................................................................................................... 264 6.7.1 Local complications ........................................................................... 264 6.7.2 Hypoxia .............................................................................................. 264 6.7.3 Fainting .............................................................................................. 265 6.7.4 Psychogenic complications ................................................................ 265 6.7.5 Other complications ........................................................................... 265 6.8 Legal aspects ...................................................................................................... 267 6.9 Conclusions ....................................................................................................... 268 6.10 Instructions to patients ..................................................................................... 269 1.11 Pictures ............................................................................................................ 270 7 APPENDICES 7.1 APPENDIX I DESCRIPTION OF THE DRUGS USED AND STUDIED ..................................... 283 7.2 APPENDIX II QUESTIONS AND PATIENTS’ COMMENTS FOR STUDIES 4 AND 5 ............. 309 7.3 APPENDIX III PLETYSTOMOGRAFIC PULSE WAVE ............................................................... 331 7.4 APPENDIX IV COMMUNICATION BETWEEN PC AND OXIMETER ...................................... 353 7.4 APPENDIX V CRITICAL THOUGHTS .......................................................................................... 361 REFERENCES...................................................................................................................... 369 13 FOREWORD In dental practice, monitors are still used extremely seldom although technical possibilities already exist. In fact there is an abundance of equipment. Fatal complications in a dental chair are so uncommon that the use of monitors cannot be mandatory. But it is certain that some dangerous episodes and threatening situations nevertheless occur. It is not so much a question of "life or death" but of the quality of care in general. Many of the principles of monitoring accepted in anaesthesia for general surgery can also be applied in dental operative care. Patient monitoring is used in order to detect dangerous deviations from normal in circulation and respiration. These complications can be due to therapeutic procedures or the medication used, but they can result as a deterioration of the patient’s own organic disease. It should be extremely important to recognise these occurrences in due time, to be able to make the right conclusions to begin the correct therapeutic manoeuvres. On the basis of these observations and conclusions, the surgeon is also able to adequately inform the patient on the occurrence. Without appropriate monitoring these goals cannot be reached with certainty. 14 Monitored intravenous sedation with local anaesthesia for dental outpatients Some patients may have such a fear for dental procedures that they need to be sedated. This study describes treatment models which have been widely accepted and reported during the last decade, but North European tradition has preferred psychological methods, nitrous oxide inhalation sedation and general anaesthesia to the intravenous sedation with local anaesthesia. However, intravenous sedation with local anaesthesia is a pleasant, efficient and safe means to treat anxiety problems both for the dentist and his patient. To reach an adequate and accurate effect, these drugs have to be administered to the vein but not at the level of general anaesthesia. The patient always remains conscious. Even intravenous sedation includes risks which must imperatively be recognised, and due precautions must be made for treating eventual complications. The basis for a secure intravenous sedation is the appropriate skills of the staff. 15 Monitored intravenous sedation with local anaesthesia for dental outpatients PREFACE The present series of eight independent studies divided into three chapters in this publication describes methods of intravenous sedation, monitoring, and the experiences of the patients. These are follow-ups with modern equipment, and the studies are descriptive reconstructions of the treatments. Each study contains a short independent introduction, review of literature, description of material, aims, observations, analyses and a discussion of the results. The first two studies and survey 6 are more statistical and analytical than descriptive. Studies 3, 7, 8, the review of the literature in part I and the appendices are written from a viewpoint of a clinician and they are mainly descriptive. Studies 4 and 5 display a double structure: a clinical descriptive view and a statistical view. Moreover, the opinions expressed are the authors’ own/personal opinions. Part II consists of two studies which are descriptive reviews of patient records during sedation, and one study which is an on-line recording of cardiovascular parameters during local anaesthesia. There were many differences in patient preparation, cannulation and intravenous infusion, sedative drugs and local anaesthesia i.e. in the underlying factors. It is important to understand that these studies were not controlled clinical experiments but clinical follow-ups of normal treatment or local anaesthesia periods. Therefore there were no reference groups in two of these works, and findings were compared with the literature. Part III describes the patients’ experiences: An anonymous questionnaire was mailed to patients previously treated with intravenous sedation with local anaesthesia at the author’s private practice. This chapter is further divided into two parts: per- and postoperative findings i.e. memories. Part IV describes some challenges and applications which arose from earlier studies. There are more sophisticated methods of monitoring, such as the Holter ECG, and a new index for stress as well as a description of difficulties in treatment, such as complications. The whole work is mainly descriptive because the statistics of real life treatments are quite complex as the material used originated from the dentist’s practical work and not a statistically perfect sample. Part V is the vertebrae of the book: It gives clinical quidelines for sedation. These quidelines are based both on authors’ clinical experience and on the studies in parts II-IV: The use of monitoring, and sedation methods, have been clinically applied in dentistry and oral surgery, methods which are widely used in anaesthesiology and critical care: the main concern is always patient safety. The topic of this book is quite unknown to dentists, then again clinicians and scientists have quite different needs. Thus the book itself can be read in three ways: 1) browsing bold prints, abstracts and clinical conclusions; 2) reading only the parts interesting for the reader, e.g. the patients’ experiences; 3) thoroughly going into the whole works. Moreover, there is quite a few various appendices at the end of this book but I am positive that their presence is justified as I hope that this book will live long as a brief introduction for intravenous sedation practice. 17 Monitored intravenous sedation with local anaesthesia for dental outpatients ACKNOWLEDGEMENTS This study is carried out primarily at the author’s private practice in Elimäki, and secondly in the department of Oral and Maxillofacial Surgery, University of Kuopio, during the years 1992-1997. I would like to thank Oral Surgeon, Associate Professor Risto Kotilainen and Anaesthesiologist, Docent Matti Mattila for supervising this study. Anaesthesiologists, Professor Matti Salo and Docent Kari Korttila has given me remarkable comments during finalishing this book. It would not have been possible to complete this work without their professional advice and guidance through the whole study. Moreover, I wish to thank Doctor Tomi Laitinen and Professor Esko Länsimies for co-operation and advice in a study dealing with the Holter ECG. I express my gratitude to my research group in the department of Oral and Maxillofacial Surgery: Janne Ryhänen, Outi Hyyppä, Sinikka Navari, Tapani Hyppönen, Marika Vainio and Hannu Vesanen. They all have helped me with reviewing the literature and performing parts of these studies with me. When we began, they were all candidates but during these years they have professionally graduated. I thank Tiina Vuori, translator for the revision of English, and Tuija Poussa, MSc for the revision and further analysis of statistical methods. Moreover, I thank Irja Virolainen for helping with the layout. I am very grateful to doctors Osmo Hiltunen, Hannu Kokki and Matti Mattila for helping me with the first Finnish intravenous sedation course in summer 1996. Special thanks goes to my oldest son Juha who has helped me so many times with computers and developed the communication program between PC and pulse oximeter for me. Last but not least, my gratitude goes to my whole family: my wife Kirsti, my sons Juha, Lauri, Eero and my daughter Johanna for their irreplaceable support. 19 Monitored intravenous sedation with local anaesthesia for dental outpatients ABBREVIATIONS SaO2 BP APW ECG HRV VAS Blood oxygen saturation Blood pressure Amplitude of pulse wave Electrocardiogram Heart rate variability Visual analogy scale 21 Monitored intravenous sedation with local anaesthesia for dental outpatients Part I PART I GENERAL INTRODUCTION AND REVIEW OF THE LITERATURE 23 Monitored intravenous sedation with local anaesthesia for dental outpatients Part I 1.1 GENERAL DESCRIPTION OF THE STUDY Our knowledge of patients’ cardiovascular and pulmonar parameters in dental chair, in real-life conditions, is still limited. It is most important that the therapy as well as premedication do not harm the patient. Thus this study was performed and specially focused on the cardiovascular and pulmonar parameters before, during and after sedation and on the methods observing them. -Main observations were: Low oxygen saturation before sedation constitutes a risk for oxygen desaturation during sedation. Pulse oximetric monitoring allows early intervention in ventilation problems. No cardiovascular problems were found when the two most commonly used local anaesthesia were used in combination. There was little need for general anaesthesia. Most patients preferred intravenous sedation. Amplitude of pulse wave was the most responsive but only descriptive measurable single parameter indicating stress. The amount of cardiac occurences were within normal limits during sedation. The maximum pulse of sedated patients was suggestively lower and the high and low frequency components of heart rate variability were higher indicating stress relief. To estimate the value of generic stress a new index was developed, which is called the stress index. 25 Monitored intravenous sedation with local anaesthesia for dental outpatients Part I 1.2 ABSTRACT saturation were found (SaO2 under 90 %), and all problems related to sedation were resolved by administering supplementary oxygen or a benzodiazepine antagonist. Blood pressure and pulse rate were slightly lower after treatment than before it (mean change in systolic blood pressure. -6.9 % units - p=0.04). Pulse oximetric monitoring was found extremely sensitive as a predictor for desaturation and it also allows early intervention in ventilation problems. 1.2.1 Part II (Monitoring...) In the first study part of the patients were monitored with three pulse oximeter equipment: oxygen saturation was detected with Ohmeda pulse oximeter, cardiovascular responses to the local anaesthesia with Datex Cardiocap multiparameter monitor and Amplitude of pulse wave with Datex Sattlite Trans pulse oximeter. In the first study of this part, 41 patients were monitored with a pulse oximeter, and blood pressure values were measured during major or protracted dental operations under intravenous sedation with local anaesthesia. The most important finding was that there seems to be a risk that low oxygen saturation (SaO2 < 90%) before sedation constitutes a risk for oxygen desaturation during sedation. Before beginning the procedure, the oxygen saturation level (SaO2) was found to be 98%. The lowest SaO2 levels were found a few minutes after injection or later during the treatment when the average level was 92 % (p<0.0001). The patients who had preoperative SaO2 over 98% declined to a minimum saturation at the average level of 94%. The patients with the initial saturation under 98% showed signs of measurable desaturation mean level 88%. However, desaturation did not correlate with the dose of the sedative agent when this was used at the therapeutic level. Only five cases of low arterial oxygen In the second study the cardiovascular effects of the two local anaesthetic agents (lidocaine and prilocaine) and two vasoconstrictors (epinephrine and phelypressine) were observed. There were no radical changes of systolic or diastolic blood pressure. The mean blood oxygen saturation values were within normal limits and the displayed SaO2 values were between 96 - 98 percent during the measuring period in 96 percent of detected values. Heart rate slightly decreased after the injection of prilocaine - phelypressine, but pulse rate increased after the epinephrinecontaining lidocaine injection. Both the prilocaine and lidocaine injections resulted in statistically significant (p=0.001) changes in heart rate. Amplitude of pulse wave was the most responsive measurable parameter. Amplitude of pulse wave diminished just before and during the injection as a result of psychological 27 General introduction and review of the literature stress. Blood flow showed the smallest values during the injection of local anaesthetic. No cardiovascular problems were found when the two most commonly used local anaesthesia preparations (epinephrine-containing lidocaine and phelypressine-containing prilocaine) were used in combination. Consequently, if the effect of one local anaesthesia preparation is not sufficient it is possible to increase the effect by adding the other preparation. the injection due to psychological stress. The blood flow showed decreasing values during and after the injections of local anaesthetic. Moreover, poor A.P.W. caused measuring artefacts into the levels of blood oxygen saturation, which can be avoided by covering the patients with a blanket. The nature of this descriptive parameter is discussed. 1.2.2 Part III (Experiences...) In study 4 of this part, 108 patients who had experienced major or protracted dental operations under intravenous sedation with local anaesthesia were asked questions concerning their experiences of the treatment using an anonymous questionnaire, and the findings are divided into two chapters according to their occurrence in time, i.e. peroperative and postoperative periods. Two clear subgroups were formed (by excluding 17 patients) according to indication for treatment: for 38 patients the main reason for undergoing intravenous sedation with local anaesthesia was a major surgical treatment (operation group), and for 53 patients the fear of any dental treatment, i.e. dental care phobia (phobia group). The operation group served as a reference group. In the third study of this part, 26 patients were monitored with pulse oximeter during major or longstanding dental operation under intravenous sedation with local anaesthesia. The cardiovascular effects of benzodiazepine (midazolam) and the local anaesthetic agent (lidocaine) and vasoconstrictor (epinephrine) were observed. Maximal pulse rate increased both during and after the injection of midazolam as well as the injection of epinephrine containing lidocaine. The increase was very slight after midazolam but notable after local anaesthesia. As a result of stress relief, pulse rate was lower after treatment than before it (p<0.05). The highest level of pulse level was recorded during local anaesthesia (p<0.005). There was no significant difference in pulse rate before treatment and during sedation. During our retrospective review of patient records, amplitude of pulse wave (A.P.W.) was the most responsive but only descriptive measurable single parameter indicating stress. In general, A.P.W. decreased towards Peroperatively the most important finding was that the patients later felt there was little need for general anaesthesia. Most patients (87%) preferred intravenous sedation with local anaesthesia. The patients were nearly unanimous in recommending intravenous sedation with local 28 Monitored intravenous sedation with local anaesthesia for dental outpatients Part I anaesthesia for others. These subgroups showed no statistical difference in unpleasant experiences during treatment, though the operation group was slightly more satisfied with the intravenous sedation with local anaesthesia than the phobia group (p= 0.05). Eight patients in the phobia group felt that they could undergo the procedure with local anaesthesia alone the next time, while only 1 patient in the operation group preferred the procedure with local anaesthesia alone. The need for general anaesthesia was low, the patients (5 cases) reporting the need for general anaesthesia belonging to the phobia group. The patients in both groups reported that pain, fear, anxiety, confusion and drowsiness had not disturbed them during the treatment. on the next day. The patients felt healthy after intravenous sedation with local anaesthesia and the feeling increased during the following days (p=0.0001). Patients felt confusion for approximately three hours, and most patients felt ready for daily work the next morning. However, sedative premedication increases the need of sleep and the patients need more rest than normally on the first day after treatment. 1.2.3 Part IV (Challenges) This part again consists of three chapters. The first describes advanced monitoring: Holter ECG and the analysis of the status of the autonomic nervous system. The second chapter introduces a new stress index, and the last chapter some complicated cases. Survey 6 comprises 23 study group patients undergoing dental procedure under intravenous sedation, and 12 control registrations of the University Clinic outpatients who underwent dental surgical operations without intravenous sedation. Patients were monitored with a Holter ECG recorder until next morning. The tapes were reviewed with an arrhythmia analysis program allowing the detection of normal sinus beats and supraventricular and ventricular extrasystoles. The heart rate variability analysis (HRV) was performed both during and after surgery. The amount of cardiac occurences were within normal limits in both groups; the maximum pulse was suggestively lower in the study Postoperatively (study 5), pain was the primary symptom after treatment under intravenous sedation with local anaesthesia. Patients reported that the pain was not a result of sedation with local anaesthesia but a result of the operation itself. The incidence of confusion and tiredness reduced after the first night. The possibilities to avoid pain and confusion are discussed. Some other disorders were detected but they were rare: headache and nausea but no vomiting. Subgroups showed statistically significant differences with the incidence of confusion immediately after the treatment. The phobia group felt more confused than the operation (control) group (p=0.05). No statistical difference appeared in unpleasant experiences 29 General introduction and review of the literature group and the high and low frequency components of heart rate variability were systematically and, in recovery stage, even statistically higher (p=0.05) in the study group, all indicating stress relief. which is called the stress index. When a subject suffers from generic stress, we can measure the most significant cardiovascular changes, such as a rising pulse rate and a diminishing amplitude of pulse wave. By dividing the pulse rate by the amplitude of pulse wave (pulse / blood flow) we get a sensitive indicator for stress, or the stress index. Study 7 is a combination of parts of two previous studies: survey 2 and survey 6, both describing amplitude of pulse wave. This study describes cardiovascular parameters indicating stress during treatment under intravenous sedation, and local anaesthetic alone. Moreover, two local anaesthetic agents (lidocaine and prilocaine) and two vasoconstrictors (epinephrine and phelypressine) were observed. Amplitude of pulse wave was the most responsive measurable parameter. Amplitude of pulse wave diminished just before and during the injection as a result of vasoconstriction due to psychological stress. Blood flow showed the smallest values during the injection of local anaesthetic. Similarly, heart rate slightly decreased after the injection of prilocaine and phelypressine, but pulse rate increased after the epinephrine-containing lidocaine injection. Controversially, both parameters increased after the injection of sedative agent: pulse rate only slightly but amplitude of pulse wave showed a remarkable increase. To estimate the value of generic stress a new index was developed, The last study (8) describes cases where remarkable and long-standing hypoxia were detected with pulse oximeter during intravenous sedation. Diazepam with soybean oily solvent, midazolam and in some cases fentanyl were used as intravenous sedative agents in these cases. The first signs of hypoxia were seen through pulse oximetry. External oxygen was added for all of these patients during the dental treatment period to avoid more complications as a result of hypoxia. Attempts were made to solve the problems related to hypoxia by administering supplementary oxygen, benzodiazepine antagonist, and ventilation. Some of the patients needed further follow-up but none of these patients developed any additional complications. The lowest SaO2 levels of these patients were found during the postoperative period and the role of poor amplitude of pulse wave in these cases is discussed. 30 Monitored intravenous sedation with local anaesthesia for dental outpatients Part I 1.3 INTRODUCTION TO OXYGEN DELIVERY SYSTEM The oxygen delivery system must provide oxygen at adequate rates to all body tissues to support their oxygen consumption for survival. In large animals, two physical constraints to transport have been solved physiologically. First, the rate of gas diffusion in liquids is extremely slow. It takes hours for oxygen to diffuse through a centimeter of water. Even though animals have increased dramatically in size from single celled to large mammals, the diffusion distance from the oxygen source to the mitochondrion has not much increased. The vast microvascular circulatory system has solved the diffusion problem by supplying an oxygen tension source near all cells. The tissue capillary density is roughly matched to the metabolic oxygen demands of the tissues. The second physical problem is that oxygen is relatively insoluble in water, the medium of cellular life. The haemoglobin molecule has effectively increased the blood's oxygen solubility by reversibly binding oxygen. The addition of haemoglobin to the water-based oxygen transport fluid (blood) increases the carried oxygen approximately 60-fold. Oxygen is taken up by blood in the lungs, transported by blood to all organs and tissues, and within microcirculation released by blood into tissues. The driving force behind oxygen uptake as well as oxygen release is the partial pressure difference of oxygen; in other words, oxygen diffuses from alveolar space into blood and from blood into tissue. In addition to this necessary transport by diffusion, oxygen is transported by convection from the lungs to the organs. The amount of oxygen transported to all organs is called oxygen supply and it is determined by the product of cardiac output and the arterial oxygen concentration. 31 General introduction and review of the literature The principal aim of monitoring during procedures is patient safety. Oxygen is the most acutely necessary substrate of aerobic life. Oxygen saturation is life-maintaining and pulse oximetry is therefore obligatory when a patient has a treatment under intravenous sedation. 120 100 % Hb SATURATION 80 60 40 20 0 0 32 20 40 60 80 PaO2 mmHg 100 Monitored intravenous sedation with local anaesthesia for dental outpatients Part I Any change in arterial tension, arterial saturation, the oxygen binding curve and the oxygen binding power of Hb, haemoglobin concentration or the physically dissolved oxygen leads to an alteration in the oxygen content of blood. As a consequence of a disturbance in lung function, hypoxaemia may be produced by a decrease in oxygen tension. In such circumstances all values, namely tension or partial pressure (PaO2), saturation (SaO2) and content or concentration (CoO2), are decreased. This is hypoxic hypoxaemia. Carbon monoxide poisoning or methaemoglobin formation decreases two variables, SaO2 and CoO2 where the PaO2 remains normal and results in toxaemic hypoxaemia. Anaemia hypoxaemia with a decrease in the haemoglobin concentration (anaemia) lowers CoO2 only while PaO2 and SaO2 remain normal. Thus, the necessary terms to understand are: blood flow and electrocardiogram), they are only useful devices and can never replace human senses, observation skills and the measured value of blood oxygen saturation. Intravenous sedation has proved helpful in avoiding cardiovascular reactions during oral surgical operations, but there is a risk of provoking respiratory depression. This adverse effect can easily be detected at an early stage, where the pulse wave and / or a drop in saturation is signalled visually with pulse oximeter and can be corrected by administering supplementary oxygen. Monitors as well as intravenous sedation are still very seldom used in dental practice in North Europe despite their low cost. Fatal complications in the dental chair are so uncommon that the use of monitors is not obligatory, and is not recommended by the Finnish authorities. This is in contrast to the situation in United States, Japan, Canada and many other parts of the world. There the monitors are in widespread use for conscious intravenous sedation; in fact, they are mandated by laws and practice standard. Our tradition relies on the high education level of the medical and dental surgeons, and no precise rules exist. The amount of haemoglobin in blood (depends on individual variation) Oxygen tension (partial pressure) in blood (depends on atmospheric pressure and oxygen concentration in atmosphere) Oxygen saturation of blood (depends on the dissociation curve. See figure on next page) Oxygen concentration in blood (depends on haemoglobin and oxygen tension) The selection of a correct monitor must originate from essential needs in each particular situation and circumstances. On the basis of experiences from surgical anaesthesia there are some clear priorities among monitored parameters and these Although this book introduces some other methods and parameters to monitor (e.g. blood pressure, pulse, 33 General introduction and review of the literature experiences can easily be applied also to dental practice. The use of monitors must rise from risk analysis. They should be used in situations which include the most concrete dangers. The selection of monitored parameters should lead to conclusions on how dangers could be surely detected. When we monitor a patient who is having a treatment under intravenous sedation, the most important factor to monitor is the amount of oxygen in blood because every sedative agent will cause some depression in the respiratory parameters. 34 Monitored intravenous sedation with local anaesthesia for dental outpatients Part I 1.4 THE STATE OF ART AT THE BEGINING OF THE WORK IN THE YEARS 1992-1993: REVIEW OF THE LITERATURE 1.4.1 SEDATION WITH LOCAL ANAESTHESIA OR GENERAL ANAESTHESIA? Intravenous conscious sedation with local analgesia is associated with less patient stress than is general anaesthesia. When intravenous sedation is used, only the levels of the plasma growth hormone and prolactin rise significantly. General anaesthesia will significantly increase heart rate, systolic blood pressure, mean arterial pressure, and the levels of plasma epinephrine, cortisone, prolactin, blood glucose; all indicative of a stress response. Conscious sedation can be used correspondingly to reduce measurable parameters of stress, such as serum cortisone levels and systolic blood pressure that patients would develop during operation. (Shepherd et al. 1988, Hempenstall et al. 1986) A cost comparison showed that it was twice as expensive to have the same procedure done in an outpatient surgical suite under general anaesthesia as it was in a private office under Intravenous sedation (Van-Sickels and Tiner 1992). 1.4.1.1 Midazolam 1.4.1.2 Midazolam compared to diatsepam Intravenous midazolam administered in conscious sedation doses reduces significantly the affection and motivational component of the pain experience (Coulthard and Rood 1992), and midazolam produces at least 20 minutes of profound amnesia for all stimuli (Hupp and Becker 1988) A bolus injection followed by the continuous infusion of midazolam shows good safety and better amnesia during procedure than a bolus injection of midazolam, but it prolonged recovery time (Luyk et al. 1992) Midazolam has more advantages for the patient than diazepam; quicker onset of sedation, less pain during injection, profound anterograde amnesia and fewer postoperative complications being the main features (Clark et al. 1987, Clark and Rodrigo 1986, Rodrigo and Clark 1986). Also a more rapid return to normal activities is seen with midazolam. Psychometric testing, however, has failed to show any objective differences between the treatments (Barker et al. 1986). 35 General introduction and review of the literature 1.4.2 PATIENT MANAGEMENT WITH INTRAVENOUS SEDATION 1.4.2.1 Dentist’s sight 1.4.2.2 Patient’s opinion Patient management and general anaesthesia are the most commonly employed techniques. The frequency of the use of intravenous and inhalation sedation varies according to the age of the patient. Only 55% of dentists in general practice have any training in a sedative technique in the UK (Edmunds and Rosen 1989). Intravenous conscious sedation in combination with local anaesthesia is an alternative during unpleasant surgical and dental procedures, and in several cases it can replace general anaesthesia. Monitoring as well as a trained staff make the methods safe and allow to reduce complications (Zoller and Zoller 1992). The length of certain implant surgery operation as well as their precision requires the complete co-operation of patients (Charlton et al. 1991). Many mentally and/or physically handicapped and anxious dental patients do not receive adequate dental treatment because effective ways of supportive treatment are insufficiently known and/or available to dentists (BouvyBerends and Makkes 1990). The predominantly favourable response of the patients leads to the suggestion of using intravenous sedation even in minor oral surgery (Kingon 1990). The majority of the patients has never heard of the availability of intravenous sedation to supplement local anaesthesia during dental surgery; and when given the chance to experience this method the majority will find it highly acceptable: 85 % of the patients prefer surgery under sedation and local anaesthesia to local anaesthesia alone. None prefers general anaesthesia for dental surgery. (Rodrigo and Clark 1986, Lundgren 1988) Postoperatively, many patients have complete amnesia for operative events, most are satisfied with the monitored anaesthesia care and would desire a similar anaesthetic technique for future procedures when intravenous midazolam and fentanyl have been used as primary pharmacological agents in intravenous sedation (Lind et al. 1990). 1.4.2.3 Antagonist to benzodiazepines Flumazenil appears to be a promising drug for reversing midazolam conscious sedation. A patient who receives flumazenil after intravenous midazolam is significantly more alert at 5 min following drug administration (Clark et al. 1991). In cases of undue sedation persisting after dental treatment, flumazenil may be used 36 Monitored intravenous sedation with local anaesthesia for dental outpatients Part I with minimal risk for resedation. Flumazenil in doses from 0.5 to 1.0 mg rapidly reverses the sedative and amnesic effects of midazolam without the apparent evidence of subsequent resedation (Davies et al. 1990). Flumazenil almost totally reverses the effects of mental sedation for approximately 2 hours, but not physical sedation or memory. A number of central nervous systemrelated side effects have been observed but none of these is considered serious (Davies et al. 1990, Ghoneim et al. 1989, Cooper et al. 1991). Flumazenil recipients are less sedated postoperatively, better oriented and more co-operative. The patients cannot remember operative events. The dental surgeons feel that flumazenil makes recovery in the supine position unnecessary and postoperative monitoring easier. Flumazenil is a drug that should be included in the armamentarium of any emergency drug kit when benzodiazepines are used intravenously. (Reed et al. 1989) 37 General introduction and review of the literature 1.4.3 BENZODIAZEPINES COMBINED WITH OPIATES anaesthesia care, and 94% would desire a similar anaesthetic technique for future procedures when intravenous midazolam and fentanyl were used as primary pharmacological agents in intravenous sedation during dental implant surgery (Lind et al. 1990). When nalbuphine and fentanyl were compared as analgesic components of intravenous conscious sedation with diazepam, 88% who received nalbuphine and 87% treated with fentanyl indicated complete pain relief. No statistically significant differences were observed between nalbuphine and fentanyl treatments. (Dolan et al. 1988) 1.4.3.1 Healthy patients The mean consumption of local anaesthetics is significantly lower with intravenous anxiolytics than with intravenous analgesics. The postoperative subjective assessment of the operation by the patients is better under anxiolytic than under analgesic sedation, too. (Breier 1992) However, opiates allow for a significant reduction in the mean dosage of midazolam required to produce satisfactory sedation when compared with experiments where midazolam alone was used. Postoperatively 95 % of the patients are able to walk unaided after 2 hours. At this time, significantly more patients who received opiates were pain free. (Hook and Lavery 1988) Diazepam and midazolam with fentanyl produce a both safe and acceptable sedation. Diazepam causes more venous sequels. The patients who had recieved midazolam had better amnesia effects with no incidence of venous sequels. (Bakaeen et al. 1987) Adequate amnesia associated with midazolam/fentanyl intravenous sedation in the intraoperative period is displayed using a dosage of midazolam 0.10 0.13 mg/kg (Miller et al. 1989). Moreover, midazolam produces at least 20 minutes of profound amnesia for all stimuli (Hupp and Becker 1988). 65% of patients had complete amnesia for operative events, 96% were satisfied with monitored 1.4.3.2 Medically compromised patients The narcotic analgesics fentanyl or alfentanil and the local anaesthetic 4% articaine with epinephrine (1:200,000) have been used for medically compromised patients aged between 32 and 80 years, with an ASA physical status of III and IV. Surgical procedures included multiple dental extraction, cystectomy and the removal of impacted teeth. All patients completed the surgery without deeper anaesthesia and mostly enjoyed a comfortable intraoperative period. Only one respiratory depression was observed, but quickly reversed. Other adverse effects were few and without 38 Monitored intravenous sedation with local anaesthesia for dental outpatients Part I consequences, haemodynamic changes remained in tolerable limits. In conclusion this anaesthetic technique can be a suitable alternative for general anaesthesia in oral surgery for high- risk patients. (Lefevre 1991) Similarly, intramuscular butorphanol was shown to be a safe and effective agent for dental premedication for institutionalised severely and profoundly retarded patients. Vomiting (2.6%) was the most frequent adverse effect observed when sedation was carried over with opiates. (Jann et al. 1987) 39 General introduction and review of the literature 1.4.4 THE COMPARISON OF ORAL AND INTRAVENOUS ADMINISTRATION Rapidly acting oral benzodiazepines such as midazolam provide safe and effective alternatives to intravenous diazepam (Hosie et al. 1988). Although surgeons' ratings indicated that sublingual lormetazepam was comparable to intravenous diazepam, patients' ratings indicated greater satisfaction with and preference for intravenous diazepam (O-Boyle et al. 1988). temazepam. (Skelly et al. 1992) Patients who were given temazepam per os showed wide variations in plasma concentrations. Patients with low plasma temazepam concentrations at the time of surgery showed no significant reduction in anxiety scores. The intravenous diazepam caused greater amnesia during surgery, but showed also a significant slowing of reaction time at the time of discharge. (Hosie et al. 1988) Another non parentheral alternative is the rectal sedation method which is equally efficient with a double dose compared to intravenous administration (Lundgren 1988). Per os temazepam elixir provided a useful sedative for oral surgery, avoiding the complications of intravenous administration. However, for equivalent levels of sedation, intravenous midazolam had greater anxiolytic and amnesic effects than 40 Monitored intravenous sedation with local anaesthesia for dental outpatients Part I 1.4.5 THE NECESSITY OF OXIMETRY DURING INTRAVENOUS SEDATION administered; only 3% of patients who received supplemental oxygen had episodes of hypoxia. The use of supplemental oxygen is recommended for all patients undergoing intravenous sedation. (Hardeman et al. 1990) However, in some patients undergoing a third molar removal with local anaesthetic alone, oxygen saturations in the range of 93-89% were recorded. The results suggest that all patients undergoing the removal of third molars are at risk of hypoxia. Short episodes of hypoxia may be of insignificant consequence in healthy patients, but in compromised patients early detection may avoid serious complications. (Lowe and Brook 1991, Rodrigo and Rosenquist 1988) Careful dosage and the use of an ultra slow technique indicates that a continuous oxygen supplement would not appear necessary routinely (Read-Ward 1990). 1.4.5.1 Hypoxia The arterial saturation of oxygen (SaO2) will decrease abruptly after the administration of sedative agents in each case but there are always individual variations. (Sugiyama et al. 1991) The decrease in saturation may appear during surgery and in the period immediately following surgery. It is suggested that it may be necessary to observe and selectively monitor some patients in the immediate post-surgical period as well as during the period of operation. This would be the case particularly with medically compromised patients and the elderly (Zacharias et al. 1992). A comparison of patients sedated with intravenous lorazepam, diazepam, or midazolam during oral surgery shows that the midazolam group had higher respiratory rates than those of the other two drugs (van-der-Bijl et al. 1991). During the induction of both midazolam and fentanyl or diazepam and fentanyl respectively, the patients had significantly lower average O2 saturation values than receiving either midazolam or diazepam alone. Patients receiving midazolam and fentanyl had lower O2 saturation than the midazolam or the diazepam and fentanyl group. (Tucker et al. 1986) 1.4.5.2 Pulse oximetry There are various technical problems involved in estimating oxygen saturation non-invasively from a light signal transmitted through tissue. The light is absorbed and scattered by tissue, dark skin, and other blood haemoglobin (capillary and venous blood haemoglobin). For these and some other reasons, spectophotometric principles and calculations do not strictly apply for 20% of patients experienced hypoxic episodes in the postanaesthetic recovery unit when no supplemental oxygen was 41 General introduction and review of the literature non-invasive oximeters. Because SaO2 cannot be theoretically calculated, it is estimated by an empirically derived algorithm based on clinical data. For example the Hewlett Packard ear oximeter accurately estimated SaO2 using eight wavelengths of light. Although this device has been useful in pulmonary function laboratories, it is too cumbersome and too expensive to be practical for intraoperative use. Two technological advances and an ingenious idea allowed the development of a new generation of oximeters. The two technological developments were the availability of light emitting diodes (LEDS) and microprocessors. LEDs provide a stable, lightweight light source. Microprocessors allow the programming of complex empirical functions into relatively inexpensive devices. The remaining problem was how to discriminate the arterial haemoglobin saturation from the transilluminated tissue signal. (Temper and Barker 1986) 60% saturation. The pulse oximeter is designed to be insensitive to haemodynamics although extreme hypotension or vasoconstriction may produce a signal that is too weak to process and the oximeter will read a default message (Tremper et al. 1985). The pulse oximeter gives incorrect SaO2 readings in the presence of abnormal haemoglobin due to medication with nitrites or a smoking habit (Sugiyama et al. 1991). In hospitals, monitoring is more regularly used for patients undergoing for example endoscopy than in private offices. During endoscopic procedures, which are comparable to short acting unpleasant dental procedures, most endoscopists monitor vital signs before and after procedures but less often during procedures. However, pulse oximetric and electrocardiographic monitoring is in common use and is also used in most cases during endoscopic procedures. There is a significant relationship between the awareness of oxygen saturation and the timing of nursing interventions e.g. oxygen or antagonist therapy. Because advanced cardiac life support training is not common among endoscopists and gastrointestinal assistants(Keeffe and O-Connor 1990), the use of pulse oximetry is in these circumstances essential (Hinzmann et al. 1992). The solution was to analyse the changes of the light signal produced by arterial pulsation. The signal is then empirically correlated to SaO2 values obtained from an invasive blood sampling which has been demonstrated to be a correct calculation (Tremper et al. 1985; Mihm and Halperin 1985; Yelderman and New 1983). This equipment is able to predict Sao2 with a 3% standard error of the estimate (Tremper et al. 1985). Mihm and Halperin (1985) reported patients with respiratory failure showing about the same standard , even below Some authors are of the opinion that oximetry monitoring may not be clinically useful because the largest mean decrease in oxygen saturation observed during procedures under intravenous sedation is less than that considered normal during sleep. 42 Monitored intravenous sedation with local anaesthesia for dental outpatients Part I Likewise the high incidence of desaturation do not cause adverse outcomes or complications (Berg et al. 1991 and Bilotta et al. 1990). However, pulse oximetry is highly valuable because it will immediately react for any progressive oxygen desaturation and therefore an early correction is possible. As the use of pulse oximetry should be considered obligatory for all endoscopic or paediatric patients during intravenous sedation (Casteel et al. 1990), it is useful as a respiratory monitor during oral surgery (Sugiyama A et al. 1991). 43 General introduction and review of the literature 1.4.6 SEVERE COMPLICATIONS DURING PROCEDURE The most numerous complications are hypoxia and venous irritation. The first is handled in previous chapters, and venous irritation only in the appendixes of this book. 1.4.6.2 Other complications Other possible complications are cardiac dysrhythmias (Rodrigo et al. 1990): During an extraction procedure under local anaesthesia with intravenous sedation using diazepam, a 14 year-old girl patient showed many multifocal premature ventricular contractions in ECG. This patient had the history of a radical operation for tetralogy of Fallot. (Himuro et al. 1989) 1.4.6.1 Psychological complications Fantasies during sedation have been reported with I.V. midazolam or diazepam: most of them had some sexual element and a minority were unpleasant experiences. Some led to litigation against the sedationist. Out of verified reports made by 25 patients of incidents occurring during sedation, 17 did not happen and in 9/13 clear descriptions there was a relation between fantasy and something that really happened under sedation. All occurred with what are now considered large doses of the drugs. Benzodiazepines have proven, in appropriate doses, to be among the safest in medicine for short term use. There have, however, been a few cases of what can be described as fantasies occurring during sedation: events occurring in a logical sequence which are very real to the patient and yet, on the evidence of two or more independent witnesses, did not occur. Many of these have had an element of sexual trespass. (Dundee 1990) The increasing use of intravenous and inhalation sedation in the dental office has the potential of increasing the incidence of malignant hyperthermia which is documented in two cases (Cantin et al. 1986). Paradoxical excitement associated with intravenous conscious-sedation in a patient undergoing dental surgery was successfully reversed with 1.0 mg physostigmine (Milam and Bennett 1987). 44 Monitored intravenous sedation with local anaesthesia for dental outpatients Part I The most important fact is that without general anaesthesia the amnesic effects of benzodiazepines are available in a real-life stress situation. (File et al. 1986) 45 General introduction and review of the literature 1.5 AIMS OF THE STUDY The principal aims of this study were to describe or determine if possible: 1. whether peroperative monitoring by pulse oximetry can detect adverse reactions during intravenous sedation. 2. whether vasoconstrictor containing local anaesthetic preparates have any effects on the blood oxygen saturation and cardiac parameters available when observed with pulse oximetry. 3. the problems related in the use of two local anaesthetic preparations in combination 4. the differences in measurable pulse oximetric recordings of commercial local anaesthetics from the effects of benzodiazepines. 46 Monitored intravenous sedation with local anaesthesia for dental outpatients Part I 5. patients' reactions to treatment under intravenous sedation with local anaesthesia i.e. whether the patients experiences of the procedure under sedation were positive or negative. 6. the patient’s condition during the hours and days following dental operations under sedation; i.e. to study how the patients felt after the treatment under intravenous sedation with local anaesthesia. 7. some false alarms of pulse oximetry, and complicated cases during intravenous sedation with local anaesthesia, and their reasons. 8. arrhythmias and the status of amplitude of pulse wave and sympatho-vagal balance during operation and the following day. 47 General introduction and review of the literature 1.5.1 MORE DETAILED DESCRIPTION OF THE BACKROUNDS AND AIMS OF THE SEPARATE STUDIES intravenous sedation with local anaesthesia. Also changes in the values of blood pressure and pulse were searched from patient monitoring data. 1.5.1.1 Part II (Monitoring...) The background of the studies has been the necessity to find an ideal relation of pain and anxiety relief when anxious patients are treated under intravenous sedation with local anaesthesia. The final reason for this article was the need to describe some false alarms in the oxygen saturation of blood during intravenous sedation, and to find explanations thereto. As benzodiazepines alone do not create pain relief, it is obligatory to also use local anaesthetics in certain cases. An experiment was made with local anaesthetics to differentiate the measurable cardiovascular effects of two commercial vasoconstrictor containing local anaesthetic preparations commonly used worldwide from the effects of benzodiazepines. A lot of information concerning certain parameters which have previously been poorly detected emerged during the course of this study. 1.5.1.2 Part III (Experiences...) Another reason was to find out whether local anaesthetic agents, and sedative vasoconstrictors, have any effects on the cardiac parameters indicating stress when observed with pulse oximetry. Moreover, any undesirable cardiac parameters when two commonly used local anaesthetic agents are used in combination were searched by monitoring. Before the treatments, a number of criteria were considered for the selection for treatment and anaesthesia: who needs sedation, for whom diazepam alone would not be sufficiently effective, and whether there might be any difference in the effectiveness of one type of anaesthesia for different types of operations. Postoperatively, in the cases where the decision is made to use intravenous sedation, many patients have complete amnesia of operative events and typically express the desire for a similar anaesthetic technique in the future. However, it remains unclear how the patients would react to diazepam sedation if used in amounts which would not essentially produce total amnesia. It was also necessary to determine whether peroperative monitoring by pulse oximetry can detect adverse reactions in oxygen saturation during The present study attempts to resolve whether the patients had had positive or negative experiences of the procedure under sedation. Patient 48 Monitored intravenous sedation with local anaesthesia for dental outpatients Part I evaluation would thus indicate whether sedation had any effect on the patient's phobia, i.e. had the phobia been relieved, remained unchanged or even worsened. could be differences between patients who suffered from dental care phobia and those whose treatment was a major oral surgery. Similarly, information was needed on how much time the patient needs for recovery. Moreover, the condition of the patient during the hours and days following dental operations were described. There was a clinical interest to study how the patients felt after the treatment under intravenous sedation with local anaesthesia. In out-patient practice, the only way to find out the patients' condition after the treatment is to make direct questions or to make different psychological measurements to the patients after treatment. In this study, an anonymous questionnaire was sent to resolve the main question, "did the patient have complications after the procedure under sedation" i.e. is the procedure as superior as it seems to be from the point of view of the dentist. It was known very well that postoperatively many patients incur complete amnesia for operative events but it was not known how the patients felt after the procedure when they recovered from the therapy. There was also a need to define if the treatment itself was the main source for the symptoms, and whether there 1.5.1.3 Part IV (Challenges) The purpose of this study is to define the safety of dental procedures under intravenous sedation by recording the arrhythmias during the operation and the following day. Another purpose is to evaluate the sympatho-vagal balance using a frequency-domain analysis of heart rate variability. Since we know that powerful sympathetic activation may increase the risk for arrhythmias, one aim of this study was to clarify the changes in ECG and in the function of the autonomic nervous system during and after oral surgery. A further reason for this article was the need to describe complicated cases during intravenous sedation with local anaesthesia, and their reasons. Moreover, a new prospective index the stress index- is introduced. 49 General introduction and review of the literature 1.6 MATERIALS AND PATIENS for the revision of databases was to get an answer to a very important clinical question: How did the patients feel? The later revised databases formed the study material (retrospective review of patient records). These records included subsequent findings, for instance that the use of a monitor enabled the determination of the correct sedation level earlier and easier than the normally used ptosis i.e. eye closure reaction does. Further questions appeared later on and were attempted to answer through study designs, but in every case the treatment of the patient has been in the first place and the study in the second. Although the monitoring equipment was changed to detect more sophisticated parameters, all the studies have only been clinical follow-ups. Because there was no reference group in every study, all of the parameters were compared with the literature on corresponding studies. 1.6.1 STUDY DESIGN This publication includes three parts of which the first and the last are retrospective descriptive reviews of patient records. There were many differences between patient preparation, cannulation and intravenous infusion, sedative drugs and local anaesthesia i.e. in the underlying factors. It is important to understand that these studies were not controlled clinical trials but clinical follow-ups i.e. observational studies of normal treatment periods. Part III (Experiences...) differs from the other study parts because it does not include monitored findings, but the opinions of treated patients. It is carried out with an anonymous questionnaire which was mailed to the patients who previously underwent intravenous sedation with local anaesthesia. The patients were divided into two main groups: patients to whom the main purpose for the treatment under intravenous sedation with local anaesthesia was the major surgical procedure itself (operation group), and to patients One study comprises course exercises which gave the author an opportunity to allow the students to practice local anaesthesia, to demonstrate cardiovascular effects thereto, and to collect objective measurable findings. Thus there was no indication of approval by an institutional review board governing human experimentation in any of these studies. During treatments and clinical follow-up with pulse oximeter, there was no study design in the first study that would answer any particular question but the aim 50 Monitored intravenous sedation with local anaesthesia for dental outpatients Part I who were scared of dental treatment, i.e. they had dental care phobia (phobia group). corresponding to the ASA I or II groups. The study was done during an ordinary local anaesthesia course for students. Every subject had to come twice to the test on separate days. Part IV is called ”Challenges” because it contains some advantages for monitoring and case studies which have showed poor performance and caused therefore further questions. Survey 3 i.e. the last study of this part is a retrospective review of patient records comprising 26 registrations of the author's private outpatients who underwent dental operations with intravenous sedation. The patients were 16 (62%) males and 10 (38%) females. Mean age was 42 years (SD 15). The patients had some oral surgical operations or they underwent large conservative dental treatment or extraction under sedation because of dental care phobia. 1.6.1.1 PATIENTS 1.6.1.1.1 Patients in Part II (Monitoring...) Survey 1 comprised 41 of the author's private outpatients who underwent dental operations between January and September 1993 with intravenous sedation and local anaesthesia. 44 % of the patients were males and 56 % females. Mean age was 47 years (SD 14). Twenty-three of the patients had surgical operations primarily for implantological reasons, and 18 patients underwent large conservative dental treatment or extraction under sedation because of dental care phobia. They were in good health and had no severe systemic diseases (in the classification of American Society of Anaesthesiology ASA I - II i.e. no systemic diseases or only a moderate disease which do not limit activity). 1.6.1.1.2 Patients in Part III (Experiences...) The research group for studies 4 and 5 consisted of 108 patients undergoing dental procedure with intravenous sedation at the author’s private practice. They were 46 % males and 54 % females. Mean age was 42 years (SD 13). Patients underwent surgery primarily for implantological reasons, major conservative dental treatment, or extraction under sedation due to dental care phobia. The subjects were unselected private practice dental patients in a good state of health or suffering from systemic disease which may moderately limit their activity, i.e. they conformed to groups I-III of the ASA (American Association of Anaesthesiologists) classification. None of the patients Survey 2 consisted of twenty dental students. The students were between 19 and 31 years of age with a mean age of 22 years (SD 3); 80 % were females. Each person accepted in the test group had to be healthy and free of any surgical risk, 51 General introduction and review of the literature corresponded to the ASA classification for groups IV - V. The patients were within the limits of generally accepted indications and contraindications as mentioned in the text books for dental anaesthesia. were within the limits of generally accepted indications and contraindications as mentioned in the text books for dental anaesthesia and oral surgery. 2. The reference group 1.6.1.1.3 Patients in Part IV (Challenges) The reference group consisted of 12 patients undergoing dental procedure without intravenous sedation. Sexual distribution was balanced between females and males, i.e. 50 % and 50 %. Mean age was 45 years (SD 15). Subjects were unselected University clinic patients, who were transmitted to the department of oral surgery. They were all voluntary for study and they conformed to groups I-II of the ASA (American Association of Anaesthesiologists). None of the patients corresponded to the ASA groups IV - V. Thus the patients were within the limits of generally accepted indications and contraindications for dental treatment. This part includes three studies. The first of them is survey 6; it is the only one which has an independent study group. The later two study groups are formed by combining the study groups of previous works, and only reorganizing the question or aim. Survey 6 combines two groups of patients, of which the author’s private practice patients are called ‘the study group’ and the university clinic patients ‘the reference group’. 1. The study group: The research group consisted of 23 patients undergoing dental procedure under intravenous sedation at the author's private practice. They were 35 % males and 65 % females. The mean age was 48 years (SD 17). The patients underwent surgery primarily for implantological reasons, major conservative dental treatment, or extraction under sedation due to dental care phobia. The subjects were ordinary, unselected private practice dental patients, who conformed to groups I-III of the ASA (American Association of Anaesthesiologists). None of the patients corresponded to the ASA groups IV - V. The patients Study 7 includes a part of patients and subjects from studies 2 and 3. Study 8 is a study of complicated cases. There were differences between patient preparation (eating instructions), cannulation and intravenous infusion as well as local anaesthesia i.e. in the underlying factors. Thus these studies are mainly non-randomised studies to compare two types of patient care. 52 Monitored intravenous sedation with local anaesthesia for dental outpatients Part I Table 1. Patients Study number: Number of subjects Indication 1 41 23 surgery 18 phobia Males % 44 Females % 56 Age years, mean 47 SD 15 range 23-76 Parameters measured SaO2 BP Pulse Main sedative agent Time Lidocain (mg) Mean SD Cases Prilocain (mg) Mean SD Cases Midazolam (mg) Mean SD Cases Diazepam (mg) Mean SD Cases Fentanyl (mg) Mean SD Cases Midazolam 1993 154 80 39 241 111 38 5.38 1.93 32 22.5 8.3 7 0.079 0.019 7 2 20 course exercise 20 80 22 3 19-31 SaO2 BP Pulse A.P.W. 1995 180 20 270 20 - - * Not available on collected data ** See text 53 3 26 surgery phobia 62 38 42 15 18-76 SaO2 Pulse A.P.W. 4-5 108 38 surgery 53 phobia 46 54 42 13 16-78 - 6 35 surgery phobia 40 60 47 16 21-81 SaO2 Pulse ECG Midazolam 1994 155 54 26 203 118 17 5.02 1.72 26 - Diazepam 1992 177 86 100 234 108 88 6.2 2.7 24 12 5 85 0.065 0.025 7 Midazolam 1996 * * ** - - General introduction and review of the literature 1.6.2 PRE- AND POSTOPERATIVE PATIENT PREPARATION In all studies except studies 4-6, patient preparation was identical: During the first examination, all patients completed a questionnaire about previous and present illnesses, allergies and medications. A dental care plan was drawn up and all the patients were referred to radiological examination (orthopantomography). All the patients who underwent major surgical operation e.g. sinus-lift procedure, were also referred to laboratory blood evaluations (Sedimentation rate, B-Hb, B-leuk, fB-glu). The patients were advised both verbally and in writing how to prepare for intravenous sedation (for example, no food or drink for four hours prior to treatment). and medication for cardiopulmonary resuscitation. All treatments were carried out by the same dentist, i.e. the author. After treatment blood pressure was recorded again and the venous cannula removed. The patients stayed in the dental chair, and pulse oximetric monitoring was continued until bleeding after extraction had stopped and until the patients felt well and were able to walk and get dressed without help. The patients left the clinic with an adult escort. Patients were not given oral premedication, sedatives nor antibiotics on the day of the operation or the previous day. Blood pressure was recorded and monitoring with a pulse oximeter initiated before the insertion of a peripheral venous cannula. After the insertion of the cannula, an infusion of 0.9% sodium chloride solution was started, and then the sedative agent was applied with disposable syringe using the slow injection technique. After sedation local anaesthesia was performed. The treatment room was equipped with dental unit, pulse oximeter, oxygen supplement unit and some resuscitation facilities, including endotracheal intubation equipment In survey 6, patient preparation was similar to the study group but for the reference group the written instructions on how to prepare for the 54 Monitored intravenous sedation with local anaesthesia for dental outpatients Part I operation it was particularly mentioned that they should eat before operation. This was a result of different preparation practices of the University clinic and the author's private office. analgesic drug) before operation. Blood pressure was recorded and Holter ECG initiated in the operation theatre before operation. The treatment room was equipped in the same way as the other studies but the treatment procedures were carried out by several surgeons. Neither in reference group patients were given oral premedication (e.g. 55 General introduction and review of the literature 1.6.3 MEDICATION for sedation (Dormicum 5 ml inj. 1 mg/ml Roche), with mean amounts 5.02 mg SD 1.72 mg. Fentanyl (Fentanyl 2 ml inj. 50 microgram/ml Orion R) was not used for additional pain relief preoperatively, only in 1 case for analgesia postoperatively (0.05 mg). 1.6.3.1 Medication in Part II (Monitoring...) 1.6.3.1.1 Sedation In survey 1 an infusion of 0.9% sodium chloride solution was started, and then the sedative agent was applied with a disposable syringe using the slow injection technique. Diazepam with soybean oily solvent was used for sedation in 7 treatment periods (Stesolid Novum 2 ml inj. 5 mg/ml Dumex/KabiVitrum) and midazolam in 32 cases (Dormicum 5 ml inj. 1 mg/ml Roche), with mean amounts 22.5 mg SD 8.3 mg and 5.4 mg SD 1.9 mg respectively. Fentanyl (Fentanyl 2 ml inj. 50 microgram/ml Orion R) was used for additional pain relief in only 3 cases (mean 79 microgram SD 19 microgram) and only if there was insufficient level of local anaesthesia. The author used intravenous agents divided into small parts (2 mg diazepam and 1 mg midazolam). This almost barely effective dose was repeated every 2 or 3 minutes until a minor decrease (2 - 3 %) in blood oxygen saturation is detected. Extra doses after the initial saturation fall were not normally used with patients aged over 60 years. The benzodiazepine antagonist used was flumazenil (Lanexat 5 ml inj. 0.1 mg/ml Roche). 1.6.3.1.2 Local anaesthesia In survey 1 local anaesthesia was performed with lidocaine (Xylocain adrenalin 1.8 ml inj. 20 mg/ml+12.5 microgram/ml ASTRA, mean 7.74 ml SD 4.23 ml) and prilocaine (Citanest Octapressin 1.8 ml inj. 30 mg/ml+0.54 microgram/ml ASTRA, mean 8.01 ml SD 3.91 ml). The same protocol to combine two agents was performed in every study of this publication. Because the dentist’s (author’s) normal practice is to avoid high epinephrine amounts he always uses two different local anaesthetics. Thus the method is used in these studies, too. In survey 2 the mentioned practice was further studied and local anaesthesia was performed with a lidocaine - epinephrine solution (Xylocain adrenalin 1.8 ml inj. 20 mg/ml+12.5 mcg/ml ASTRA) and prilocaine - phelypressine solution (Citanest Octapressin 1.8 ml inj. 30 mg/ml+0.54 mcg/ml ASTRA). The site of injection was the upper jaw, the buccal sulcus just distal of the second upper molar. Both sides of the maxilla were anaesthetised. This site In survey 2 no sedation was used. In survey 3 after starting an infusion, only midazolam was used 56 Monitored intravenous sedation with local anaesthesia for dental outpatients Part I was chosen because there is room for a large enough volume of local anaesthetic, and the trifurcation of the trigeminal nerve is near the anaesthetised area. Local anaesthesia was performed in combination with lidocaine (Xylocain adrenalin 1.8 ml inj. 20 mg/ml+12.5 mcg/ml ASTRA) mean 8.8 ml SD 4.3 ml and prilocaine (Citanest Octapressin 1.8 ml inj. 30 mg/ml+0.54 mcg/ml ASTRA) mean 8.6 ml SD 3.6 ml. In survey 3 local anaesthesia was performed with a lidocaineepinephrine combination (Xylocain adrenalin 1.8 ml inj. 20 mg/ml + 0.0125 mg/ml, ASTRA, mean 155 mg SD 54.3 mg lidocaine and 0.097 mg SD 0.034 mg epinephrine) and prilocaine-phelypressine combination (Citanest Octapressin 1.8 ml inj. 30 mg/ml+0.54 microgram/ml ASTRA, mean 203 mg SD 118 mg prilocaine and 0.0036 mg SD 0.0021 mg). 1.6.3.3 Medication in Part IV (Challenges) In the study group of survey 6 an infusion of 0.9% sodium chloride solution was started, and then the sedative agent was applied with a disposable syringe using the slow injection technique. Midazolam was used for sedation (Dormicum 5 ml inj. 1 mg/ml Roche). The benzodiazepine antagonist used when needed was flumazenil (Lanexat 5 ml inj. 0.1 mg/ml Roche). Local anaesthesia was performed with lidocaine (Xylocain adrenalin 1.8 ml inj. 20 mg/ml+12.5 microgram/ml ASTRA) and prilocaine (Citanest Octapressin 1.8 ml inj. 30 mg/ml+0.54 microgram/ml ASTRA). 1.6.3.2 Medication in Part III (Experiences...) In studies 4 and 5 diazepam with soybean oil solvent was used for sedation in 85 cases (Stesolid Novum 2 ml inj. 5 mg/ml Dumex/KabiVitrum) or midazolam in 24 cases (Dormicum 5 ml inj. 1 mg/ml Roche) with the mean amounts corresponding to 12 mg SD 5.0 mg and 6.2 mg SD 2.7 mg, respectively. For pain relief, fentanyl (Fentanyl 2 ml inj. 50 microgram/ml Orion) was rarely used (only in 7 cases, combined with some of the sedative agent mentioned above); when used it was administered in the slightest amounts (mean 1.3 ml SD 0.5 ml). The benzodiazepine antagonist which was available, and used when needed in these cases, was flumazenil (Lanexat 5 ml inj. 0.1 mg/ml Roche). No sedatives were used in the reference group, only local anaesthesia was performed with lidocaine (Xylocain adrenalin 1.8 ml inj. 20 mg/ml+12.5 microgram/ml ASTRA) or/and prilocaine (Citanest Octapressin 1.8 ml inj. 30 mg/ml+0.54 microgram/ml ASTRA). Medication in studies 7 and 8 are described solely in these studies. 57 General introduction and review of the literature 1.6.4 MONITORING AND DATA REVIEW In part II (Monitoring...) of the first study the patients were monitored with an Ohmeda Biox 3740 (Ohmeda, USA) Pulse Oximeter, in the second study with a CARDIOCAP II CH-S (Datex, Helsinki Finland) multiparameter physiological monitor, and in the third study with SATLITE TRANS TM (Datex, Helsinki Finland) pulse oximeter. The monitors were connected to the serial port of Toshiba T1000SE portable computer for the trend collection of data by a collection program. In the first study the program was Ohmeda's own program: 37XX, but in the other studies custom-made programs were used for the real-time collection of data. Later programs recorded numerical values from pulse oximeter after the whole treatment and followup period. The data on blood pressure, pulse, initial and minimal SaO2 were collected from patient history files which were formed as on-line registerations during operations and parameters were further analysed using the computer. In the second study, blood pressure was measured and the data collected automatically every two minutes from the subjects' left upper arm. Ohmeda pulse oximeter but no data collection was done. In Part III (Challenges), monitoring was a combination of pulse oximetry (Ohmeda) and ECG which was performed with Holter recordings. All of the Holter tapes in the study population were analysed using the Marquette 8500 scanner running version 5.7 of the Marquette arrhythmia analysis program allowing the detection of normal sinus beats and supraventricular and ventricular extrasystoles. After an automatic analysis of the tape, the data file was visually reviewed and manually corrected. Heart rate variability analysis was performed by running the Marquette heart rate variability analysis program. The HRV analyses were performed using four consecutive minutes’ periods during surgery and the three following hours after the operation. Total power (TP) between 0 - 0.40 Hz along with the power in the low-frequency band (LF, 0.04 to 0.15 Hz) and in the highfrequency band (HF, 0.15 to 0.40 HZ) were calculated and logarithmically transformed. In addition to spectral components, also LF to HF ratios and normalised units were used as markers of sympatho-vagal balance during the different stages of operation and recovery period. In Part III (Experiences...) the patients were monitored with 58 Monitored intravenous sedation with local anaesthesia for dental outpatients Part I 1.6.5 THE WORKING PRINCIPLE OF THE PULSE OXIMETRIC EQUIPMENT A pulse oximetry probe includes a light emitter and detector (finger probe), which are connected to the monitor. The emitter emits red and infrared light, which passes through the tissue to the detector. The pulse wave is derived from the detected infrared signals so that the actual pulse wave is displayed as a mirror image of the intensity wave form. In pulse oximetry a photoelectric measures the absorption of light using two different wave lengths. In the area of infrared light the absorption is not affected by the changes in the oxyhemoglobin concentration and so the changes in infrared absorption essentially reflect only changes in local blood volume. The pulsation of the arterial blood flow modulates the light passing through it, and the oximeter converts this light intensity information into pulse rate values, which are presented together with SaO2 values on a monitor screen. The pulse wave is derived from the intensity of the transmitted light. The pulsating blood flow in the finger is the result of the left ventricle contraction of the heart, which fills the vascular bed of the finger with arterial blood. It is important to understand that the pulse wave reflects changes in blood volume, not changes in blood pressure. The oximeter converts this light intensity information into pulse rate values which are presented with SaO2 value in a liquid crystal display or on the screen. The microprocessor calculates the SaO2 e.g. 25 times per second. These calculations are averaged by running-weighted-average method which allows erroneous SaO2 values to be discarded when the displayed value is determined. 1.6.5.1 Different equipment philosophies Ohmeda Biox 3740 Pulse Oximeter is a stand-alone, noninvasive, arterial oxygen saturation monitor, providing continuous, realtime SaO2 and pulse rate readings. The light generated in the finger probe passes through the tissues. The oximeter measures the relative absorption of red light at 660 nm and infrared light at 940 nm by Hb and HbO2. Two different forms of haemoglobin, oxyhemoglobin and reduced haemoglobin allow different amounts of light to pass at these wave lengths. Similarly, the pulsation of the arterial blood flow modulates the passing light. The oximeter converts these changes in information into pulse rate and SaO2 value. Similarly Datex pulse oximetric equipment (Cardiocap and Satlite Trans) function using the light which is generated in the finger probe, and the light passes through the tissues. The total absorption of the light depends on the absorbing components 59 General introduction and review of the literature again: tissues, venous blood and the pulsating arterial blood. Different amounts of light are absorbed by oxygenated haemoglobin (HbO2) and unoxygenated or reduced haemoglobin (Hb). These oximeters measure the relative absorption by Hb and HbO2 of red light at 660 nm and infrared light at 910 nm. automaticaly correct the amount of amplitude of pulse wave when represented on screen. This gives one additional measurable parameter for analysis: the level of vasoconstriction which is controlled by autonomic nervous system. The main difference between the equipment is that Datex do not 60 Monitored intravenous sedation with local anaesthesia for dental outpatients Part II PART II MONITORING THE PATIENTS WITH THREE PULSE OXIMETER EQUIPMENT 61 Monitored intravenous sedation with local anaesthesia for dental outpatients Part II 2.1 Survey 1 Detection of oxygen saturation under intravenous sedation with Ohmeda pulse oximeter and registration of other cardiovascular parameters 2.1.1 ABSTRACT In this survey 41 patients were monitored with a pulse oximeter giving oxygen saturation and pulse values. Blood pressure values were measured separately during major or protracted dental operations under intravenous sedation with local anaesthesia. The most important finding was that there seems to be a risk that low oxygen saturation (SaO2 < 90%) before sedation constitutes a risk for oxygen desaturation during sedation. Before starting the procedure, the mean of oxygen saturation level (SaO2) was found to be 98,1%. The lowest SaO2 levels were found some minutes after injection or later during the treatment when the average level was 92,7 % (p<0.0001). For patients who had preoperative SaO2 over 98% the minimum saturation was at the average level of 94%. The patients with the initial saturation under 98% showed signs of measurable desaturation - mean level 88%. However, desaturation did not correlate with the dose of the sedative agent when this was used at the therapeutic level. Only five cases with low arterial oxygen saturation were found (SaO2 under 90 %), and all the problems related to sedation were resolved by administering supplementary oxygen or a benzodiazepine antagonist. Blood pressure and pulse rate were slightly lower after the treatment than before it. In systolic blood pressure the difference was significant (p=0.04). Pulse oximetric monitoring was found to be extremely sensitive as a predictor for desaturation and it also allows early intervention in ventilation problems. 63 Monitoring the patients with three pulse oximeter equipments arterial blood oxygenation, as measured by pulse oximetry (Matthews et al. 1992). Arterial oxyhemoglobin saturation (SaO2) drops regularly after the administration of a notable amount of a sedative agent. There is also a significant decrease in the saturation level of oxygen as sedation progresses from light to deep. Age is positively correlated with desaturation, but a history of disease or medications have failed to be sensitive predictors of desaturation (Bilotta et al. 1990). The protracted half-lives of some benzodiazepines, and drug interactions, if opioids are used in combination with benzodiazepines, appear to be potential hazards in the elderly. Desaturation slightly below 90% may be clinically insignificant since no complications have been noted at this level (5,4). As it is impossible to identify patients at risk for hypoxaemia beforehand, it is recommended that supplemental oxygen should be given to all patients and that monitoring should be performed by pulse oximetry. 2.1.2 INTRODUCTION Intravenous sedation has been shown helpful in avoiding cardiovascular reactions in oral surgical operations, but there is a risk of provoking respiratory depression. This adverse effect can easily be detected at an early stage, where the pulse wave and / or a drop in saturation is signalled visually and can be corrected by administering supplementary oxygen. Monitors as well as intravenous sedation are still very seldom used in Europe in dental practice despite their low cost. Fatal complications in the dental chair are so uncommon that the use of monitors is not obligatory, and is not recommended by the local authorities. This is in contrast to the situation in United States, Japan, Canada and many other parts of the world. There the monitors are in widespread use for conscious intravenous sedation; in fact, they are mandated by laws and practice standard. Our tradition relies on the high education level of the medical and dental practicians and no exact rules exist. However, episodes involving some degree of risk or discomfort do occur, and changes in the patients’ cardiovascular status also occur regularly . It is not so much a question of "life or death" but of the quality of care in general. Many of the basic principles of monitoring accepted in anaesthesia for general surgery can also be applied in dental surgery. The method of early detection of hypoxia with pulse oximetry during intravenous sedation has been previously described by the author. When the decrease of SaO2 is observed, external oxygen or alternatively an injection of The administration of diazepam until ptosis is observed is a safe procedure and although changes in SaO2 and pulse rate do occur, these alterations are not significant and SaO2 remains above 95% (Gallon et al. 1992). Similarly, intravenous sedation with midazolam causes a statistically significant but physiologically insignificant fall in 64 Monitored intravenous sedation with local anaesthesia for dental outpatients Part II benzodiazepine antagonist can be used. peroperative monitoring by pulse oximetry can detect adverse reactions in oxygen saturation during intravenous sedation with local anaesthesia. Also information on changes in the values of blood pressure and pulse was needed from patient monitoring data. The aim The aim of this survey was to determine the usefulness of pulse oximetry during intravenous sedation in dental practice i.e. whether 65 Monitoring the patients with three pulse oximeter equipments 2.1.3 PATIENTS AND METHODS 2.1.3.1 Study design This survey consisted of all (i.e. 41) of the author's private outpatients who underwent dental operations between January and September 1993 with intravenous sedation. The patients were 44 % males and 56 % females. Mean age was 47 years (SD 14). Twenty-three of the patients had surgical operations primarily for implantological reasons, and 18 patients underwent large conservative dental treatment or extraction under sedation because of dental care phobia (Table 1). Some patients had a second sedated and monitored treatment period later. These later treatments are excluded from the study material. This study is a retrospective descriptive review of patient records which were formed with on-line registeration program. The method is still retrospective because the recordings were not made for study but for normal careful patient and treatment follow-up and notes. There were many differences between patient preparation, cannulation and intravenous infusion, sedative drugs and local anaesthesia i.e. in the underlying factors. It is important to understand that this study was not a controlled clinical trial but a clinical follow-up of normal treatment periods. Thus there was no indication of approval by an institutional review board governing human experimentation. During treatments and the clinical follow-up with pulse oximeter there was no study design that would answer a particular question. The later revised databases formed the study material (retrospective review of patient records). These records included subsequent findings, for instance that the use of a monitor made it possible to determine the correct sedation level earlier and easier than the normally used ptosis i.e. eye closure reaction does. Because there was no reference group, e.g. the appearance of oxygen desaturation (Sao2 < 90%) was compared with the literature. During the first examination, the patients completed a questionnaire about previous and present illnesses, allergies and medications. A dental care plan was drawn up and all the patients were referred to radiological examination (orthopantomograph) and all the implantological patients except patients aged under 50 years requiring a single tooth replacement were also referred to laboratory blood evaluations (B-Se, B-Hb, B-leuk, fBglu). The patients were advised both verbally and in writing on how to prepare for intravenous sedation (for example, no food or drink for four hours prior to treatment). They were in good health and had no severe systemic diseases (in the classification of American Society of Anaesthesiology ASA I - II i.e. no 2.1.3.2 Patients 66 Monitored intravenous sedation with local anaesthesia for dental outpatients Part II systemic diseases or only a moderate disease which do not limit activity). 2.1.3.3 Sedation Patients were not given oral premedication, sedatives nor antibiotics on the day of the operation or the previous day. Blood pressure was recorded and monitoring with a pulse oximeter initiated before the insertion of a peripheral venous cannula. After the insertion of the cannula, an infusion of 0.9% sodium chloride solution was started, and then the sedative agent was applied with disposable syringe using the slow injection technique. The treatment room was equipped with dental unit, pulse oximeter, oxygen supplement unit and some resuscitation facilities, including endotracheal intubation equipment and medication for cardiopulmonary resuscitation. All treatments were carried out by the same dentist, i.e. the author. Diazepam with soybean oily solvent was used for sedation for 7 patients (Stesolid Novum 2 ml inj. 5 mg/ml Dumex/KabiVitrum) and midazolam in 32 cases (Dormicum 5 ml inj. 1 mg/ml Roche). Table 2 presents the doses of the agents used. Fentanyl (Fentanyl 2 ml inj. 50 microgram/ml Orion R) was used as an additional pain relief in only 3 cases (mean 79 microgram SD 15.5 microgram), and only if there was an insufficient level of local anaesthesia. Intravenous agents were divided into small parts (2 mg diazepam and 1 mg midazolam). This almost barely effective dose is repeated every 2 or 3 minutes until a minor decrease (2 - 3 %) in blood oxygen saturation is detected. Extra doses after the initial saturation fall were not normally used with patients aged over 60 years. The benzodiazepine antagonist used was flumazenil (Lanexat 5 ml inj. 0.1 mg/ml Roche). Table 1. Distribution of patients according to sex and type of treatment. Number of patients. MALE FEMALE Local anaesthesia was performed with lidocaine (Xylocain adrenalin 1.8 ml inj. 20 mg/ml+12.5 microgram/ml ASTRA, mean 7.74 ml SD 4.23 ml) and prilocaine (Citanest Octapressin 1.8 ml inj. 30 mg/ml+0.54 microgram/ml ASTRA, mean 8.01 ml SD 3.91 ml). There was no particular reason for the use of two different local anaesthetics; it was only the author’s normal practice to avoid high epinephrine amounts. TOTAL Conservative treatment 8 10 18 Surgical operation 10 13 23 Total 18 23 41 After treatment, blood pressure was recorded again and the venous cannula removed. The patients stayed 67 Monitoring the patients with three pulse oximeter equipments in the dental chair and pulse oximetric monitoring was continued until bleeding after extraction had stopped, and until patients felt well and were able to walk and get dressed without help. Table 2B. The average amounts and standard deviations of the medications used in this survey. Quantities of the agents are expressed in milligrams. Table 2A. The average amounts and standard deviations of the medications used in this survey. Quantities of the sedative agents are expressed in millilitres and those of the local anaesthetics in 1.8 ml syringe ampoules. MEDICATION Dormicum MEAN SD 5.38 1.93 32 4.50 1.66 7 1.58 0.38 3 4.21 2.22 39 4.47 2.06 38 ml Xylocain 1.8 ml ampoules Citanest SD CASES Midazolam mg 5.38 1.93 32 Diatzepam mg 22.5 8.3 7 Fentanyl mg 0.079 0.019 3 Lidocaine mg 154 80 39 Prilocaine mg 241 111 38 Patients were monitored with an Ohmeda pulse oximeter and the data was collected with Ohmeda's own program (37XX) using a Toshiba T1000SE computer. The 37XXprogram do not allow exact notes from the patients, it is mainly visual. Thus in many case maximum or minimum values had to exclude because of unvaluable data. Ohmeda Biox 3740 Pulse Oximeter is a standalone, non-invasive, arterial oxygen saturation monitor, providing continuous, real-time SaO2 and pulse rate readings. ml Fentanyl MEAN 2.1.3.4 Monitoring and data review CASES ml Stesolid MEDICATION 1.8 ml ampoules The monitor was connected to the serial port of Toshiba T1000SE portable computer for the trend collection of data by a collection program (The Ohmeda program 37XX). The program recorded numerical values from pulse oximeter after the whole treatment and followup period. 68 Monitored intravenous sedation with local anaesthesia for dental outpatients Part II Blood pressure values were measured with a separate noninvasive automatic meter (Omron, model-hem 700CP), and the values were saved in the patient history files. saturation was associated with the change in other variables. The correlation coefficient (r) was calculated using the analysis of a variance table, i.e. in the case of oxygen saturation and systolic blood pressure, the correlation (Bland and Altman 1995) was calculated using the formula: The collected data was reviewed and every registration with oxygen saturation under 90% or pulse rate over 120 per minute was printed out for further investigations. The data on blood pressure, pulse, initial and minimal SaO2 was collected from patient history files and parameters were further analysed using the Microsoft Works-2 and MedStat programs and the previously mentioned Toshiba AT personal computer. r= Sum of squares for systolic BP Sum of squares for systolic BP + residual sum of squares A stepwise multiple regression analysis was performed to find the possible preoperative indicator variables on minimal oxygen saturation during a dental operation. The variables introduced to the model were preoperative diastolic and systolic blood pressure, pulse and oxygen saturation. 2.1.3.5 Statistical methods Paired t-test was used to compare response variables before and after a dental operation. The changes were described as means and 95% confidence intervals. Analysis of covariance (ref) was used to study whether the change in oxygen The data were analysed using SPSS statistical package (Version 6.1.3). 69 Monitoring the patients with three pulse oximeter equipments 2.1.4 RESULTS certain period of time between 8589%. In three cases, SaO2 fell below 85% and hypoxia was severe. The lowest detection in the collected data was, however, higher: 82%. Pulse rate over 120 was detected only in two cases. In some cases, very short periods of extrasystoles (which were impossible to diagnose precisely with pulse oximeter) were detected but no severe arrhythmias or cyanoses were found, and the oxygen desaturation could be corrected in every case with supplementary oxygen or with flumazenil, a benzodiazepine antagonist. 2.1.4.1 Oxygen saturation of the blood The highest oxygen saturation of arterial blood (SaO2) detected in the patients were at the beginning of measuring. The average of these levels was 98.1 % (SD 1.4 %). The lowest SaO2 levels were found some minutes after the injection of sedative agents or later during the treatment period (mean 92.7 % SD 3.3%). The maximal effects of the midazolam on oxygen saturation are shown in Fig. 2 as a function of dose. Significant is the correlation between initial SaO2 and minimum saturation, as shown in Fig. 1. Patients who had preoperative SaO2 over 98% had the minimum saturation at the average level of 94%, and when the initial saturation was exactly 98% the average minimum saturation was 93%. Patients with the initial saturation under 98% showed signs of measurable desaturation - mean level 88%. This means that low oxygen saturation before sedation constitutes a risk for oxygen desaturation during sedation. However, it was impossible to show any sensitivity to desaturation because the percent decreases of SaO2 were identical in each group. Desaturation did not correlate with the dose of sedative agent if used at therapeutical level. 2.1.4.2 Other remarks Blood pressure and pulse rate were also measured before and after treatment, and they are shown in Table 3. Both values were slightly lower after treatment but there was no statistical significance in pulse rate and diastolic blood pressure but, however, in the systolic blood pressure the decrease was significant (p=0.04). Cardiovascular reactions to medication are shown in Fig. 2 as function of the dose of sedative agents. No significant changes were seen in blood pressure or in pulse rate. A multiple regression analysis of preoperative variables on minimal oxygen saturation (SaO2) during a dental operation shows that only low initial oxygen saturation predicts desaturation during the treatment under sedation (table 5). Desaturation (SaO2 below 90%) was detected only in five cases. In two of these the hypoxia was mild, i.e. oxygen saturation remained for a 70 Monitored intravenous sedation with local anaesthesia for dental outpatients Part II Table 3. Blood pressure, (mmHg), pulse rate and oxygen saturation (%) before and after a dental operation. Before After Change Mean SD Mean SD Mean p-value 95 % CI Systolic BP 148.6 24.8 141.6 21.3 -6.9 0.04 (-13.4 to -0.4) Diastolic BP 91.0 16.8 87.9 13.7 -3.1 0.12 (-11.0 to +1.3) Pulse rate 77.8 16.1 72.9 12.2 -4.9 0.12 (-11.0 to +1.3) Oxygen saturation 98.1 1.4 92.7 3.3 -5.4 <0.0001 (-6.3 to -4.5) Table 4. Correlation between individual changes in oxygen saturation and changes in blood pressure and pulse rate. Changes in oxygen saturation vs. changes in Correlation coefficient p-value Systolic BP 0.37 0.05 Diastolic BP 0.30 0.13 Pulse rate 0.21 0.31 Table 5. A multiple regression analysis of preoperative variables on minimal oxygen saturation (SaO2) during a dental operation. Coefficient Constant Preoperative Sa02 -21.7 (SE) 25.2 1.190 0.255 Model R2=0.44 71 p-value 0.40 0.0001 Monitoring the patients with three pulse oximeter equipments Figure 1. The relation between SaO2 before and after or during (minimum value) the dental operation. The values were determined from the screen as a clinical dentist will see it. Figure 1 Minimum saturation % 100 98 96 94 92 90 88 86 84 82 80 94 95 96 97 98 99 100 Preoperative oxygen saturation % Figure 2. The relationship of midazolam dose to minimum oxygen saturation. Only the cases who had recieved only midazolam are represented. Figure 2 100 Minimum saturation % 98 96 94 92 90 88 86 84 82 80 1 2 3 4 5 6 7 8 Dose of m idazolam (m g) 72 9 10 11 Monitored intravenous sedation with local anaesthesia for dental outpatients Part II 2.1.5 DISCUSSION previously mentioned, large amounts of sedatives were used in the present survey but the desaturation (< 90 %) incidence was only slightly over 10 %. 2.1.5.1 Desaturation Arterial oxyhemoglobin saturation (SaO2) is lower after the administration of a notable amount of sedative agents. There is also a significant decrease in the saturation level of oxygen as the patient progresses from light to deep sedation. The intravenous diazepam and midazolam have been shown to decrease oxygen saturation by 3% as compared to the preoperative level when administered in the average dosages of 6.4 mg and 3.3 mg respectively. (Matthews et al. 1992) In this survey, much greater amounts of sedative agents were used (three times the previously mentioned amount of diazepam and 1.5 times that of midazolam, and consequently the decrease in saturation was greater (approx. 5%). However, even unsedated patients who only have local anaesthesia have a small postoperative fall in oxygen saturation (Matthews et al. 1992), but the decrease as a result of local anaesthesia is under 1% (survey 2). Ventilation hazards of intravenous midazolam may appear in the elderly, and the use of benzodiazepines with lower hypnogenic effects is recommended (Heinze and Rohrbach 1992). The incidence of saturation falling to less than 90% have reported to have been between 4% and 40% depending of the level of sedation (Tay et al. 1991, McKee et al. 1991, Hardeman et al. 1990) which is an interesting finding. As Premedication with a combination of fentanyl and diazepam until eye closure is induced leads to a more significant reduction of SaO2. In most of the patients, minimum SaO2 has been lower than 90%, and it has been lower than 85% in more than every third patient (Castillo et al. 1990). No effect of the opiate and sedative combination on oxygen saturation was seen in the present survey, because fentanyl was used so rarely (in only three patients) and in normal amounts (79 microgram). However, extreme care is essential if this combination is used. It is possible that the relatively low incidence of desaturation in this survey is a result of early recognition of initial 2-3% SaO2 decrease with pulse oximetry during the initiation of the sedation. Patients at risk for hypoxaemia cannot be identified definitely prior to the initiation of the procedure (Visco et al. 1989). However, if dental patients are monitored with pulse oximetry, and an ultra-slow technique is used with careful dosage in the administration of sedative agents, no continuous oxygen supplement is necessary routinely (Read-Ward 1990), although it should be available. No routine oxygen supplement was used with the 73 Monitoring the patients with three pulse oximeter equipments patients in this survey. The minor decrease in SaO2 was used as a sign of sufficient sedation during the initiation of medication and oxygen was added only if the 90% level lasted a long time. However, Lowe and Brook (1991) have reported oxygen saturation in the range of 9389% in some patients undergoing third molar removal with local anaesthetic alone! They concluded that all patients undergoing removal of third molars are at risk of hypoxia. Short episodes of hypoxia may be of little consequence in healthy patients, but with compromised patients early detection may avoid serious complications (Rodrigo and Rosenquist 1988). Moreover, there is some information available that a cardiac patient might develop a decrease in oxygen delivery that may be due to increased pulmonary vascular resistances (Nishida et al.1996, Slater et al. 1995, Francoise et al. 1996). However, no negative correlation between diastolic blood pressure and minimal oxygen saturation could be shown in this survey. This finding is important to remember in patient selection: sedation is often used to reduce the stress of cardiac patients. the medication used, and they can lead to a deterioration of the patient's own organic disease. It is extremely important to recognise this in good time, so that the right decisions can be made on appropriate therapeutic actions. The patients in this survey accepted this non-invasive monitoring method quite easily. For the dentist, the machine was easy to use. The size of the monitor is small, and sufficient in dental chair surroundings. Without these features the device is useless in the dental office. Moreover, the monitor should react dynamically to changes and give a clear warning if any problems arise. It should monitor the arterial oxygen saturation and the continuous pulse wave should be visible on the screen. The review of the follow-up immediately after treatment is recommendable, and an internal trend memory makes it possible to review and document the patient's reactions during the treatment period. Monitoring is more regularly used in hospitals than in private offices. During endoscopic procedures, which are comparable to short acting unpleasant dental procedures, most endoscopists monitor vital signs before and after the procedure. Moreover, pulse oximetric and electrocardiographic monitoring are in common use. There is a significant relationship between the knowledge of oxygen saturation and the timing of nursing interventions like oxygen or antagonist therapy. Since knowledge of advanced cardiac lifesupport is not common among 2.1.5.2 Monitoring Sugiyama et al (1991) have reported that a pulse oximeter is useful as a respiratory monitor during oral surgery. Patient monitoring is used to detect dangerous deviations from normal in circulation and respiration. Such deviations may be due to therapeutic procedures or to 74 Monitored intravenous sedation with local anaesthesia for dental outpatients Part II endoscopists and gastrointestinal assistants (Keeffe et al. 1989), the use of pulse oximetry in these circumstances is essential (Hinzmann et al. 1992). The experience of the author as well as that expressed in the literature suggests that electronic monitoring is very uncommon in dental practice. However, clinical experience shows that not only a good resuscitation education but also the use of pulse oximetry could increase patient safety in dental offices. Pulse oximeter, oxygen supplement unit and resuscitation facilities were available for the patients in this survey. The author has been educated in the use of endotracheal intubation and the use of medication for cardiopulmonary resuscitation. Probably as a result of the use of pulse oximetric monitoring, there has never been any use for these skills, although the described intravenous method was used long before and after this survey. another; i.e. sedation correlates with respiratory depression. Oxygen was added when the 90% level lasted a long time. The pulse oximeter is valuable because it will react immediately to any progressive oxygen desaturation, making early correction possible. Hence the use of pulse oximetry should be obligatory for all endoscopic or paediatric patients during intravenous sedation (Casteel et al. 1990) and it is also useful as a respiratory monitor during oral surgery (Sugiyama et al. 1991). A pulse oximeter primarily monitors arterial oxygen saturation. This, of course, is an essential safety factor. It also provides a continuous display of pulse rate and, in some advanced pulse oximeters like Ohmeda, also a visible pulse wave on the screen. An internal trend-memory greatly increases the benefit of monitoring. The monitoring period can be reconstructed, printed, analysed and reported. This feature is very valuable in case of complications. A pulse oximeter with these internal features has the first priority among the vital function monitors. These findings are a justification for recommending its use in dentistry and in oral surgery for all patients who are sedated regardless of venous or oral route. Since the largest mean decrease in oxygen saturation observed during procedures under intravenous sedation is less than that considered normal during sleep, some researchers are of the opinion that oximetry monitoring is not needed. Likewise the high incidence of desaturation does not cause adverse outcomes or complications. (Berg et al. 1991, Bilotta et al. 1990) However, in this survey a small decrease of SaO2 was found to be a sign of sufficient sedation during the initiation of medication. This is very understandable because it is more than probable that one central nervous effect correlates with In conclusion, low initial saturation may be a warning signal of hypoxia and the use of a monitor may help to determine the correct sedation level earlier and easier than the normally used ptosis i.e. eye closure reaction. This survey was not a clinical trial: there were differences 75 Monitoring the patients with three pulse oximeter equipments in the underlying factors and no reference group exists. Therefore it is not justified to conclude that low initial oxygen saturation might be a contraindication for sedation or that the sedationist should use the pulse oximeter to estimate the sufficient level of sedation before local anaesthesia. This is mainly a question of clinical experience indicating the need for randomised clinical trial. 76 Monitored intravenous sedation with local anaesthesia for dental outpatients Part II 2.1.6 Clinical conclusions Peroperative pulse oximetric monitoring detects adverse reactions such as hypoxia and high pulse level during intravenous sedation. Low initial oxygen saturation may be a warning signal of hypoxia during sedation. The use of a monitor may help to determine the correct sedation level - when the venous route is used - earlier and easier than the normally used ptosis i.e. eye closure reaction. 77 Monitored intravenous sedation with local anaesthesia for dental outpatients Part II 2.2 Survey 2 Detection of cardiovascular responses to local anaesthesia with Datex Cardiocap multiparameter monitor 2.2.1 ABSTRACT In this survey the cardiovascular effects of two local anaesthetic agents (lidocaine and prilocaine) and two vasoconstrictors (epinephrine and phelypressine) were observed. There were no radical changes in systolic or diastolic blood pressure. The heart rate slightly decreased after the injection of prilocainephelypressine, but increased after the epinephrine-containing lidocaine injection. Both prilocaine- phelypressine and lidocaine- epinephrine injections resulted in statistically significant (p=0.001) changes in heart rate. Amplitude of pulse wave was the most responsive measurable parameter. Amplitude of pulse wave diminished just before and during the injection as a result of psychological stress. The blood flow showed the smallest values during the injection of local anaesthetic. Mean blood oxygen saturation values were within normal limits and the displayed SaO2 values were between 96 - 98 percent during the measuring period in 96 percent of detected values. No cardiovascular problems were found when these preparations were used in combination. Consequently, if the effect of one local anaesthesia preparation is not sufficient it is possible to increase the effect by adding the other preparation without a danger of adverse reactions. safety of epinephrine with dental local anaesthesia is well known. Epinephrine-containing lidocaine has little effect on haemodynamics, while norepinephrine-containing lidocaine causes more changes in the 2.2.2 INTRODUCTION It is important to identify the ideal balance of pain and anxiety relief when anxious patients are treated under intravenous sedation. The 79 Monitoring the patients with three pulse oximeter equipments cardiovascular system (Hirota et al. 1992). Most studies have not noted any severe changes in heart rate or blood pressure when a local anaesthetic is used with epinephrine (Davenport et al. 1990). Montebugnoli et al. (Montebugnoli et al. 1990) found that there were no significant differences in cardiovascular response when a group of patients under non-specific stress were given an anaesthetic with or without epinephrine. The cardiovascular response during dental stress may not be associated with the use of epinephrine in an anaesthetic solution. Individual reactions seem to dominate in certain cases (Montebugnoli et al. 1990, Meyer 1990). injection, but during the real operative procedure the cardiovascular parameters do not correlate with the level of epinephrine derived from the solution of local anaesthetic (Knoll-Kohler et al. 1989). Although there are some changes in cardiovascular parameters, the mean oxygen saturation does not change when local anaesthetics are used (Daublander et al. 1992). Toxic reactions may appear in cases of intravascular injection of local anaesthetics with epinephrine or norepinephrine (Tsirlis and Iakovidis 1989). Bachmann et al. (Bachmann et al. 1988) showed that there is a risk of systemic side effects in experimental infiltration anaesthesia if an amount near but slightly below maximum is used. In this survey, the amount of each agent was 1/3 of the known maximum which is enough to cause cardiovascular changes but far less than enough to induce toxic reactions. Exact reactions in the cardiovascular system caused by local anaesthetics and vasoconstrictors are only partially and controversially documented. Salonen et al. (Salonen et al. 1988) reported that a lidocaineepinephrine solution elevates heart rate but does not affect systolic or diastolic blood pressure. The increase in heart rate is reported to be rare and never by more than 10 beats per minute (Frabetti et al. 1992). However, every clinically experienced dentist knows that sometimes patients will develop unpleasant tachycardia if an anaesthetic containing epinephrine is used. Moreover, other reports show a sharp decrease in the diastolic blood pressure (Montebugnoli et al. 1990, Meyer 1990). Lidocaine with epinephrine has been shown to cause a doubling of the plasma epinephrine concentration two minutes after The aims This experiment was performed with local anaesthetics to differentiate the measurable cardiovascular effects of two commercial local anaesthetics commonly used world-wide, to be able to differentiate the same reactions if sedatives are used with local anaesthetics. Another aim was to find any undesirable cardiac parameters when two commonly used local anaesthetic agents are used in combination. 80 Monitored intravenous sedation with local anaesthesia for dental outpatients Part II Thirdly there was a need to see if the Datex pulse oximeter allows the measuring of changes in amplitude of pulse wave as a result of local anaesthesia. The final aim of this survey was to discover whether local anaesthetic agents and vasoconstrictors have any effects on blood oxygen saturation values when observed with pulse oximetry. 81 Monitoring the patients with three pulse oximeter equipments 2.2.3 PATIENTS AND METHODS measurable findings. Every subject had to come twice to the test on separate days. There were two dropouts who left the study after the first day, thus a total of 38 registration periods were obtained for analysis. During every registration period local anaesthetics was injected into both sides of the upper jaw, hence obtaining 76 injection periods. In one case the test had to be discontinued during the second injection as a result of a sinus tachycardia reaction. 2.2.3.1 Study design This paper is a retrospective descriptive review of follow-up records. It is important to understand that this survey was not a controlled clinical trial but a clinical follow-up of a normal course exercise and a demonstration. Later revised databases formed the study material. Thus there was no indication of approval by an institutional review board governing human experimentation. 2.2.3.3 Local anaesthesia 2.2.3.2 Subjects Local anaesthesia was performed with a lidocaine - epinephrine solution (Xylocain adrenalin 1.8 ml inj. 20 mg/ml+12.5 mcg/ml ASTRA) and prilocaine - phelypressine solution (Citanest Octapressin 1.8 ml inj. 30 mg/ml+0.54 mcg/ml ASTRA). The site of injection was the upper jaw, the buccal sulcus just distal of the second upper molar. Both sides of the maxilla were anaesthetised. This site was chosen because there is room for a large enough volume of local anaesthetic, and the trifurcation of the trigeminal nerve is near the anaesthetised area. The study group consisted of twenty dental students. The students were between 19 and 31 years of age with a mean age of 22 years (SD 3); 80 % were females. Each person accepted in the test group had to be healthy and free of any surgical risk, corresponding to the ASA (American Society of Anaesthesiologist) I or II groups. Oral contraceptives were the commonest medication (three of females). One subject was undergoing a thyroxin substitution therapy for hypothyreosis. No other illness or permanent medication was reported. Patients were in a horizontal position during the infiltration of local anaesthetic. The survey was done during a normal local anaesthesia course for students. This provided an opportunity to allow the students to practice local anaesthesia, to demonstrate cardiovascular effects thereto and to collect objective 82 Monitored intravenous sedation with local anaesthesia for dental outpatients Part II time taken for the injection of the 4 cartridges was 2 min 11 seconds (SD 24.6 seconds) (Table 1). 2.2.3.4 Timing of the procedure During the first appointment (method 1), the subjects received 4 cartridges (4 x 1.8 ml) of CitanestOctapressin, corresponding to 216 mg of prilocaine and 3.89 mcg of phelypressine, injected submucosally 5 minutes after beginning the pulse oximetric measurement. The area of injection was the upper right buccal sulcus. Ten minutes later they received a similar injection to the left side of the maxilla, but the local anaesthetic this time was Xylocain adrenalin. The dose was also 4 x 1.8 ml. The amount of anaesthetic corresponded to 144 mg of lidocaine and 90 mcg of epinephrine. The mean During the second appointment (method 2) after two days wash-out, the subjects received two cartridges of Citanest-Octapressin to the right side and two cartridges of the same agent to the left side 5 minutes after beginning the pulse oximetric measurement. Ten minutes later, they received two cartridges of Xylocain adrenalin to both sides of the maxilla, so every subject had two measuring sessions. The injection sites were the same in both sessions (Table 2). 83 Monitoring the patients with three pulse oximeter equipments Table 1. Timing of the procedure with each patient in method 1: Preparations injected into separate areas Time(min) 0 min start of measurement 5 min onset of injection into right upper jaw, 4 cartridges of Citanest- Octapressin 15 min initiating injection into left upper jaw, 4 cartridges of Xylocain adrenalin 25 min end of measurement Two days wash-out before method 2 Table 2. Timing of the procedure with each patient in method 2: Both preparations injected into same areas. Time (min) 0 min start of measurement 5 min onset of the first injection: 2 cartridges of Citanest-Octapressin into both sides of maxilla (total 4 cartridges) 15 min initiating the second injection: 2 cartridges of Xylocain adrenalin into both sides of maxilla (total 4 cartridges) 25 min end of measurement 84 Monitored intravenous sedation with local anaesthesia for dental outpatients Part II flow in the finger is the result of left ventricle contraction of the heart, which fills the vascular bed of the finger with arterial blood. It is important to understand that the pulse wave reflects changes in blood volume, not changes in blood pressure. 2.2.3.5 Monitoring Subjects were monitored using a CARDIOCAP II CH-S (Datex, Helsinki Finland) multiparameter physiological monitor. This pulse oximeter is a stand-alone, noninvasive, arterial oxygen saturation monitor which can monitor ECG and blood pressure. It gives continuous, real-time SaO2 and pulse rate readings. Follow-up information is available through both the analog and digital output ports. The monitor was connected directly to the serial port of a Toshiba T1000SE portable computer for realtime collection of data by a collection program ("KERÄÄ" by Dr Matti A.K. Mattila). The program recorded numerical values from Cardiocap at 10 seconds intervals. The pulse oximetric equipment works using light which is generated in the finger probe and passes through the tissues. The total absorption of the light depends on the absorbing components: tissues, venous blood and the pulsating arterial blood. Different amounts of light are absorbed by oxygenated haemoglobin (HbO2) and unoxygenated or reduced haemoglobin (Hb). The oximeter measures the relative absorption by Hb and HbO2 of red light at 660 nm and infrared light at 910 nm. These two different forms of haemoglobin allow different amounts of light to pass through at these wave lengths. The oximeter converts this relative light intensity information into arterial oxygen saturation values. Blood pressure was measured automatically every two minutes from the subjects' left upper arm. A finger probe was used for pulse oximetric registration, i.e. blood oxygen saturation (SaO2). The probe was placed on the subject's right middle finger. The data from the Cardiocap were further analysed using at first the Microsoft Works-2 and MedStat programs and the previously mentioned Toshiba AT personal computer. 2.2.3.6 Statistical methods The total of 6840 numerical values of pulse, amplitude of pulse wave, systolic and diastolic blood pressure and oxygen saturation of blood were first reduced to averages for each minute and for the five-minute pretreatment period (0-4 min), and for two ten-minute periods after the first and the second injections (5-14 min; 15-24 min). The pre-treatment five- The pulsation of the arterial blood flow modulates the light passing through it, and the oximeter converts this light intensity information into pulse rate values, which are presented together with SaO2 values on a monitor screen. The pulse wave is derived from the intensity of the transmitted light. The pulsating blood 85 Monitoring the patients with three pulse oximeter equipments minute average was used as a baseline value. Pre-treatment baseline-values were compared between method 1 and 2 using paired t-test. To test whether the site of the injection had any effect (method 1 vs. method 2), the twentyminute averages (5-24 min) were calculated and tested using paired ttest. The data were analysed using STATISTICA (StatSoft, Tulsa, USA). Analysis of variance (ANOVA) for repeated measurements was applied using the successive periods 0-4 min, 5-14 min and 15-24 min. In cases where the ANOVA gave a significant (p<0.05) result, paired contrasts were made in order to identify which injections accounted for the significant overall p-value. 86 Monitored intravenous sedation with local anaesthesia for dental outpatients Part II 2.2.4 RESULTS minute (p=0.0004, 2 to 5) in method 1 and method 2 respectively. Then, after the second injection the heart rate increased 6 beats per minute (p<0.0001, 4 to 8) and 10 beats per minute (p<0.0001, 6 to 13) during method 1 and 2 respectively (Table 3). 2.2.4.1 Pulse At the beginning of the measurement, the heart rate was quite stable. After the first injection (prilocaine and phelypressine), the heart rate slightly decreased in both methods. The injection with lidocaine - epinephrine (Xylocain adrenalin) increased the heart rate, because of the epinephrine. In method 2, when both preparations were injected into the same areas, the results were very similar to those in method 1, where injection areas were separated. After the second injection (lidocaine epinephrine), the heart rate increased faster with method 2 than with method 1, but heart rate levels were very similar. Towards the end of the measurement, the heart rate increased about 10/min from base level in both methods. However, a prilocainephelypressine combination (CitanestOctapressin) affects the cardiovascular system less than a lidocaine-epinephrine combination (Xylocain adrenalin). The results of heart rate measurements are presented in Fig. 1. The two days with methods 1 and 2 were comparable with respect to the baseline values (0-4 min). During the 24-minute periods, heart rates changed significantly (p<0.0001, ANOVA of repeated measurements). Compared to the baseline, the heart rate decreased after the first injection approximately 4 beats per one minute (p<0.0001, 95% confidence interval 3 to 6 beats per one minute) and 4 beats per 2.2.4.2 Amplitude of pulse wave Amplitude of pulse wave was the most impressionable of the measurable parameters during the survey. (Fig. 2) Amplitude of pulse wave observations are subject not only to biologic and measurement variation but also to temporal variation in clinical circumstances. Standardising the circumstances to reduce the environmental variation (e.g. room temperature) was not possible during a local anaesthesia course, and therefore the findings should be regarded as tentative. Blood flow showed the smallest values during and immediately after the injection of local anaesthetic in both methods. In baseline blood flow levels there was a considerable difference (p=0.02) between days. The difference in baseline-levels, decrease of 8 units, can be interpreted as the consequence of reduced stress. During the first session, employing method 1, no significant changes in blood flow could be observed. During the second session, employing method 2, the blood flow level differs 87 Monitoring the patients with three pulse oximeter equipments significantly across time (p=0.0001, ANOVA of repeated measurements). After the first injection the blood flow decreased 9 units (p=0.005, 95% confidence interval 3 to 15) compared to the baseline. After the second injection, the level of blood flow further decreased by 6 units (p=0.01, 2 to 10). The total effect of the two injections was approximately 15 units (p=0.002, 6 to 23) compared to the baseline (Table 3). 2.2.4.4 Oxygen saturation of blood (SaO2) Oxygen saturation slightly decreased towards the end of the measurement period, but so marginally that the differences caused by injections or methods were less than one percent. (Fig. 5) During the first session, however, the level of oxygen saturation decreased statistically significantly (p=0.04, ANOVA of repeated measurements). This significant result was caused by the difference between baseline level and the level after the second injection (p=0.05). This finding, although statistically significant, has no clinical significance. The mean saturation values after the first injection varied between 94 % and 98.8% and 95.7 % and 98.5 %, during methods 1 and 2 respectively (Table 3). 2.2.4.3 Blood pressure There were no clinically or statistically significant changes in systolic (Fig. 3) or diastolic (Fig. 4) blood pressure in either of the study methods (Table 3). It seems that the local anaesthetics used in this survey only have a very small effect on blood pressure when used lege artis in dentistry, although the doses used were considerable. 88 Monitored intravenous sedation with local anaesthesia for dental outpatients Part II Figures 1 – 5. Cardiovascular responses after local anaesthesia are presented below. Fig 1. Pulse 90 PULSE (1 min) 85 80 75 70 prilocainphelypressin 65 lidocain epinephrine Method 1 Method 2 60 0 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 MINUTES Fig 2. Amplitude of pulse wave AMPLITUDE OF PULSE WAVE 45 40 35 30 25 20 15 10 5 lidocain epinephrine prilocainphelypressin Method 1 Method 2 0 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 MINUTES 89 Monitoring the patients with three pulse oximeter equipments SYSTOLIC BLOOD PRESSURE (mmHg) Fig 3. Systolic blood pressure 130 125 120 115 110 105 100 95 90 85 80 75 70 65 lidocain epinephrine prilocainphelypressin 1 2 4 6 8 10 12 14 16 Method 1 Method 2 18 20 22 24 MINUTES DIASTOLIC BLOOD PRESSURE (mmHg) Fig 4. Diastolic blood pressure 130 125 120 115 110 105 100 95 90 85 80 75 70 65 prilocainphelypressin 1 2 4 6 Method 1 Method 2 lidocain epinephrine 8 10 12 14 MINUTES 90 16 18 20 22 24 Monitored intravenous sedation with local anaesthesia for dental outpatients Part II BLOOD OXYGEN SATURATION (SaO2) Fig.5. Blood oxygen saturation 98 97 prilocainphelypressin lidocain epinephrine Method 1 Method 2 96 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 MINUTES 91 Monitoring the patients with three pulse oximeter equipments Table 3. Cardiovascular responses during the follow-up of 24 minutes. Prilocaine-phelypressine was injected five minutes after starting the follow-up, and lidocaine-epinephrine ten minutes later. Method 1 = subjects received prilocaine-phelypressine injections in the right upper jaw and lidocaine-epinephrine injections in the left side. Method 2 = two days later the same subjects received prilocaine-phelypressine injections in both sides of the upper jaw and lidocaine-epinephrine injections in the same areas. Method Before anaesthesia (0-4 min.) After prilocaine (5-14 min.) After lidocaine (15-24 min.) Effects of agents Difference of methods Mean SD Mean SD Mean SD p-value* p-value** Pulse 1 79.2 15.2 74.8 14.3 80.9 14.1 <0.0001 ab 2 77.5 12.5 74.0 11.5 83.6 9.8 <0.0001 abc 0.74 SaO2 1 97.3 0.8 97.2 0.7 97.1 0.7 0.04 c 2 97.2 0.5 97.2 0.5 97.2 0.5 0.94 0.84 A.P.W. 1 27.8 28.7 26.0 22.3 23.3 18.5 0.25 2 36.3 29.7 27.3 22.1 21.5 17.5 0.0001 abc 0.73 Syst. BP 1 125.0 10.3 125.0 12.2 124.4 11.8 0.71 2 122.8 8.7 122.6 8.8 123.5 8.7 0.66 0.73 Diast. BP 1 86.8 8.3 86.6 8.0 86.3 7.3 0.60 2 85.3 6.6 85.7 7.0 85.6 6.6 0.08 *) ANOVA of repeated measurements. Significant (p<0.05) contrasts are between: a) 0-4 min vs. 5-14 min. b) 5-14 min vs. 15-24 min. c) 0-4 min vs. 15-24 min. **) Paired t-test to compare method 1 vs. method 2 (5-24 min) 92 0.79 Monitored intravenous sedation with local anaesthesia for dental outpatients Part II 2.3.5 DISCUSSION patients undergoing surgical removal of a third molar with local anaesthesia experienced hypoxic periods during surgery. Breath holding was suggested to be responsible for the observed falls in SaO2. Their conclusion was that other types of dental care which cause breath holding or restrict the upper airway may also cause changes in SaO2 levels. 2.3.5.1 Amplitude of pulse wave and the measuring equipment The regulation of peripheral arterial circulation is in the control of the autonomic nervous system. Vasoconstriction is induced by the stimulation of the smooth muscles of arterioles. This decreases the amplitude of the pulse wave and may be due to some discomfort such as pain, fear, low temperature or hypovolaemia. Rapid and strong vasodilatation is often seen after the injection of a sedative agent, as a result of feeling good. The amplitude of the pulse wave is the most informative indicator of changes in circulation, and CARDIOCAP II CHS allows us to observe this parameter. Hypoxia may also be related to underlying medical problems (White et al. 1989). A considerable portion of these desaturations might be due to patient movement or movement of the photodetector probe. Wilson (Wilson 1990) found that 87 % of the desaturations in child patients under sedation resulted from patient movement. 2.3.5.2 Oxygen saturation of blood during dental treatment There is some evidence that even unsedated patients develop small postoperative falls in oxygen saturation (Matthews et al. 1992). The study by White et al. (White et al. 1989) showed that nearly half of the patients developed clinically significant desaturation during minor oral surgery under local anaesthesia. White et al. assumed that this might be due to breath holding or peripheral vasoconstriction as a response to anxiety or fear. Moreover, the influence of local anaesthetics on oxygen saturation is not clear. In this survey, the saturation values were not more than 0.5 % lower at the end of the measurement than the base level. The displayed readings also stayed stable between the values of 96 and 98% during the test period. We may conclude that local anaesthesia is not a possible source of measuring failures, and that the agents used in local anaesthesia do not affect the level of the patients' oxygen saturation. Lowe and Brook (Lowe and Brook 1991) noticed that one fifth of the 2.3.5.3 Toxic reactions 93 Monitoring the patients with three pulse oximeter equipments (Gortzak et al. 1992a) studied subjects during routine restorative dental treatment and found that patients showed considerable blood pressure variation. Those treated without local anaesthesia showed a significant mean blood pressure increase, while patients treated under local anaesthesia with articaine showed no significant changes in blood pressure during treatment. Cioffi et al. (Cioffi et al. 1985) concluded that routine restorative dental care with lidocaine and epinephrine local anaesthesia did not produce clinically important haemodynamic responses despite an increase in epinephrine levels. Too large plasma concentrations of a local anaesthetic may result in toxic reactions. Systemic toxicity may occur either in the presence of excessive volumes of anaesthetic or during inadvertent intravascular injections (Fiset et al. 1985). In this survey, the amount of each agent was one-third that of the known maximum, which is enough to cause cardiovascular changes but far too little to induce toxic reactions. Also, slow biotransformation or elimination may be the cause of toxic reactions in some patients. Those with decreased renal function or with advanced liver disease are at risk of the accumulation of anaesthetic or its by-products (Laskin 1984). The unpleasant subjective experiences (CNS effects) reported by the subjects in this survey after the administration of local anaesthetics were not seen as measurable registrations in pulse oximetry or in blood pressure values. This is at variance with the view that blood pressure and heart rate should be seen as unreliable indices of the onset of systemic local anaesthetic toxicity (Pateromichelakis 1992). Moreover, it is possible to reduce the amount of one local anaesthetic agent using a combination of two agents, which will even enhance the effect (Luotio et. al 1997). Frabetti et al. (Frabetti et al. 1992) found that patients undergoing surgical treatment had higher heart rate values than patients undergoing conventional therapy. Patients undergoing muco-gingival surgery had the mean heart rate values of one hundred per minute, while the group undergoing scaling had the mean heart rate values of 78 beats per minute. In this survey, the mean pulse rate of the patient rose from 70 to 86 beats per minute after the injection of local anaesthetics containing epinephrine. Meyer (Meyer 1987) also found that the increases in heart rate and alterations of blood pressure were different in a group undergoing extraction from a group to whom local anaesthesia only had been administered, and these differences are possibly rather an expression of an endogenous catecholamine release as a result of stress than a pharmacological effect. He also concluded that endogenous 2.3.5.4 Pulse and blood pressure after local anaesthesia Considerable controversy exists in the literature regarding the haemodynamic changes caused by local anaesthetics. Gortzak et al. 94 Monitored intravenous sedation with local anaesthesia for dental outpatients Part II alternations always take place in the same way. It has also been found that there is a temporary blood pressure increase during the injection of local anaesthetic (21,19) and at the time of extraction of a tooth (Meyer 1987). Also, the heart rate had two peak values during the extraction of the tooth: the first during the injection of the local anaesthetic, and the second during the extraction phase (Meyer 1987). There may also be some increase in systolic blood pressure (Gortzak et al. 1992a). However, no clinically significant change could be detected in either systolic or diastolic blood pressure. during a normal local anaesthesia course for students. There were differences in the underlying factors i.e. the survey was non-randomised: the order of the injections of lidocaine and prilocaine were the same in both methods; external conditions were not constant because there was even a difference in the base level of the stress between the methods which were performed in separate days without randomization. Moerover, the order of methods 1 and 2 was not randomized. This causes the problem that a comparison of methods 1 and 2 is not valid. Therefore it is not justified to conclude that one method of local anaesthesia is better than another. However, this survey showed that the common clinical practice to combine different local anaesthetic agents do not obviously harm a healthy patient. It may be concluded that no reasons to avoid the combination of lidocaine and prilocaine were found. However, the study design was very complex because this was not a clinical trial but a monitory period 95 Monitored intravenous sedation with local anaesthesia for dental outpatients Part II 2.3.6 Clinical conclusions Changes in pulse rate were possible to detect with pulse oximetry: Heart rate slightly decreased after the injection of prilocaine with phelypressine, but pulse rate increased after the epinephrine-containing lidocaine injection. There is no reason to avoid the combination of lidocaine and prilocaine, if needed, because no increase in a non-desired effect can bee seen. Consequently, if the effect of one local anaesthesia preparation is not sufficient it is possible to add the other preparation. Amplitude of pulse wave was the most reactive parameter during injection. Local anaesthesia does not affect blood oxygen saturation to a degree that should be taken into account clinically. 97 Monitored intravenous sedation with local anaesthesia for dental outpatients Part II 2.3 Survey 3 Detection of maximal pulse and amplitude of pulse wave under intravenous sedation with a Datex Sattlite Trans pulse oximeter 2.3.1 ABSTRACT In this survey 26 registrations of 26 patients were monitored with pulse oximeter during major or long-standing dental operation under intravenous sedation with local anaesthesia. This survey was not a controlled clinical trial but normal treatment periods and a clinical follow-up with pulse oximeter. Later revised databases formed the survey material (retrospective review of patient records). The cardiovascular effects of benzodiazepine (midazolam) and the local anaesthetic agent (lidocaine) and vasoconstrictor (epinephrine) were observed. Pulse rate increased both during and after the injection of midazolam as well as epinephrine containing lidocaine injection. The increase was very slight after midazolam but after local anaesthesia it was notable. As a result of stress relief, pulse rate was lower after the treatment than before it (p<0.05). The highest level of pulse level was recorded during local anaesthesia (p<0.005). There was no significant difference in pulse rate before treatment, during sedation and during treatment. During the retrospective review of patient records, amplitude of pulse wave (A.P.W.) was the most responsive measurable single parameter indicating stress. In general A.P.W. decreased towards the injection due to psychological stress. Blood flow showed decreasing values during and after injections of local anaesthetic. Moreover, poor A.P.W. caused measuring artefacts into the levels of blood oxygen saturation, which can be avoided by covering the patients with a blanket. The nature of this descriptive parameter is discussed. 99 Monitoring the patients with three pulse oximeter equipments 2.3.2 INTRODUCTION 2.3.2.2 Local anaesthesia 2.3.2.1 Monitored sedation Epinephrine containing lidocaine has little effect on haemodynamics (Hirota et al. 1992). Most study groups have not noted significant changes in heart rate or blood pressure if local anaesthetic is used with epinephrine (Davenport et al. 1990).The increase in heart rate is reported to be rare and never by more than 10 beats per minute (Frabetti et al. 1992). Cardiovascular parameters have been documented to increase as early as after the one minute waiting period after injection; after two and three minute waiting periods the increases were far less pronounced (Daublander et al. 1992). Lidocaine with epinephrine has shown to cause a doubling of the plasma epinephrine concentration two minutes after injection, but during the treatment procedures which cause emotional stress, the cardiovascular parameters do not correlate with the level of epinephrine derived from the solution of local anaesthetic (Knoll-Kohler et al. 1989). However, every clinically experienced dentist knows that patients sometimes develop unpleasant tachycardia reactions if epinephrine containing anaesthetic is used. In dental practice monitors are still extremely seldom used despite the fact that simple and low-cost technical solutions, such as pulse oximeters, already exist. The pulse oximeter primarily monitors arterial oxygen saturation, which is of course an essential safety factor. Secondarily a continuous display of pulse rate is obtained and in some advanced pulse oximeters also a visible pulse wave on the screen. The information of the pulse wave can be widely utilised in the monitoring of circulation and patient's reactions to pain and discomfort. The correct monitor should, however, be selected on the basis of the essential needs in each particular situation and circumstances. The methodology of the early detection of hypoxia with pulse oximeter during intravenous sedation has been previously described by the author. Intravenous sedation with midazolam causes a statistically significant but physiologically insignificant fall in arterial blood oxygenation, as measured by pulse oximetry (Matthews et al 1992). Desaturation slightly below 90% may be clinically insignificant since no complications have been noted (Berg et al. 1991 and Bilotta et al. 1990) but because patients at risk for hypoxaemia cannot be predetermined it is recommended that the patients be monitored with a pulse oximeter (McKee et al. 1991). 100 Monitored intravenous sedation with local anaesthesia for dental outpatients Part II because they are very similar in shape. Their information is, however, totally different. A visible pulse wave means practically that blood is circulating at the site of measurement. During normal sinus rhythm consecutive pulse waves are uniform, but during arrhythmia they can continuously vary in size and shape. In fact, these observations can be applied also to evaluate the importance of that particular arrhythmia for circulation (Mattila et al 1989, Mattila 1990). 2.3.2.3 Amplitude of pulse wave (A.P.W.) Observing the A.P.W. enables the dentist to notice constriction in the peripheral arteries as a result of psychological stress: The blood flow of the finger shows diminishing values before the injection of local anaesthetic i.e. before any possible cardiovascular effect. A pulse oximeter probe is usually placed on a finger; other alternatives are toes or earlobes. These alternative locations are equally suitable as a finger when measuring oxygen saturation and pulse rate, but they do not indicate the reactions in the pulse wave amplitude. In general, peripheral arteries in fingers react to painful stimuli much stronger than arteries in other places (Mattila et al 1990). 2.3.2.4 Aim of the study The background for this survey has been a necessity to find the ideal relation of pain and anxiety relief when anxious patients are treated under intravenous sedation with local anaesthesia. Quite naturally, the absorption of infrared light is relative and dependent on the thickness of the finger, being different in individual fingers. Consequently, the reliability of the pulse wave amplitude recording requires that the recording site is not changed. Because of the relativity of amplitude it is important to have a basis for comparison (Mattila et al 1989). In practice this means that when monitoring sedation, the recording should be started before cannulation. Some confusion seems to exist between direct arterial blood pressure and visible pulse wave The aim of this retrospective review of patient records was to evaluate the effect of intravenous sedatives and local anaesthetic agents with vasoconstrictors to pulse rate and amplitude of pulse wave when observed with pulse oximetry. Another reason for this article was the need to describe some false alarms of the oxygen saturation of blood during intravenous sedation, and find explanations thereto. 101 Monitoring the patients with three pulse oximeter equipments 2.3.3 PATIENTS AND METHODS The program recorded numerical values from SATLITE at every 10 seconds. A finger probe was used for pulse oximetric registration i.e. blood oxygen saturation (SaO2). The probe was placed to the patient's right middle finger. The data from Cardiocap was further analysed using the Microsoft Works-2 and MedStat programs and the above mentioned computer. 2.3.3.1 Study design This survey is a retrospective descriptive review of patient records. There were many differences between patient preparation, cannulation and intravenous infusion as well as local anaesthesia, i.e. in the underlying factors. It is important to understand that this survey was not a controlled clinical trial but a clinical follow-up of normal treatment periods. Later revised databases formed the survey material. During the treatments there was no survey design to answer any particular question. Thus there was no indication of approval by an institutional review board governing human experimentation. 2.3.3.3 The working principle of the Datex pulse oximetric equipment Light is generated in the finger probe and it passes through the tissues. The total absorption of light can be derived into absorbing components: tissues, venous blood and the pulsating arterial blood. Different amounts of light are absorbed by oxygenated haemoglobin (HbO2) and unoxygenated or reduced haemoglobin (Hb). The oximeter measures the relative absorption of red light at 660 nm and infrared light at 910 nm by Hb and HbO2. These two different forms of haemoglobin allow different amounts of light to pass at these wave lengths. The oximeter converts this information on relative light intensity into arterial oxygen saturation values. 2.3.3.2 Monitoring During the measuring, patients were monitored with SATLITE TRANS TM (Datex, Helsinki Finland). This pulse oximeter is a stand-alone, non-invasive, arterial oxygen saturation monitor which can also monitor ECG and blood pressure. It gives continuous, realtime SaO2 and pulse rate readings. Follow-up information is available through both the analog and digital output ports. The monitor was connected directly to the serial port of Toshiba T1000 SE portable computer for the real-time collection of data by a collection program. The pulsation of the arterial blood flow modulates the passing light. The oximeter converts this light intensity information into pulse rate values which are presented by SaO2 value 102 Monitored intravenous sedation with local anaesthesia for dental outpatients Part II on a monitor screen. The pulse wave is derived from the intensity of transmitted light. The pulsating blood flow in the finger is the result of left ventricle contraction of the heart which fills the vascular bed of the finger with arterial blood. It is important to understand that the pulse wave-form reflects changes in blood volume, not changes in blood pressure. laboratory blood evaluations (B-Se, B-Hb, B-leuk, fB-glu). The patients were advised both verbally and in writing on how to prepare for intravenous sedation (for example, no food or drink for four hours prior to treatment).They were in good health and had no severe systemic diseases (in the classification of American Society of Anaesthesiology ASA I - II i.e. no systemic diseases or only a moderate disease which does not limit activity). 2.3.3.4 Patients Patients were not given oral premedication, sedatives nor antibiotics on the day of the operation or the previous day. Blood pressure was recorded and monitoring with a pulse oximeter initiated before the insertion of a peripheral venous cannula. After the insertion of the cannula, an infusion of 0.9% sodium chloride solution was started, and then the sedative agent was applied with disposable syringe using the slow injection technique (Table 1). The treatment room was equipped with dental unit, pulse oximeter, oxygen supplement unit and some resuscitation facilities, including endotracheal intubation equipment and medication for cardiopulmonary resuscitation. All treatments were carried out by the same dentist, i.e. the author. This retrospective review of patient records comprised 26 registrations of 26 of the author's private outpatients who underwent dental operations under intravenous sedation with local anaesthesia. The survey was carried out between October 1993 and February 1994 and included all the patients treated under intravenous sedation with local anaesthesia at the clinic during that period of time. Patients were 16 (62%) males and 10 (38%) females. Mean age was 42 years SD 15 years. The patients had some oral surgical operations or they underwent large conservative dental treatment or extraction under sedation because of dental care phobia. During the first examination, the patients completed a questionnaire about previous and present illnesses, allergies and medications. A dental care plan was drawn up and all the patients were referred to radiological examination (orthopantomography). All the patients who underwent major surgical operation e.g. sinus-lift procedure, were also referred to 2.3.3.5 Sedation Midazolam was used for sedation (Dormicum 5 ml inj. 1 mg/ml Roche), with mean amounts 5.02 mg SD 1.72 mg. Table 2 presents the doses of the agents used. 103 Monitoring the patients with three pulse oximeter equipments in the dental chair, and pulse oximetric monitoring was continued until bleeding after extraction had stopped and until the patients felt well and were able to walk and get dressed without help. The patients left the clinic with an adult escort. Fentanyl (Fentanyl 2 ml inj. 50 microgram/ml Orion R) was not used for additional pain relief preoperatively, only in 1 case for analgesia postoperatively (0.05 mg). (Table 2) Local anaesthesia was performed with a lidocaine-epinephrine combination (Xylocain adrenalin 1.8 ml inj. 20 mg/ml + 0.0125 mg/ml, ASTRA, mean 155 mg SD 54.3 mg lidocaine and 0.097 mg SD 0.034 mg epinephrine) and a prilocainephelypressine combination (Citanest Octapressin 1.8 ml inj. 30 mg/ml+0.54 microgram/ml ASTRA, mean 203 mg SD 118 mg prilocaine and 0.0036 mg SD 0.0021 mg). 2.3.3.6 Statistical methods Paired t-test was used to compare maximal pulse readings during different parts of the survey. Changes in maximal pulse from baseline, and from the previous part of the survey were described as means and 95% confidence intervals. Fisher's exact test was used to study the association between room temperature (covered/uncovered patient) and amplitude of pulse wave (satisfactory/unsatisfactory p.b.f). The data were analysed using SPSS statistical package (Version 6.1.3). After treatment, most of the patients (16 cases) received 30 mg ketorolak (Toradol inj. 30 mg/ml, Syntex) injection for analgesics via venous cannula. Blood pressure was recorded again and the venous cannula removed. The patients stayed 104 Monitored intravenous sedation with local anaesthesia for dental outpatients Part II Table 1. The treatment was divided into five periods as described in this table. The maximal pulse rate was determined during every period. Treatment periods in which cardiovascular parameters were observed. Name of period Description Duration 1. Waiting (Before) Patient in the chair before cannulation 5 - 10 minutes 2. Sedation After cannulation but before local anaesthetic injections 5 - 10 minutes 3. Local anaesthesia Injections of local anaesthetic agents 5 - 10 minutes 4. Treatment Operative period: incisions, drilling, extraction, sealing, fillings, etc. 15 - 120 minutes 5. After Intravenous-cannula removed, patient still in the chair Table 2. The premedications used in this survey. Quantity of the agents is expressed in milligrams and local anaesthetics also in 1.8 ml ampoules (in brackets). Medication No. of patients Mean Midazolam (mg) 26 5.02 Lidocaine (mg) 26 155 (4.31) Prilocaine (mg) 17 203 (3.76) 105 SD 1.72 54.3 118 Monitoring the patients with three pulse oximeter equipments 2.3.4 RESULTS per minute, SD 14.4, p<0,001) as a result of stress relief (Tables 4-6). 2.3.4.1 Maximal pulse rate Pulse alone was a good indicator for stress but the maximal pulse rate during a period reflects the highest discomfort better. There were no considerable differences between the waiting period (89.8 beats per minute, SD 14.4), the sedation period (91.3 SD 13.6), and the treatment period (91.4 SD 11.5) compared to pulse measurements recorded during the waiting period before cannulation: 89.8 beats per minute (Table 4). As a conclusion, maximal pulse rates before operation, during sedation and during treatment were constant but were increased by local anaesthesia and decreased by the end of the procedure. 2.3.4.2 Amplitude of pulse wave (A.P.W.) A.P.W. will rise after the injection of benzodiazepine and afterwards the local anaesthesia will cause some vasoconstriction. A single dose of benzodiazepine produced effective vasodilatation which remained for 45 minutes (fig 2). In general, P.B.F decreased towards the injection due to psychological stress. The blood flow showed decreasing values during and after the injections of local anaesthetic. Maximal pulse rate increased slightly both during and after the injection the midazolam, but after the epinephrine containing lidocaine injection the increase from base level was notable (8.8 beats per minute, p<0.005, Table 5, Fig. 1). Injection with lidocain epinephrine (Xylocain-adrenalin) increased the heart rate because of epinephrine. The heart rate increased about 10/min from base level (Tables 5 and 6). The effect of low room temperature to the A.P.W. was notable. The difference in A.P.W. between the patients who were covered with a blanket and the patients who were not is both clinically and statistically significant. (p=0.07 using Fisher’s exact test, Table 3). The higher pulse level was detectable for 20 minutes although the injection period for local anaesthesia only took 10 minutes (Fig 3). During the treatment period itself the pulse rate decreased into the level of 91.4 (SD 11.5). Moreover, maximal pulse rates were lower after the treatment (80.8 beats per minute, SD 13.2) than before it (89.8 beats 106 Monitored intravenous sedation with local anaesthesia for dental outpatients Part II Table 3. The effect of low room temperature to the amplitude of pulse wave (A.P.W.). Covered patients 1. satisfactory A.P.W. 2. unsatisfactory A.P.W. Total feel cold. Low temperature has also closing effect in A.P.W. and this may often cause measuring failures because of low signal. Thus pulse oximetric measuring works properly only in cases where the patient has comfortable conditions. Figure 4 combines the patients whose A.P.W. was under 20 (in relative scale) all the time. The upper line presents the measured SaO2. There is a great amount of artefacts (*) on this line. An artefact is described as an extensive fall in SaO2 readings without any organic reasons such as breathing failure or obstructed airways. Good A.P.W. allows the right detection of SaO2 during the sedation and treatment period (Fig. 5). Uncovered Total patients 12 (92%) 7 (54%) 19 1 (8%) 6 (46%) 7 13 (100%) 13 (100%) 26 13 patients were covered with a blanket an 13 were not. The decision to cover the patient with a blanket or not was not based on a randomisation, the dentist only realised that some of the patients felt cold. Therefore all the uncovered patients had their treatment earlier than the covered patients. This vasoconstriction occurs if the treatment is carried out in a cool operation room where patients may 2.3.4.3 Other observations False alarms were observed during momitoring as represented in fig 4. 107 Monitoring the patients with three pulse oximeter equipments Fig 1. Pulse rate in the different stages of treatment. The boxplots are formed from "boxes", which contain 50% of the values falling between the 25th and 75th percentiles, and the "whiskers", lines that extend from the box to the highest and lowest values, excluding outliers. A line across the box indicates the median. (Four patients were excluded from this figure because of missing values.) P u ls e 120 110 100 90 80 70 60 50 N= 22 B e fo r e 22 S e d a tio n 22 L o c a l a n e sh t. 22 T r e a tm e n t 22 A fte r T r e a tm e n t p e r io d Table 4. Maximal pulse values during the survey Before Sedation Mean 89.8 91.3 98.6 91.4 80.8 SD 14.4 13.6 12.5 11.5 13.2 72.8-121.8 72.8-113.4 54.6-105.0 Range 64.4-120.4 71.4-116.2 Local anaesthesia Treatment After 108 Monitored intravenous sedation with local anaesthesia for dental outpatients Part II Table 5. Maximal pulse. Changes from baseline. Change from baseline (=before) to Mean SD 95% confidence interval p-value* Sedation +1.5 10.2 -2.6 to +5.6 0.46 Local anaesthesia +8.8 8.8 +5.2 to +12.3 <0.001 Treatment +1.6 11.7 -3.2 to +6.3 0.50 After -9.0 11.9 -13.8 to -4.2 0.001 *) paired t-test Table 6. Maximal pulse. Changes from the previous part of treatment. Change from previous part of treatment Mean SD 95% confidence interval p-value* Baseline to sedation +1.5 10.2 -2.6 to +5.6 0.46 Sedation to local anaesthesia +7.2 9.1 +3.6 to +10.9 <0.001 Local anaesthesia to treatment -7.2 6.6 -9.9 to -4.5 <0.001 -10.6 7.6 -13.6 to -7.5 <0.001 Treatment to after *) paired t-test 109 Monitoring the patients with three pulse oximeter equipments Fig 2. Pulse rate (A) and amplitude of pulse wave (B) after the injection of midazolam. The figure consists of five (n=5) patients. Only the cases in which the quality of detections was most excellent were accepted to this figure. These five measurements are in combination so that the injections of midazolam occur at the same time; two minutes after beginning i.e. at the left corner of the 60 minutes scale. The line itself is the mean of the five registrations. PULSE RATE A 100,0 90,0 80,0 70,0 60,0 50,0 40,0 30,0 20,0 10,0 0,0 Injection of sedative agent sedation local anesthesia treatment 0 MIN < TIME IN MINUTES > 60 MIN AMPLITUDE OF PULSE WAVE B 100,0 90,0 80,0 70,0 60,0 50,0 40,0 30,0 20,0 10,0 0,0 Injection of sedative agent sedation local anesthesia treatment 0 MIN < TIME IN MINUTES > 60 MIN 110 Monitored intravenous sedation with local anaesthesia for dental outpatients Part II Fig 3. Pulse rate (A) and amplitude of pulse wave (B) after local anaesthesia with lidocaine - epinephrine. The figure consists of five (n=5) patients. Only the cases in which the quality of detections was most excellent were accepted to this figure. These five measurements are in combination so that the first injections of lidocaine - epinephrine occur at the same time; two minutes after beginning i.e. some millimetres from the left corner of the 30 minutes scale. The line itself is the mean of the five registrations. PULSE RATE A 100,0 90,0 80,0 70,0 60,0 50,0 40,0 30,0 20,0 10,0 0,0 0 MIN < TIME IN MINUTES > 30 MIN AMPLITUDE OF PULSE WAVE B 100,0 90,0 80,0 70,0 60,0 50,0 40,0 30,0 20,0 10,0 0,0 0 MIN < TIME IN MINUTES > 30 MIN 111 Monitoring the patients with three pulse oximeter equipments Fig 4. The oxygen saturation readings (A) and amplitude of pulse wave (B) in cases where the patients were treated in a cool operation room without blanket covering. The figure consists of five (n=5) patients. Only the cases in which the quality of detections was worst were accepted to this figure. These five measurements are in combination so that the injections of midazolam occur at the same time; two minutes after beginning i.e. at the left corner of the 1 hour and 20 minutes scale. There are three major areas of the artefacts (*) in the oxygen saturation readings. The line itself is the mean of the five registrations. A SaO2 ***** **** 100 90 80 70 60 50 40 30 20 10 0 0 MIN < TIME IN MINUTES > 1 H 20 MIN AMPLITUDE OF PULSE WAVE B 100 90 80 70 60 50 40 30 20 10 0 0 MIN < TIME IN MINUTES > 1 H 20 MIN 112 ****** Monitored intravenous sedation with local anaesthesia for dental outpatients Part II Fig 5. The oxygen saturation readings (A) and amplitude of pulse wave (B) in cases where the patients were treated with a blanket covering. Figure consists of five (n=5) patients (the same as in figures 2 and 3). Only the cases in which the quality of detections was most excellent were accepted to this figure. These five measurements are in combination so that the injections of midazolam occur at the same time; two minutes after beginning i.e. at the left corner of the 60 minutes scale. The line itself is the mean of the five registrations. No artefacts are available. SaO2 A 100,0 90,0 80,0 70,0 60,0 50,0 40,0 30,0 20,0 10,0 0,0 0 MIN < TIME IN MINUTES > 60 MIN AMPLITUDE OF PULSE WAVE B 100,0 90,0 80,0 70,0 60,0 50,0 40,0 30,0 20,0 10,0 0,0 0 MIN < TIME IN MINUTES > 60 MIN 113 Monitoring the patients with three pulse oximeter equipments 2.3.5 DISCUSSION patient warm covering him or her with a blanket. Of course it is possible to block this autonomic vasoconstriction reaction with local anaesthetic injected into the patient's finger (Eastwood 1992 and Sakurada 1995) but when we are treating a scared patient, it is wise to avoid such painful procedures. Moreover, an alarm delay lasting 12 to 30 seconds would prevent most false alarms (Pan and Gravenstein 1994). 2.3.5.1 False alarms An SaO2-artefact or false alarm is here described as extensive fall in SaO2 readings without any organic reasons like breathing failure or obstructed airways (Fig. 4). The study of White et al. (1989) have showed that nearly half of the patients developed clinically significant desaturation during minor oral surgery under local anaesthesia. They assumed that this might be due to breath-holding or peripheral vasoconstriction as a response to anxiety or fear (White et al. 1989). This retrospective review of patient records explains those observations: poor amplitude of pulse wave (A.P.W.) has caused false alarms. Even Lowes and Brooks' (1991) finding, that every fifth patient undergoing the surgical removal of third molar with local anaesthesia alone experienced hypoxic periods during surgery, is explained by false alarms. The influence of local anaesthetics to oxygen saturation has been studied by the author. In a previous study the saturation values were no more than 0,5 % lower (statistically insignificant) than the base level at the end of the measurement. Local anaesthesia is a possible source of measuring failures (Fig. 4) because it causes vasoconstriction but the agents used in local anaesthesia do not affect the level of the patient’s oxygen saturation. The easiest way to avoid these false alarms is to keep the 2.3.5.2 Reactions to local anaesthesia Considerable controversy exists in the literature regarding the haemodynamic changes caused by local anaesthetics. Previous studies have shown that there are no radical changes in blood pressure after local anaesthesia but the pulse rate will rise approximately 10 beats per minute if epinephrine containing lidocaine is used. Octapressin containing agents do not affect the pulse rate (previous article). Gortzak (et al. 1992b) studied subjects during routine restorative dental treatment. They found that all patients showed considerable blood pressure variation. Patients treated without local anaesthesia showed a significant mean blood pressure increase while patients treated with articaine as an agent of local anaesthesia showed no significant changes in blood pressure during treatment. Cioffi et al. (1985) concluded that routine restorative 114 Monitored intravenous sedation with local anaesthesia for dental outpatients Part II dental care with lidocaine epinephrine local anaesthesia did not produce clinically important haemodynamic response despite an increase in epinephrine levels. Frabetti et al. (1992) found also that patients who underwent surgical treatment had higher heart rate values than patients that underwent conventional therapy. According to this retrospective review of patient records the maximal pulse of the patient elevates from 91.3 beats to 98.6 beats per minute after the injection of epinephrine containing local anaesthetics but if prilocainephelypressine injection is used only one stress point is found: at the moment of injection (Study 7). .After the injection of lidocaineepinephrine there was an additional period of high pulse 5 - 10 minutes later when the epinephrine began to spread to the blood stream from the injection area. These new findings will explain also why the maximum st-segment depression in electrocardiogram was recorded 11 minutes after infiltration (Veit et al. 1993): the effect of epinephrine takes 20 minutes and that is the time during which the patient may have subjective disorders. If the patient has dental care phobia the situation may become frightful to the patient when the operative manoeuvres are begun before these epinephrine derived disorders have disappeared. If it is obligatory to use epinephrine containing lidocaine to avoid pain it is possible to reduce the amount of epinephrine by combining it with prilocaine - phelypressin. The combination does not cause adverse effects (Luotio et. al 1996) and may even enhance the local anaesthetic effect (Luotio et. al 1997). 2.3.5.3 Clinical monitoring The light generated in the finger probe of the pulse oximeter passes through the tissues. Different amounts of light are absorbed by oxygenated haemoglobin (HbO2) and unoxygenated or reduced haemoglobin (Hb). The pulsation of the arterial blood flow modulates the passing light. The pulse wave is derived from the intensity of the transmitted light. The total absorption of the light can be derived into absorbing components: tissues, venous blood and the pulsating arterial blood. The pulse wave-form reflects changes in blood volume and is the result of left ventricle contraction of the heart which fill the vascular bed of the finger with arterial blood (Mattila et al. 1989). Patients show vasoconstriction if the treatment is carried out in a cool operation room where they may feel cold. This also has a closing effect in A.P.W. which may often cause measuring failures because of low signal. Thus pulse oximetric measuring is reliable only in cases where the patient has comfortable surroundings. Without capillary pulsating blood flow, the pulse oximeter cannot compute the saturation value and the equipment will lose its proper function. However, possible measuring failures do not allow us to leave the patients without monitoring in the operation theatre. 115 Monitoring the patients with three pulse oximeter equipments A.P.W. will increase after the injection of benzodiazepine, and afterwards the local anaesthesia will cause some vasoconstriction. The regulation of peripheral arterial circulation is controlled by the autonomic nervous system. Vasoconstriction is induced by the stimulation of smooth muscles of arterioles. This decreases the amplitude of the pulse wave and may be due to some discomfort such as pain, fear, low temperature, as well as hypovolaemia (Mattila et al 1990). Vasodilatation is often seen after the dosage of sedative agent as a result of feeling good. The amplitude of the pulse wave is the most informative indicator of the changes in circulation. In most equipment these changes in amplitude are automatically corrected before expressed in display. This of course helps the operator as no manual correction is needed but at the same time one very informative parameter is lost if anxious patients are treated or if the patient is going to develop a vasoconstriction due to uncomfortable conditions or situations. 116 Monitored intravenous sedation with local anaesthesia for dental outpatients Part II 2.3.6 Clinical conclusions The main difference in the measurable pulse oximetric effects of local anaesthetics from benzodiazepines lies in amplitude of pulse wave. That will rise after the injection of benzodiazepine and afterwards local anaesthesia will cause some vasoconstriction: Vasodilation is often seen after the dosage of sedative agent as a result of feeling good. The decreases of the amplitude of pulse wave may be due to some discomfort such as pain, fear or low temperature and these may cause artefacts into the measuring values. The amplitude of the pulse wave is the most informative indicator of changes in circulation. In most equipment these changes in amplitude are automatically corrected before the pulse wave is expressed in display. At the same time one very informative parameter is lost. 117 Monitored intravenous sedation with local anaesthesia for dental outpatients Part III PART III PATIENTS’ EXPERIENCES DURING AND AFTER SURGERY UNDER INTRAVENOUS SEDATION 119 Monitored intravenous sedation with local anaesthesia for dental outpatients Part III 3.1 Study 4 Peroperative experiences In this study 108 patients who had experienced major or protracted dental operations under intravenous sedation with local anaesthesia were asked questions concerning their experiences, using an anonymous questionnaire. The most important finding was that the patients felt there was little need for general anaesthesia. Most patients (87%, 95% concidence interval 81% to 94%) preferred intravenous sedation with local anaesthesia. The patients were nearly unanimous in recommending intravenous sedation for other patients. Two clear subgroups were formed (by excluding 17 patients) according to their reasons: for 38 patients the main reason for undergoing intravenous sedation with local anaesthesia was a major surgical treatment (operation group), and for 53 patients the fear of any dental treatment, i.e. dental care phobia (phobia group). These subgroups showed no statistical difference in unpleasant experiences during treatment, though in the operation group the general impression of the treatment was slightly higher than in the phobia group (p= 0.05). Eight patients in the phobia group felt that they could undergo the operation next time with local anaesthesia alone, while only 1 patient in the operation group preferred the operation with local anaesthesia alone. The need for general anaesthesia was low, the patients (5 cases) reporting the need for general anaesthesia belonging to the phobia group. Local anaesthesia alone, as well as general anaesthesia, had somewhat higher preference in the phobia group than in the operation group (p=0.05). The patients in both groups reported that pain, fear, anxiety, confusion and drowsiness had not disturbed them during the treatment although the phobia group reported more confusion and fear during the operation than others (p<0.05). 121 Patients’ experiences 3.1.1 INTRODUCTION through sedation, since it is a rapid way to control fear and does not require any activity from the patient. This contrasts with the view of Krochak and Rubin (1992) who argue that although antianxiety pharmacological agents have their indications, they do not always treat the psychological needs of the patient. 3.1.1.1 Fear Fear activates the autonomic nervous system causing many clinical problems. Notable changes occur in the patient's heart rate, peripheral pulse volume, sweat activity and muscle tension as well as steroid levels in blood (Schahachter and Singer 1962, Berggren 1984). However, subjective feelings do not always correlate with measured physiological reactions (Tuutti 1986). Moreover, in many cases the adverse reactions to local anaesthetic are psychogenic in nature. Fear of injection, or of dental treatment in general, may lead to some of the most frightening "allergic" reactions tachycardia and vasodepressor syncope (Kleinhauz and Eli 1993). 3.1.1.2 Sedation Both types of patients, those presenting with only phobias and those with psychiatric disorders, can be treated in the dental office. However, a patient who suffers from dental care phobia can also be a source of stress for the dentists. Many dentists feel uncomfortable having to ease the patient's anxiety, nor do they want to spend the extra time required to treat this type of patient (Milgrom and Weinstein 1993). An anxious patient poses a problem for the dentist because the fear can prevent the dentist from working effectively. Moreover, insufficient knowledge and understanding of the psychological and emotional reactions caused by fear may affect the dentist's sense of professional satisfaction (Berggren 1984). Several factors have been discussed as causing dental fear: patients may have a phobic or psychopathological syndrome, they may suffer from neurosis or high general anxiety levels (Berggren 1984). Excessive levels of presurgical fear are even harmful to postoperative recovery (Edelman 1992 ). Fear is a learned behaviour, and can therefore be unlearned to be substituted by another way of behaviour (Krochak and Rubin 1992). However, psychological treatment is an extremely long way and of little use if the patient suffers from an acute disorder. For the dentist, the easiest way to control the patient's fear is A number of both psychological and pharmacological techniques are available to the dentist to reduce fear. Such pharmacological methods 122 Monitored intravenous sedation with local anaesthesia for dental outpatients Part III include premedication with sedative drugs or nitrous oxide, and general anaesthesia. Alternatively, the use of intravenous, inhalation or oral sedation have been reported (Lemasney et al. 1989). Intravenous conscious sedation with local anaesthesia has been shown to produce less patient stress than does general anaesthesia. Indeed, the use of intravenous sedation produces no clinically meaningful physiological changes in the patient's condition. Conversely, general anaesthesia increases heart rate and blood pressure as well as the levels of plasma epinephrine and cortisone, which are all indicative of a stress response. Thus, conscious sedation can be used to reduce the measurable parameters of stress that patients would develop during operations or other dental procedures (Shepherd et al. 1988, Hempenstall et al. 1986). Moreover, cost comparison has showed that it is twice as expensive to have the same procedure conducted under general anaesthesia as it is under intravenous sedation (Van Sichels and Tiner 1992). A further argument in favour of intravenous sedation is that though general anaesthesia may resolve the immediate dental problem, the phobia still remains (Lemasney et al. 1989). Despite its advantages, the majority of patients have never heard of the availability of intravenous sedation to supplement local anaesthesia during dental surgery. Nevertheless, earlier studies reveal that when given the opportunity to experience this method, the majority of patients have found it highly acceptable. (Rodrigo et Clark 1986, Lundgren 1988) Lind (et al. 1990) has previously reported that postoperatively many patients have complete amnesia of operative events and typically express the desire for a similar anaesthetic technique in future procedures when intravenous midazolam and fentanyl have been used in combination. However, it remains unclear how the patients would react to diazepam sedation if used in amounts which would not essentially produce total amnesia. An easy way to find out the patients' subjective feelings towards the use of sedation is to pose direct questions or to use different psychological measurements (precise instruments for the measurement of dental fear) made to the patient after treatment. However, a patient may sometimes lie and we can thus not always be sure about the real truth (Bernstein 1976). 123 Patients’ experiences patients had had positive or negative experiences of the procedure under sedation. Patient evaluation would thus indicate whether the sedation had any effect on the patient's phobia, i.e. had the phobia been relieved, remained unchanged or even become worse. 3.1.1.3 Aims of the study The aim of this study was to determine patients' reactions to treatment under intravenous sedation and to compare different patient groups with respect to subjective experiences and opinions. The present study attempts to resolve this question by determining whether the 124 Monitored intravenous sedation with local anaesthesia for dental outpatients Part III 3.1.2 PATIENTS AND METHODS or whose subgroup was difficult to determine, i.e. no answer in this question (1 patient) or double ticks (2 patients). These patients are still in the whole material as members of the”others” group. For 37 patients, the main reason for treatment under intravenous sedation was the major nature of the surgical procedure itself (operation group). 53 patients were scared of the dental treatment, i.e. they had dental care phobia (phobia group). The groups were comparable with respect to gender distribution (Chi-square test, p=0.66). The patients in the phobia group were significantly younger than the patients in the operation group (37.0 vs. 48.9; p<0.0001), and also younger than the other patients (37.0 vs. 43.5; p=0.05). The phobia group differed significantly from other patients also with respect to the time lag between the operation and the questionnaire and the time between the last appointment at the dentist and the operation (Tables 1-2) 3.1.2.1 Patients The research group consists of 108 patients undergoing dental procedure with intravenous sedation at the first author’s private practice. The material comprises all the patients who had their treatment under intravenous sedation before the mailing of the questionnaire. Patients underwent surgery primarily for implantological reasons, major conservative dental treatment, or extraction under sedation due to dental care phobia. The subjects were private practice dental patients, who are mostly in a good state of health, though there is always a minority of patients suffering from systemic disease which may limit their activity, i.e. they conformed to groups I-III of the ASA (American Association of Anaesthesiologists) classification. None of the patients corresponded to the ASA classification for groups IV V. No patients were excluded. The patients were within the limits of generally accepted indications and contraindications as mentioned in the text books for dental anaesthesia. Before the treatments, a number of criteria were considered for treatment and anaesthesia selection: who needs sedation, for whom would diazepam alone not be sufficiently effective and whether there might be any difference in the effectiveness of one type of anaesthesia for different types of operations. The mean age was 42 years (SD 13). The patients were divided into two main groups by the dentist according to their main reason for the treatment: phobia or oral surgery (question 1.). These subgroups were formed or refined by excluding 17 patients who answered ”other reason” 125 Patients’ experiences Table 1. Types of treatments in the different clinical groups of patients All patients Subgroups Type of treatmens (108) Phobia (53) Operation (38) restorative works 52 (48%) 39 (74%) 4 (10%) extraction 47 (44%) 32 (60%) 7 (18%) scaling 38 (35%) 26 (49%) 5 (13%) oral surgery 44 (41%) 8 (15%) 30 (79%) Table 2. Patient characteristics in the phobia group, the operation group and in ”others”. All (n=108) 46% 54% Phobia (n=53) 43% 57% Operation (n=38) 46% 54% Others (n=17) 56% 44% Gender males females Age (years) mean SD range 42.1 12.8 16-78 37.0 9.9 16-63 48.9 12.9 19-78 43.5 13.9 22-67 Time (months) from operation mean SD range 11.4 8.3 1-30 13.6 8.5 1-30 7.9 6.9 1-30 11.8 8.0 4-30 Previous visit mean before operation range 4.9 0-30 7.3 0-30 2.1 0-10 126 3.6 0.2-15 Monitored intravenous sedation with local anaesthesia for dental outpatients Part III years for the phobia and operation groups respectively. 3.1.2.2 Questionnaire An anonymous questionnaire was mailed to the 136 patients who had previously undergone intravenous sedation with local anaesthesia. The response rate to the mailed survey was 79.4% (108 patients). Two patients could not be located by postal authorities and 26 declined to respond. Of the patients who responded, 49 (46 %) were found to be males and 57 (54 %) females, yielding a total sample of 108 (2 patients did not answer this question). The whole study group received the following treatments: restorative work in 52 cases (48%), extraction in 47 cases (44%), scaling in 38 cases (35%) and a surgical procedure in 44 cases (41%). For the operation group, the corresponding figures were: restoration 4 (10%), extraction 7 (18%), scaling 5 (13%) and surgery 30 (79%), and for the phobia group 39 (74%), 32 (60%), 26 (49%) and 8 (15%), respectively. Almost all patients underwent treatments (e.g. extraction or major surgery) after which postoperative pain was to be expected. The mean period of time between the treatment and answering the questionnaire was 11.4 months (SD 8.2) for the whole study group. For the phobia group and the operation group, this period was 13.1 (SD 8.4) and 7.9 (SD 6.8) months respectively. (There is no particular explanation for the difference of response delay between the groups: these patients were the whole material of the intravenously sedated patients of the clinic during one period of time.) Previous contact with a dentist prior to this treatment was 4.9 (SD 5.9) years for the whole study group, and 7.0 (SD 7.0) years and 2.1 (SD 2.7) The questionnaire used a vertical visual analogy scale (V.A.S.) which plumbed the patients’ subjective opinions about experiences during treatment (peroperative). The patients were asked to mark the point on a 100-millimetre scale between satisfying and displeasing. The lower end indicated a lack of the asked experience and the upper end a strong presence of the experience. 127 Patients’ experiences 3.1.2.3 Medication For sedation, diazepam with soybean oil solvent were used in 85 cases (Stesolid Novum 2 ml inj. 5 mg/ml Dumex/KabiVitrum) or midazolam in 24 cases (Dormicum 5 ml inj. 1 mg/ml Roche), with the mean amounts corresponding to 12 mg SD 5.0 mg and 6.2 mg SD 2.7 mg, respectively. For pain relief, fentanyl (Fentanyl 2 ml inj. 50 microgram/ml Orion) was rarely used (only in 7 cases, combined with some of the sedative agents mentioned above); when used, it was administered only in low amounts (mean 1.3 ml SD 0.5 ml). The benzodiazepine antagonist which was available and used in cases, when needed, was flumazenil (Lanexat 5 ml inj. 0.1 mg/ml Roche). Local anaesthesia was performed in combination with lidocaine (Xylocain adrenalin 1.8 ml inj. 20 mg/ml+12.5 mcg/ml ASTRA) mean 8.8 ml SD 4.3 ml and prilocaine (Citanest Octapressin 1.8 ml inj. 30 mg/ml+0.54 mcg/ml ASTRA) mean 8.6 ml SD 3.6 ml (Table 3). At the first examination, the patients completed a questionnaire about previous and present illnesses, allergies and medications. A dental care plan was prepared. All patients were referred to radiological examination (orthopantomography) and the majority of the implantological patients were also referred to laboratory blood evaluations (B-Se, B-Hb, B-leuk, fBglu). Patients were advised both verbally and in writing on how to prepare for intravenous sedation (for example, no food or drink during the four hours prior to treatment). No oral premedication was given to the patients on either the day of the operation or the preceding day. Before the insertion of peripheral venous cannula, blood pressure was recorded, and monitoring with a pulse oximeter was initiated if midazolam was used as the sedative agent. These patients were followed up with an Ohmeda pulse oximeter and the data collected with the program supplied by Ohmeda (37XX) using a Toshiba T1000SE computer. After canulation, an infusion of 0.9% sodium chloride solution was started and a sedative agent was applied with a disposable syringe using the slow injection technique. The surgery was equipped with a dental unit, pulse oximeter, oxygen supplement unit and resuscitation facilities including endothracheal intubation equipment and medication for cardiopulmonary resuscitation. After treatment, blood pressure was recorded again and the venous cannula removed. The patients remained in the dental chair until the bleeding following extraction had subsided and the patient felt well and was able to walk and dress without help. 128 Monitored intravenous sedation with local anaesthesia for dental outpatients Part III Table 3. Medication (mg) in groups Midazolam n Mean Range All (n=108) 24 6.2 2.5-15 Diazepam n Mean range 8.5 12.0 5-40 Fentanyl n Mean Range Lidocain* n Mean range 100 177.1 36-468 53 194.4 36-360 31 146.3 72-360 16 180 72-468 Prilocain** n Mean range 88 234 54-648 47 261 54-648 27 196.2 54-378 14 212.4 108-432 7 0.065 0.025-0.1 Phobia (n=53) 9 8.1 5-15 Operation Others (n=38) (n=17) 11 4 5. 1 5. 1 2.5-10 3.5-25 45 13.2 7.5-40 27 10.3 5-20 2 0.065 0.025-0.1 4 0.065 0.05-0.1 13 11.7 5-25 1 0.065 * the amount of vasoconstrictor (epinephrine) not expressed on this table ** the amount of vasoconstrictor (phelypressine) not expressed on this table 129 Patients’ experiences used to compare the VAS values between phobia group and other groups. 3.1.2.4 Statistical methods The answers were measured from the VAS-scale and represented as boxplots which are made up of "boxes" which contain 50% of the values falling between the 25th and 75th percentiles, and the "whiskers", lines that extend from the box to the highest and lowest values, excluding outliers. A line across the box indicates the median. The patients in the phobia group were significantly younger compared to the other patients. It was also discovered that age was significantly (negatively) correlated with most of the experiences and symptoms. For that reason, an analysis of covariance (ANCOVA) was performed to compare the phobia group to other patient groups. In the ANCOVA model, age was included as a covariate to control the differences in age distributions between groups. A visual analoque scale (VAS) was used to describe the experiences (0=unpleasant, 100=pleasant) and symptoms (0=none, 100=extreme) during the treatment. These VAS values are depicted in Box-andwhisker plots. The box indicates the lower and upper quartiles (25th and 75th percentiles) and the central line is the median. The points at the ends of the whiskers indicate the lowest and highest values (excluding outliers). Mann-Whitney U test was Chi-square test was used to test the differences in preferences between patient groups if the therapy had to be repeated. The data were analysed using SPSS statistical package (Version 6.1.3). 130 Monitored intravenous sedation with local anaesthesia for dental outpatients Part III 3.1.3 RESULTS therapy under intravenous sedation with local anaesthesia for other patients. Only one patient left this question unanswered. Most of the patients (78 cases, 72%) subsequently made a new appointment with the dentist (Fig. 4, Table 6). 3.1.3.1 All patients (n=108) The results for the whole study group indicated that the patients felt the experience of treatment under intravenous sedation with local anaesthesia to be more pleasant than unpleasant (Mean 62, SD 16 in the VAS-scale) and were more satisfied than displeased (76, SD 13) with the treatment. When asked about their unpleasant experiences, the responses for the whole study group were the following (scale 100 = extreme, 0 = none): low pain (18, SD 16), some fear (26, SD 23), low anxiety (17, SD 19), low confusion (18, SD 20), and some drowsiness (28, SD 24). (Medians and ranges are expressed in table 4) 3.1.3.2 Phobia group (n=53) In the phobia group, the patients felt that the experience of the treatment under intravenous sedation with local anaesthesia was more pleasant than unpleasant (Mean 62, SD 17 in the VAS-scale) and were more often satisfied than displeased (75, SD 14) with the treatment. When asked about unpleasant experiences, these patients reported experiencing the following (scale: 100 = extreme, 0 = none): low pain (17, SD 14), moderate fear (33, SD 25), low anxiety (19, SD 21) low confusion (22, SD 22) and some drowsiness (29, SD 24). (Medians and ranges are expressed in table 4) In addition, the patients were asked which type of anaesthesia they would prefer if the therapy had to be repeated. For the whole study group, the perceived need for general anaesthesia was very low (5 patients, 5%), with most patients preferring intravenous sedation and local anaesthesia (94 patients, 87%) and only 11 patients (10%) reporting they could repeat the operation with local anaesthesia alone. (Some of the patients made several ticks for each question in the questionnaire) However, none of the patients felt that they could undergo the treatment without local anaesthesia. With only one exception all patients (99%) stated that they could recommend In response to which type of anaesthesia would be preferred if the therapy had to be repeated, even the phobia group felt little need for general anaesthesia (5 patients, 9.4%). Interestingly, all patients who had sought general anaesthesia were in this group. Most patients expressed a preference for intravenous sedation with local anaesthesia (43 patients, 81%). Eight patients (15%) stated 131 Patients’ experiences they would repeat the operation with local anaesthesia alone. (Some of the patients made several ticks for each question in the questionnaire). None of the patients, however, felt they could undergo the treatment without local anaesthesia. All patients, except one, (98%) reported they could recommend the therapy under intravenous sedation with local anaesthesia for other patients. One patient did not respond to this question. Most of the patients in the phobia group (28 patients, 52%) were found to make a new appointment with the dentist later(Fig. 4, Table 6). anaesthesia was expressed by those in the operation group. Almost all these patients preferred intravenous sedation with local anaesthesia (36 patients 95%). Only one patient (2.6%) reported that the operation could be repeated with local anaesthesia alone. None of the patients felt that they could withstand the treatment without local anaesthesia. All patients reported that they could recommend the therapy under intravenous sedation with local anaesthesia for other patients. All, except one patient, (36 patients 95%) later made a new appointment with the dentist (Fig. 4, Table 6). 3.1.3.3 Operation group (n=38) 3.1.3.4 Differences In the operation group, the patients reported feeling that the experience of treatment under intravenous sedation with local anaesthesia was more pleasant than unpleasant (Mean 58, SD 16 in the scale 100-0) and were more often satisfied than displeased (73, SD 14) to the treatment. When questioned concerning unpleasant experiences, patients in the operation group reported experiencing low levels of the following (scale: 100 = extreme, 0 = none): pain (19, SD 19), fear (17, SD 17), anxiety (13, SD 14), confusion (15, SD 17). Only drowsiness (28, SD 26) was reported at a moderate level. (Medians and ranges are expressed in table 4) There was a statistical difference (p=0.05) between the operation and phobia groups in the general impression on the treatment; the phobia group felt the treatment a little bit more pleasant than the operation group but the difference was minimal (1 VAS unit). Satisfaction with the treatment showed a similar or even higher tendency but the statistical significance was not so strong (p=0.09). Fear and confusion during the operation were the only parameters which were higher in the phobia group than in both of the other groups (table 4), but in confusion the statistical analysis failed to show any high significance between the operation and the phobia group. The patients’ age did not correlate with fear (Table 5) but there was, however, a correlation with confusion. A When the patients were asked which type of anaesthesia they would prefer if the therapy were to be repeated, no need for general 132 Monitored intravenous sedation with local anaesthesia for dental outpatients Part III preference (if the therapy had to be repeated) comparison showed that intravenous sedation had the highest preference in the operation group (95%). The phobia group also preferred intravenous sedation in the first place (81%) but the preferences for local anaesthesia alone or general anaesthesia were higher in this group (p=0.05). Although there were some statistically significant differences between the groups, the values of those differences were minimal. 133 Patients’ experiences Table 4. Subjective experiences during the treatment in the phobia group, operation group and ”others” group. Experiences: General impression* (0=unpleasant 100=pleasant) Range** Satisfaction with treatment* ( 0=displeased 100=satisfied) ** Symptoms during treatment: Pain* ** Fear* ** Anxiety* ** Confusion* ** Drowsiness* ** All Phobia patients group Operation group Others p-values***: p-values: phobia vs. phobia operation vs. others 67 0.05 0.77 (54-68) (51-71) (52-67) 69 78 68 (67-68) 68 0.09 0.26 (67-87) (67-92) (67-85) (68-72) 15 15 (4-33) (4-33) 22 34 (4-37) (14-50) 7 9 (2-33) (2-35) 8 20 (2-35) (3-38) 30 31 (5-39) (6-43) 17 (4-22) 10 (3-33) 2 (2-19) 3 (1-5) 22 (5-34) 0.73 0.64 0.004 0.04 0.37 0.12 0.18 0.009 0.54 0.33 67 67 66 15 (4-33) 12 (4-34) 7 (2-29) 8 (3-30) 26 (4-50) *) Visual Analogue Scale (VAS) values were used. In symptoms a higher value denotes a more extreme disorder, i.e. pain, fear, anxiety, confusion or drowsiness. The figures are median (IQR). **) IQR = inter-quartile range (25th centile - 75th centile). ***) Mann-Withney U-Test 134 Monitored intravenous sedation with local anaesthesia for dental outpatients Part III Table 5. Comparison of study groups with respect to subjective experiences and symptoms during the treatment. The results based on the analysis of co-variance, where the groups' experiences are being compared and age is included as a covariance. Experiences * Phobia vs. Operation p-value Phobia vs. Others p-value effect of age beta-coefficient p-value General impression 0.17 0.36 0.24 0.07 Satisfaction 0.08 * 0.12 -0.09 0.43 Pain 0.33 0.70 -0.29 0.04 Fear 0.0007 0.02 -0.25 0.20 Anxiety 0.16 0.16 -0.20 0.24 Confusion 0.06 * 0.008 -0.38 0.03 Drowsiness 0.77 0.26 -0.54 0.01 135 Patients’ experiences Figure 1 a and b. General impression (0=unpleasant, 100=pleasant) in all patients and in phobia group, operation group and in others. Figure 1a All patients (n=108) 0 20 40 60 80 100 V.A.S: Unpleasant - Pleasant Figure 1b Subgroups Phobia (n=53) Operation (n=38) Others (n=17) 0 20 40 60 V.A.S: Unpleasant - Pleasant 136 80 100 Monitored intravenous sedation with local anaesthesia for dental outpatients Part III Figure 2 a and b. Satisfaction with treatment (0=unpleasant, 100=pleasant) in all patients and in phobia group, operation group and in others. Figure 2a All patients (n=108) 0 20 40 60 80 100 V.A.S: Displeased - Satisfied Figure 2b: Supgroups Phobia (n=53) . Operation (n=38) . Others (n=17) . 0 20 40 60 V.A.S: Displeased - Satisfied 137 80 100 Patients’ experiences Figure 3 a-d. The level of unpleasant experiences in the study groups. Unpleasant experiences are presented as a visual analogy scale: a higher value denotes a more extreme disorder, i.e. pain, fear, anxiety or confusion. Figure 3a All patients (n=108) Fear . Anxiety . Confusion . Pain . Disorder 0 20 40 60 80 100 V.A.S. No symptom - severe symptom Figure 3b Phobia subgroup (n=53) Fear . Anxiety . Confusion . Pain . Disorder 0 20 40 60 80 V.A.S. No symptom - severe symptom 138 100 Monitored intravenous sedation with local anaesthesia for dental outpatients Part III Figure 3c Operation subgroup (n=38) Fear . Anxiety . Confusion . Pain . Disorder 0 20 40 60 80 100 V.A.S. No symptom - severe symptom Figure 3d Other (n=17) Fear . Anxiety . Confusion . Pain . Disorder 0 20 40 60 80 V.A.S. No symptom - severe symptom 139 100 Patients’ experiences Figure 4. The preference for the different types of peroperative anaesthesia. The patients were asked: "Which type of anaesthesia would you prefer if the treatment had to be repeated." 100 90 80 PERCENTS OF PATIENTS 70 60 50 40 30 20 10 0 GENERAL ANESTH. I.V. SEDATION WHOLE GROUP LOCAL ANESTH. OPERATION GROUP NO ANESTHESIA PHOBIA GROUP Table 6. Preferences (%) if the therapy had to be repeated. Groups: All Phobia Oper. Others p-values * Phobia vs. Operations Preferences: Phobia vs. Others Intravenous sedation with local anaesthesia 87% 81% 95% 88% 0.06 0. 50 Local anaesthesia alone 10% 15% 3% 12% 0.05 0.73 Without local anaesthesia 0% 0% 0% 0% General anaesthesia 5% 9% 0% 0% 0.05 0.19 *) Chi-square test 140 Monitored intravenous sedation with local anaesthesia for dental outpatients Part III 3.2 Study 5 Postoperative experiences In this study, 136 patients had major or protracted dental operations under intravenous sedation with local anaesthesia. They were later mailed an anonymous questionnaire. The most important finding was that pain was the primary symptom after treatment under intravenous sedation with local anaesthesia. Patients reported that the pain was not a result of sedation but the result of the operation itself. The incidence of confusion and tiredness reduced after the first night. The possibilities to avoid pain and confusion are discussed. Some other disorders were detected but they were rare: headache and nausea but no vomiting. Two clear subgroups were formed (by excluding 17 patients) according to their reasons: for 38 patients the main reason for undergoing intravenous sedation with local anaesthesia was a major surgical treatment (operation group), and for 53 patients the fear of any dental treatment, i.e. dental care phobia (phobia group). The operation group served as a reference group. These subgroups showed statistically significant differences with the incidence of confusion immediately after the treatment. The phobia group felt more confused than the operation group (p= 0.05) and were more often incapable of daily work or driving a car (p<0.05). No statistical difference appeared in unpleasant experiences on the next day. The patients felt healthy after intravenous sedation with local anaesthesia and the feeling increased during the following days (p<0.0001). The patients felt confusion for approximately three hours and most patients felt ready for the daily work in the next morning. However, sedative premedication increases the need of sleep and the patients need more rest than normally on the first day after treatment. example the duration of the operation, cannot explain the wide variations in postoperative morbidity after oral surgery (Berge and Boe 1994). Common side effects such as nausea and vomiting may occur in up to one third of the patients if opioids are used. However, the incidences of emetic symptoms in the postoperative 3.2.1 INTRODUCTION 3.2.1.1 Postoperative recovery There is some evidence available that excessive levels of presurgical fear are even harmful to postoperative recovery (Edelman RJ 1992 ), but commonly used predictors, for 141 Patients’ experiences period have failed to show any difference although benzodiazepines are used (Bonazzi et al 1994). Similarly, the proper combination of two differently acting sedative agents have not prolonged the recovery time (Taylor et al. 1992). Thomson (et al. 1993) have found that, although initial postoperative recovery to a 'fully awake' state occurred more rapidly if benzodiazepine antagonist (flumazenil) had been used, objective psychomotor testing have revealed even poorer performance if compared with spontaneously recovering patients. They believed that the patients need at least 1 h before the discharge home. There have been only minor differences in postoperative recovery time between the methods of sedation, even in the cases when patient-controlled sedation was used (Osborne et al. 1994). 3.2.1.2 Aim of the study This article attempts to describe the condition of the patient during the hours and days following dental operations. The aim for this study was a clinical interest to find out how the patients felt after treatment under intravenous sedation with local anaesthesia. An anonymous questionnaire was sent to resolve the main question, "did the patient have complications after the procedure under sedation" i.e. is the procedure as superior as it seems to be from the point of view of the dentist. Moreover, it was tried to define if the treatment itself was the main source for the symptoms, and if there could be differences between patients who suffered from dental care phobia and those whose treatment was a major oral surgery. There was also a need to find out how much time the patient needs for recovery. 142 Monitored intravenous sedation with local anaesthesia for dental outpatients Part III 3.2.2 PATIENTS AND METHODS The study group is the same as in the previous study 4. test, pairwise comparisons were made using Wilcoxon test for matched pairs. Mann-Whitney U test was used to compare the VAS values and duration of confusion between phobia group and other groups. Chi-square test was used to compare the patient groups with respect to nominal data. The data were analysed using SPSS statistical package (Version 6.1.3). 3.2.2.1 Statistical methods A visual analoque scale (VAS) was used to describe the postoperative general condition (0 = awful, 100 = wonderful). Friedman's nonparametric analysis of variance was performed to compare the VAS values from three successive periods: before sleep, next day and next week. Following a significant Friedman's 143 Patients’ experiences 3.2.3 RESULTS decrease of most postoperative disorders from the time before sleep to the time after sleep. Tiredness was the primary symptom, caused mainly by diazepine, and therefore it was the most rapidly decreasing disorder. However, it was impossible to show the decrease of the pain and "the other symptoms" (Table 2). 3.2.3.1 All patients (n=108) The patients in the whole study group felt more healthy (wonderful feeling) than unhealthy (awful feeling) after intravenous sedation with local anaesthesia. This question was further divided into three time limits: before sleep, from the following morning to the following night, and the following week. In the visual analog scale 0-100 (awful wonderful) the answers were (Mean and standard deviation, medians and ranges are expressed in table 1): before sleep 67 (SD 18.8), next day 73 (SD 19.1) and following week 80 (SD 19.8). The time effect (Table 1) was significant (p=0.0001). Interpreted into words this means that the patients felt well all along and the feeling was enhanced with time. (Fig. 1a ) As a whole, patients felt that they were confused for 2.7 hours (SD 3.5); the escorts thought that the patients were confused 2.6 hours (SD 3.8). Most patients (64 cases, 59%) felt capable of daily work the next morning. The opinion of the escort was similar (59 cases, 54%). Respectively they felt capable of driving a car the next morning: patients themselves in 69 cases (64%) and in the escorts' opinion in 62 cases 57%. The remainder of the patients answered in the negative or left the question unanswered. In 40 cases (37%) the patients believed that the main reason for disorders was the treatment itself. 34 patients (32%) felt that sedation caused the main disorders and 16 (15%) felt local anaesthesia was responsible for disorders. 8 patients (7%) expressed that there was "some other reason" for those disorders. The patients in the whole examination group suffered following major postoperative disorders after treatment but before going to sleep: 16 patients felt to be confused (15%), 39 felt tired (36%), 29 felt pain (27%). Other disorders were rare: headache in 5 cases (5%), nausea in 3 cases (3%), no vomiting, other disorder in 8 cases (7%). (Fig.2) After sleep the disorders were at a lower level: confused 6 cases 6%, tiredness 13 cases 12%, pain 23 cases 21%, headache 3 cases 3%, nausea 1 case 1%, no vomiting, other disorder 9 cases 8%. (Fig.3). There was a The following questions were made to the patients: At which time did the treatment begin, when was it over; when did they sleep the next time; when did they wake up? On the 144 Monitored intravenous sedation with local anaesthesia for dental outpatients Part III basis of the answers the sleeping behaviours could be divided according to the treatment time. Three subgroups were formed: 1."aftrnoon nap group" which comprises the patients who slept and woke up before the actual night. 2. "evening group" which comprises patients who went into bed before midnight and woke up the next morning. 3."night group" contains the rest of the patients, who had their night's sleep after midnight. It was found that if the treatment was before or at noon (mean at 11:09), the patients had a sleeping period in the afternoon. The duration of the sleep varied considerably on this day. If the treatment was carried out in the afternoon (mean at 5:20 p.m.) the patients went to sleep early evening (mean at 7:58 p.m.) and they had an extended period of sleep. The patients who were treated in the evening (mean at 7:00 p.m.) got to sleep late at night (mean at 00:37 a.m.). The sleeping patterns are presented in tables 3a and 3b. 23). Pairwise comparisons showed a significant (p=0.05) increase in VAS values (Table 1). In other words they felt well all the time and the feeling intensified with time. (Fig. 1b) After treatment but before going to sleep the patients in the phobia group suffered the following postoperative disorders: 13 patients felt confused (24%), 18 felt tired (34%), 15 felt pain (28%). Other disorders were again rare: headache in 1 case (2%), nausea in 3 cases (6%), no vomiting at all, other disorders in 3 cases (6%). (Fig.2, table 2). After sleep the disorders were at a lower level: confusedness 4 cases 8%, tiredness 8 cases 24%, pain 13 cases 24%, headache 1 cases 2%, nausea 1 case 2%, no vomiting, other disorders 5 cases 9%. The most important disorders were the pain from the operation and the tiredness from the sedative. (Fig.3, table 2) The patients (phobia group) felt that they were confused for 2.3 hours (SD 2.8), and the escorts thought that the patients were confused 2.2 hours (SD 3.9). Most patients felt (29 cases 55%) capable of daily work the next morning. The opinion of the escort was similar (27 cases 51%). Respectively, they felt capable of driving a car the next morning: patient’s opinion 29 cases (55%) and escort’s opinion in 27 cases (51%). The patients believed that the main reason for the disorders was the treatment itself in 18 cases (34%). 13 patients (25%) felt that sedation caused the main disorders and 8 3.2.3.2 The phobia group (n=53) In the phobia group, as in all groups, the patients felt more healthy (wonderful feeling) than unhealthy (awful feeling) after intravenous sedation with local anaesthesia. In the visual analog scale 0-100 (awful wonderful) the answers were (Mean and standard deviation, medians and ranges are expressed in table 1): before sleep 65 (SD 22), next day 70 (SD 23) and following week 77 (SD 145 Patients’ experiences (15%) felt that local anaesthesia was responsible for disorders. 4 patients (8%) expressed that there was "some other reason" for the disorders. Pain was the most important disorder in this group. The patients (operation group) felt that they were confused 3.5 hours (SD 4.7), the escorts thought that the patients were confused 3.2 hours (SD 4.1). Most patients felt (25 cases 66%) capable of daily work the next morning. The opinion of the escort was similar (23 cases 60%). Respectively, they felt capable of driving a car the next morning: patient’s opinion in 31 cases (82%) and escort’s opinion 27 cases 71%. The remaining patients answered in the negative or left the question unanswered. Nearly half of the patients believed that the main reason for the disorders was the treatment itself (in 14 cases = 37%). The same number of patients (14 patients = 37%) felt that sedation caused the main disorders and 5 (13%) felt that local anaesthesia was responsible for disorders. 3 patients (8%) expressed that there was "some other reason" for those disorders i.e. the patients felt pain equally disturbing as tiredness. 3.2.3.3 Operation group (n=37). In the operation (control) group the patients felt healthy after intravenous sedation with local anaesthesia. In the visual analog scale 0-100 (awful - wonderful) the answers were (Mean and standard deviation, medians and ranges are expressed in table 1): before sleep 66 (SD 15), next day 72 (SD 14) and following week 78 (SD 15). Pairwise comparisons showed significant increase in VAS again (p<0.05). This means in practice that they felt well all the time and the feeling was intensified with time. (Fig. 1c) After treatment but before going to sleep the patients in the operation (control) group suffered from the following major postoperative disorders: 13 patients felt tired (35%), 12 felt pain (32%). Other disorders were rare: headache in 3 cases (8%), 2 patients felt confused (5%), no nausea nor vomiting at all, other disorders in 1 case (3%). (Fig.2, table 2) After sleep the disorders were at a lower level: confused 2 cases 5%, tiredness 5 cases 13%, pain 8 cases 22%, headache 1 case 3%, no nausea nor vomiting, other disorders 2 cases 5%. (Fig.3, table 2) 146 Monitored intravenous sedation with local anaesthesia for dental outpatients Part III 3.2.3.4 Differences groups when all symptoms were investigated. The statistically significant difference between the groups was in the incidence of confusion immediately after the treatment. The phobia group was more confused than the operation (control) group (p=0.01). Likewise there were differences between the groups in the capability of driving or daily works (p<0.05, table 5). However, a statistical analysis failed to show any differences in disorders between these If the treatment took place in the morning or at noon, the patients had a sleeping period in the afternoon. The duration of this afternoon nap varied considerably. If the treatment was carried out in the afternoon, the patients went to sleep early in the evening and they had an extended sleep. The patients who were treated in the evening went to sleep late at night. (Table 3) 147 Patients’ experiences Table 1. General condition (VAS* values) before sleep, the next day and the next week in the phobia group, the operation group and others group. Groups: All Phobia Oper. Others p-values*** Median (IOR) Median (IQR) Median (IQR) Median (IQR) Phobia vs. Oper. Phobia vs. Others Before sleep 68 (57-72) 68 (58-75) 68 (58-70) 70 (54-72) 0.83 0.89 Next day 70 (66-93) 68 (56-97) 70 (67-75) 74 (70-82) 0.77 0.41 Next week 83 (70-97) 87 (69-99) 77 (70-91) 90 (82-98) 0.33 0.56 P<0.0001 P=0,0001 P<0.001 Time: p-value of P<0.0001 time effect*** *) Visual Analoque Scale was used. 0=awful and 100=wonderful. **) Mann-whitney U-test ***) Friedman*s test. In all three groups the time effect is significant (p<0.0001), and in the phobia and operation groups all the pairwise comparisons (before sleep vs. next day and next day vs, next week) showed a significant (p<0.05) increase in VAS values. In the ”others” group the increase of VAS values from next day to next week was significant (p<0.05). 148 Monitored intravenous sedation with local anaesthesia for dental outpatients Part III Figure 1a -d. Postoperative feeling (0=unpleasant, 100=pleasant) in all patients and in phobia group, operation group and in others. Figure 1a: All patients (n=108) Next evening Next day Next week 0 20 40 60 80 100 80 100 V.A.S: unpleasant - pleasant Figure 1b: Phopia subgroup (n=53) Next evening Next day Next week 0 20 40 60 V.A.S: unpleasant - pleasant 149 Patients’ experiences Figure 1c: Operation subgroup (n=38) Next evening Next day Next week 0 20 40 60 80 100 80 100 V.A.S: unpleasant - pleasant Figure 1d: Other (n=17) Next evening Next day Next week 0 20 40 60 V.A.S: unpleasant - pleasant 150 Monitored intravenous sedation with local anaesthesia for dental outpatients Part III Figure 2. Postoperative disorders after treatment on the day of the treatment. The phobia group felt more confused than the operation (control) group. 100 Incidence (%) of dissorder 90 80 70 60 50 40 30 20 10 0 w hole group Confusion Tiredness operation group Pain Headache phobia group Nausea Other 2) Figure 3. Postoperative disorders after treatment and first sleep. No differences between the groups. 100 Incidence (%) of dissorder 90 80 70 60 50 40 30 20 10 0 w hole group Confusion Tiredness operation group Pain 151 Headache phobia group Nausea Other Patients’ experiences Table 2. The occurrence (%) of different symptoms before (B) and after (A) the first sleep at home in the phobia group, operation group and ”others” group… and reasons for those disorders. Groups: All Phobia Oper. Others 15% 6% 36% 12% 27% 21% 5% 3% 3% 1% 0% 0% 7% 8% 25% 8% 34% 15% 28% 25% 2% 2% 6% 2% 0% 0% 6% 9% 5% 5% 34% 13% 32% 21% 8% 3% 0% 0% 0% 0% 3% 5% 6% 0% 47% 0% 12% 12% 6% 6% 0% 0% 0% 0% 24% 12% 34% 15% 25% 37% 13% 37% 8% 8% Disorder: Confusion Tiredness Pain Headache Nausea Vomiting Other Reason for disorder: treatment itself sedation local anaesthesia other reason B A B A B A B A B A B A B A 152 p-values Phobia Phobia vs. vs. Operation Others 0.09 0.01 0.67 0.24 0.98 0.33 0.79 0.09 0.74 0.17 0.70 0.26 0.17 0.39 0.81 0.39 0.14 0.32 0.39 0.57 0.49 0.39 0.03 0.78 47% 18% 41% 0.79 0.79 0.20 0.33 0.80 0.19 6% 0.95 0.82 Monitored intravenous sedation with local anaesthesia for dental outpatients Part III Table 3 A. Sleeping behaviour after treatment. This table consists of patients (N=76) who went into bed before midnight and woke up the next morning. The patients who had a previous afternoon nap or who had their night's sleep after midnight are excluded. Treatment began 5:20 p.m. (SD 2:42) Treatment completed 7:16 p.m. (SD 2:44) Patient fell asleep 7:58 p.m. (SD 6:51) Patient woke up 7:05 a.m. (SD 1:22) Table 3 B. Sleeping behaviour after treatment. This table consists of previously excluded patients. AFTERNOON NAP GROUP Treatment began 11:09 a.m. (SD 3:03) This group (N=10) consists of those Treatment completed 12:37 p.m. (SD 2:45) patients who slept Patient fell asleep 3:27 p.m. (SD 2:44) and woke up before the actual night. Patient woke up 3:56 p.m. (SD 5:52) LATE NIGHT GROUP Treatment begun 7:00 p.m. (SD 0:37) (N=5) contains the rest of the patients Treatment completed 9:15 p.m. (SD 0:50) who had their night's Patient fell asleep 00:48 a.m. (SD 0:24) sleep after midnight. Patient woke up 08:06 a.m. (SD 0:48) 153 Patients’ experiences Table 4. Duration of confusion (hours) in the phobia group, the operation group and others group Group: All Phobia Oper. Others p-values Phobia vs. Opinion: Mean SD Mean SD Mean SD Mean SD Oper. Others Patient’s 2.8 3.5 2.6 2.8 3.5 4.8 2.3 2.2 0.91 0.96 Escort’s 2.7 3.9 2.4 4.0 3.2 4.2 2.5 2.9 0.86 0.82 Table 5. Capability (%) of daily work or driving Group: Phobia Operation Others Daily work: p-value Phobia vs. Phobia vs. Operation Others patient’s opinion 55% 66% 59% 0.29 0.77 escort’s opinion 53% 64% 64% 0.31 0.45 Driving: patient's opinion 60% 82% 56% 0.03 0.77 escort's opinion 57% 79% 53% 0.04 0.78 154 Monitored intravenous sedation with local anaesthesia for dental outpatients Part III 3.3 GENERAL DISCUSSION OF PART III types of therapy: drugs or behavioural treatment. Even when sedative agents are used, patient preparation will influence the effectiveness. The determination to use a sedative is often a reflection of the personal style of the dentist. Some patients strongly believe in the power of drugs. Others fear the effects of the drugs themselves, or fear the loss of control if they take a psychoactive drug. For example, some do not want their minds clouded by a mind altering drug. If the patient feels that dental treatment will be safe, and overall trust is high, but the patient is still scared, he or she is a good candidate for drug therapy. Patients who worry about the treatment not being safe, or exhibit a low level of trust, are again poor candidates (Milgrom and Weinstein 1993). This is in harmony with our finding that the phobia group’s acceptance for treatment under intravenous sedation with local anaesthesia was not as high as the others’. 3.3.1 The anxious patient Since its introduction in the late 1800s, the use of local anaesthesia has revolutionised the field of surgery. Today, local anaesthesia stands alone as the method of choice for pain control in dentistry. There are many reports on the relationship between fear and pain, but in general there are no mentions in the literature on other psychological factors that may influence the inadequacy of local anaesthesia. Because there is a close association between the memory of pain and expected pain, dental procedures causing pain - in connection with anxiety - constitute a major barrier to seeking dental care for some people (Vassend 1993). The patients in this study could not remember any significant unpleasant experiences, such as pain, during treatment. As a result, as many as half of the patients, even in the phobia group, subsequently made a new appointment with the dentist following this major and frightening operation. Previous studies have documented that patients' memories of dental pain may later turn into consistent anxiety (Kent 1984, 1985). The author believes that intravenous sedation may have prevented this as well as caused some relief from anxiety. If the dentist chooses drug therapy, it is still important to discuss the treatment with the patient: patients might be told that the drug is a relaxant and will make them feel more comfortable, and that the patient will loose cognition of time, and that after treatment, most patients do not remember any unpleasant episodes of the therapy. According to the author's clinical experience, many patients will decide after a few appointments Many clinicians believe they must choose between two quite different 155 Patients’ experiences that they no longer need the drug. This is extremely important: we can break the circulus vitiosum of anxiety. Clark et Rodrigo 1986, Rodrigo et Clark 1986). Previous psychometric studies, however, have failed to show any objective differences between these treatments (Barker et al. 1987). 3.3.2 Amnesia 3.3.3 Sedation and confusion Intravenous benzodiazepine administered in conscious sedation doses reduces significantly the affection and motivational component of the pain experience (Coulthard et Rood 1992) and will produce approximately 20 minutes of profound amnesia (Hupp et Becher 1988). Common experience shows that the injections of local anaesthetics form the only painful procedures during dental treatment. The author used the 20-minute period to perform local anaesthesia, and results show that the patients had no memory of this painful period. Although a continuous infusion of sedative produces better amnesia during the procedure than a bolus injection, it also prolongs the recovery time (Luyk et al. 1992). In private practices, rapid recovery is crucial. Most of the patients in this study received diazepam, and a minority midazolam. They did not receive a continuous infusion, though additional boluses were available in case of need. Midazolam has been shown to offer more advantages for the patient than diazepam, with a more rapid onset of sedation, less pain during injection, profound anterograde amnesia and fewer postoperative complications being the main features (Clark et al. 1987, Patient management and general anaesthesia are the techniques most commonly employed in the cases of dental care phobia and the frequency of the use of inhalation sedation varies according to the age of the patient as it is mainly used for treating children. Only 55% of dentists in general practice have any training in sedative techniques in the UK (Edmunds and Rosen 1989). Intravenous conscious sedation in combination with local anaesthesia is an alternative during unpleasant surgical and dental procedures, and in several cases can replace general anaesthesia. Monitoring as well as a trained staff make the methods safe and enable to reduce complications like hypoxia (Zoller and Zoller 1992, Luotio et al. 1993) The length and precision of certain implant surgery operations require the complete cooperation of patients (Charlton et al. 1991). Many mentally and/or physically handicapped and anxious dental patients do not receive adequate dental treatment because effective ways of supportive treatment are insufficiently known and/or available to dentists (BouvyBerends and Makkes 1990). The predominantly favourable response of the patients leads to the suggestion of 156 Monitored intravenous sedation with local anaesthesia for dental outpatients Part III using intravenous sedation with local anaesthesia even in minor oral surgery. (Kingon 1990) with spontaneously recovering patients, and they concluded that they could not allow the discharge of patients sooner than 1 hour after the injections. Moreover, the clinical experience of the author of this study has shown that, although the patients who suffer from dental care phobia are more confused after treatment than others and may need flumazenil, these very patients are possible candidates for the central nervous system-related side effects of this drug. However, the confusion will be relieved by itself during the hours to come: The patients felt confused for three hours only and did not need any observation the next morning (Tables 4 and 5 in study 5). Sedation and confusion are the two sides of the same patient management: we call it sedation when we want to relax the patient but confusion when we want to send him or her back home... It is possible to remove confusion or sedation with flumazenil, which appears to be a promising drug for reversing the conscious sedation by midazolam. The patient who receives flumazenil after intravenous midazolam is significantly more alert as early as after 5 min following drug administration. (Clark et al 1991) In cases of undue sedation persisting after dental treatment, flumazenil in doses from 0.5 to 1.0 mg rapidly reverses the sedative and amnesic effects of midazolam without apparent evidence of subsequent resedation. (Davies et al 1990) Flumazenil reverses almost totally the effects of mental sedation for approximately 2 hours but not physical sedation or memory (Ghoneim et al 1989, Cooper et al 1991). Flumazenil makes recovery in the supine position unnecessary and hence is a drug that should be included in the armamentarium of any emergency drug kit when benzodiazepines are used intravenously (Rosenbaum and Hooper 1988). Thomson (et al. 1993) have controverted this in their study where they found that psychomotor testing after flumazenil have revealed even poorer performance if compared 3.3.4 Postoperative pain The main disorders after the operation under intravenous sedation were tiredness and pain. The first does not require anything else but sufficient sleep. However, pain is a more complicated symptom and often overlooked by the doctor but easily relieved with more effective analgesics. At the time of this study the patients got a prescription for some non-steroidal anti-inflammatory drugs (NSAIDs) which inhibit peripheral prostaglandins. Today these drugs are the framework in the treatment of postoperative pain. Analgesic agents, with do not operate against peripheral prostaglandin synthesis (e.g. paracetamol), may also provide some pain relief. However, long-acting NSAIDs like piroxicam 157 Patients’ experiences have proved to be superior to paracetamol, which does not induce a complete relief from pain (Dolci et al. 1993). Because the patients are canulated, the use of parentheral analgesic is simple and advisable. The intramuscular dosage of ketorolac, a new NSAID, has shown a similar degree of pain relief to that of parentheral diclofenac. This safe and effective drug is an important new addition to the available intramuscular NSAIDs preparations. (Walton et al. 1993) Moreover, it is possible to enhance pain relief by combining analgesic agents with different drugs like opioids and NSAIDs (Dionne et al 1994). within dental surgery, although they are very effective. Local anaesthetics are not only effective for the termination of intraoperative pain but postoperative pain as well. They are useful for lengthy dental treatments and for the prevention of severe pain following many types of surgical procedures. However, the timing of normal short-acting local anaesthesia does not reduce the postoperative pain experience (Zacharias et al. 1993). It is an interesting point that the American patients of European origin have felt the pain less severe than those of American African or Latin origin (Faucett et al. 1994). More understandable is the fact that the increased rates of postoperative complications and a tendency for increased postoperative pain were found when the patients were treated by a general practitioner and not an oral surgeon. Even the number of days off work have been higher in these cases (Berge and Gilhuus 1993). Baxendale (et al.1993) have reported that the use of prophylactic oral dexamethasone is useful in reducing postoperative analgesia requirements. Similarly the injection of a slow-release methylprednisolone have reduced the frequency and intensity of postoperative pain (Kaufman et al. 1994). Neither of these corticosteroids nor long-acting local anaesthetics are in common use 158 Monitored intravenous sedation with local anaesthesia for dental outpatients Part III Parentheral medication with local anaesthetics is every-day practice in dentistry, but there must be a psychological barrier to prohibit the use of other parentheral drugs, although they could significantly reduce the patients' unpleasant experiences. 159 Patients’ experiences 3.4 Clinical There was more confusion in the phobia group than in the operation (control) group perhaps because the patients in this group received more sedative agents. It is possible to remove the sedation with flumazenil but the relatively high price of the product limits the use. Moreover, half of the patients felt both ready for work and vehicle driving, but because a great deal of them felt they were not capable of these activities, it is more than advisable to The most important reason for the disorders was the treatment itself (i.e. pain). After getting the results expressed in this study, the author changed the protocol of analgesic drugs. The previous tolfenamic acid - ibuprofen type therapy was abandoned and a single dose of intravenous ketorolac after operation and a subsequent prescription of long-acting piroxicam was introduced. After oral surgery the patients should also receive an opiate addition. Since the pain needs to be relieved and the most effective medications against pain contain opioids, the need for resting days may continue for several days. forbid all the patients to drive or work on the next day. Sedative premedication increases the need of sleep and the patient will rest more than normally on the first day after the treatment. As a conclusion it can be expressed that there are no severe problems after treatment under intravenous sedation if the problems are provided against during the procedure, the patient is domesticated with an adult escort and the patient is well medicated against pain. 160 Monitored intravenous sedation with local anaesthesia for dental outpatients Part III conclusions However, even in these cases, the author could carry the therapy through to the end without any objective difficulties. Most of the According to this study, the recollection of the treatment by the patients seems to be rather positive. Patients prefer sedation in major operations. patients felt only minimally uncomfortable experiences during the therapy under intravenous sedation. Some of the patients showing dental care phobia may need general anaesthesia. However, such patients accounted for only 10% of the phobia group. The authors' clinical experience has shown that mental problems, such as a previously diagnosed panic disorder or some psychiatric medications, may form relative contraindications for intravenous sedation. Nevertheless, if the patient is extremely scared, there is little that we could or can do to remove all anxiety. 161 Monitored intravenous sedation with local anaesthesia for dental outpatients Part IV PART IV CHALLENGES 163 Monitored intravenous sedation with local anaesthesia for dental outpatients Part IV 4.1 Survey 6 Advanced monitoring: Holter ECG and analysis of the status of autonomic nervous system 4.1.1 ABSTRACT This survey comprised 23 study group patients undergoing dental procedures under intravenous sedation and 12 control registrations of the University Clinic outpatients who underwent dental surgical operations without intravenous sedation. Patients were monitored with a Holter ECG recorder until the next morning. The tapes were reviewed with an arrhythmia analysis program allowing the detection of normal sinus beats and supraventricular and ventricular occurences. The heart rate variability analysis (HRV) was performed during surgery and also after the operation. The amount of cardiac occurences were within normal limits in both groups; the maximum pulse was suggestively lower in the study group and the high and low frequency components of heart rate variability were systematically and in recovery stage even statistically higher (p=0.05) in the study group, all indicating stress relief. Moreover, in many cases, the adverse reactions to local anaesthetic are psychogenic in nature. Fear of injection, or of dental treatment in general, may lead to some of the most frightening pseudo-allergic reactions tachycardia and vasodepressor syncope (Kleinhauz and Eli 1993). There is no oral surgical procedure without fear, pain and drugs, all of which may cause changes in the balance of the autonomic nervous system. The autonomic nervous 4.1.2 INTRODUCTION 4.1.2.1 Autonomic nervous system and fear The autonomic nervous system is activated by fear, which causes many clinical problems. There are changes in the patient’s heart rate, peripheral pulse volume, sweat activity and muscle tension as well as in steroid levels in blood (Berggren 1984). 165 Challenges system controls the visceral functions of the body e.g. body temperature, cardiac muscle, arterial pressure and respiratory function. Oral surgical procedures may change the balance to the activation of the sympathetic system and may also cause changes in respiratory habits. The activation of the sympathetic system prepares the body for physical activities through increasing heart rate and blood pressure (fight or flight). We also know that a powerful sympathetic activation may increase the risk for arrhythmias. and the function of cardiac branches. Holter also allows the studying of ischemic occurrences, which is the most promising character because for the dentist the easiest way to control the patient’s fear i.e. autonomic responses is sedation, but sedation always causes a risk of hypoxia. Arterial oxyhemoglobin saturation (SaO2) decreases regularly after the administration of a notable amount of any sedative agent. The decrease in the saturation level of oxygen is significant if sedation progresses from light to deep level. Age is positively correlated with desaturation, but a history of disease or medications have failed to be sensitive predictors of desaturation (Bilotta et al. 1990). The protracted half-lives of some benzodiazepines, and drug interactions, if opioids are used in combination with benzodiazepines, appear to be potential hazards in the elderly. Desaturation slightly below 90% may be clinically insignificant since no complications have been noted at this level (Berg JC et al. 1991, Bilotta et al. 1990). The use of Holter makes it able to detect real cardiac problems like ST-depressions derived from desaturation. Heart rate variability analysis has been documented to be a method for evaluating a risk of arrhythmia; it has also created interest for use as a monitoring method during and after surgery (Marsch et al 1994), but no method for simultaneous heart rate variability analysis is available. Moreover, more information is required on the relationship between the detected changes of autonomic status using HRV and real arrhythmia. At this moment the study of HRV as well as the documentation of brady- and tachycardias are most exclusively done on 24 hours Holter recordings. This makes it easy to evaluate the basal rhythm, heart rate and its changes as well as ectopias 166 Monitored intravenous sedation with local anaesthesia for dental outpatients Part IV recording the arrhythmia during operation and the following day. 4.1.2.2 The aim of the study The backroud of this survey was that powerful sympathetic activation may increase the risk for arrhythmias; the purpose of this survey was to analyse the changes in ECG and in the function of autonomic nervous system during and after oral surgery. The second aim is to define the need for ECG monitoring during operations under intravenous sedation. The third purpose is to evaluate the sympatho-vagal balance using a frequency-domain analysis of heart rate variability. The first aim of this survey is to investigate the safety of dental procedures under intravenous sedation with local anaesthesia by 167 Challenges 4.1.3 PATIENTS AND METHODS previous and present illnesses, allergies and medications. A dental care plan was drawn up and all the patients were referred to radiological examination (orthopantomograph) The patients were advised both verbally and in writing on how to prepare for intravenous sedation (for example, no food and no drink for four hours prior to treatment). 4.1.3.1 Patients: preparation, sedation and local anaesthesia 1. Study group: The research group consisted of 23 patients undergoing dental procedure under intravenous sedation at the author's private practice. The mean age was 48 years (SD 17). The patients underwent surgery primarily for implantological reasons, major conservative dental treatment, or extraction under sedation due to dental care phobia. The subjects were ordinary, private practice dental patients, who conformed to groups IIII of the ASA (American Association of Anaesthesiologists). None of the patients corresponded to the ASA groups IV - V. The patients were within the limits of generally accepted indications and contraindications as mentioned in the text books for dental anaesthesia and oral surgery. Patients were not given oral premedication, sedatives nor antibiotics on the day of the operation or the previous day. Blood pressure was recorded and monitoring with a pulse oximeter and Holter ECG initiated before the insertion of a peripheral venous cannula. After the insertion of the cannula, an infusion of 0.9% sodium chloride solution was started, and then the sedative agent was applied with a disposable syringe using the slow injection technique. Midazolam was used for sedation (Dormicum 5 ml inj. 1 mg/ml Roche). The benzodiazepine antagonist used was flumazenil (Lanexat 5 ml inj. 0.1 mg/ml Roche). Local anaesthesia was performed with lidocaine (Xylocain adrenalin 1.8 ml inj. 20 mg/ml+12.5 microgram/ml ASTRA) and prilocaine (Citanest Octapressin 1.8 ml inj. 30 mg/ml+0.54 microgram/ml ASTRA). After treatment the blood pressure was recorded again and after follow-up the venous cannula removed. The patients remained in the dental chair until the bleeding The patients were monitored with an Ohmeda pulse oximeter and with a Holter ECG recorder. The data from the pulse oximeter was collected with a Microsoft Works program using a Toshiba T1000SE computer. The analysis of the 24-hour electrocardiographic recordings is based on the Holter recordings. During the first examination, the patients completed a questionnaire on 168 Monitored intravenous sedation with local anaesthesia for dental outpatients Part IV following extraction had subsided and the patient felt well and was able to walk and dress without help. Patient preparation was similar than in the study group but when the patients were advised in writing on how to prepare for the operation it was mentioned that they should eat before the operation. This was the result of different preparation practices in the University clinic and the author's private office. The treatment room was equipped with dental unit, pulse oximeter, oxygen supplement unit and some resuscitation facilities, including endotracheal intubation equipment and medication for cardiopulmonary resuscitation. Both treatment periods were carried out by the same dentist, i.e. the author. Patients were not given oral premedication (e.g. analgesic drug) before operation. Blood pressure was recorded and Holter ECG initiated in the operation theatre immediately before operation. Local anaesthesia was performed with lidocaine (Xylocain adrenalin 1.8 ml inj. 20 mg/ml+12.5 microgram/ml ASTRA) or/and prilocaine (Citanest Octapressin 1.8 ml inj. 30 mg/ml+0.54 microgram/ml ASTRA). 2. Reference group The reference group consisted of 12 patients undergoing dental procedure without intravenous sedation. The mean age was 45 years (SD 15). Subjects were unselected University clinic patients, who were transmitted to the department of oral surgery with normal indications. They were all voluntary for survey and they conformed to groups I-III of the ASA (American Association of Anaesthesiologists). None of the patients corresponded to the ASA groups IV - V. Thus the patients were within the limits of generally accepted indications and contraindications for dental treatment. There were differences between patient preparation (eating instructions), cannulation and intravenous infusion and local anaesthesia i.e. in the underlying factors, but it is important to understand that this survey was not a controlled clinical trial but a clinical follow-up to compare two types of patient care i.e. a non-randomised survey. The treatment room was equipped with dental unit, pulse oximeter, oxygen supplement unit and some resuscitation facilities, including endotracheal intubation equipment and medication for cardiopulmonary resuscitation. These treatment periods were carried out by several surgeons. The patients were monitored only with a Holter ECG recorder. The analysis of the 24-hour electrocardiographic recordings were based on the Holter recordings. 169 Challenges 4.1.3.2 Monitoring There are no statistically significant differences in patient characteristics between the groups: Age had an effect on variables, but it is not a confounding factor in this survey. All of the Holter tapes in the study population were analysed using the Marquette 8500 scanner running version 5.7 of the Marquette arrhythmia analysis program allowing the detection of normal sinus beats and supraventricular and ventricular extrasystoles. After an automatic analysis of the tape, the data file was visually reviewed and manually corrected. Table 1. Patient characteristics in patients undergoing dental procedure under intravenous sedation (study group) and in patients without intravenous sedation (reference group) Study group (n=23) Sex (%) males Age (years) ASA Heart rate variability analysis was performed by running the Marquette heart rate variability analysis program. HRV analyses were performed using four consecutive minutes’ periods during surgery and the three following hours after the operation. Total power (TP) between 0 - 0.40 Hz along with the power in the low-frequency band (LF, 0.04 to 0.15 Hz) and in the high-frequency band (HF, 0.15 to 0.40 HZ) were calculated and logarithmically transformed. In addition to spectral components, also LF to HF ratios and normalised units were used as markers of sympatho-vagal balance during the different stages of operation and recovery period. Reference group (n= 12) 35% 50% females 65% 50% mean 48 45 SD 17 15 range 21-81 28-80 1 57% 83% 2 43% 17% 170 Monitored intravenous sedation with local anaesthesia for dental outpatients Part IV independent samples or MannWhitney U, test when appropriate, was used to compare the groups with respect to heart rate and HRV variables at the baseline, and with respect to the changes from baseline. 4.1.3.3 Statistical methods Mann-Whitney U test was used to compare the groups with respect to the number of cardiac occurences. Heart rate variability (HRV) analysis includes four variables to be analysed; total power (TP), lowfrequency band (LF) high-frequency band (HF), and the ratio LF/HF. These variables are expressed and analysed using logarithmic transformed values. T-test for Fisher's exact test was used to compare the patient groups with respect to nominal data. The data were analysed using SPSS statistical package (Version 6.1.3). 171 Challenges 4.1.4 RESULTS There was no depression of the heart rate variability (HRV) during or after the treatment. In the study group HRV was afterwards even at a higher level (Figure 1). At the baseline, there was a remarkable difference between the groups (table 6). The differences at the baseline were controlled by forming variables to express changes from baseline. The difference between the groups was significant in recovery stage (p<0.05) in HF and LF. The TP differed in all stages (p<0.05) except during local anaesthesia (table 7). None of the patients in either group had any meaningful arrhythmia during or after the treatment. The amount of extrasystoles were within normal limits. There is no significant difference between groups with respect to the occurrence or number of cardiac incidents (Tables 2,4 and 5). No ST-depressions indicating the hypoxia of cardiac muscle were detected, not even in the cases where pulse oximeter reported oxygen saturation under 85% (Table 3). 172 Monitored intravenous sedation with local anaesthesia for dental outpatients Part IV Table 2. The number of unknown but registered cardiac occurrences in both groups Study group Reference group Peroperative atrial premature complexes 1.9 SD 0.9 1.3 SD 0.6 Postoperative atrial premature complexes 2.4 SD 0.7 1.2 SD 0.5 Peroperative atrial tachycardias Postoperative atrial tachycardias 0.04 SD 0.04 0.08 SD .08 0.17 SD 0.14 - Peroperative ventric. prem. complexes Postoperative ventric. prem. complexes 0.17 SD 0.14 3.0 SD 2.0 1.2 SD 0.6 7.3 SD 7.3 Peroperative ventricular tachycardias Postoperative ventricular tachycardias - - - - ST-decrease - - T-inversion - - Table 3. The number of correction manoeuvres for respiratory problems: Oxygen delivery: peroperatively postoperatively Intravenous flumazenil: peroperatively postoperatively Long term recovery postoperatively Study group Reference group (n=23) (n=12) 3 2 - 5 - 2 - 173 Challenges Table 4. Peroperative and postoperative cardiac occurrences (%) in groups of patients undergoing dental procedure under intravenous sedation (study group) and in patients without intravenous sedation (reference group) Extra systoles Period arterial peroperative 43% 50% 0.74 postoperative 70% 50% 0.29 peroperative 9% 33% 0.15 postoperative 22% 50% 0.13 83% 92% 0.65 ventricular At least one cardiac incident (peroperative / postoperative) Study group (n=23) *Fisher's exact test 174 Reference p-value* group (n= 12) Monitored intravenous sedation with local anaesthesia for dental outpatients Part IV Table 5. Total number of peroperative and postoperative cardiac occurrences in groups of patients undergoing dental procedure under intravenous sedation (study group) and in patients without intravenous sedation (reference group) Study group Reference group (n=23) (n= 12) 1 1 IQR 0-2 0-5 range 0-21 0-30 2 1 IQR 0-6 1-3 range 0-14 0-50 2 2 IQR 1-11 1-8 range 0-23 0-80 p-value* Number of preoperative cardiac occurrences: Median 0.40 Number of postoperative cardiac occurrences: Median 0.60 All cardiac occurrences: Median * Mann-Whitney U- test 175 0.99 Challenges Table 6. Heart rate variability: HF, LF, TP and LF/HF during different periods of follow-up in patients undergoing dental procedure under intravenous sedation (study group) and in patients without intravenous sedation (reference group). Frequency Period Study group (n=23) Reference group (n= 12) pvalue HF* before operation local anaesthesia surgery recovery the next morning Mean 4.63 4.45 5.19 5.23 5.84 LF* before operation local anaesthesia surgery recovery the next morning 5.63 5.20 5.87 6.38 6.37 1.20 1.32 1.13 1.20 1.29 6.25 5.77 6.16 6.40 6.54 0.60 0.97 0.61 0.82 0.92 0.05 TP* before operation local anaesthesia surgery recovery the next morning 7.36 7.21 7.52 7.95 7.93 0.70 0.64 0.64 0.67 0.75 7.71 7.43 7.56 7.86 7.87 0.56 0.89 0.58 0.54 0.58 0.14 Median 3.73 2.83 2.51 3.63 1.77 IQR 1.33-4.93 1.47-4.57 1.40-3.54 1.74-5.04 1.16-4.34 Median 3.03 3.06 2.68 4.06 2.59 LF/HF** before operation local anaesthesia surgery recovery the next morning SD 1.30 1.30 1.25 1.25 1.41 Mean 5.13 4.68 5.37 5.11 5.48 SD 0.77 0.96 0.79 0.79 1.02 IQR 2.36-4.23 2.30-4.47 2.17-3.74 3.16-5.09 1.71-5.69 * logarithmic transformed values, t-test for independent samples ** in LF/HF, LF and HF are in original units, Mann-Whitney U-test. 176 0.07 0.78 Monitored intravenous sedation with local anaesthesia for dental outpatients Part IV Table 7. Heart rate variability: Mean in HF, LF, TP and LF/HF from baseline during follow-up in patients undergoing dental procedure under intravenous sedation (study group) and in patients without intravenous sedation (reference group). Frequency Period Study group (n=23) Reference group (n=12) pvalue H F* local anaesthesia surgery recovery the next morning Mean -0.18 0.56 0.59 1.21 SEM 0.18 0.14 0.17 0.31 Mean -0.45 0.24 -0.02 0.35 SEM 0.24 0.19 0.23 0.20 0.40 0.19 0.05 0.07 LF* local anaesthesia surgery recovery the next morning -0.43 0.25 0.75 0.74 0.21 0.15 0.17 0.25 -0.48 -0.08 0.16 0.29 0.24 0.19 0.22 0.19 0.88 0.20 0.05 0.24 TP* local anaesthesia surgery recovery the next morning -0.15 0.16 0.59 0.57 0.10 0.08 0.10 0.17 -0.27 -0.14 0.16 0.16 0.22 0.09 0.13 0.10 0.56 0.03 0.02 0.05 LF/HF** local anaesthesia surgery recovery the next morning Median -0.19 -0.72 0.23 -0.38 IQR -0.86-0.46 -2.03-0.02 -0.72-1.02 -2.79-0.18 IQR -0.91-0.87 -1.32-0.79 0.10-1.58 -1.62-2.34 0.89 0.31 0.14 0.09 Median -0.16 -0.26 0.63 0.26 * logarithmic transformed values, t-test for independent samples ** in LF/HF, LF and HF are in original units, Mann-Whitney U-test. SEM= standard error of mean IQR= inter quartile range 177 Challenges Table 8. Pulse rate during and after the operation in patients undergoing dental procedure under intravenous sedation (study group) and in patients without intravenous sedation (reference group). Heart rate Study group Reference group (n=23) (n=12) Mean SD Mean SD p-value* Maximum pulse: during operation 98.4 15.5 100.8 17.5 0.68 109.0 17.4 121.7 23.5 0.08 during operation 59.9 7.7 60.6 10.7 0.82 after operation 54.3 7.6 56.5 8.1 0.43 after operation Minimum pulse: *t-test for independent samples 178 Monitored intravenous sedation with local anaesthesia for dental outpatients Part IV Fig 1. The difference between the groups in total power. Higher score indicates the relief of symphatic activity (expressed in logarithmic scale: ln(ms2/Hz)). The non- sedated control patients are the first 12 patients on the left corner of the figure. The sedated patients are found on the right side. The time is expressed in z-axis: S1-S3; before operation S4-S5; local anaesthesia S6-S10; surgery S11-S15; recovery S16-; the next morning Heart rate variability (total power) 10 9-10 9 8-9 7-8 7 6-7 6 5-6 5 S19 4 S13 3 33 25 29 17 21 9 patients 4-5 3-4 2-3 S7 13 1 2 5 total pover 8 S1 179 Challenges 4.1.5 DISCUSSION reference group. The anxiety of nonsedated patients was a possible cause for the poorer performance of the reference group, but because this survey was not a controlled clinical trial and no statistical significance could be detected, the result is mainly suggestive. Moreover, no ST-segment depression indicating hypoxia was detected although several correction manoeuvres of oxygen level were performed in the study group, not even in cases who needed long-term recovery postoperatively. Thus no need for ECG monitoring during dental treatment under intravenous sedation was discovered. 4.1.5.1 Cardiac occurrences Psychological and physiological changes and pharmacological treatments during dental surgery have effects on circulatory and respiratory functions. The regulatory mechanisms, especially the autonomic nervous tone, are altered. Pain and anxiety can cause direct sympathetic activation. Changes in the normal breathing frequency and the tidal volume affect cardiac vagal input, which can be observed in reduced respiratory sinus arrhythmia. Local anaesthetic drugs containing epinephrine have direct systemic effects on the autonomic nervous system changing the balance toward sympathetic activation. Also, sedative drugs have significant effects on the regulation of respiration and circulation. Since the impairment of cardiac vagal modulation has been found to be associated with the electrical instability of the heart, also in dental surgery, susceptibility to arrhythmias is in theory increased. However, this survey shows that sedation rather prevents than provokes arrhythmias, especially the amount of ventricular premature complexes. Although no statistical significance could be found between the groups, not even in the peroperative occurrences (p=0.15), the most important finding is that the study group did not show any signs of poorer performance than the 4.1.5.2 Pulse Cioffi et al. (1985) concluded that routine restorative dental care with lidocaine and epinephrine local anaesthesia did not produce a clinically important haemodynamic response despite an increase in epinephrine levels. Frabetti et al. (1992) also found that patients who underwent surgical treatment had higher heart rate values than patients who underwent conventional therapy. Patients with muco-gingival surgery had the mean heart rate values of one hundred per minute while a group with scaling and root planing had the mean heart rate values of 78 beats per minute. According to a previous study by the author, the mean pulse of 180 Monitored intravenous sedation with local anaesthesia for dental outpatients Part IV the patient elevates from 70 beats to 86 beats per minute after the injection of epinephrine containing local anaesthetics (Survey 2). Meyer (1987) also found that the increase of heart rate and the alterations of blood pressure were different in a group with extraction than in a group undergoing local anaesthesia only, and that they are possibly an expression of an endogenous catecholamine release as a result to stress and not to a pharmacological effect. He also concluded that endogenous alternations always take place in the same way. 1985). The development of the equipment and analysis programs has enabled the increased importance of autonomic nervous tests in clinical cardiology during the last decade. Today most cardiologists prefer the heart rate variability analysis or baroreflex sensitivity testing to classical methods when they have to evaluate the risk for arrhythmia (Farrel et al. 1992). Clinical studies have shown that decreased heart rate variability will forecast higher risk for sudden cardiac death. This appears not only in the cases of medically compromised patients (Kleiger et al. 1987, Töyry et al. 1996) but healthy people as well (Tsuji et al. 1994). Similarly, as in during local anaesthesia a high heart rate indicates stress; when we are investigating the effect of sedation, a lower heart rate indicates stress relief. In this survey there was no statistical significance between the study and reference groups, although there were informative differences in the maximum pulse after surgery. The stress relief decreased the maximum pulse of the study group 13 counts per minute (p=0.08). This is in harmony with the other finding that intravenous sedation causes a decrease in sympathetic activation. The heart is well-supplied with both sympathetic and parasympathetic nerves which affect cardiac pumping in to ways: by changing the heart rate and through the strength of contraction. This stimulation on the S-N node illustrates the antagonism of these two systems. Norepinehrine released from sympathetic nerve endings stimulates an increase in the spontaneous rate of forming of the SA node. Controversially the acethylcholine decreases this rate. If the heart rate was constant at 72 beats per minute it could easily be described at a frequency of 1.2 Hz i.e. 833 ms. Since it is not truly constant, multiple frequency components comprise its make-up. 4.1.5.3 Heart rate variability The immediate influence of sympathetic activation has been directly linked to a higher risk for cardiac arrest as has been documented with an animal model (Schwartz et al. 1984, Bilman et al. In HRV the measurements are derived from the R-R intervals of the 181 Challenges ECG, and the connection of these intervals creates a rhythmic pattern. Research has demonstrated three discrete components in the frequency domain. The first is a low-frequency component (0.02-0.09 Hz) which constitutes the functions of thermoregulation and vasomotor tone and the renin-angiotensin control system all mediated by autonomic nervous system (Kitney and Rompelman 1977). The increase of the LF component appears as a result of parasympathetic activation (Kamath and Fallen 1993, Malliani et al. 1991). The second one is a midfrequency component (0.09-0.15 Hz) as a result of the baroreceptor reflex and regulation of blood pressure, and not of interest in this survey. The last one is a high-frequency (HF) component (0.15-49 Hz) and derived from respiration. These frequencies are present when the heart rate changes suddenly or as a result of respiration. Normal respiration rate is 10/min which is 0.17 Hz and this frequency will transfer into the highfrequency component. Moreover this frequency seems to be a marker of sympathetic function (Paganini et al. 1986, Hirsch and Bishop 1981). New methods for the quantification of autonomic nervous functions and the measuring of sympatho-vagal balance have made it possible to analyse the significance of these reactions: In this survey there were systematic differences between groups in both of these parameters and the difference was even statistically significant in the recovery period (p=0.05) immediately after treatment. Moreover, there were significant differences in total power (TP) at all stages except during local anaesthesia (p=0.05). These observations indicated that there was a remarkable increase in parasymphatic and/or decrease in symphatic activity in the study group. Moreover, the stress from local anaesthesia in both groups and the later stress relief especially in the study group is visible in figures 24, and in harmony with the finding that during local anaesthesia the groups did not differ from each other. 182 Monitored intravenous sedation with local anaesthesia for dental outpatients Part IV 4.1.6 Clinical conclusions Intravenous sedation decreases the activation of the sympathetic component, increases heart rate variability and decreases maximum pulse, indicating the need of sedation when cardiac patients are under dental surgery. The decrease of SaO2 as a result of intravenous sedation does not cause per- or postoperative unsatisfactory cardiac occurrences. No need for ECG monitoring during dental treatment under intravenous sedation was discovered. The safety of medically comprimised patients will increase as a result of stress relief. 183 Monitored intravenous sedation with local anaesthesia for dental outpatients Part IV 4.2 Study 7: Stress index 4.2.1 ABSTRACT In this descriptive study cardiovascular parameters indicating stress during treatment under intravenous sedation and local anaesthetic alone are described. Moreover the two local anaesthetic agents (lidocaine and prilocaine) and two vasoconstrictors (epinephrine and phelypressine) were observed. Amplitude of pulse wave was the most responsive measurable parameter. Amplitude of pulse wave diminished just before and during the injection as a result of vasoconstriction due to psychological stress. Blood flow showed the smallest values during the injection of local anaesthetic. Similarly, heart rate slightly decreased after the injection of prilocaine and phelypressine, but pulse rate increased after the epinephrine-containing lidocaine injection. Controversially both parameters increased after the injection of sedative agent: Pulse rate a little but amplitude of pulse wave showed a remarkable increase. To estimate the value of generic stress, a new index, the stress index was developed. When a subject suffers from generic stress, we can measure most significant cardiovascular changes, such as rising pulse rate and diminishing amplitude of pulse wave. By dividing the pulse rate by the amplitude of pulse wave (pulse / blood flow), a sensitive estimator for the stress is acquired, namely the stress index. causes more changes in the cardiovascular system (Hirota et al. 1992). Most studies have not noted any severe changes in heart rate or blood pressure when a local anaesthetic is used with epinephrine (Davenport et al. 1990). Montebugnoli et al. (1990) found that there were no significant differences in cardiovascular response when a group of patients under non-specific 4.2.2 INTRODUCTION It is important to identify the ideal balance of pain and anxiety relief when anxious patients are treated under intravenous sedation. The safety of epinephrine with dental local anaesthesia is well known. Epinephrine-containing lidocaine has little effect on haemodynamics, while norepinephrine-containing lidocaine 185 Challenges stress were given an anaesthetic with or without epinephrine. The cardiovascular response during dental stress may not be associated with the use of epinephrine in an anaesthetic solution. Individual reactions seem to dominate in certain cases (Montebugnoli et al. 1990, Meyer 1990). The increase in heart rate is reported to be rare and never by more than 10 beats per minute (Frabetti et al. 1992). However, every clinically experienced dentist knows that sometimes patients will develop unpleasant tachycardia if an anaesthetic containing epinephrine is used. effects of surgical stress on changes in polymorphonuclear leukocyte elastase (PMNE) levels; Poon (et al. 1995) have studied plasma corticol levels as well as catecholamine and glucose levels. Even beta-endorphin release has been found to indicate stress during surgery (Acosta et al. 1995). All of these methos need a blood sample and are therefore not suitable for dental practice because of lack of hospital blood laboratory. An example of noninvasive methods is the ascorbyl free radical monitored by electron spin resonance spectroscopy (Pietri et al. 1994). This method could be of great value in clinical practice in hospitals during e.g. open heart surgery, but it is absolutely impossible to apply in a dental practice. But how to measure the level of stress? We do have many indicators for stress. High systolic blood pressure, high pulse, and cold fingers (peripheral vasoconstriction) have been the most frequently used signs of stress. However, they are sometimes contradictory because the body tries to keep the homeostasis: a change in one parameter will cause a compensatory change in another parameter. Thus many attemps have been made to develop indicators for stress even during the last years. Noshima (et al. 1997) examined the Aim of the study The aim of this study was to discover whether sedative agents or vasoconstirctor containing local anaesthetic agents have any effects on cardiac parameters indicating stress when observed with pletysmographic pulse oximetry. 186 Monitored intravenous sedation with local anaesthesia for dental outpatients Part IV 4.2.3 PATIENTS AND METHODS 4.2.3.1 Study design 4.2.3.2 Monitoring This paper is a retrospective descriptive review of patient records of two individual study groups. There were many differences between patient preparation, cannulation and intravenous infusion and local anaesthesia i.e. in the underlying factors. The first study group comprised the authors’ private practice patients who had an operation under intravenous sedation with local anaesthesia. These patients were monitored with Datex Satlite Trans pulseoximeter. The second study group is formed of dental students who had a course exercise of local anaesthesia. Their cardiovascular parameters are monitored with Datex Cardiocap. Both equipment allowed the monitoring of the level of amplitude of pulse wave. It is important to understand that this study was not a controlled clinical trial but a clinical follow-up of normal treatment or exercise periods. Later revised databases formed the study material. Thus there was no indication of approval by an institutional review board governing human experimentation. Moreover, this study is completely descriptive, no statistical analysis in performed. During measuring the patients of the first group were monitored with SATLITE TRANS TM (Datex, Helsinki Finland) This pulse oximeter is a stand-alone, non-invasive, arterial oxygen saturation monitor. It gives continuous, real-time SaO2 and pulse rate readings. Follow-up information is available through both the analog and digital output ports. The subjects of the second group were monitored using a CARDIOCAP II CH-S (Datex, Helsinki Finland) multiparameter physiological monitor. This pulse oximeter is a stand-alone, noninvasive, arterial oxygen saturation monitor which can also monitor ECG and blood pressure. It gives continuous, real-time SaO2 and pulse rate readings. Follow-up information is available through both the analog and digital output ports. Both pulse oximetric equipment function using light which is generated in the finger probe and passes through the tissues. The total absorption of the light depends on the absorbing components: tissues, venous blood and the pulsating arterial blood. Different amounts of light are absorbed by oxygenated haemoglobin (HbO2) and unoxygenated or reduced haemoglobin (Hb). The oximeter 187 Challenges measures the relative absorption by Hb and HbO2 of red light at 660 nm and infrared light at 910 nm in Cardiocap. Ohmeda uses 660 and 949 nm wavelengths. These two different forms of haemoglobin allow different amounts of light to pass through at these wave lengths. The oximeter converts this relative light intensity information into arterial oxygen saturation values. 4.2.3.3 Patients The first study group is based on the retrospective review of patient records comprising 26 registrations of 26 of the author's private outpatients who underwent dental operations under intravenous sedation with local anaesthesia. Patients had some oral surgical operations or they underwent large conservative dental treatment or extraction under sedation because of dental care phobia. From this base group five patients were selected and their parameters combined to represent the changes. These cases were selected because the time table of the different parts of their treatments were identical enough and their amplitude of pulse wave was on a sufficient level. The treatment was divided into five periods as described in table 1. The maximal pulse rate was determined during every period. The pulsation of the arterial blood flow modulates the light passing through it, and the oximeter converts this light intensity information into pulse rate values, which are presented together with SaO2 values on a monitor screen. The pulse wave is derived from the intensity of the transmitted light. The pulsating blood flow in the finger is the result of left ventricle contraction of the heart, which fills the vascular bed of the finger with arterial blood. It is important to understand that the pulse wave reflects changes in blood volume, not changes in blood pressure. During the first examination, the patients completed a questionnaire on previous and present illnesses, allergies and medications. A dental care plan was drawn up and all the patients were referred to radiological examination (orthopantomography). The patients were advised both verbally and in writing on how to prepare for intravenous sedation (for example, no food or drink for four hours prior to treatment).They were in good health and had no severe systemic diseases (in the classification of American Society of Anaesthesiology ASA I - II i.e. no The monitors were connected directly to the serial port of a Toshiba T1000SE portable computer for realtime collection of data by a collection program ("KERÄÄ" by Dr Matti A.K. Mattila). The program recorded numerical values from Cardiocap at 10 seconds intervals. A finger probe was used for pulse oximetric registration, i.e. blood oxygen saturation (SaO2). The probe was placed on the subject's right middle finger. 188 Monitored intravenous sedation with local anaesthesia for dental outpatients Part IV systemic diseases or only a moderate disease which does not limit activity). pulse oximeter initiated before the insertion of a peripheral venous cannula. After the insertion of the cannula, an infusion of 0.9% sodium chloride solution was started, and the sedative agent was then applied with disposable syringe using the slow injection technique. The treatment room was equipped with dental unit, pulse oximeter, oxygen supplement unit and some resuscitation facilities, including endotracheal intubation equipment and medication for cardiopulmonary resuscitation. All treatments were carried out by the same dentist, i.e. the author. The second study group consisted of twenty dental students. The students were between 19 and 31 years of age with a mean age of 22.5 years (SD 3.22); 80 % were females. Each person accepted in the test group had to be healthy and free of any surgical risk corresponding to the ASA (American Society of Anaesthesiologist) I or II groups. Oral contraceptives were the commonest medication (three of females). One subject was undergoing a thyroxin substitution therapy for hypothyreosis. No other illness or permanent medication was reported. 4.2.3.5 Local anaesthesia The study was done during a normal local anaesthesia course for students. This provided an opportunity to allow the students to practice local anaesthesia, to demonstrate cardiovascular effects thereto and to collect objective measurable findings. In the first study group local anaesthesia was performed with a lidocaine-epinephrine combination (Xylocain adrenalin 1.8 ml inj. 20 mg/ml + 0.0125 mg/ml, ASTRA) and a prilocaine-phelypressine combination (Citanest Octapressin 1.8 ml inj. 30 mg/ml+0.54 microgram/ml ASTRA). Lidocain mean 88 mg (range 40-100) and additional prilocain 60 mg only in one case. 4.2.3.4 Sedation Sedation was performed only in the first study group and midazolam was used for sedation (Dormicum 5 ml inj. 1 mg/ml Roche), Midazolam mean 5.7 mg, (range 7-5 mg). After treatment, most of the patients (16 cases) received 30 mg ketorolak (Toradol inj. 30 mg/ml, Syntex) injection for analgesics via venous cannula. Blood pressure was recorded again and the venous cannula removed. The patients stayed in the dental chair, and pulse oximetric monitoring was continued until bleeding after extraction had Patients were not given oral premedication, sedatives nor antibiotics on the day of the operation or the previous day. Blood pressure was recorded and monitoring with a 189 Challenges stopped and until the patients felt well and were able to walk and get dressed without help. The patients left the clinic with an adult escort. maxilla; the dose was also 4 x 1.8 ml. The amount of anaesthetic corresponded to 144 mg of lidocaine and 90 mcg of epinephrine. The mean time taken for the injection of the 4 cartridges was 2 min 11 seconds (SD 24.6 seconds) (Table 2). In the second study group local anaesthesia was performed with a lidocaine - epinephrine solution (Xylocain adrenalin 1.8 ml inj. 20 mg/ml+12.5 mcg/ml ASTRA) and a prilocaine - phelypressine solution (Citanest Octapressin 1.8 ml inj. 30 mg/ml+0.54 mcg/ml ASTRA). The doses were 80 mg lidocaine and 120 mg prilocaine. The site of injection was the upper jaw, the buccal sulcus just distal of the second upper molar. Both sides of the maxilla were anaesthetised. This site was chosen because there is room for a large enough volume of local anaesthetic, and the trifurcation of the trigeminal nerve is near the anaesthetised area. Patients were in a horizontal position during the infiltration of local anaesthetic. 4.2.3.7 Statistical methods The values of amplitude of pulse wave (A.P.W.) are not suitable for a statistical analysis in real life treatment conditions, since they are too sensitive to external conditions, e.g. room temperature. Because there is no solid base level of that parameter measured from individual patients, only the means were calculated and these values are represented in the graphics, but no statistical analysis has been performed. The scheme for the stress index (S.I.) is: S.I. = pulse / amplitude of pulse wave 4.2.3.6 Timing of the procedure During the appointment, the subjects received 4 cartridges (4 x 1.8 ml) of Citanest-Octapressin, corresponding to 216 mg of prilocaine and 3.89 mcg of phelypressine, injected submucosally 5 minutes after beginning the pulse oximetric measurement. The subjects received two cartridges of CitanestOctapressin to the right side and two cartridges of the same agent to the left side. Ten minutes later, they received two cartridges of Xylocain adrenalin to both sides of the Systolic and diastolic BP, pulse, and SaO2 were measured before, during and after injection. The changes were tested using paired ttest or Wilcoxon matched pairs test, when appropriate. Spearman rank correlations were calculated to study whether the individual change in stress index (=pulse/APW) is correlated with the change in other variables. The data were analysed using SPSS statistical package (Version 6.1.3). 190 Monitored intravenous sedation with local anaesthesia for dental outpatients Part IV Table 1. Treatment periods in which cardiovascular parameters were observed in the first study group. Name of period Description Duration 1. Waiting (Before) Patient in the chair before cannulation 5 - 10 minutes 2. Sedation After cannulation but before local anaesthetic injections 5 - 10 minutes 3. Local anaesthesia Injections of local anaesthetic agents 5 - 10 minutes 4. Treatment Operative period: incisions, drilling, extraction, sealing, fillings, etc. 15 - 30 minutes Table 2. Timing of the procedure with each patient in the second study group. Time (min) Intervention 0 min start of measurement 5 min starting of the first injection: 4 cartridges of Citanest-Octapressin 15 min starting of the second injection: 4 cartridges of Xylocain adrenalin 25 min end of measurement 191 Challenges 4.2.4 OBSERVATIONS In both study groups, amplitude of pulse wave (A.P.W.) was the most reactive of the measurable parameters. Amplitude of pulse wave observations depend not only on biological and measurement variations but also on temporal variations in clinical circumstances. Standardising the circumstances to reduce the environmental variations (e.g. room temperature) or to include these circumstances as covariates was not possible during the treatments or during a local anaesthesia course, and therefore the findings should be regarded as tentative. by amplitude of pulse wave (pulse / blood flow), and a new index, the stress index was obtained. This is a very responsive estimator for stress. The stress index (pulse rate/A.P.W.) shows the maximal effect of stress relief 5- 15 minutes after the injection of benzodiazepine in the first study group. Local anaesthesia and treatment will increase stress. After the injection of lidocaine-epinephrine there was an additional stress period 5 - 10 minutes later as the epinephrine began to spread to the blood stream from the injection area. Epinephrine induced stress relieved approximately 20 minutes after first injection. Three stress peaks were found: cannulation, the epinephrine reaction and the treatment. (fig 1, table 3) Similarly, in the second study group the prilocaine-phelypressine injection had only one stress point: at the moment of injection, but after the injection of lidocaine-epinephrine, there was an additional stress period 5 - 10 minutes later, when the epinephrine began to spread to the blood stream from the injection area (fig 2, table 4). No end point of epinephrine induced stress is visible in the figure, because the measuring was stopped 10 minutes after the lidocaine-epinephrine injection. A.P.W. will rise after the injection of benzodiazepine and afterwards the local anaesthesia will cause some vasoconstriction. A single dose of benzodiazepine produced an effective vasodilatation which remained for 45 minutes in the first study group. In general A.P.W. decreased towards the injection due to psychological stress. Blood flow showed decreasing values during and after the injections of local anaesthetic. Similarly, in the second study group the blood flow showed the smallest values during the injection of local anaesthetic with both methods (fig 2). The difference in baseline-levels, a decrease of 8 units, can be interpreted as a consequence of reduced stress. The statistical test of the stress indicating parameter (tables 5-7) showed that no statistically significant indicator is available. To estimate the value of stress, the pulse rate (fig 1 and 2) was divided 192 Monitored intravenous sedation with local anaesthesia for dental outpatients Part IV Only the stress index may be trend setting. Although there is a correlation in changes in other parameters vs. stress index (table 8), the level of change is without clinical significance. 193 Challenges Fig 1. Stress index after the injection of midazolam. Stress index is calculated by dividing the pulse rate by the amplitude of pulse wave. Five measurements are in combination so that the injections of midazolam occur at the same time; two minutes after the beginning. The cannulation is clearly visible at the left corner. Lidocaine and epinephrine are injected 15-30 minutes later i.e. in the left mid portion of the 46 minutes scale. The effect of treatment remains for 30-46 minutes. Stress Figure 1 4,5 4,0 3,5 3,0 2,5 2,0 1,5 1,0 0,5 0,0 sedation 2 4 6 local anaest. treatment 8 10 12 14 16 18 20 22 24 26 28 30 32 34 36 38 40 42 44 46 Time 194 Monitored intravenous sedation with local anaesthesia for dental outpatients Part IV Fig 2. Stress index during local anaesthesia. Prilocaine-phelypressin is injected five minutes and lidocaine-epinephrine 15 minutes after the beginning. Both injections are visible in the curve but the later injection caused a constant elevation of the value. F ig u r e 2 Stress 4 ,5 4 ,0 3 ,5 3 ,0 2 ,5 2 ,0 1 ,5 1 ,0 0 ,5 0 ,0 0 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 T im e 195 Challenges Table 3. Heart rate, amplitude of pulse wave and stress index after the injection of midazolam. Stress index is calculated by dividing the pulse rate by the amplitude of pulse wave. Time (Min) 2 4 6 8 10 12 14 16 18 20 22 24 26 28 30 32 34 36 38 40 42 44 46 Period and effect Cannulation Injection of sedative Sedative effect Sedative effect Sedative effect Sedative effect Sedative effect Sedative effect Local anaesthesia Epinephrine effect Epinephrine effect Epinephrine effect Epinephrine effect Epinephrine effect Treatment begins Operation effect Operation effect Operation effect Operation effect Operation effect Operation effect Operation effect Operation effect Pulse Mean 79,0 86,8 88,0 86,3 84,2 84,1 85,0 83,2 85,7 86,0 86,7 87,2 85,5 86,2 89,4 90,0 90,3 89,1 87,5 87,2 86,9 84,0 83,0 196 A.P.W. Mean 28,5 46,5 65,7 74,3 83,7 82,7 84,1 80,9 66,0 52,0 48,8 55,9 52,7 52,5 33,3 36,4 43,9 37,5 40,5 38,2 30,8 30,5 27,3 Stress Index Mean 2,8 2,0 1,3 1,2 1,0 1,0 1,0 1,0 1,3 1,7 1,8 1,6 1,7 1,7 2,7 2,5 2,1 2,4 2,2 2,3 2,9 2,8 3,1 Monitored intravenous sedation with local anaesthesia for dental outpatients Part IV Table 4. Heart rate, amplitude of pulse wave and stress index during local anaesthesia. Stress index is calculated by dividing the pulse rate by the amplitude of pulse wave. Time (Min) 0 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 Period and effect Waiting Waiting Waiting Waiting Waiting Injection of prilocaine Phelypressine effect Phelypressine effect Phelypressine effect Phelypressine effect Phelypressine effect Phelypressine effect Phelypressine effect Phelypressine effect Phelypressine effect Injection of lidocaine Epinephrine effect Epinephrine effect Epinephrine effect Epinephrine effect Epinephrine effect Epinephrine effect Epinephrine effect Epinephrine effect Epinephrine effect Pulse Mean A.P.W. Mean 76 77 76 79 79 76 74 72 73 74 74 73 74 75 76 76 77 82 86 88 87 86 85 84 84 40 40 37 34 32 22 25 32 35 32 27 28 27 25 20 20 21 21 22 23 23 22 21 22 20 197 Stress index Mean 1,9 1,9 2,1 2,4 2,5 3,5 3,0 2,3 2,1 2,3 2,7 2,6 2,8 3,0 3,9 3,9 3,7 3,9 3,9 3,8 3,8 4,0 4,0 3,8 4,2 Challenges Table 5. Systolic and diastolic blood pressure, pulse, Sao2, APW, and stress index 2-3 minutes before injection, during injection and after injection. A: B: C: Before injection of During injection of After injection of local anaesthetics local anaesthetics local anaesthetics Systolic BP 125 SD 10.9 125 SD 14.5 126 SD 13.2 Diastolic BP 71.3 SD 8.4 71.0 SD 7.8 70.7 SD 7.1 Pulse 76.5 SD 16.1 76.2 SD 15.1 72.4 SD 15.1 SaO2 97.4 SD 0.99 97.1 SD 1.2 97.4 SD 0.8 APW 23.0 SD 22.7 22.9 SD 23.9 27.3 SD 25.7 3.3 SD 11.7 7.8 SD 8.4 5.6 SD 4.3 Stress index Table 6. Mean changes in systolic and diastolic BP, pulse, Sao2, APW, and stress index from A to B and B to C. From A to B p-value From B to C p-value* Systolic BP -0.05 0.98 +0.65 0.79 Diastolic BP -0.35 0.86 -0.25 0.89 Pulse -0.30 0.93 -3.75 0.38 SaO2 -0.25 0.43 +0.30 0.33 APW +0.1 0.99 -4.4 0.43 Stress index +4.5 0.43 -2.2 0.12 *) Paired T-test A, B, C as in Table 5. 198 Monitored intravenous sedation with local anaesthesia for dental outpatients Part IV Table 7. Changes in APW and stress index from A to B and B to C From A to B p-value Median IQR From B to C p-value* Median IQR APW -0.50 -13 to 9 0.78 +1.00 -5 to 13 0.45 Stress index -0.22 -5 to 3 0.77 -1.06 -3 to 0.2 0.09 *) Wilcoxon matched pairs test A, B, C as in Table 5. Table 8. Correlation (r, Spearman rank correlation) between the changes in stress index versus the changes in other variables Stress index vs. from A to B p-value r from B to C p-value r Systolic BP -0.12 0.63 +0.61 0.004 Diastolic BP -0.48 0.03 +0.44 0.05 Pulse -0.33 (0.15) +0.22 (0.21) SaO2 +0.15 0.53 -0.07 0.78 APW -0.74 -0.78 (<0.0001) (0.0002) (In brackets: result of the scheme of the stress index: Pulse/APW) A, B, C as in Table 5. 199 Challenges 4.2.5 DISCUSSION induced stress is visible approximately 20 minutes after the first injection. It can be concluded that local anaesthesia and treatment increase stress. 4.2.5.1 Stress during treatment Under generic stress of any subject we can measure the most significant changes in a rising pulse rate and the decrease of A.P.W. A good indicator for evaluating stress during operation is the "stress index" i.e. pulse rate per A.P.W.. The stress index shows the maximal effect of stress relief 5- 15 minutes after injection of benzodiazepine. A single dose of benzodiazepine produced effective vasodilatation which remained for 45 minutes. This amount of time is sufficient for unpleasant manoeuvres in dental treatment. Observing the A.P.W. enables the dentist to notice that there is constriction in the peripheral arteries as a result of psychological stress: The elevation in the heart rate due to exogenic as well as endogenic epinephrine during and after the local anaesthetic injection was clearly visible. Blood flow showed diminishing values during the injection of local anaesthetic before any possible cardiovascular effect, and similarly later after the injection as a result of these cardiovascular occurrences. It is assumed that the reason for the first change was the psychological stress before injection. After the injection of lidocaineepinephrine there was an additional stress period 5 - 10 minutes later when the epinephrine began to spread to the blood stream from the injection area. The end point of epinephrine 4.2.5.2 Amplitude of pulse wave (A.P.W.) Observing the amplitude of pulse wave enables the dentist to notice constriction in the peripheral arteries as a result of psychological stress: The blood flow of the finger shows diminishing values before the injection of local anaesthetic i.e. before any possible cardiovascular effect. A pulse oximeter probe is usually placed on a finger; other alternatives are toe or earlobe. These alternative locations are equally suitable as a finger when measuring oxygen saturation and pulse rate, but they do not indicate the reactions in the pulse wave amplitude. In general, peripheral arteries in fingers react to painful stimuli much stronger than arteries in other places (Mattila et al 1990). However, the finger causes serious problems as a site for measuring because the deviations of the detected values will increase to a levels which fade out of statistical significance (table 5). Quite naturally, the absorption of infrared light is relative and dependent on the thickness of the finger being different in individual 200 Monitored intravenous sedation with local anaesthesia for dental outpatients Part IV fingers. Consequently the reliability of the pulse wave amplitude recording requires that the recording site is not changed. Because of the relativity of amplitude it is important to have a basis for comparison (Mattila et al 1989). In practice this means that when monitoring sedation, recording should be started before cannulation. injection of a sedative agent, as a result of feeling good. The amplitude of the pulse wave is the most informative indicator of changes in circulation, and CARDIOCAP II CHS allows us to observe this parameter. An observation of the amplitude of pulse wave might reveal that there is a constriction in the peripheral arteries resulting from psychological stress. The blood flow in this study showed the smallest values during the injection of local anaesthetic, before any possible cardiovascular effect. The author has observed vasoconstriction in patients if the treatment is carried out in a cool operation room, where patients may feel cold. This also has a closing effect on peripheral arteries, which may often cause measuring failures due to a low signal (Survey 3). Pulse oximetric measuring seems to work properly only in cases where the patient is comfortable. However, a few false desaturation registrations in pulse oximetry obviously do not harm the patient, and possible measuring failures do not allow us to abandon patient monitoring in the operation theatre. Some confusion seems to exist between direct arterial blood pressure and visible pulse wave because they are very similar in shape. Their information is, however, totally different. A visible pulse wave means practically that blood is circulating in the site of measurement. During normal sinus rhythm consecutive pulse waves are uniform, but during arrhythmia they can continuously vary in size and shape. In fact, these observations can be applied also to evaluate the importance of that particular arrhythmia for circulation (Mattila et al 1989, Mattila 1990). 4.2.5.3 Amplitude of pulse wave and the measuring equipment The regulation of peripheral arterial circulation is under the control of the autonomic nervous system. Vasoconstriction is induced by a stimulation of the smooth muscles of arterioles. This decreases the amplitude of the pulse wave and may be due to some discomfort such as pain, fear, low temperature or hypovolaemia. Rapid and strong vasodilatation is often seen after the In most other pulse oximeters these changes in amplitude are automatically corrected before being shown in the display. This, of course, helps the operator, because no manual correction is needed, but at the same time one very informative parameter is lost when anxious patients are being treated. Other parameters, for example the crest time and closing 201 Challenges time of the aortic valve, are available on screen, and even some arrhythmia can be verified. the finding of Veit et al. (Veit et al. 1993) where maximum ST-segment depression (indicating hypoxia in cardiac muscle) in the electrocardiogram was recorded 11 minutes after infiltration. Moreover, in survey 2 there was different baselevel in the stress index in methods 1 and 2. This can be explained with the reduced level of fear on the second exercise appointment. 4.2.5.4 Stress index There was a clear elevation in the heart rate due to exogenic and endogenic epinephrine during and after the local anaesthetic injection. It is assumed that the reason for this was psychological stress before injection and the relief of the stress after injection. To estimate the value of the physiological stress, a new index, the stress index was developed. When a subject suffers from generic stress, the most significant cardiovascular changes can be measured, such as rising pulse rate and diminishing amplitude of pulse wave. However, the values of amplitude of pulse wave are too sensitive to external conditions and to the variation of the basic levels of this indicator between patients. Consequently the "the stress index" is only a descriptive indicator and it is useful only when we want to measure the changes of the sympathetic status of one individual patient. The prilocaine-phelypressine injection had only one stress point: at the moment of injection. After the injection of lidocaine-epinephrine, there was an additional stress period 5 - 10 minutes later, when the epinephrine began to spread to the blood stream from the injection area. The end point of epinephrine induced stress could not be determined because the follow-up time was too short. This may explain During treatment the stress index shows the maximal effect of stress relief 5- 15 minutes after the injection of benzodiazepine. A single dose of benzodiazepine produced an effective vasodilatation which remained for 45 minutes. This time is sufficient for unpleasant manoeuvres in dental treatment. Observing the A.P.W. enables the dentist to notice the constriction in the peripheral arteries as a result of psychological stress: The elevation in the heart rate due to exogenic as well as endogenic epinephrine during and after the local anaesthetic injection was clearly visible. Blood flow showed decreasing values during the injection of local anaesthetic before any possible cardiovascular effect, and similarly later after injection as a result of these cardiovascular occurrences. It could be assumed that the reason for the first change was the psychological stress before injection. After the injection of lidocaineepinephrine there was an additional stress period 5 - 10 minutes later when the epinephrine began to spread to the blood stream from the injection area. The end point of epinephrine 202 Monitored intravenous sedation with local anaesthesia for dental outpatients Part IV an operation or treatment with the stress index, i.e. pulse rate per amplitude of pulse wave. But the equipment itself does not express this parameter. Thus it needs calculations during treatment, which decreases the clinical value of this parameter. induced stress is visible approximately 20 minutes after the first injection. But is it possible to conclude the self-evident fact that local anaesthesia and treatment increase stress when observed with some cardiovascular parameter? To test this hypothesis, a statistical test of the stress indicating parameter (tables 5-7) was performed. The test included three observation periods: before, during and after injection. It could be assumed that there should be some increase of stress during injection and some relief after it. The test showed that no statistically significant indicator for stress is available. Only the stress index may be trend setting (p=0.09). Although there is correlation in changes in other parameters vs. stress index (table 8), the level of change is without clinical significance. This study was not a clinical trial, but two clinical follow ups with two individual study designs. Moreover, there were differences in the underlying factors and the study was non-randomised. Therefore it is not justified to conclude that we should always monitor the stress of the patient. However, this study showed that it is possible measure the level of stress, and this may be necessary when medically compromised patients are under treatment. Therefore further research is needed to validate the new stress index. It can be concluded that it might be possible to evaluate stress during 203 Monitored intravenous sedation with local anaesthesia for dental outpatients Part IV 4.2.6 Clinical conclusions The best indicator for evaluating stress with pulse oximeter during an operation or treatment is amplitude of pulse wave or stress index, i.e. pulse rate per amplitude of pulse wave. The problem is that there is no constant base level; during the operation the elevation of the index is only an indicator. This study showed that it is possible to measure the level of stress, and this may be necessary when medically compromised patients are treated. Stress itself is not an adverse reaction but often predominates them. 205 Monitored intravenous sedation with local anaesthesia for dental outpatients Part IV 4.3 Study 8: Complicated cases 4.3.1 ABSTRACT This case study describes cases of the early detection of hypoxia with pulse oximeter during intravenous sedation with local anaesthesia. These patients are selected from previous two study groups which are further described in studies 1 and 6. The first signs of hypoxia were seen through pulse oximetry. In the first study group, two of the patients were treated with a surgical operation and one patient underwent a large conservative dental treatment under sedation because of dental care phobia. During the dental treatment period, external oxygen was added for all the three patients to avoid more complications as a result of hypoxia. Two of the patients also received an injection of benzodiazepine antagonist. One patient needed further follow-up but none of the patients developed additional complications. As a conclusion, pulse oximetric monitoring was discovered extremely sensitive as a predictor for coming complications as well as allowing early intervention in ventilation problems. In the last study group, five cases were found who developed long-standing low oxygen saturation levels which were detected with pulse oximeter. Three cases were solved by administering supplementary oxygen and/or benzodiazepine antagonist. However, two cases needed a long period of recovery afterwards. The lowest SaO2 levels of these patients were found during the postoperative period. Attempts were made to solve the problems related to hypoxia by administering supplementary oxygen, benzodiazepine antagonist and ventilation stimulates but without any improvement. The role of poor amplitude of pulse wave in these cases is discussed. 207 Challenges 4.3.2 INTRODUCTION Hardeman et al (1990) have found that twenty percent of sedated patients experienced hypoxic episodes in the postanaesthetic recovery unit when no supplemental oxygen was administered. Only three percent of patients who received supplemental oxygen had episodes of hypoxia. They recommended the use of supplemental oxygen for all patients undergoing intravenous sedation. Short episodes of hypoxia may be of little consequence in healthy patients (Rodrigo and Rosenquist 1988), but in compromised patients early detection may avoid serious complications. The principal aim of monitoring during procedures is patient safety. It is not so much a question of "life or death" but of the quality of care in general. Many of the principles in monitoring accepted in the anaesthesia for general surgery can be applied also in dental operative care. Patient monitoring is used in order to detect dangerous deviations from normal in circulation and respiration. These complications may be due to therapeutic procedures or the medication used, but they can also result from a deterioration of the patient’s own organic disease. It should be extremely important to recognise these occurrences in due time, to be able to make right conclusions for beginning correct therapeutic manoeuvres. On the basis of these observations and conclusions the surgeon is also able to adequately inform the patient on the event. Without appropriate monitoring these goals can certainly not be reached. Aim of the study The aim of this study was to describe hypoxia cases, their causes and the necessary treatments after this most recurrent complication. 208 Monitored intravenous sedation with local anaesthesia for dental outpatients Part IV 4.3.3 PATIENT MANAGEMENT AND METHODS The three first cases were selected from the material of the first study. The other cases are from the original unselected patient material of survey 6. Two years fall between these treatment periods, and much had been learned but the complications were there like they always are. However, pulse oximetric equipment was still the same: Ohmeda Biox 3740. detected with pulse oximeter and which forced the sedationist to make corrective manoeuvres. In most cases mild respiratory depression was corrected with intravenous flumazenil postoperatively (five patients). Three of the subjects had received supplementary oxygen previously during the procedure. Two of these needed a long-term recovery afterwards. Five cases in the last study group (survey 6) developed long-standing low oxygen saturation which was 209 Challenges 4.3.4 OBSERVATIONS 4.3.4.1 CASE 1. FIG. 1 The patient was a 28 years old female student who had a medication of amitriptylin hydrochloride (Pertriptyl, ORION) and tematsepam (Tenox, ORION) for depression. She also had atopic eczema without any medication. Moreover, she was highly overweight (160 cm, 98 kg) and a cigarette smoker. She underwent a large cariological and periodontological therapy with intravenous sedation. At first she received 20 mg diazepam without any sedative effect. The dose was duplicated with a low sedation effect. Before medication the SaO2 was 95%, and after 92%. External oxygen (3 l/min) was added during the dental treatment period. After treatment the nasal oxygen cannula was removed and the SaO2 fell to the level of 88%. As a result, the patient received a 0,5 mg injection of flumazenil and another 0,5 mg with isotonic NaCl infusion during the following hours. After the patient had received the previously mentioned amount of benzodiazepine antagonist, SaO2 remained within normal limits. The patient spent the following night under nurse supervision and connected into the pulse oximeter. Figure 1 210 Monitored intravenous sedation with local anaesthesia for dental outpatients Part IV 4.3.4.2 CASE 2. FIG. 2 The next patient was a 45-year old female housekeeper, 56 kg in weight, without any disease or medication. The treatment was an implantation into the right side of the upper jaw with a sinus lift operation, and into the molar area in the right side of the mandible with a revision of the mandible nerve. 7,5 mg midazolam was used for sedation. After 10 minutes the SaO2 fell under 90%. 40 minutes late, external oxygen was added and 0,5 mg flumazenil was injected. 40 minutes later again, while the mandibular nerve was prepared, the saturation suddenly decreased to a level under 80%. The patient was again medicated with 0,5 mg flumazenil; as a result the SaO2 rose extremely quickly back to 100%. The patient left the clinic with adult supervisor after the treatment. Figure 2 211 Challenges 4.3.4.3 CASE 3. FIG. 3 The last patient was a 81-year old female pensioner ( 64 kg ) without any medication or known disease. Some previous operations had been done. The operation this time (1993) was an implantation into the anterior area of the lower jaw. The dose of the sedative agent was 2.5 mg midazolam. The patient fell immediately into deep sleep. External oxygen was added again; as a result, the saturation of oxygen in blood rose from 83% to 97%. After one hour the operation was over and the oxygen cannula removed without any complications. Figure 3 212 Monitored intravenous sedation with local anaesthesia for dental outpatients Part IV 4.3.4.4 CASE 4 FIG 4 The patient was a 24-year old female barkeeper, 60 kg in weight, suffering from some undiagnosed chronic nasal problems without medication. She expressed a fear of the operation. She underwent a third molar surgery combined with an upper front teeth implantation under intravenous sedation. At first she received 8.0 mg midazolam with normal sedative effect. During the dental treatment period, one and a half hours after premedication, external oxygen (3 l/min) was added. After the treatment the SaO2 fell under the level of 90%. As a result, the patient received a 0,5 mg injection of flumazenil and another dose of 0,5 mg with an isotonic NaCl infusion during the following hour. After the patient had received the previously mentioned amount of benzodiazepine antagonist, SaO2 still remained below normal. She was then given a slow injection of 0.25mg salbutamol with no effect. The patient spent the following 8 hours under nurse supervision, connected into the pulse oximeter in the local hospital. She was domesticated before night. The possibility of peripheral vasoconstriction remained open. Case 4 100 90 Pulse and SaO2 80 70 60 SaO2 50 Pulse 40 30 20 10 0 Tim e 213 Challenges 4.3.4.5 CASE 5 FIG. 5 The patient was a 20-year old female student, 54 kg in weight, without any disease or medication, but she had considerable dental care phobia. The treatment was a third molar operation. 8 mg midazolam was used for sedation. There were no problems or complications during the treatment. After the operation, one hour later, the SaO2 fell under 90% and external oxygen was added. 0,5 mg flumazenil was injected and another dose of 0,5 mg with an isotonic NaCl infusion during the following hour, without any improvement of measured low oxygen saturation level. She was then given a slow injection of 20 mg doxapramic hydrochloride (respiratory stimulant) without any effect. A diagnosis of peripheral vasoconstriction was done because the equipment showed a low signal and neither the flumazenil nor doxapramic corrected the saturation values. Although the SaO2 remained at 86-87%, the patient was fully ordinated and felt in good condition of health. In conclusion, the symptoms appeared after operation but they did not complicate the procedure. The only real problem was the need of long-term recovery. After the treatment the patient stayed in the dental chair, and pulse oximetric monitoring was continued until all attempts to correct the oxygen saturation were shown to be ineffective. The patient desired to be sent home and she left the clinic under adult supervision. Case 5 140 Pulse and SaO2 120 100 80 SaO2 60 Pulse 40 20 0 Tim e 214 Monitored intravenous sedation with local anaesthesia for dental outpatients Part IV It is possible to cancel sedation with flumazenil and a fall in saturation can be corrected by administering supplementary oxygen. 215 Challenges Figure 6. The range of saturation in the described cases as a percentage of total time. Figure 6 35 % 30 % 20 % 15 % Case Case 4 Case 3 Case 2 5 84 86 88 90 94 0% 92 SaO2 96 5% 98 100 10 % 216 Case 1 Percent 25 % Monitored intravenous sedation with local anaesthesia for dental outpatients Part IV Table 1. The range of saturation in the described cases as a percentage of total time. SaO2 Case 1 Case 2 Case 3 Case 4 Case 5 100 0% 31 % 12 % 4% 6% 99 0% 8% 33 % 14 % 12 % 98 0% 2% 10 % 6% 8% 97 2% 3% 9% 4% 4% 96 6% 10 % 5% 8% 6% 95 6% 9% 11 % 3% 4% 94 16 % 5% 11 % 2% 2% 93 16 % 6% 3% 1% 2% 92 10 % 6% 2% 3% 6% 91 10 % 5% 2% 5% 6% 90 10 % 4% 2% 3% 4% 89 6% 5% 1% 2% 8% 88 11 % 4% 1% 17 % 9% 87 6% 1% 0% 21 % 11 % 86 2% 1% 0% 8% 4% 85 0% 0% 0% 0% 6% 84 0% 0% 0% 0% 4% 217 Challenges 4.3.5 DISCUSSION the intravenous agent divided into small parts (1 mg midazolam). This almost barely effective dose is repeated every 2 or 3 minutes until a minor decrease (2 - 3 %) in blood oxygen saturation is detected. The incidence of saturation falling to less than 90% have been between 4% and 40%, depending on the level of sedation (Tay et al. 1991, Hardeman et al. 1990). 4.3.5.1 Respiratory problems and oxygen Intravenous sedation has been shown helpful in avoiding cardiovascular reactions in oral surgical operations, but there is a risk of provoking respiratory depression. This adverse effect can easily be detected at an early stage, where the pulse wave and / or a fall in saturation is signalled visually and can be corrected by administering supplementary oxygen. There is also a significant decrease in the saturation level of oxygen as the patient progresses from light to deep sedation. The intravenous diazepam and midazolam have been shown to decrease oxygen saturation by 3% compared to the preoperative level, when administered in the average dosages of 6.4 mg and 3.3 mg respectively. (Matthews et al. 1992). However, even unsedated patients who only have treatment under local anaesthesia have a small postoperative fall in oxygen saturation (Matthews et al. 1992). Lowe and Brook (1991) have reported oxygen saturation in the range of 93-89% in some patients undergoing third molar removal with local anaesthetic alone. Ventilation hazards of intravenous midazolam may appear in the elderly, and the use of benzodiazepines with lower hypnogenic effects is recommended (Heinze et al. 1992). The author used Hardeman et al. (1990) found that 20% of sedated patients experienced hypoxic episodes in the postanaesthetic recovery unit when no supplemental oxygen was administered, while only 3% of patients who received supplemental oxygen had such episodes. They recommend the use of supplemental oxygen for all patients undergoing intravenous sedation in oral surgery. However, if dental patients are monitored with pulse oximetry, and an ultra-slow technique is used with careful dosage in the administration of sedative agents, no continuous oxygen supplement is necessary routinely (Read-Ward 1990), although it should be available. No routine oxygen supplement was used with the patients in this study. The minor decrease in SaO2 was used as a sign of sufficient sedation during the initiation of sedation, and oxygen was added when the 90% level lasted a long time. However, this supplementary oxygen did not correct 218 Monitored intravenous sedation with local anaesthesia for dental outpatients Part IV the "hypoxia" in every case. In fact, only in one case of five it was alone effective. suffer from dental care phobia are more confused after treatment than others and may need flumazenil, the very patients are possible candidates for central nervous system related side effects of this drug. The confusion will relief by itself during the following hours but flumazenil should mainly be used in the cases of low pulse oximeter values to diagnose the real condition of the patient. In these five cases, it was used four times. In one case the corrective treatment was successful and in three cases it enabled to suspect the wrong detection of hypoxia. 4.3.5.2 Antidote for correction the hypoxia It is possible to cancel sedation with flumazenil, which appears to be a promising drug for reversing midazolam conscious sedation. The patient who receives flumazenil after intravenous midazolam is significantly more alert as early as at 5 min following drug administration (Clark et al 1991). In cases of undue sedation persisting after dental treatment, flumazenil in doses from 0.5 to 1.0 mg rapidly reverses the sedative and amnesic effects of midazolam without an apparent evidence of subsequent resedation (Davies et al 1990). Flumazenil reverses almost totally the effects of mental sedation for approximately 2 hours, but not physical sedation or memory. (Ghoneim et al 1989, Cooper et al 1991) Flumazenil makes recovery in the supine position unnecessary and moreover it is a drug that should be included in the armamentarium of any emergency drug kit when benzodiazepines are used intravenously (Rosenbaum and Hooper 1988). This study showed that flumazenil is needed to remove confusion in the cases of low oxygen saturation and to diagnose real hypoxia from other, vasoactive problems. However, the clinical experience of the author has already shown that, although the patients who 4.3.5.3 Wrong detection of hypoxia The highest oxygen saturation of arterial blood (SaO2) detected in the patients were of course at the beginning of measuring. The lowest SaO2 levels were found some minutes after the injection of sedative agents or later during the treatment period. The study of White et al. (1989) showed that nearly half of the patients developed clinically significant desaturation during minor oral surgery under local anaesthesia. They assumed that this might be due to breath-holding or peripheral vasoconstriction as a response to anxiety or fear. This study may explain those observations. There may have been 219 Challenges false alarms as a result of poor amplitude of pulse wave. False alarms may explain even Lowe's and Brook's (1991) finding that every fifth patient undergoing surgical removal of third molar with local anaesthesia alone experienced hypoxic periods during surgery. The easiest way to avoid these alarms is to keep the patient warm by covering him or her with a blanket which allows better amplitude of pulse wave. Of course it is possible to block this autonomic vasoconstriction reaction with local anaesthetic injected into the patient’s finger (Eastwood 1992, Sakurada et al. 1995) but when treating a scared patient it is advisable to avoid such painful operations. Moreover, an alarm delay lasting 12 to 30 seconds would prevent most false alarms (Pan and Gravenstein 1994). of the pulse wave is the most informative indicator of the changes in circulation. (Part I, article 3) In most equipment - as in this case the Ohmeda pulse oximeter - these changes in amplitude are automatically corrected before expressed in display. This of course helps the operator as no manual correction is needed, but at the same time one very informative parameter is lost if anxious patients are treated. And we know that the equipment needs the pulsating component of the pulse to work properly. Automatic correction of the amplitude of pulse vawe may prevent us to find the decrease in amplitude of pulse wave and create wrong trust in the equipment. This was the problem in these cases because Ohmeda pulse oximeter was used. This equipment does not express the level of A.P.W., it only indicates the low quality of signal. The regulation of peripheral arterial circulation is controlled by the autonomic nervous system. Vasoconstriction is induced by the stimulation of smooth muscles of arterioles. This decreases the amplitude of pulse wave and may be due to some discomfort like pain, fear, low temperature as well as hypovolaemia. (Mattila et al. 1990) Vasodilation is often seen after the dosage of sedative agent as a result of feeling good. This reveals one alternative to correct low-signal problems: To add sedative. But there is no sedationist who will do this while the oximeter is warning about low saturation values. During pulse oximetric observation the amplitude In order to reach the quality level of the individual tailoring of premedication a simple monitoring method is needed for the monitoring and evaluation of patients' anxiety, the efficacy of premedication as well as the influences of premedication on the course of anaesthesia. Michael Johnstone showed already in 1976 in his monograph named "Adult preoperative medication" that pulse plethysmography can well be applied for the estimation of premedicant effects. Despite of its obvious advantages, plethysmographic pulse wave was practically used only by few. Since that time 220 Monitored intravenous sedation with local anaesthesia for dental outpatients Part IV plethysmographic pulse wave registration has become available for most instances, because pulse wave is an intrinsically essential part of pulse oximetry recording. haemoglobin due to medication with nitrites or even due to smoking habits, but the described cases, with one exception (Case 1), did not smoke or have any medication. Patients who have higher anxiety score have smaller pulse wave amplitude. This difference is seen also during maximal vasodilatation. (Mattila et al. 1990) Does this mean that patients who are anxious of anaesthesia have different (more vasoconstriction) vasomotor behaviour also during their normal life? Saumet et al (l986) observed that changes in skin thermal clearance correlated well with the amplitude of the plethysmographic wave. A cold surrounding can of course partly account for the vasoconstriction detected in the patients, but environmental circumstances were similar for all patients. The pulse oximeter may give incorrect SaO2 readings in the presence of abnormal One explanation for the false positive detection of hypoxia in dental operations is the so-called peripheral cyanosis or Raynaud's disease; a condition in which the mechanism is peripheral vasoconstriction and delayed peripheral circulation due to sympathetic activation. This leads to the desaturation of capillary haemoglobin although central circulation is well maintained. Women are affected five times more often than men and the age of presentation is between 20 and 40 years (Wilson et al 1991). This is in harmony with the authors’ experience and the fact that all these cases have been females. 221 Monitored intravenous sedation with local anaesthesia for dental outpatients Part IV 4.3.6 Clinical conclusion Intravenous sedation may be helpful in avoiding cardiac reactions during oral surgery, but there is a risk of provoking respiratory depression. This reaction can be corrected by administering supplementary oxygen and/or flumazenil. Wrong positive detection of hypoxia appears in particular situations. Flumazenil should be available in the cases of low pulse oximeter values to diagnose the real condition of the patient. 223 Monitored intravenous sedation with local anaesthesia for dental outpatients Part V PART V 225 Monitored intravenous sedation with local anaesthesia for dental outpatients Part V 5 GENERAL DISCUSSION AND CONCLUSIONS 5.1 Detection of adverse reactions recognition of initial 2-3% SaO2 decrease with pulse oximetry during the initiation of the sedation. The main purpose in evaluating the patient with pulse oximeter is to detect the changes in blood oxygen level early, which is a life maintaining function. Adverse reactions in this parameter is hypoxia. Arterial oxyhemoglobin saturation (SaO2) is lower after the administration of a notable amount of sedative agents. There is also a significant decrease in the saturation level of oxygen as the patient progresses from light to deep sedation. The incidence of saturation falling to less than 90% have been reported to have been between 4% and 40%, depending on the level of sedation (Tay et al. 1991, McKee et al. 1991, Hardeman et al. 1990), which is an interesting finding. Large amounts of sedatives were used in survey 1 but the desaturation incidence was only slightly over 10 %. It is possible that the relatively low incidence of desaturation in this study is a result of the early Since the largest mean decrease in oxygen saturation observed during procedures under intravenous sedation is less than that considered normal during sleep, some investigators are of the opinion that oximetry monitoring is not needed. Likewise the high incidence of desaturation does not cause adverse outcomes or complications. (Berg et al. 1991, Bilotta et al. 1990) However, in this study a small decrease of SaO2 was found to be a sign of sufficient sedation during the initiation of medication. Oxygen was added when the 90% level lasted a long time. The pulse oximeter is valuable because it will react immediately to any progressive oxygen desaturation, making early correction possible. Hence the use of pulse oximetry should be obligatory for all endoscopic or paediatric patients during intravenous sedation (Casteel et al. 1990), and it is also 227 General discussion and conclusions useful as a respiratory monitor during oral surgery (Sugiyama et al. 1991). It can be said that low initial saturation may be a warning signal of hypoxia and that the use of a monitor may help to determine the correct sedation level earlier and easier than the normally used ptosis i.e. eye closure reaction. hundred per minute, while the group undergoing scaling had mean heart rate values of 78 beats per minute. In this study, the mean pulse rate of the patient rose from 70 to 86 beats per minute after the injection of local anaesthetics containing epinephrine. Meyer (Meyer 1987) also found that the increases in heart rate and alterations of blood pressure were different in a group undergoing extraction and in a group to whom only only local anaesthesia had been administered, and these differences are possibly an expression of an endogenous catecholamine release as a result of stress rather than a pharmacological effect. He also concluded that endogenous alterations always take place in the same way. It has also been found that there is a temporary blood pressure increase during the injection of local anaesthetic (21,19) and at the time of extraction of a tooth (Meyer 1987). Also, heart rate had two peak values during the extraction of the tooth; the first during the injection of the local anaesthetic, and the second during the extraction phase (Meyer 1987). There may also be some increase in systolic blood pressure (Gortzak et al. 1992a). However, no clinically significant change could be detected in this study in either systolic or diastolic blood pressure. This means that the only parameter necessary to monitor after local anaesthesia is pulse, and the pulse oximeter is the equipment of first choice for this purpose. 5.2 Effects of local anaesthetic preparations Local anaesthetic preparations do not affect blood oxygen saturation in the clinical meaning but it was quite astonishing that in survey 2 there was a statistically significant decrease (0.1 - 0.3%) in this parameter. It is most important to understand in this particular case that the statistical significancy depends on the amount of measurements, it does not have any clinical meaning. The study by White et al. (White et al. 1989) showed that nearly half of the patients developed clinically significant desaturation during minor oral surgery under local anaesthesia. White et al. assumed that this might be due to breath holding or peripheral vasoconstriction as a response to anxiety or fear. This study at least excluded the effect of local anaesthesia. Frabetti et al. (Frabetti et al. 1992) found that patients undergoing surgical treatment had higher heart rate values than patients undergoing conventional therapy. Patients undergoing muco-gingival surgery had mean heart rate values of one 228 Monitored intravenous sedation with local anaesthesia for dental outpatients Part V parameters were found, whether the agents were combined or not. Thus there is no reason to avoid this combination which does not harm a healthy patient anyhow. 5.3 The use of two local anaesthetic preparations in combination This is a subject which has almost completely been ignored in previous studies. Simcock (et al. 1994) studied this with a combination of lidocaine 2% and bupivacaine 0.5%, and a combination of lidocaine 2% and prilocaine 1%. Patient evaluation of discomfort during the administration of the anaesthetic and during operation was assessed on a visual analogue scale but no statistically significant difference between groups was found. Similarly the subject is studied concerning the quality of motor block: the mixture of bupivacaine and lidocaine was less effective than the other combinations, of which the mixture of bupivacaine and prilocaine showed the best motor block. The combination of the two long-acting local anaesthetics bupivacaine and etidocaine had the longest effect (Keckeis et al. 1994). The most interesting point in these findings is that the lidocaineprilocaine combination had an equal effect to bupivacaine combination, although bupivacaine is a long-acting local anaesthetic preparation. This is in synergy with the author’s finding that combining lidocaine and prilocaine enables the time increase of local anaesthesia (Luotio et al. 1997). Moreover, the existence of EMLA (Astra®), the only ointment for skin surface anaesthesia which contains this combination, is indicating potentiation. In the present study no differences in cardiovascular 5.4 Effects of benzodiazepines vs. local anaesthetics Benzodiatzepines cause the decrease of SaO2 and the epinephrine in local anaesthetics increase the heart rate. Thus they do not affect the same parameter. Moreover, the different local anaesthetic preparations have different actions: according to the retrospective review of patient records in survey 2, the maximal pulse of the patient elevates from 91.3 beats to 98.6 beats per minute after the injection of epinephrine containing local anaesthetics but if a prilocainephelypressine injection is used only one stress point is found: at the moment of injection. After the injection of lidocaine-epinephrine there was an additional period of high pulse 5 - 10 minutes later when the epinephrine began to spread to the blood stream from the injection area. The parameter which was affected by both sedation and local anaesthesia was amplitude of pulse wave (A.P.W.). Observing the amplitude of pulse wave enables the dentist to notice a constriction in the peripheral arteries as a result of psychological stress: the blood flow of the finger shows diminishing values before the injection of local 229 General discussion and conclusions anaesthetic i.e. before any possible cardiovascular effect. A pulse oximeter probe is usually placed on a finger; other alternatives are toe or earlobe. These alternative locations are equally suitable as a finger when measuring oxygen saturation and pulse rate, but they do not indicate the reactions in the pulse wave amplitude. In general, peripheral arteries in fingers react to painful stimuli much stronger than arteries in other places (Mattila et al 1990). Therefore a pulse oximeter with a finger probe and a possibility to observe this parameter allows to observe the main difference: local anaesthetic preparations will cause vasoconstriction and diminishing values of A.P.W. but sedatives cause vasodilatation and elevating values. However, such patients accounted for only 10% of the phobia group. The authors' clinical experience has shown that mental problems, such as a previously diagnosed panic disorder or some psychiatric medication may form relative contraindications for intravenous sedation. However, even in these cases, the therapy could be carried through without any objective difficulties. Most patients felt only minimally uncomfortable experiences during therapy under intravenous sedation with local anaesthesia. Nevertheless, if the patient is extremely scared, there is little that can be done to remove all anxiety. Intravenous benzodiazepine administered in conscious sedation doses reduces significantly the affection and motivational component of the pain experience (Coulthard et Rood 1992) and will produce approximately 20 minutes profound amnesia (Hupp et Becher 1988). Common experience shows that the injections of local anaesthetics form the only painful procedures during dental treatment. The author used this period of time to perform the local anaesthesia, and results show that the patients had no memory of this painful period. As a result, as many as half of the patients - even in the phobia group - subsequently made a new appointment with the dentist following this major and frightening operation. Previous studies have documented that patients' memories of dental pain may later turn into consistent anxiety (Kent 1984, 1985). There is a strong indication in this 5.5 Patients' reactions to treatment under intravenous sedation with local anaesthesia Afterwards the level of preference for intravenous sedation with local anaesthesia among the different types of peroperative anaesthesia was extremely high, over 80% in every group. The reason for this was that the patients could not remember any significant unpleasant experiences, such as pain, during treatment. According to this study, the recollection of the treatment of the patients treated under intravenous sedation with local anaesthesia seems to be rather positive but some of the patients showing severe dental care phobia may need general anaesthesia. 230 Monitored intravenous sedation with local anaesthesia for dental outpatients Part V study that intravenous sedation may have prevented this as well as caused some relief from anxiety. Moreover, it is possible to enhance pain relief by combining analgesic agents with different drugs like opioids and NSAIDs (Dionne et al 1994). After getting the results expressed in study 5 the author changed the protocol of analgesic drugs. The previous tolfenamic acid ibuprofen type therapy was abandoned and a single dose of intravenous ketorolac after operation and a subsequent prescription of longacting piroxicam was introduced. After oral surgery the patients should also receive on opiate addition. Since pain needs to be relieved and the most effective medications against pain contain opioids, the need for resting days may continue for several days. 5.6 The patient’s condition after treatment under intravenous sedation with local anaesthesia The main disorders after an operation under intravenous sedation with local anaesthesia were tiredness and pain. The first does not require anything but sufficient sleep. However, pain is a more complicated symptom and often overlooked by the doctor, but easily relieved with more effective analgesics. At the time of this study the patients got a prescription for some non-steroidal anti-inflammatory drugs (NSAIDs) which inhibit peripheral prostaglandins. Today these drugs are the framework in the treatment of postoperative pain. Analgesic agents, which do not operate against peripheral prostaglandin synthesis (e.g. paracetamol), may also provide some pain relief. However, longacting NSAIDs like piroxicam have proved to be superior to paracetamol which does not induce a complete relief from pain (Dolci et al. 1993). Because the patients are canulated, the use of parentheral analgesic is simple and advisable. Intramuscular dosage of ketorolac, a new NSAID, has shown a similar degree of pain relief to that of parentheral diclofenac. This safe and effective drug is an important new addition to the available intramuscular NSAIDs preparations (Walton et al. 1993). 5.7 Arrhythmias and the status of autonomic nervous system This study shows that sedation rather prevents than provokes arrhythmia, especially the amount of ventricular premature complexes. Although no statistical significance could be found between the groups, not even in the peroperative occurrences (p=0.15), the most important finding is that the study group did not show any signs of poorer performance than the reference group. The anxiety of nonsedated patients was a possible cause for the poorer performance of the reference group but because this study was not a controlled clinical trial and no statistical significance could be detected, the result is mainly suggestive. Today most cardiologists 231 General discussion and conclusions prefer the heart rate variability analysis or baroreflex sensitivity testing to classical methods when they have to evaluate the risk for arrhythmia (Farrel et al. 1992). Clinical studies have shown that decreased heart rate variability will forecast higher risk for sudden cardiac death. This appears not only in the cases of medically compromised patients (Kleiger et al. 1987, Töyry et al. 1996) but healthy people, too (Tsuji et al. 1994). The increase of the low frequency component appears as a result of parasympathetic activation (Kamath and Fallen 1993, Malliani et al. 1991). Moreover, high frequency seems to be a marker of sympathetic function (Paganini et al. 1986, Hirsch and Bishop 1981). New methods for the quantification of autonomic nervous function and measuring sympatho-vagal balance have made it possible to investigate the significance of these reactions: in this study there were systematic differences between the groups in both of these parameters, and the difference was even statistically significant in the recovery period (p=0.05) immediately after treatment. These observations indicated that there was a remarkable increase in parasymphatic and/or decrease in symphatic activity in the study group. term recovery postoperatively. Thus no need for ECG monitoring during the dental treatment under intravenous sedation was found. 5.8 False alarms in pulse oximetry An SaO2-artefact or false alarm is here described as extensive fall in SaO2 readings without any organic reason such as breathing failure or obstructed airways (Fig. 4). The study of White et al. (1989) has showed that nearly half of the patients developed clinically significant desaturation during minor oral surgery under local anaesthesia. They assumed that this might be due to breath-holding or peripheral vasoconstriction as a response to anxiety or fear (White et al. 1989). This retrospective review of patient records explains those observations: poor amplitude of pulse wave (A.P.W.) has caused false alarms. Even Lowes and Brooks' (1991) finding that every fifth patient undergoing surgical removal of third molar with local anaesthesia alone experienced hypoxic periods during surgery, is explained by false alarms. The influence of local anaesthetics to oxygen saturation has been studied by the author. In a previous study the saturation values were no more than 0,5 % lower (statistically insignificant) than the base level at the end of the measurement. Local anaesthesia is a possible source of measuring failures (Fig. 4) because it causes vasoconstriction but the agents used in local anaesthesia do not affect Moreover, no ST-segment depression indicating hypoxia was detected although in the study group several correction manoeuvres of oxygen level were performed; not even in the cases that needed long232 Monitored intravenous sedation with local anaesthesia for dental outpatients Part V the level of the patient’s oxygen saturation. The easiest way to avoid these false alarms is to keep the patient warm. 5.9 Complicated cases The most important complication resulting from intravenous sedation is too low level of SaO2 and it is treated by correcting respiratory function with supplementary oxygen and removing sedation with antidote. Hardeman et al. (1990) found that 20% of sedated patients experienced hypoxic episodes in the postanaesthetic recovery unit when no supplemental oxygen was administered, while only 3% of patients who received supplemental oxygen had such episodes. They recommend the use of supplemental oxygen for all patients undergoing intravenous sedation in oral surgery. An interesting alternative is that the level of sedation is too light and psychological stress keeps the periphery closed. If this is correct, it shoud be possible to remove false alarms by increasing the amount of sedatives. But it is hardly likely that any sedationist would give more of an agent which may cause respiratory depression while the oximeter is warning about possible hypoxia! One explanation for the false positive detection of hypoxia in dental operations is the so-called peripheral cyanosis or Raynaud's disease; a condition in which the mechanism is peripheral vasoconstriction and delayed peripheral circulation due to sympathetic activation. This leads to the desaturation of capillary haemoglobin although central circulation is well maintained. Women are affected five times more often than men and the age of presentation is between 20 and 40 years, which is in harmony with the authors’ experience (Wilson et al 1991). Sedation can be cancelled with flumazenil, which appears to be a promising drug for reversing midazolam conscious sedation. The patient who receives flumazenil after intravenous midazolam is significantly more alert as early as at 5 mins following drug administration (Clark et al 1991). In cases of undue sedation persisting after dental treatment, flumazenil in doses from 0.5 to 1.0 mg rapidly reverses the sedative and amnesic effects of midazolam without apparent evidence of subsequent resedation (Davies et al 1990). Flumazenil reverses almost totally the effects of mental sedation for approximately 2 hours, but not physical sedation or memory. (Ghoneim et al 1989, Cooper et al 1991) 233 General discussion and conclusions groups have only been too limited in those cases. More important is that we should not believe all differences which could be shown to have statistical significance, e.g. in these studies there was statistically significant decreases in SaO2 after local anaesthesia: 0.5 percent units! Nevertheless, even the dentist’s experience brings the indication in proportion with real life conclusions. However, many of the results have been so marked that they indicate further studies. 5.10 Statistical view vs. clinical view The whole work is mainly descriptive because the statistics of real life treatments is quite complex. Because the material used originated form the dentist’s practical work and not a statistically perfect sample, the data in every case is distorted. The further analysis of an underlying factor does not bring any further benefit because the possibility of the effect of these underlying factors can never be excluded within this study framework. Clinically the author has reached a high level in patient monitoring in European dental tradition: the use of monitoring and sedation methods have been applied in dentistry and oral surgery which are widely used in anaesthesiology and critical care. These methods will cause an elevation in patient safety which is, of course, the main issue. In medical science the clinical view should always be in the first place and the statistics giving support to the observations. It is not that much the question of occurrences or symptoms when we are not able to show statistical significance although some difference might have a high clinical significance: The study 234 Monitored intravenous sedation with local anaesthesia for dental outpatients Part V 5.11 Conclusions A pulse oximeter is very sensitive in detecting adverse reactions. High pulse, if not detected, cause most of the problematic conditions of the patient in the dental office. When sedatives are used, the main deorientation is hypoxia and oversedation. Pulse oximetry often prevents them. Controversially, local anaesthetics are not causing the decrease in blood oxygen saturation but especially epinephrine in these preparations may cause high pulse levels which, combined with fear as mentioned, may lead to vasovagal problems or even harm a medically compromised patient. However, the high level of pulse rate can be avoided e.g. by combining the lidocaine and prilocaine preparations when epinephrine containing preparations do not produce sufficient anaesthesia in therapeutical doses. Moreover, an early detection of rising pulse with pulse oximeter will prevent complications. However, fear, cold and external epinephrine together and alone cause peripheral vasoconstriction whereas sedatives open the periphery. This controversial effect of sedatives and symphatomimetics should be remembered during sedation because the vasoconstriction will cause artefacts to measurements. Intravenous sedation is the method of patients’ choice in oral surgery and even in cases of dental phobia, although the preference is a little bit lower among the latter. After treatment the only seriously disturbing disorder was pain, which should be avoided with proper analgesia. The studied sedative method is simple to monitor with pulse oximeter alone because it does not cause cardiac problems but rather prevents them by decreasing the activity of the symphatetic component of autonomic nervous system. During the sedation the main problem is the low level of oxygen saturation which in certain cases may be long-standing but can be corrected with external oxygen and/or flumazenil. There is also a risk of false detection of hypoxia i.e. the condition of patient is good but the monitor indicates problems. This condition can be diagnosed from cold fingers and the ineffectiveness of correction manoeuvres, and it is most easily avoided by preventing the patient from shivering with cold. 235 Monitored intravenous sedation with local anaesthesia for dental outpatients Part VI PART VI 6. CLINICAL GUIDELINES 237 Monitored intravenous sedation with local anaesthesia for dental outpatients Part VI INTRAVENOUS SEDATION PROTICOL 239 Monitored intravenous sedation with local anaesthesia for dental outpatients Part VI LIST OF CONTENTS: CLINICAL GUIDELINES ................................................................................................. 237 INTRAVENOUS SEDATION PROTOCOL............................................................ 239 6.1 Introduction ....................................................................................................... 243 6.2 The Patient for Sedation .................................................................................... 245 6.2.1 Examining the Patient ........................................................................ 245 6.2.2 Clinical Anatomy ............................................................................... 245 6.3 Benzodiazepines ................................................................................................ 247 6.3.1 Operating mechanism ......................................................................... 247 6.3.2 Half-life .............................................................................................. 247 6.3.3 Pharmacodynamics ............................................................................. 248 6.3.4 Pharmacokinetic anomalies ................................................................ 248 6.4 The Commercial Drugs ...................................................................................... 249 6.4.1 Selecting a suitable drug..................................................................... 249 6.4.2 Diazepam ............................................................................................ 249 6.4.3 Midazolam .......................................................................................... 250 6.4.4 Administration equipment .................................................................. 251 6.4.5 First aid equipment ............................................................................. 252 6.5 Monitoring the Patient ....................................................................................... 254 6.5.1 Blood pressure monitors ..................................................................... 254 6.5.2 Pulse oximetry .................................................................................... 254 6.5.2.1 The monitoring principle and equipment ........................................ 255 6.5.2.2 Monitoring during sedation ............................................................. 256 6.5.2.3 Emergency situation ....................................................................... 256 6.5.2.4 Sources for defaults ......................................................................... 257 6.5.3 Pulse wave oximetry........................................................................... 257 6.6 Intravenous Sedation in Practice ........................................................................ 259 6.6.1 Cannulating the vein in the crook of the arm ..................................... 259 6.6.2 Administering the drug and observing the effects .............................. 260 6.6.3 Recovery from sedation ...................................................................... 261 6.6.3.1 Oxygen saturation............................................................................ 261 6.6.3.2 Flumazenil ....................................................................................... 261 6.7 Complications ..................................................................................................... 264 6.7.1 Local complications ........................................................................... 264 6.7.2 Hypoxia .............................................................................................. 264 6.7.3 Fainting .............................................................................................. 265 6.7.4 Psychogenic complications ................................................................ 265 6.7.5 Other complications ........................................................................... 265 6.8 Legal aspects ...................................................................................................... 267 6.9 Conclusions ....................................................................................................... 268 6.10 Instructions to patients ..................................................................................... 269 1.11 Pictures ............................................................................................................ 270 241 Monitored intravenous sedation with local anaesthesia for dental outpatients Part VI 6.1 INTRODUCTION Some patients may have such a fear for dental procedures that they need to be sedated. To reach an adequate and accurate effect these drugs have to be administered to the vein. This is called intravenous sedation (sedative medication given through the vein). It is not general anaesthesia. Even intravenous sedation includes risks which must imperatively be recognised, and due precautions for treating eventual complications must be made. with these doses, to the effect that they are practically in a very deep anaesthesia during the whole procedure, which severely impairs the dentist's work. Also recovery from the procedure takes several hours, which will then paralyse the operations of the dental surgery for the remaining hours. Although the basic doses for intravenous sedation are 10 mg of diazepam and 5 mg of midazolam (notice the difference in the efficiency ratio of midazolam), the individual amount for the patient is titrated to the exact point through intravenous dosage. Hence oversedation or undersedation will be extremely rare. There will be no problems with the procedures and the patient's recovery is swift. Why should we use intravenous sedation, recognizing all its intrinsic risks, instead of oral sedation? This is a typical question made by dentist colleagues to the author of this study. To answer it we need to look at some principles: orally, a useful dosage of diazepam is 10 mg for young and adults, 5 mg for children. Smaller doses will not produce a useful sedation. The dosages per os for midazolam are 7,5 to 15 mg. For the patient, intravenous sedation is a necessary alternative in dental care. It should nevertheless not include risks that are greater than the advantages. The dentist and the dental surgery assistant must acquire sufficient training for and a good command of this procedure. The skills must also be regularly sustained and developed. This is the way to avoid emergencies and complaints. Given orally, for the majority of patients these doses create a good sedation sufficient for a normal procedure. The problem is that a minority of patients will not get any sedative effect with these doses. In a case of a frightened patient, the experience of the treatment will be most unpleasant. Another minority of patients will become oversedated The purpose of these instructions is to provide a theoretical basis for the understanding of intravenous 243 Clinical guidelines sedation, but the practical application of the procedure necessitates manual training and displayed skill of commanding the subject. 244 Monitored intravenous sedation with local anaesthesia for dental outpatients Part VI 6.2 The Patient for Sedation a serious muscular weakness, Myastenia gravis a serious neurological illness an alcohol problem or a drug addiction advanced age or underage sensitivity to benzodiazepine (extremely rare) pregnancy, also extreme care should be taken with breastfeeding mothers 6.2 1 Examining the Patient A careful recording of the medical history is the precondition of safe intravenous sedation. An example of an easily filled medical history form is enclosed. This form will be further complemented by an interview, as it gives the best contact with the patient. It is important to define the patient's weight and length so that the drug dosages can be correctly chosen. The interview also gives an opportunity to draft a psychological profile of the patient. The dentist should aim at establishing the level of anxiety and the level of self-control in the patient. If the patient is extremely frightened and he/she reacts to the slightest stimulus during the examination, it should be seriously considered whether intravenous sedation is the right method of treatment. Besides a consent from the patient, intravenous sedation requires also the surgeon's command of this method of treatment and its complications. Intravenous sedation is not suitable for a patient who has: In case of any doubt that this treatment might be unsuitable to the patient, it is advised to consult his/her practising general physician. Despite the consultation it must be remembered, though, that the responsibility for the sedation lies with the treating dentist. 6.2.2 Clinical anatomy When undertaking intravenous sedation it is important to know the anatomy of the vascular system in the hand. Suitable sites of injection for a dental sedation are the cubical fossa and the dorsum of the hand. The advantages of the cubical fossa are the large veins that are easy to punctuate, and the fact that the injection is less painful than when punctuating the dorsum of the hand. Also eventual haematomas caused by the injection are less visible in the cubical fossa than the dorsum of the acute lung disorder a serious disorder in the liver functions operating disorder of the kidneys steroid medication psychiatric medication, including benzodiazepines 245 Clinical guidelines tenderness of the site of injection the possibility of puncturing the cannula into an artery and the possibility of injecting the drugs into arterial circulation hand, and they are easily covered with clothes. The dorsum of the hand may at times be the only possibility when the patient's clothing prevents the use of the cubical fossa or when no visible vein is found in the cubical fossa. The complications of an intraarterial injection are very severe; in the worst case they may lead to the loss of the whole limb or a serious circulation disorder therein. Therefore patients sedated intravenously shall always be connected into the open line. There is a risk at the cubical fossa of accidentally punctuating the cannula into an artery, or of causing an arterial bleeding into the tissues. There may also be problems in the liquid flow of the cannula when the patient is bending his arm. When a free-flowing liquid infusion tube is connected to the cannula which is placed in an artery, a fast and powerful blood intrusion to the infusion tube and upwards all the way to the infusion bottle or bag can be observed. At this point there is no doubt about the cannula being misplaced. When the cannula alone is placed in the vein there is never an absolute certainty that it is securely in the vein and not in an artery. The disadvantages of the dorsum of the hand are above all smaller veins, more sensitive site of injection and the visibility of the bruises. The complications of cannulation are: bleeding from the injection area to the tissues (haematoma) thrombus and infection of the vein (thromboflebite) 246 Monitored intravenous sedation with local anaesthesia for dental outpatients Part VI 6.3 Benzodiazepines that this is not the time the drug takes to disappear from the body, nor is it the time when the drug's effect can be seen in the body. The terms 'long half-time', 'short half-time' may sometimes be confused with 'longacting' and 'short-acting', and therefore the meaning of each should be kept clearly in mind. For instance the half-time of diazepam is several dozens of hours (24-48), whereas its active sedation time is only a few dozen minutes. 6.3.1 Operating mechanism It is important to know the operating mechanisms of the applied drugs. In the clinical pharmacology of benzodiazepines the main issue is pharmacodynamics or how the drug works in the body. Although it is easy to measure the drug plasma levels for most drugs, estimating the drug's concentration at the receptor sites is extremely difficult. Many drugs are attached to receptors and their plasma levels do not necessary correlate with their effect. This often causes problems in defining the correct dosage. This is also the case for benzodiazepines. Nevertheless it is clear that there is no clear correlation between benzodiazepine plasma levels and their clinical effect. Hence follows that the calculation of pharmacokinetic parameters from plasma levels is not clinically relevant. This applies e.g. to the halflife of benzodiazepines. The very effect of benzodiazepines is based on their connecting to receptors in the brain. Therefore their clinical effect have a very vague correlation with their plasma levels. The following steps shall be observed when dosing intravenous drugs: 1. The uptake or absorption phase which is the time taken to inject the drug, in the case of drugs dosed straight into the vein. The absorption phase of oral drugs is long and it depends on the uptake of the drug. 2. The distribution phase, where the drug is distributed into tissue components according to its properties, e.g. the liquid system or fatty tissues. 3. The elimination phase which begins when a balance between plasma and the other tissues of the body has been reached. Subsequently, the drug is 6.3.2 Half-life Half-life means the time taken for the plasma concentration to decrease by 50 per cent. It is important to note 247 Clinical guidelines eliminated through liver metabolism or kidney secretion according to the drug's half-life. The patient will recover clinically considerably better when the drug is eliminated from his body. dose), plasma levels are extremely high for several days. The patient will, however, recover clinically to the extent that he is fully alert and fit to leave the hospital considerably faster than what would be the elimination time of the drug. It is important to understand that the clinical maximum effect of a drug does not have a correlation with its plasma level. This is quite apparent when a drug is administered intravenously: when the drug's plasma level is still increasing, the patient is much more sedated and tired than when the plasma level is already decreasing (compare with getting drunk and coming down). 6.3.3 Pharmacodynamics All diazepines has the following four characteristics: 1. Hypnotic or sleep inducing 2. Anxiolytic (sedative, eliminating anxiety, calming) 3. Muscle relaxant effect 4. Prevention and reduction of convulsions. The lack of correlation between drowsiness and drug plasma levels is also evident when the patient is prescribed diazepam for continued use. The patients tend to be tired during the first few days even though the plasma level is still rising over the following days. The steady state level where the elimination and further administration is in balance, is reached much later. The effect of a given dose depends more on the speed of increase of the plasma level than the plasma level itself. The action of benzodiazepines is based on the stasis of benzodiazepine receptors. These receptors are found in the central nervous system. The receptors are very specific to the agonists and antagonists of benzodiazepine. They are not receptive to other sedative agents such as barbiturates. 6.3.4 Pharmacokinetic anomalies In overdose cases where the patient has taken massive amounts of diazepam (even 400 times the usual 248 Monitored intravenous sedation with local anaesthesia for dental outpatients Part VI 6.4 The commercial drugs combination does irritate veins, and in an oil-water emulsion which does not carry the irritating effect and which is the only acceptable solution in intravenous sedation. In Finland the trade name of the latter is Stesolid Novum 5mg/ml injection liquid and it is packed in 2 ml ampoules, which means that one ampoule contains 10 mg diazepam. In Stesolid Novum the diazepam is solved in an oil phase. The organic solvents used in conventional parentheral diazepam products have been found to cause unpleasant symptoms and pain in 78 % and thrombophlebitis in 30 % when injected in the vein and thus they may be considered unsuitable for intravenous sedation. The corresponding frequencies for the Stesolid Novum injections are 5.3 and 1.1 %. Stesolid Novum is ready for injection and it may also be administered to small peripheral veins. Diazepam should never be injected in the muscle because of very insecure absorption. 6.4.1 Selecting a suitable drug The ideal sedating agent should possess the following properties: 1. Sufficient sedative and anxiolytic properties 2. Amnesia or cutting off memory for the duration of the procedure 3. Easy administration 4. No irritating effects on veins or tissues 5. Short and speedy recovery 6. No effects on cardiovascular or respiratory systems 7. Low toxicity 8. No side-effects 9. Compatibility with other drugs. Both diazepam in an emulsified form and midazolam come very close to the above principles. Therefore they are widely used in the world in connection with dental procedures as well as e.g. with gastroenterological procedures. The most common drugs used in dental procedures are diazepam, midazolam and flumazenil. The official indication of the drug is premedication before the procedure. Dosage for premedication is intravenously 0.1-0.2 mg diazepam/kg. A rule of thumb for the maximum dosage of diazepam in dental procedures is that doses over 20 mg may only be used for exceptionally lengthy procedures. The initial dose of diazepam should 6.4.2 Diazepam Diazepam is available in 2 ml ampoules containing 10 mg diazepam. Diazepam is available both in a water-alcohol solution, which 249 Clinical guidelines never exceed 20 mg. It should also be borne in mind that the clinical effect for elderly and weak patients is usually reached with smaller doses. This means in practice that elderly persons should be administered only ca. 2.5 mg diazepam at a time and allowed a few minutes for the effects to become apparent after each dose. Other facts to remember are the contraindications and the fact that diazepam impairs the tolerance for alcohol, sedatives and sleeping tablets. cause an exceptionally strong reaction if other sedatives are taken before complete elimination, and this carries a risk of danger. On the other hand these problems occur quite rarely even though diazepam is a very common drug. After oral administration diazepam is absorbed rapidly. A single dose of 10-15 mg gives a plasma concentration of 0.2-0.3 micrograms/ml within 2 hours. The elimination of the drug is initially rapid but it slows down into a total half-life of 1-2 days. The effect of diazepam to the central nervous system is localised in the subcortical areas and the reflexes. Its half-life in the plasma is 24-48 hours. The long half-life causes a risk of drug accumulation in the body if the doses are repeated before an earlier drug has been eliminated. If a patient uses diazepam daily for his medication, a dose given in the vein may lead to respiratory depression. Recording the drugs used by the patient is therefore imperative in the medical history. Following an intravenous administration (10-15 mg), the plasma concentration of 1 microgram/ml is reached within 4 minutes and a strong sedative effect is immediate. The concentration then falls to 0,25 micrograms/ml per hour and the clinical effect is reduced at the same rate. The main effect of the intravenous dose falls within the first hour, whereafter the effect resembles that of an oral dose. To reach the same concentrations orally as are created intravenously for the first hour, extremely high doses of the drug would be needed. The main metabolite of diazepam is desmethyldiazepam, which has a half-life of 100 hours. Yet diazepam may interact with any drug that has depressant effects on the central nervous system. It can potentiate the effect of other hypnotics and sedatives on the brain. It may also increase the effects of alcohol. The use of diazepam is also problematic if the patient has anti-depressant medication. The slow elimination of diazepam and its metabolites may 6.4.3 Midazolam Midazolam is available in 5 ml ampoules containing 5 mg midazolam or a content of 1 mg/ml, and in 3 ml ampoules containing 15 mg midazolam or a content of 5 mg/ml. The latter have been intended solely 250 Monitored intravenous sedation with local anaesthesia for dental outpatients Part VI for general anaesthesia use and are not suitable for dental applications. The former, dilute solution should be used for dental procedures as it enables the safe titration of the dose. not needed to create the desired response. The easiest means of dosage is to titrate 1 mg of the drug through a cannula every second minute and then follow up for the response. Midazolam is sold under the trade name Dormicum. Midazolam can form water-soluble salts with acids which provide a well-tolerated watersoluble injection liquid. The drug has a short duration and is well suited for premedication. Midazolam typically shows a rapid action on the onset and a short duration due to a fast metabolism. Due to its low toxicity, the therapeutical scale of midazolam is wide. A short-term anterograde amnesia is seen after intravenous dosage, and patients show a clear tendency of drowsing off after the desired sedation level has been reached. The elimination half-life is 1.5-3 hours. The effect of midazolam is so strong and individual that there is risk for serious side effects. A respiratory depression may turn into the discontinuation of respiration which, undetected, leads to cardiac arrest. This is a great risk with elderly or weak patients, and resuscitation equipment should always be available. Midazolam interacts with the following drugs: analgesics, sleeping drugs, anxiolytes, antidepressants, neuroleptics, simeditine and erythromycin. All these drugs contribute to a longer active period or a stronger response. It must especially be noted that midazolam should be administered with special caution to elderly people and weak patients, and to patients suffering from an obstructive pulmonary disease, chronic kidney deficiency or cardiac insufficiency. The elimination half-life of the principal metabolite, alfahydroxy midazolam, is shorter than that of midazolam. With elderly people, the half-life of midazolam may become even three times longer. Therefore an intravenous dosage should be titrated against the patient's response. The official indication of midazolam is intravenous basic sedation in connection with diagnostic or surgical procedures carried out in local anaesthesia. The initial dose is 2.5 mg 5-10 minutes before the operation. Additional doses of 1 mg may be given in case of need. Over 5 mg doses are generally 6.4.4 Administration equipment Disposable syringe: for premedication with midazolam, the most practical size is 5 ml and with diazepam 2 ml. Needle: needles are needed for the suction of the drug from the ampoules 251 Clinical guidelines to the syringe. Ideal needles are as wide and long as possible, e.g. ones with a Luer connector 20 g x 1" or 0.9 x 40 mm. the infusion may be set to one drop per 2-3 seconds (=1 ml/min). Surgical tape: The cannula is attached without allowing any movement for it. A strong adhesive tape, preferably in a y-form bandage. Pharmacies have a wide range of various surgical tape materials packed in rolls so finding a suitable one for attaching the cannula should cause no problems. Cannula: in intravenous sedation, the patient should also have a venal cannula. Ideal would be one with three entrances, which facilitates the possible change of infusion bag. The cannula needle may be very thin as only salt solution needs to be transferred through the cannula, and a thin needle will also make the cannulation procedure much more pleasant. A suitable width of cannula is 20 G (Gauge) which corresponds to a diameter of 1 mm, and a sufficient length for the needle is 30 mm. This size of cannula will allow the transfer of 50 ml liquid per minute which is quite sufficient for this need. With a thin cannula the injection is painless and succeeds well. Also venal irritation is much smaller than when using a larger cannula. Venous stasis: A venous stasis is attached above the cannulation site to bring up the veins. It should direct the pressure to prevent the return of the blood through the veins but to let the blood pressure to fill the limb. 6.4.5 First aid equipment Additional oxygen is the most frequent supplement needed in intravenous sedation. An oxygen cylinder is absolutely necessary and no procedures should be started if there is not enough oxygen for several hours' administration. Nasal cannula are ideal for administering oxygen during the procedure as an oxygen mask cannot be used. Infusion tube: The simplest transfer tube with an infusion chamber, restriction valve and a Luer lock for connecting the cannula. Infusion liquid: A physiological sodium chloride liquid (0.9 %), available at the pharmacy, is used in intravenous sedation. It comes in both glass and plastic holders. A volume of half a litre is quite sufficient for sedation purposes. The rate of the infusion should be fast at the beginning of sedation, and when the sedation level is sufficient the rate of Precautions against respiratory arrest shall be made with a emergency resuscitator, "Ambu", that is connected to the oxygen. During the procedure the sedationist must have both the possibility and the ability to perform an endothracheal intubation for the patient when needed. This makes intravenous 252 Monitored intravenous sedation with local anaesthesia for dental outpatients Part VI sedation a suitable next step after getting experienced with nitrous oxide. The above mentioned resuscitation methods must be acquired for the permit to use nitrous oxide. ampoules. They contain 0.5 mg of the drug or 0.1 mg/ml. It is important always to have the antagonist within reach in case any problems should arise during the procedures. -doxazepram; (Dopram®), which stimulates the respiratory center in the brain; -salbutamol (Ventoline®) opens the pulmonary tubes e.g. in connection with status asthmaticus; -etilephrine (Effortil®) which is used to increase the volume per minute of the heart and to increase blood pressure. The resuscitation drugs listed in the general dental studies shall naturally be found at the surgery. These are 1) epinephrine, 2) diazepam, 3) atropine, 4) cortisone, and various liquids to solve the above, as well as the syringes and needles to administer them. In addition to these, intravenous sedation procedures require certain drugs primarily intended to cure respiratory depression and to support the cardiovascular system. These drugs are: All the above mentioned drugs are in injection form and require the acquiring of due training in addition of learning their properties from books. It is of utmost importance that all necessary emergency/resuscitation drugs are within reach for the dental surgeon making the procedure, and that the expiry dates of ampoules are duly followed. Moreover, the ampoules should not be opened until immediately before use as an opened ampoule will not keep. -nalorphin (Nalorfin®), which cures the respiratory depression caused by opiates; -flumazenil (Lanexat®) to impede the benzodiazepine receptors and thus cure the respiratory depression caused by benzodiazepines. Flumazenil is a benzodiazepine antagonist and it is available in 5 ml 253 Clinical guidelines 6.5 Monitoring the patient The safety and well-being of the patient is the responsibility of the operating dental surgeon. All sedated patients must be monitored. The price of monitoring equipment is no excuse for not monitoring the patient. Also monitoring findings should be carefully registered. The most important monitors of all are the eyes and ears of the person carrying out the procedure, which means that the patient must be observed closely during the whole procedure. This is the way to avoid unnecessary problems. If the data gained through electronic monitoring is in contradiction with clinical observations, human intelligence and observation skills are needed to solve the situation. Even if monitoring is essential, it will never replace the human senses, only complete them. so monitoring need not be continuous. The basic requirement is the possibility to measure and record the pressure before and after the procedure, and also during the procedure according to the patient's symptoms. 6.5.2 Pulse oximetry The functions of the body depend on a continuous intake of oxygen. This vital supply has been secured by many means, the most important of which is the ability of haemoglobin to bind oxygen. The amount of oxygen tied in haemoglobin depends on the prevailing oxygen pressure, but an essential fact is that the dependence is not linear but creates a co-ordination curve of a gentle S. The amount of oxyhaemoglobin, oxygenated haemoglobin in the total amount of haemoglobin is called oxygen saturation, measured as a percentage. The flat ending of the oxygen dissociation curve of haemoglobin ensures a good oxygen saturation on a wide variation scale of the oxygen pressure. On the other hand the steep fall of the curve enables quick delivery of oxygen in the areas with oxygen pressure characteristic to certain tissues. 6.5.1 Blood pressure monitors There is a variety of pulse and blood pressure monitors on the market, the simplest of which measure the blood pressure automatically at the pressing of a button, the more complicated ones measuring the blood pressure independently at pre-set minute intervals. All monitors should enable recording the results with a printer. There are no drastic changes in blood pressure during intravenous sedation Oximetry saturation or 254 measures oxygen the percentage of Monitored intravenous sedation with local anaesthesia for dental outpatients Part VI oxyhaemoglobin. It can also be measured in a laboratory test from an arterial blood sample, but nowadays oximetry means a non-invasive monitoring system where the monitoring occurs continually through the skin. The oximeter is usually connected to a finger, but other monitoring sites such as the earlobe are also suitable. 6.5.2.1 The monitoring principle and equipment Oximetry is based on the fact that the light absorption characteristics of haemoglobin and oxyhaemoglobin are different, and they also vary according to different wavelengths of light. The oximeter has a sensor with diodes steadily pulsating two different wave-lengths. The equipment measures the variation in the absorption of red (R ) and infrared (IR) light during systole and diastole, and on the basis of these quantities it calculates the value of oxygen saturation. Typically the sensor is connected to a finger. It is important that the sensor stays steadily in place. It causes no pain or disturbance to the patient so this method is an ideal case of non-invasiveness. The equipment works very quickly after the sensor has been placed and no calibration is needed. Pulse oximetry has been developed for clinical use in the mid1970's in Japan. During 1980's this monitoring system has become extremely popular and during the last few years it has in many countries even been considered compulsory in the control of general anaesthesia. Since 1986 pulse oximetry has become so popular also in Finland that it is considered by many as the most important monitoring system in anaesthesia. Pulse wave oximetry also utilizes the information contained in the pulse wave. Even though it only used to function in the monitoring of the timing of the saturation, the pulse wave printed on the screen is becoming a normal feature in the equipment. The size of the pulse wave easily shows great variation according to various factors and thus it reflects the changes in blood flow at the monitoring site. Several pulse oximeters on the market operate in the above mentioned principle, some of which may be called pulse wave oximeters. The equipment may be designed solely for pulse oximetry but it may also be an integrated part of the monitoring equipment. Pulse oximeters are small in size. Some of them have a video display, some LCD display. Typically they display oxygen saturation and pulse rate in numerical values, and the pulsating wave-form beat by beat. Adjustments are usually limited to setting alarm limits. Modern technology has also brought an output for data recording. 255 Clinical guidelines Even if this property is not used as a routine, it is irreplaceable when carrying out clinical studies on pulse oximetry. Many equipment offer the possibility to follow the development of monitoring quantities in a specific trend memory. This information gives a learning basis for a secure intravenous sedation. The equipment usually works on ordinary current but they are secured with a built-in battery. most changes in saturation occur. Even extensive local anaesthesia creates more decreases in saturation than is commonly believed. Saturation may decrease in cases where anaesthesia has to be complemented with intravenous analgesics or sedatives. The situation is usually relieved with a dosage of oxygen. In many countries the pulse oximeter has been considered such an essential safety factor that its use is compulsory or close to compulsory during general anaesthesia. In Finland its use is recommended, but the decision still lies in the consideration of the anaesthesia team. The range of application of pulse oximetry covers the whole of anaesthesiology and the intensive care related thereto. It is always applicable when there may be exceptions in normal oxygen saturation. Pulse wave oximetry may also be used to monitor changes in peripheral circulation when no changes in oxygen saturation are expected. 6.5.2.3 Emergency situations There would be plenty of use for pulse oximetry in estimating the danger of sudden emergencies and the corresponding efficiency of correcting measures. Lack of oxygen is connected with many acute illnesses and damages and with them creates a concrete risk factor. A pulse oximeter also immediately displays the effectiveness or inefficiency of the corrective measures. If the patient is transferred to a hospital, the monitoring should be continued as unexpected changes in the patient's condition may arise in emergencies. 6.5.2.2 Monitoring during sedation The most feared of possible emergencies in connection with sedation is a sudden lack of oxygen. Therefore pulse oximetry is a safety factor which enables the quick perception of sudden lack of oxygen and the counteraction of its consequences. Attention must be paid to a continual decrease of the saturation already before it reaches the stage of actual lack of oxygen. Pulse oximetry is particularly applicable in the beginning of sedation as this is the phase where 256 Monitored intravenous sedation with local anaesthesia for dental outpatients Part VI method before, but with pulse oximetry it has acquired a new renaissance. 6.5.2.4 Sources for default There are certain sources of default within pulse oximetry and pulse wave oximetry although as such they are quite reliable methods. The photoelectric pletysmography measures the absorption of infrared light and prints the mirror image as a pulse wave. The shape and height of the pulse wave depend on the volume increase caused by the pulsation of the heart at the site of monitoring. Thus the value of infrared light absorption (IR) correlates to blood flow but does not give an absolute value for the volume of circulation, only a relative value. The pulse curve resembles in shape the direct arterial pressure curve, but should not be confused to it. In general most attention is paid to the height of the curve, which is indeed its most informative feature. The absorption of red light is not specific to oxyhaemoglobin but the same phenomenon is created by the setting of carbon monoxide to haemoglobin. This is visible e.g. in the case of extensive smoking. Pulse oximetry measures oxygen saturation which only decreases a little although there would be a considerable decrease in the venal oxygen pressure. Therefore the shape of the dissociation curve should always be considered when interpreting the oxygen saturation values! The smooth muscles of the finger veins are very sensitive towards sympathetic nervous stimuli. When the patient is anxious, his hands are cold and pale. Also pain creates a reaction of strong venal contraction. Many drugs used in anaesthesia, and in fact the anaesthesia itself, enlarge peripheral veins. If due to bleeding the amount of blood is insufficient, circulation in fingers decreases drastically. If the circulation in a limb is disturbed due to pressure on an artery, the pulse wave is significantly decreased. In fact there is much more variation in the pulse wave than in the pulse rate or the oxygen saturation. In pulse oximetry the saturation and pulse rate values require a pulsating circulation but the values remain reliable even during poor peripheral circulation. 6.5.3 Pulse wave oximetry The pulse wave was originally only assisting the timing of oxygen saturation monitoring. A visible pulsating wave-form has, however, such an important information value that it deserves its visibility. A visible pulse wave changing in volume gives the equipment an additional feature of pulse wave oximetry. The pulse wave has been used as a monitoring A precondition for using the height of the pulse wave for 257 Clinical guidelines monitoring is that it is visible and that only changes in volume at the monitoring site affect its size. In some equipment the pulse wave is maintained at the same size by changing the amplification, thus losing its informative value. The size of the pulse wave often changes to such an extent that the amplification has to be changed but this should be done in progressive steps rather than in a sliding fashion. The visibility of the pulse wave also confirms the reliability of the saturation and pulse rate values. Usually the pulse wave needed for a reliable monitoring is suprisingly small, but without a smallest pulsation no value is obtained. the pulse wave shows a regular increase. Depending on the starting point, its height is increased four to five times. In a peaceful phase the pulse wave is high, but a procedure will again contract it. During anaesthesia the pulse wave will react to painful stimuli and superficial anaesthesia. The height of the pulse wave is not an absolute but only a relative quantity. In different fingers the height of the pulse wave is different; in the right hand it is usually higher than in the left hand, and in the middle finger it is the highest. The height of the pulse wave has no quality, but its changes in the same patient are significant. As the pulse wave is so sensitive and the changes in its height can be due to many causes, learning to interpret the height of the pulse wave should be done taking into account the other simultaneous monitoring methods. When the patient has been given premedication and is transferred to the operation room, the height of the pulse wave gives an indication on the sufficiency of the given premedication. The pulse wave of an anxious patient is minute. In sedation 258 Monitored intravenous sedation with local anaesthesia for dental outpatients Part VI 6.6 Intravenous sedation in practice Before beginning intravenous sedation the dentist should make sure that all necessary resuscitation equipment and drugs are close at hand and also, that there is oxygen in the oxygen cylinder and that the expiry dates of the drugs have been followed. The patient is placed into an almost supine position, his blood pressure is taken and the probe for the pulse oximeter is attached, and the initial values for blood pressure and oxygen saturation are recorded. The cannulation can also be done completely without pain with an emulsion ointment or plaster (Emla ®) to numb the skin for the cannulation procedure. The plaster is evidently more practical for cannulation purposes as it is individually packed and can be attached by the patient or his parent to an agreed place. The anaesthetic effect begins after 1 hour and thus to be useful the product should be given beforehand for the patient to apply at home. More detailed information of the product can be found in the national Pharmaca. 6.6.1 Cannulating the vein in the crook of the arm Before the patient arrives, the following equipment should be made available: a 5 ml syringe a large needle (G 21) for the suction of the drug intravenous cannula alcohol swab drugs venous stasis infusion fluid package infusion tube A venous stasis is placed at the patient's arm to provide good visibility of the veins. When fitting the venous stasis it should be remembered that the pressure should not be so great that arterial circulation in the arm is obstructed. After this the cannula is attached and fixed to the skin with plaster. The patient's weight should be found out beforehand or, if it has not, it should be verified at the latest at this point. The drug is nevertheless dosed primarily according to individual reactions and only secondarily in accordance with the patient's weight. 259 Clinical guidelines the patient closes his eyes or seems to be somnolent the value in the pulse oximeter decreases by 2-3 % of the initial value as a result of decreased respiration rate. The salt solution is placed in the infusion stand and the chamber of the intravenous-line is filled with the liquid. The whole length of the tube is checked carefully for air bubbles. The infusion tube is attached to the cannula and for a while the infusion restrictor is set to allow maximum flow. This is to ensure that the flow is free and the surrounding tissue is not swelling as a sign of paravenous infusion. At this point it will be evident if the injection has hit an artery as blood will then rush up the injection tube. Sedation is commenced, and especially for anxious patients, local anaesthetics containing epinephrine should be avoided as a possible tachycardia reaction caused by epinephrine may disturb a good sedation. Calmness should always be prevalent when handling the patient as he is awake and by no means anaesthetised. 6.6.2 Administering the drug and observing the effects After the sedation phase it is possible to give additional doses of midazolam if the patient's bearing would indicate a need for further medication. However, the pulse oximeter should be observed before every additional dose, and no further doses should be given if the pulse oximeter value is equal to or lower than 95 %. When the infusion is working normally, the administration of midazolam is commenced. With a disposable syringe, midazolam (1 mg/1 ml) is given in 1 mg doses. The doses are repeated every 2 minutes. A conversation is held with the patient throughout the administration, on any subject, to observe the impairment of the motor co-ordination of speech. Other motor disorders can be observed e.g. by asking the patient to touch his nose before every new dose of drugs. When the patient closes his eyes is also noted, and pulse oximeter values are observed. An appropriate level of sedation is reached when one of the following observations is made: the patient's slurred speech If sedation is followed by a surgical procedure, it is worth reminding the patient that he may freely sleep while the team is preparing the operating room ready for surgery. The patient will usually fall asleep a few minutes after the conversation with him has been stopped. Before surgical procedures it is always good to give the patient a small dose of fentanyl (50 microgram/ml) immediately before becomes 260 Monitored intravenous sedation with local anaesthesia for dental outpatients Part VI the surgery, e.g. some 25 micrograms of fentanyl is usually sufficient. The advantage of this is that the patient reacts less to small sensations of pain which may arise despite of sedation. As fentanyl is also a powerful respiration depressant, the value in the pulse oximeter must be checked before administering the drug. In conventional treatment (e.g. extraction, root treatments etc.) the treatment should be initiated immediately after the sedation becomes effective. An additional 1 mg of midazolam (see the pulse oximeter) is recommended, whereafter the saliva aspirator is placed on site. A recommendable suction fan is the short loop-form aspirator. These aspirators work like a string thus helping the patient to keep his mouth open. to another finger, but only after the exclusion of real oxygen desaturation. In case you suspect the malfunction of probe, use your own finger to test the function of the probe. If the value remains unchanged, airways are open and patient is breathing, additional oxygen should immediately be given to the patient. Nasal cannula and a regular 3-10 l oxygen cylinder (e.g. AGA) is suitable, when checked that there is enough oxygen for several hours' need. The administration of additional oxygen will repair almost without exception a beginning hypoxia. If the respiratory depression is caused by benzodiazepines and the low oxygen saturation is not increased by oxygen administration, the patient should be administered intravenously some flumazenil (Lanexat 0.1 mg/ml à 5 ml). This drug can be dosed in 0.1 mg i.e. 1 ml portions which are repeated every minute until the oxygenation has returned to normal. The dosage may at a maximum rise up to 1 mg (10 ml). 6.6.3 Recovery from sedation 6.6.3.1 Oxygen saturation Oxygen saturation is monitored closely both during the procedure as well as during the reversal of sedation. If oxygen saturation falls under 90 %, it is important to check immediatelly the patient’s respiration movements and openess of airways. It is also diagnostic to know if the decrease is sudden or slow. In some cases the reason can be local at the measuring finger: it should be checked that the probe does not give so much pressure to the monitoring site that circulation is obstructed. In this case the probe should be moved If respiration depression is caused by benzodiazepines, return to normal oxygenation is very fast and will occur during the very first doses. As flumazenil is a benzodiazepine antagonist, it blocks the same receptors where benzodiazepines are attached. Therefore flumazenil may be given in a sufficiently small amount to revert an eventual respiration depression, but not to lose 261 Clinical guidelines the sedation. The procedure may then be carried out normally. 1. an efficient emergency drug for oversedated patients 2. full co-operation of the patient 3. a safer recovery period 6.6.3.2 Flumazenil The possibility of using flumazenil as an antagonist in overdose cases makes it an extremely important drug for securing the sedation process. It must be kept within reach whenever a patient is sedated. A part of the patients are very sensitive to benzodiazepines and in these cases an antagonist may even prove to be a life-saving drug. Elderly patients are much more sensitive than the young to the effect of benzodiazepines. In the cases where general anaesthesia is contraindicated due to the patient's respiratory illness, intravenous sedation is the only possibility to enable certain procedures, and flumazenil ensures that the sedation is safe. A general rule for elderly patients is not to send them home immediately after treatment with intravenous sedation, but rather to arrange for an overnight monitoring for them at the ward. Besides treating complications, flumazenil may be used to end the sedation of a patient after a short procedure. The patient may be given 0.05 mg per 5 minutes of flumazenil, until he can walk without assistance. As the half-time of flumazenil is shorter than that of benzodiazepine, a resedation may occur within 2-3 hours, and this should be notified to the patient and his escort. The initial dose of 0.2 mg flumazenil is administered through the cannula while it is still in place in the cubical fossa. It must be noted here that the cannula should remain in place during the whole procedure and must not be removed until the patient is fully recovered. A few seconds after being given flumazenil, the patient is likely to open his eyes. When the patient is fully awake he is given permission to sit up and, after a few further minutes, he is also given written instructions for recovery which are referred to orally. The instructions should essentially forbid driving and the use of alcohol. At this stage there is no point in explaining too complicated things to the patient. The instructions will order the patient to rest for the following day. The advantages of benzodiazepine antagonist are: When the patient is sedated, his level of consciousness has decreased and this may encumber complicated procedures, e.g. the preparation of a dental crown. What can be done is to make the unpleasant procedures immediately in the beginning of sedation. When the stage is reached when the patient should no longer be sedated but co-operative, he is given flumazenil until he can contribute to the procedure (e.g. the fitting of occlusion and dentures). the 262 Monitored intravenous sedation with local anaesthesia for dental outpatients Part VI The patients which have undergone treatment under intravenous sedation and have been given flumazenil to eliminate the sedation, can sit and stand up normally. It must, however, be remembered that they still remain sedated and cannot fully look after themselves. It is crucial to know that the effective time of flumazenil is shorter than that of midazolam and in theory the sedation with eventual respiration depressions may return, even though the long duration of dental procedures makes it highly unlikely. The presence of an escort is even in these cases absolutely necessary. The escort gives the patient a feeling of security and someone to talk to about the experience. After the procedure, the patient may be sent home 3 hours after the last dose of midazolam. He should be sent with an adult escort. Both the patient and his escort should be reminded of the written instructions which the patient received already on his previous call; the main points being that the patient's ability to observe traffic is not sufficient in the 12 hours to follow, and that he should not take alcohol during this time, as it would increase the effect of the drugs and vice versa. Some people may show unpredictable individual reactions. The patient should be made aware of the dentist's office and home telephone numbers in case any help might be needed after the treatment. 263 Clinical guidelines 6.7 Complications cannula ending up in circulation. The breaking of a venal cannula and the drifting of a loose part into circulation is without exception poor medical practice caused by the cannulation technique, and it will lead to prosecutions and claims. 6.7.1 Local complications Intravenous injections may produce a reaction at the injection site, later turning into a thrombophlebitis. This is an inflammatory reaction found at the injection site: redness of skin, swelling and pain. The vein may be blocked due to the infection (thrombus), but although painful, this is not a dangerous condition. Also haematomas are found at the injection site. They are generally a result of a damage occurred in the vein, and the consequent bleeding into the surrounding tissues. To avoid paravenous injections please make sure that the needle really is in the vein. The most reliable way to control this is to connect the infusion bottle to the cannula. If the cannulation has failed, do not try the same vein again but use another vein which should be as large as possible. With appropriate technique, an extravenous injection will be observed almost as soon as it has occurred. The cannula is then taken out and a compression bandage is tied on the site, eventually even lifting the hand slightly to avoid swelling. If a thrombophlebitis is developing, it will heal itself in a few days, or one to two weeks. 6.7.2 Hypoxia A serious hypoxia is a most rare complication of diazepam or midazolam, and it occurs most likely as a consequence of an obstruction in the respiratory passages. When the sedation is too strong, the airways are not held open naturally. The patient will perform breathing movements but no air is going through. During a partial obstruction the patient's breathing sounds like snoring. Drugs may interact to emphasise the respiratory depression effect of diazepam. Oversedation and overdose will also cause respiratory depression. It is important to titrate the sedation dose to the exact point. As mentioned above, pulse oximetry of the patient is of utmost importance. There are descriptions in medical literature of the broken tip of a metallic needle or plastic parts of the 264 Monitored intravenous sedation with local anaesthesia for dental outpatients Part VI intravenous sedation have had sexually coloured illusions, the worst of which have even led to prosecution against the sedating physician. This is why it is very important that all monitoring is set up before the sedation. This applies especially to EKG monitoring; the patient should not under sedation undergo such procedures which he would not expect a dentist to do. For security reasons it is also vital that another member of the staff is present during the whole of the treatment process: in the initiating of sedation, during the procedure and during the recovery period. A good precaution for the dentist's legal protection is taking a video of the procedure and filing the tapes. 6.7.3 Fainting An extremely fearful patient may produce a vasovagal collapse, either before or during the administration of the drug. In this case the procedure will be immediately discontinued and normal instructions against fainting are followed. First the limbs are lifted up. No dental procedure should be done at that time. The patient is given a new appointment and it should be considered whether part of the diazepam or midazolam should be given beforehand per os for instance 1-2 hours before the appointment. 6.7.4 Psychogenic complications Patients who are under psychiatric medication or treatment are not suitable for intravenous sedation. There are some descriptions on paradoxical excitement which is mainly found in children, but in single cases there has been evident aggressive reactions even with adults. The only way to deal with the situation seems to be to discontinue the procedure. A more common reaction is the decrease of the patient's conscious inhibition, where the patient becomes very talkative and would say things he would normally not mention. When initiating sedation it is good to lead the conversation into harmless topics as the amnesia caused by the drug may further distort the recollection on the contents of the conversation. Some cases have been recorded where patients undergoing 6.7.5 Other complications There is a small group of patients which, after being given a few milligrams of diazepam or midazolam, will fall into deep sleep as the dose does not depend on the patient's weight. A large patient may reach a deep sedation while a small patient with not much weight may take considerable doses. The latter group may look the dentist in the eye after a 10 mg dose and say, "It doesn't feel at all". What must be remembered, however, is that the patient may be sedated even though he might claim otherwise. This case would call for psychomotor tests such as asking the patient to touch his nose. It is likely that he cannot perform this trick. Also a signature on 265 Clinical guidelines a piece of paper would easily reveal the depth of the sedation. Increasing the dose for an extremely resistant patient may lead to a quick and deep fall into oversedation. Therefore a key rule is not to give the patient more than 10 mg midazolam or 20 mg diazepam intravenously. infusion and when giving the first drugs. Ask whether he can feel any local pain and if not, all is well. An intra-arterial infection may cause an ischemy and necrose of the distal part of the whole arm. In case of acute respiratory or oral infection causing the obstruction of airways, intravenous sedation is contraindicated. Acute dental patients are ill suited for intravenous sedation. Thus acute processes must first be brought in control through draining or antibiotics, and only thereafter can the procedure be undertaken in local anaesthesia and intravenous sedation. The intravenous administration of midazolam has only few cardiovascular effects. The problems i.e. intra-arterial injections are easily avoided when the following is kept in mind: Only use a vein that is clearly visible, and after placing the cannula connect the infusion tube. Always ask how the patient feels both at the beginning of the 266 Monitored intravenous sedation with local anaesthesia for dental outpatients Part VI 6.8 Legal aspects Sedation creates operational disorders in the patient's memory which may cause misunderstandings leading at their worst into prosecution against the dentist. Therefore certain principles shall be adopted: -if teeth need to be extracted during the procedure, the patient must be informed about this beforehand, before the procedure -no payments shall be made at the sedation appointment -the most important principle is to explain all procedures diligently to the patient, and to give him written instructions. -the patient shall be told what preparations the procedure will require and what he has to observe after the procedure. -careful recording of the patient's medical history When these instructions are followed, everything is likely to go fine. If problems would arise with the patient, they can mostly be solved in a quiet and informative discussion with the patient. If not, it might be useful for the dentist to contact a more experienced colleague. Also the patient should be offered a meeting with this more experienced colleague. If legal procedures must be taken, the primary task is to contact the lawyer of the dentist or the dentists' union. -the patient must come with a reliable escort -the procedure must be suitable for intravenous sedation -the staff must be trained -emergency equipment and drugs close at hand and effective 267 Clinical guidelines 6.9 Conclusions Intravenous sedation is both for the dentist and his patient a pleasant, efficient and safe means to treat anxiety problems. The basis for the security is, however, the appropriate skills of the staff. Therefore in the conditions prevailing in the area of North European dental education tradition, instructions could be given where the dentist should first be qualified in using nitrous oxide, thus having a command and practice of patient handling, intravenous injections and endothracheal intubations from before. Thereafter the dentist could attend an intravenous sedation course and start apprenticeship with a colleague who is experienced in sedation. Individual sedation should be commenced only when the dentist has thorough knowledge on this anesthesiological method. The skill should also be continuously maintained. Endothracheal intubation exercises should not be left at one time but this life-saving procedure in a severe complication should be practised annually at a central hospital. Also intravenous sedation should not remain a measure to be taken only when the treatment cannot be done in any other way. The skills to carry out the sedation would then be too weak and the object could be an extremely difficult patient that would test the skills of even an experienced sedationist. The best way to maintain sedation skills is to use the method constantly. 268 Monitored intravenous sedation with local anaesthesia for dental outpatients Part VI 6.10 Instructions to patients You should be followed by an adult escort who will see to your safe journey home and who will be available for you until the following morning. During the 24 hours after the procedure YOU MUST NOT: leave home alone take alcohol drive a vehicle go to work Please also make sure that you have informed the operating dentist of all your possible illnesses and medications. A feverish cold or cough as well as other feverish illnesses, until they have been cured, will prevent any treatments. Also in the case of an open labial herpes the treatment cannot be carried out. If you have to cancel your appointment, please do so 2 weeks before the agreed time Immediately before coming to the appointment please use the toilet. Instructions for an extensive dental procedure: Please have an X-ray and the laboratory tests taken within a week from the control appointment. Please take the X-ray pictures and laboratory results to the next appointment. The procedure will be made in local anaesthesia and using a sedative premedication. Therefore no pain or fear is experienced during the treatment. Please dress lightly: a shortsleeved shirt and loose-fitting trousers. Do not use make-up or other chemicals in the face. Nail enamel should be removed. Wrist watch, rings, necklaces and other jewellery should be left at home if you are entering a surgical procedure. Remember to take the X-ray picture with you. EATING AND DRINKING IS FORBIDDEN 4 HOURS PRIOR TO THE APPOINTMENT. Therefore please take the medication you may have been prescribed at exactly 4 hours before the appointment. 269 Clinical guidelines 6.11 Pictures The most feared of possible emergencies in connection with sedation is a sudden lack of oxygen. Therefore pulse oximetry is a safety factor which enables the quick perception of sudden lack of oxygen and the counteraction of its consequences. Attention must be paid to a continual decrease of the saturation already before it reaches the stage of actual lack of oxygen. Pulse oximetry is particularly applicable in the beginning of sedation as this is the phase where most changes in saturation occur. Saturation may decrease in cases where anaesthesia has to be complemented with intravenous analgesics or sedatives. The situation is usually relieved with a dosage of oxygen. 270 Monitored intravenous sedation with local anaesthesia for dental outpatients Part VI 271 Clinical guidelines 272 Monitored intravenous sedation with local anaesthesia for dental outpatients Part VI The simplest transfer tube with an infusion chamber, restriction valve and a Luer lock for connecting the cannula is the best for dental use. A physiological sodium chloride liquid (0.9 %), available at the pharmacy, is used in intravenous sedation. It comes in both glass and plastic holders. A volume of half a litre is quite sufficient for sedation purposes. The rate of the infusion should be fast at the beginning of sedation, and when the sedation level is sufficient the rate of the infusion may be set to one drop per 2-3 seconds (=1 ml/min). 273 Clinical guidelines 274 Monitored intravenous sedation with local anaesthesia for dental outpatients Part VI Suitable sites of injection for a dental sedation are the cubical fossa and the dorsum of the hand. The advantages of the cubical fossa are the large veins that are easy to punctuate, and the fact that the injection is less painful than when punctuating the dorsum of the hand. Also eventual haematomas caused by the injection are less visible in the cubical fossa than the dorsum of the hand, and they are easily covered with clothes. The dorsum of the hand may at times be the only possibility when the patient's clothing prevents the use of the cubical fossa or when no visible vein is found in the cubical fossa. 275 Clinical guidelines 276 Monitored intravenous sedation with local anaesthesia for dental outpatients Part VI When the infusion is working normally, the administration of midazolam is commenced. With a disposable syringe, midazolam (1 mg/1 ml) is given in 1 mg doses. The doses are repeated every 2 minutes. A conversation is held with the patient throughout the administration, on any subject, to observe the impairment of the motor co-ordination of speech. 277 Clinical guidelines An appropriate level of sedation is reached when one of the following observations is made: the patient's speech becomes slurred the patient closes his eyes or seems to be somnolent the value in the pulse oximeter decreases by 2-3 % of the initial value as a result of decreased respiration rate. After the sedation phase it is possible to give additional doses of midazolam if the patient's bearing would indicate a need for further medication. However, the pulse oximeter should be observed before every additional dose, and no further doses should be given if the pulse oximeter value is equal to or lower than 95 %. 278 Monitored intravenous sedation with local anaesthesia for dental outpatients Part VI 279 Clinical guidelines 280 Monitored intravenous sedation with local anaesthesia for dental outpatients Part VI Besides treating complications, flumazenil may be used to end the sedation of a patient after a short procedure. The initial dose of 0.2 mg flumazenil is administered through the cannula while it is still in place in the cubical fossa. It must be noted here that the cannula should remain in place during the whole procedure and must not be removed until the patient is fully recovered. A few seconds after being given flumazenil, the patient is likely to open his eyes. After that, infusion of rest flumazenil is recommended. When the patient is fully awake he is given permission to sit up and, after a few further minutes, he is also given written instructions for recovery which are referred to orally. As the half-time of flumazenil is shorter than that of benzodiazepine, a resedation may occur within 2-3 hours, and this should be notified to the patient and his escort. 281 Monitored intravenous sedation with local anaesthesia for dental outpatients Appendicies 7.1 APPENDIX I DESCRIPTION OF THE DRUGS USED AND STUDIED Published with permissions of Roche, Dumex and Astra 283 Monitored intravenous sedation with local anaesthesia for dental outpatients Appendicies MIDAZOLAM International Standard Prescribing Information November 30 1995 DORMICUM, ampoule RO 21-3981 Dormicum Midazolam Short-acting benzodiazepine for the premedication, sedation, induction and maintenance of anesthesia Ampoules for intravenous, intramuscular and rectal administration of Dormicum to form water -soluble salts with acids. These produce a stable and well tolerated injection solution. Composition Active ingredient: midazolam as hydrochloride. The pharmacological action of midazolam is characterized by rapid onset and, because of rapid metabolic transformation, short duration. Because of its low toxicity, midazolam has a wide therapeutic range. Ampoules 5 mg/1 ml, 15 mg/3 ml, 5 mg/5 ml and 50 mg/10 ml for i.v., i.m. and rectal administration. Excipients: sodium chloride, hydrochloric acid, sodium hydroxide, water for injection. Midazolam has a very rapid sedative and sleep -inducing action of pronounced intensity. It also exerts an anxiolytic, an anticonvulsant and a muscle-relaxant effect. Properties and effects Midazolam, the active ingredient of Dormicum, is a derivative of the imidazobenzodiazepine group. The free base is a lipophilic substance with low solubility in water. After parenteral administration anterograde amnesia of short duration occurs (the patient does not recall events that occurred during the peak of activity of the compound). The basic nitrogen in position 2 of the imidazobenzodiazepine ring system enables the active ingredient 285 Appendix I drugs, this has been confirmed in vivo (see Interactions) Pharmacokinetics Absorption after intramuscular injection Absorption of midazolam from the muscle tissue is rapid and complete. Maximum plasma concentrations are reached within 30 minutes. Bioavailability is over 90%. Elimination In healthy volunteers, the elimination half -life is between 1.5 and 2.5 hours. Plasma clearance is in the range of 300-400 ml/min. When midazolam is given by i.v. infusion, its elimination kinetics do not differ from those following bolus injection. The elimination half -life of the main metabolite, -hydroxy-midazolam, is shorter than that of the parent substance. It is conjugated with glucuronic acid (inactivation). The metabolises are renally excreted. Absorption after rectal administration Midazolam is absorbed quickly. Maximum plasma concentration is reached within 30 minutes. Bioavailability is about 50%. Distribution When midazolam is injected intravenously, the plasma concentration -time curve shows two distinct phases of distribution. The volume of distribution calculated under steady -state conditions is Pharmacokinetics in special clinical situations In adults over 60 years of age, the elimination half -life may be prolonged up to three times and in some intensive -care patients requiring midazolam by i.v. infusion for long -term sedation, up to six times. In these patients infusion at an unchanged rate results in higher plasma levels at steady state. 0.7-1.2 l/kg bodyweight. Studies show a protein binding of 96 -98%. In animals and humans, midazolam has been shown to cross the placenta and to enter fetal circulation. Small quantities of midazolam are found in human milk. The elimination half -life may also be prolonged in patients with congestive heart failure and with reduced hepatic function. Metabolism Midazolam is metabolized rapidly and completely. The primary metabolise is (-hydroxy-midazolam. The fraction of the dose extracted by liver has been estimated at 40-50%. Many medicaments have been found to inhibit the production of this metabolite in vitro; for some of these In children (3-10 years) the elimination half-life is between 1 and 1.5 hours. In neonates the half-life of elimination is prolonged with a mean of 6 hours (3-12 hours) due to liver immaturity. 286 Monitored intravenous sedation with local anaesthesia for dental outpatients Appendicies the dose should be determined with caution, the special factors relating to each patient being taken into consideration. Indications and usage Conscious sedation before diagnostic or therapeutic procedures with or without local anesthesia (i.v. administration). a) Intravenous conscious sedation The intravenous injection of Dormicum should be given slowly at a rate of approximately 1 mg in 30 seconds. The drug takes effect in about 2 minutes after the injection has been given. Premedication before induction of anesthesia (i.m. or rectal administration in children). Induction and maintenance of anesthesia. As an induction agent in inhalation anesthesia or a sedative component in combined anesthesia, including total intravenous anesthesia (i.v. injection, i.v. infusion). In adults below the age of 60 the initial dose is 2.5 mg given 5 - 10 minutes before the beginning of the procedure. Ataralgesia in combination with ketamine in children (i.m. administration). Further doses of 1 mg may be given as necessary. A total dose greater than 5 mg is usually not necessary. Long-term sedation in intensive care units (i.v. administration as bolus injection or continuous infusion). In adults over 60 years of age, debilitated or chronically ill patients, the initial dose must be reduced to 11.5 mg and given 5-10 minutes before the beginning of the procedure. Further doses of 0.5-1 mg may be given as necessary. A total dose greater than 3.5 mg is usually not necessary. Dosage and administration Midazolam is a potent sedative agent which requires slow administration and individualization of dosage. The dose should be individualized and titrated to the desired state of sedation according to the clinical need, physical status, age and concomitant medication. In adults over 60 years of age, debilitated or chronically ill patients 287 Appendix I b) Anesthesia Rectal administration in children: The total dose of Dormicum ranging from 0.3-0.5 mg/kg bodyweight should be administered 20-30 minutes before induction of anesthesia. Pre-medication: Pre-medication with Dormicum given shortly before a procedure does produce sedation (induction of sleepiness or drowsiness and relief of apprehension) and preoperative impairment of memory. Rectal administration of the ampoule solution is performed by means of a plastic applicator fixed on the end of the syringe. Dormicum can also be administered in combination with anticholinergics. If the volume to be administered is too small, water may be added up to a total volume of 10 ml. The pre-medication is usually administered 20-60 minutes before induction of anesthesia. Intramuscular administration: In adults below the age of 60 the dose of Dormicum ranges from Induction: The desired level of anesthesia is reached by stepwise titration. The intravenous induction dose of Dormicum should be given slowly in increments. Each increment of not more than 5 mg should be injected over 20-30 seconds allowing 2 minutes between successive increments. 0.07-0.1 mg/kg according to the general condition of the patient. The usual dose is 5 mg. In adults over 60 years of age, debilitated and chronically ill, the dose ranges from 0.025-0.05 mg/kg. In pre-medicated adults below the age of 60 the dose can range from 0.15-0.2 mg/kg but a total dose greater than 15 mg is usually not necessary. The usual dose is 2-3 mg. In children between ages of 1 and 15 proportionally higher doses are required than in adults in relation to body weight. The dose range from 0.08-0.2 mg/kg bodyweight has been shown to be effective and safe. In non pre-medicated adults below the age of 60 the dose may be higher (0.3-0.35 mg/kg bodyweight), but a total dose greater than 20 mg is usually not necessary. Dormicum should be administered deep into a large muscle mass 30-60 minutes prior to the induction of anesthesia. In adults over 60 years of age, debilitated and chronically ill patients, lower doses will be required. 288 Monitored intravenous sedation with local anaesthesia for dental outpatients Appendicies Maintenance: The maintenance of the desired level of unconsciousness can be achieved by either further intermittent doses or continuous infusion of intravenous Dormicum typically in combination with analgesics. allowing 2 minutes successive increments. between The maintenance dose usually ranges from 0.03-0.1 mg/kg/hr when used in combination with narcotics or ketamine. In hypovolemic, vasoconstricted or hypothermic patients the loading dose should be reduced or omitted. The intravenous loading dose can range from 0.03-0.3 mg/kg but a total dose greater than 15 mg is usually not necessary. The maintenance dose can range from 0.03-0.2 mg/kg/hr. In adults over 60 years of age, debilitated or chronically ill patients, lower maintenance doses will be required. The level of sedation should be assessed regularly if permitted by patient's condition. In children receiving ketamine for anesthesia (ataralgesia), an intramuscular dose of Dormicum of 0.15 - 0.20 mg/kg is recommended. In hypovolemic, vasoconstricted or hypothermic patients the maintenance dose should be reduced, at times to as low as 25 % of the usual dose. A sufficiently deep level of sleep is generally achieved after 2-3 minutes. When Dormicum is given with potent analgesics, the latter should be administered first so that the sedative effects of Dormicum can be safely titrated on top of any sedation caused by the analgesic. c) Intravenous sedation in the intensive care unit The desired level of sedation is reached by stepwise titration of Dormicum followed by either continuous infusion or intermittent bolus. Special dosage instructions Compatibility with infusion solutions: The Dormicum ampoule solution can be diluted with sodium chloride 0.9 %, dextrose 5 % and 10 %, levulose 5 %, Ringer's solution and Hartmann's solution in a mixing ratio of 15 mg midazolam per 100 1000 ml infusion solution. These solutions remain physically and chemically stable for 24 hours at The intravenous loading dose should be given slowly in increments. Each increment of 1-2.5 mg should be injected over 20-30 seconds 289 Appendix I room temperature, or 3 days at 5 C (see also Special remarks). involuntary movements (including tonic/clonic convulsions and muscle tremor) have also been observed. Should such symptoms suggestive of a paradoxical reaction occur, the response to Dormicum should be evaluated before proceeding. The Dormicum Ampoule solution should not be diluted with Macrodex 6 % in Dextrose or mixed with alkaline injections. Convulsions have been reported in premature infants and neonates. Contraindications Known hypersensitivity benzodiazepines. to Dormicum ampoules should be used only when resuscitation facilities are available, as i.v. administration of Dormicum may depress myocardial contractility and cause apnea. After receiving Dormicum parenterally, patients should not be discharged from hospital or consulting room for at least 3 hours and then only if accompanied by an attendant. Prior to receiving Dormicum, the patient should be warned not to drive a vehicle or operate a machine for at least 12 hours. Precautions Special caution should be exercised when administering Dormicum parenterally to patients representing a higher risk group: adults over 60 years of age, debilitated or chronically ill, patients with obstructive pulmonary disease, with chronic renal failure, impaired hepatic function or with congestive heart failure. These higher risk patients require lower dosages (see Dosage and administration) and should be continuously monitored for early signs of alterations of vital functions. After prolonged i.v. administration of Dormicum, abrupt discontinuation of the product may be accompanied by withdrawal symptoms. Therefore, a gradual reduction of Dormicum is recommended. As with any substance with CNS depressant and/or muscle-relaxant properties, particular care should be taken when administering Dormicum to a patient with myasthenia gravis, owing to pre-existing muscle weakness. Pregnancy, nursing mothers Dormicum - like other drugs should not be used in the first three months of pregnancy unless considered absolutely necessary by the physician. Special care must be taken when benzodiazepines are used during labour and delivery, as high In rare cases paradoxical reactions such as agitation, hyperactivity and aggressivity have occurred; 290 Monitored intravenous sedation with local anaesthesia for dental outpatients Appendicies single doses may produce respiratory depression, hypotonia, hypothermia and poor sucking in the neonate. Midazolam passes into breast milk and in general, should not be administered to breastfeeding mothers. In rare cases paradoxical reactions such as agitation, hyperactivity and aggressivity have occurred; involuntary movements (including tonic/clonic convulsions and muscle tremor) have also been observed. Undesirable effects Local effects on veins (pain on injection and thrombophlebitis) can occur. Dormicum is well tolerated. Slight decrease in arterial blood pressure and slight changes of heart rate and respiration are fairly common. In isolated cases, generalized hypersensitivity, from skin reactions to anaphylactoid reactions, have been reported. Severe cardiorespiratory adverse events have occurred on rare occasions. These have included respiratory depression, apnea, respiratory arrest and/or cardiac arrest. Such life-threatening incidents are more likely to occur in adults over 60 years of age and those with pre-existing respiratory insufficiency or impaired cardiac function, particularly when the injection is given too rapidly or when a high dosage is administered. Dormicum ampoules should be used only when resuscitation facilities are available. Convulsions have been reported in premature infants and neonates. After prolonged i.v. administration of Dormicum, abrupt discontinuation of the product may be accompanied by withdrawal symptoms. After rectal administration, slight euphoria has been observed. a Interactions Enhancement of the central depressive effect may occur when Dormicum is used concomitantly with antipsychotics, hypnotics, anxiolytics /sedatives, antidepressants, narcotic analgesics, antiepileptic drugs, anesthetics and sedative antihistamines. The following adverse events have also been observed: Nausea, vomiting, headache, hiccoughs, laryngospasm, dyspnea, hallucination, oversedation, drowsiness, ataxia. Anterograde amnesia may still be present at the end of the procedure and in isolated cases prolonged amnesia has been reported. There is a potentially relevant interaction between midazolam and compounds which inhibit certain 291 Appendix I hepatic enzymes (particularly cytochrome P 450 III A). Overdosage The symptoms of overdose are mainly an intensification of the pharmacological effects; central depression (from oversedation to coma), mental confusion, lethargy and muscle relaxation or paradoxical excitation. In most cases only observation of vital functions is required. Data clearly indicate that these compounds influence the pharmacokinetics of midazolam and that this may lead to prolonged sedation. At present this reaction is known to occur in vivo with ketoconazole, itraconazole, erythromycin, diltiazem, verapainil and cimetidine, but not with cyclospon'n and nitrendipine. Extreme overdosage may lead to coma, areflexia, cardiorespiratory depression and apnea, requiring appropriate countermeasures (ventilation, cardiovascular support). The effects of overdosage can be controlled with the benzodiazepine antagonist Anexate (active ingredient: flumazenil). Therefore patients receiving the above compounds or others which inhibit P 450 III A together with midazolam should be monitored carefully for the first few hours after administration of midazolam. (Studies have shown that ranitidine has no significant effect on the pharmacokinetics of intravenously given midazolam.) Special remarks One study in-vitro has shown the hydroxylation of midazolam to be inhibited by a number of other substances (e.g. amiodarone, neuroleptics); accordingly, interaction with a whole range of medicaments is theoretically possible. However, there is no evidence that these results are of clinical relevance. Incompatibilities Do not dilute Dormicum ampoule solutions with macrodex 6% in Dextrose. Alcohol may enhance the sedative effect of midazolam. Storage Dormicum ampoules should not be frozen because they can burst. Furthermore, precipitation can occur which dissolves on shaking at room temperature. Do not mix Dormicum ampoule solutions in alkaline injections. Midazolam precipitates in sodium bicarbonate. Stability 292 Monitored intravenous sedation with local anaesthesia for dental outpatients Appendicies This medicine should not be used after the expiry date (EXP) shown on the pack. Medicine: Keep out of reach of children Current at November 1995 Packs Ampoules 5 mg in 1 ml Ampoules 15 mg in 3 ml Ampoules 5 mg in 5 ml Ampoules 50 mg in 10 ml Rectal applicators F. Hoffmann-La Roche Ltd, Basel, Switzerland 10 5 10 5 50 293 Appendix I FLUMAZENIL International Standard Prescribing Information November 1993 ANEXATE RO 15-1788 Anexate (Lanexat in Finland) Flumazenil Benzodiazepine antagonist In animal experiments the effects of compounds showing not affinity for benzodiazepine receptors, e.g. barbiturates, ethanol, meprobamate, GABA mimetics, adenosine receptor agonists, were not affected by Anexate, but those of nonbenzodiazepine agonists of benzodiazepine receptors, such as cyclopyrrolones (e.g. zopiclone) and triazolopyridazines, were blocked. The hypnotic-sedative benzodiazepine effects are rapidly reversed by Anexate after its i.v. injection (within 30-60 seconds) and may reappear gradually within the next few hours, depending on the half-life and dose ratio of the agonist and antagonist. In animal toxicity studies, Anexate proved to be of low toxicity and devoid of mutagenic activity. Anexate may possess some weak intrinsic agonistic, e.g. anticonvulsant, activity. Composition Active ingredient: flumazenil. Ampoules containing 0.5 mg active ingredient in 5 ml aqueous solution and 1 mg active ingredient in 10 ml aqueous solution (for i.v. administration). Excipients: ethylenediaminetetraacetic acid, acetic acid, sodium chloride, sodium hydroxide, water for injections. Properties and effects Anexate, an imidazobenzodiazepine, is a benzodiazepine antagonist which, by competitive inhibition, specifically blocks the central nervous effects of agents acting through benzodiazepine receptors. The antagonistic effect was documented in studies involving 17 different benzodiazepine derivatives. 294 Monitored intravenous sedation with local anaesthesia for dental outpatients Appendicies In animals pretreated with high doses of benzodiazepines over several weeks, Anexate elicited symptoms of withdrawal. Indications and usage Anexate is indicated for reversal of the centrally sedative effects of benzodiazepines. It is therefore used in anesthesia and intensive care in the following indications: Pharmacokinetics Distribution Flumazenil, a weak lipophilic base, is about 50% bound to plasma proteins. Albumin accounts for two thirds of the plasma protein binding. The mean volume of distribution at steady state (Vss 0.95 l/kg) is similar to that of structurally related benzodiazepines. In anesthesia: Termination of general anesthesia induced and maintained with benzodiazepines in inpatiens. Metabolism The carboxylic acid in free and conjugated form is the main metabolite in human urine. In pharmacological tests, this main metabolise was inactive as a benzodiazepine agonist or antagonist. In intensive care: Anexate provides diagnostic indications of intoxication with benzodiazepines or rules such intoxication out. Reversal of benzodiazepine sedation in short diagnostic and therapeutic procedures in both inpatients and outpatients. As a diagnostic measure in unconsciousness of unknown origin to differentiate between involvement of benzodiazepines, other drugs or brain damage. Elimination Flumazenil is almost completely (99%) nonrenally eliminated. 'The mean total plasma clearance of flumazenil is 1 1/min and can be attributed almost entirely to hepatic clearance. The low renal clearance rate suggests effective reabsorption of the drug after glomerular filtration. The average elimination half-life of the drug is 50-60 minutes. As specific reversal of the central effects of benzodiazepines in the drug overdose (return to spontaneous respiration and consciousness in order to render intubation unnecessary or allow extubation). Dosage and administration Standard dosage Anexate should be administered i.v. by an anesthesiologist or experienced physician. For infusion, 295 Appendix I Anexate may be diluted with dextrose 5% or sodium chloride 0.9%; it may also be used concurrently with other resuscitative procedures. Restrictions on use Contraindications In anesthesia: The recommended initial dose is 0.2 mg administered i.v. over 15 seconds. If the desired degree of consciousness is not obtained within 60 seconds, a second dose (0.1 mg) can be injected, and this may be repeated at 60-second intervals where necessary, up to a total dose of 1 mg. The usual dose is 0.3-0.6 mg. Anexate is contraindicated in patients with known hypersensitivity to the drug. In mixed intoxications with benzodiazepines and cyclic antidepressants, the toxicity of the antidepressants can be masked by protective benzodiazepine effects. In the presence of autonomic (anticholinergic), neurological (motor abnormalities) or cardiovascular symptoms of severe intoxication with tricyclics/tetracyclics, Anexate should not be used to reverse benzodiazepine effects. In the intensive care unit: The recommended initial dose is 0.3 mg i.v. If the desired degree of consciousness is not obtained within 60 seconds, Anexate may be injected repeatedly until the patient awakes or up to a total dose of 2 mg. If drowsiness recurs, an i.v. infusion of 0.1-0.4 mg per hour has been shown to be useful. The rate of infusion should be individually adjusted up to the desired level of arousal. Precautions The use of Anexate is not recommended in epileptic patients who have been receiving benzodiazepine treatment for a prolonged period. Although Anexate exerts a slight intrinsic anticonvulsant effect, its abrupt suppression of the protective effect of a benzodiazepine agonist can give rise to convulsions in epileptic patients. In the intensive care unit, in patients treated for a long time with high doses of benzodiazepines, the individually titrated injections of Anexate, slowly administered, should not produce withdrawal syndromes. If unexpected signs of overstimulation occur, 5 mg diazepam or 5 mg midazolam should be given i.v. Patients with severe head injury (and/or unstable intracranial pressure) treated with Anexate to reverse the effects of benzodiazepines may develop raised intracranial pressure. If a significant improvement in consciousness or respiratory function is not obtained after repeated doses of Anexate, a nonbenzodiazepine etiology must be assumed. Effect on driving and other psychomotor skills in outpatients 296 Monitored intravenous sedation with local anaesthesia for dental outpatients Appendicies Although after i.v. administration of Anexate the patients are awake and conscious, they should be warned against engaging in hazardous activities requiring complete mental alertness (such as operating dangerous machinery or driving a motor vehicle) during the first 24 hours after administration since the effect of the originally ingested or administered benzodiazepine may return. injection of Anexate. These undesirable effects usually did not necessitate special treatment. Very rarely, seizures have been reported, particularly in patients known to suffer from epilepsy. Rapid injection of Anexate in patients with long-term exposure to benzodiazepines ending at any time within the weeks preceding Anexate administration may produce withdrawal symptoms and should therefore be avoided. If such symptoms arise, a slow i.v. injection of 5 mg diazepam or 5 mg midazolam should be given. Pregnancy, nursing mothers Although studies in animals given high doses of Anexate have not shown evidence of embryotoxicity or teratogenicity, no controlled studies involving pregnant women have been conducted. Attention is therefore drawn to the general medical principle that no drugs should be administered in the early stages of pregnancy except where absolutely necessary. Interactions Anexate blocks the central effects of benzodiazepines by competitive interaction at the receptor level. The effects of nonbenzodiazepine agonists at benzodiazepine receptors, such as zopiclone, triazolopyridazines and others, are also blocked by Anexate. Parental administration of Anexate in emergencies is not contraindicated during lactation. Particular caution is necessary when using Anexate in cases of mixed drug overdose since the toxic effects (such as convulsions and cardiac dysrhythmias) of other drugs taken in overdose (especially cyclic antidepressants) may emerge with the reversal of the benzodiazepine effects by Anexate. Undesirable effects Anexate was well tolerated even at high parenteral doses of up to 100 mg. In rare cases during use in anesthesia, flush, nausea and/or vomiting have been reported. Complaints such as feeling of anxiety, palpitations and fear have been infrequently observed after rapid The pharmacokinetics of benzodiazepine agonists are unaltered 297 Appendix I in the presence of Anexate and vice versa. Stability This medicine should not be used after the expiry date (EXP) shown on the pack. Overdosage Even when given at a dosage of 100 mg i.v., no symptoms of overdosage were observed. For withdrawal symptoms attributable to the agonist, see under Standard dosage. Packs Ampoules 0.5 mg in 5 ml Ampoules 1 mg in 10 ml 5,25 5,25 Medicine: keep out of reach of children Special remarks Current at November 1993 Please note When used in anesthesiology at the end of an operation, Anexate should not be injected until the effect of peripheral muscle relaxants has subsided. F. Hoffmann-La Roche Ltd, Basel, Switzerland 298 Monitored intravenous sedation with local anaesthesia for dental outpatients Appendicies DIAZEPAM The national board of health Summary of product characteristics for Stesolid Emulsion, injection 26 October 1995 1. Trade name of the medicinal product Stesolid Emulsion 2. Qualitative and quantitative composition Diazepam 5 mg/ml 3. Pharmaceutical form Injection 4. 4.1 CLINICAL PARTICULARS Therapeutic indications Conditions of anxiety and restlessness. Attacks of convulsions. Spasticity. Alcohol withdrawal symptoms. Pre-anaesthetic medication. Induction of anaesthesia and short-acting anaesthesia. 4.2 Posology and method of administration Convulsions: Adults: 10-20 mg by slow intravenous injection, repeated if necessary. Children: 0.25-0.5 mg/kg by intramuscular or slow intravenous injection. Pre-anaesthetic medication: 0,2 mg/kg intramuscularly, or 0.1-0.2 mg/kg by slow intravenous injection. Reduce the dose for elderly patients. 4.3 Contra-indications Myasthenia gravis. Sleep apnoea. Severe liver insufficiency. Acute respiratory depression. 4.4 Special warnings and precautions for use Very slow intravenous injection, owing to the danger of respiratory depression. Reduced dose for elderly patients. Habituating. 299 Appendix I 4.5 Interaction with other medicaments and other forms of interaction Alcohol, hypnotics, neuroleptics, antihistamines, clonidine, and opioids potentiate the sedative effect. Cimetidine, disulfiram, and oestrogen reduce the rate of metabolism. Omeprazole may prolong the elimination time of diazepam. Theophylline counteracts the sedative and psychomotor actions of diazepam. 4.6 Pregnancy and lactation Pregnancy: May be used, but not in the last trimester. Lactation: Should not be used. 4.7 Effect on ability to drive and use machines Warning symbol. 4.8 Undesirable effects Tiredness. Drowsiness. Dizziness. Loss of memory, Ataxia. Disturbance of the balance. Anterograde amnesia. Confusion. Paradoxical reactions, such as confusion, excitation, and dysphoria, may occur (particularly in children and elderly patients). Respiratory depression. Phlebitis. 4.9 Overdose Loss of consciousness rising to come. Respiratory depression. Treatment: Symptomatic, possibly flumazenil. 4.10 Dispensing category A. 5. PHARMACOLOGICAL PARTICULARS 5.0 Therapeutic classification N 05 BA 01 5.1 Pharmacodynamic properties Pharmacotherapeutic group: Anxiolytic, belonging to the benzodiazepine group. Mode of action: Diazepam is an agonist, which binds to specific benzodiazepine receptors in the brain, thereby potentiating the normal transmission of the signal substance, GABA. GABA inhibits the transmission of important signal substance, thus resulting in neuronal inhibition. The muscle-relaxing effect is mediated via spinal synaptic reflexes. 300 Monitored intravenous sedation with local anaesthesia for dental outpatients Appendicies Pharmacodynamic effects: Diazepam is an anxiolytic, which acts by suppressing the symptoms of anxiety, restlessness, and tension. Moreover, diazepam possesses sedative and muscle-relaxing actions. 5.2 Pharmacokinetic properties Distribution: The maximum plasma concentration sets in within 30-60 minutes of intramuscular injection of diazepam. Intravenous injection of diazepam 10 mg produces a maximum plasma concentration of about 600 ng/ml within a few minutes. Further distribution brings about a marked fall in the plasma concentration lasting for 2-4 hours. Protein binding: 96-98%. Diazepam is lipid-soluble, penetrates tissue well, and crosses the blood-brain barrier. Metabolism: Diazepam is metabolised chiefly in the liver by hydroxylation and glucuronidation. The half-life of N-desmethyldiazepam, the metabolically active metabolite, is 2-4 days. Elimination: Diazepam is eliminated chiefly with the urine in the form of metabolites and about 10% is excreted with the faeces. Half-life: Adults: 2050 hours, elderly patients 70-100 hours. Children: premature infants 40-110 hours; new-born full-term infants about 30 hours; up to 1 year of age about 10 hours; and above 1 year of age about 20 hours. 5.3 Preclinical safety data 6. PHARMACEUTICAL PARTICULARS 6.1 List of excipients Diazepam, fractionated soya bean oil, diacetylated monoglycerides, fractionated egg phospholipids, glycerol, sterile water. 6.2 lncompatibilities Miscibility: Intralipid in all concentrations. Glucose solutions 55-300 mg/ml in glass infusion bottles. May be injected through an infusion tube while the infusion is being given. Adsorption of diazepam to polyvinyl chloride infusion containers may occur. 6.3 Shelf life 18 months. 6.4 Special conditions for storage Room temperature. 301 Appendix I 6.5 Nature and contents of container Glass ampoules. 6.6 Instructions for use/handling None. 7. Marketing authorisation holder A/S Dumex (Dumex Ltd) Prags Boulevard 37, DK-2300 Copenhagen S. 8. 9. Marketing authorisation No. 9850 Date of authorisation/revision of summary of product characteristics 26 October 1995. 302 Monitored intravenous sedation with local anaesthesia for dental outpatients Appendicies LIDOCAINE CATALOGUE TEXT 23.3.1981 XYLOCAIN ADRENALIN 20 mg/ml + 12,5 microg/ml solution for injection (Declaration) Dosage Lidocaine hydrochloride anhydrous 20 mg, adrenaline tartrate corresp. to adrenaline 12,5 microg (1:80 000), sodium chloride, sodium metabisulphite, methylparahydroxybenzoate 1 mg, water for injection to 1 ml. Usually 1-2 ml (20-40 mg lidocaine chloride). With surgery 2-35 ml (40-60-100 mg lidocaine chloride). Larger doses may be used in special cases. Larger dose than 25 ml = 13 cylinder ampoules (500 mg lidocaine chloride) should not be exceeded. Dose for children and debilatated has to be lower. (Description) In infiltration anesthesia the duration of analgesia in pulpa is 60 minutes when Xylocaine Adrenalin 20 mg/ml + 12,5 microg/ml is used. Due to the long duration of analgesia and remarkable ischemic effect this preparation is effective and gives good visibility to the site of operation. Adverse events Undesirable reactions are very rare in the doses used in dental procedures. Vertigo and drowsiness may occur now and then followed by overdosage or in connection with decreased tolerance. Symptoms do not usually require special treatment. Serious undesirable reactions may occur followed by clear overdosage, accidental i.v. injection or in connection with decreased tolerance. The nature of complications depends on the volume of the dose, the administration route and the status of the patient. Undesirable reactions Indications Local analgesia (anesthesia) with odontological surgery, complicated extractions and gingival surgery. The preparation has a good ischemic effect. 303 Appendix I are mainly CNS and/or cardiovascular reactions. CNS effects cause depression of the cerebral cortex and medulla oblongata. Cerebral cortex effects manifested in anxiety, drowsiness, blurred vision, difficulties to speak, tremor and convulsions. Medulla oblongata effects induce vomiting, paleness, cold sweat and finally apnoea (respiratory depression). Hypotension is a sign of cardiovascular effect and it may occur after, concomitantly or also before CNS excitation. Myocardial depression may lead to cardiovascular collapse and possible cardiac arrest. affecting the child at therapeutic levels. Serious reactions have to be treated rapidly by ventilation, (resuscitation), administrating barbiturates or muscular relaxants. 2 years. Keep cool but free from frost. Reactions caused by an overdose of adrenaline see professional literature. Metal ions may dissolve e.g. from cannules and syringes containing metal parts. Solution must not be kept long in contact with metal surfaces, since dissolved metal ions may cause severe local irritation (swelling) at the site of injection. There is no data if adrenaline excreted in the breast milk, but it is very unlikely that adrenaline has absorption in the gastrointestinal channel of the child. Interactions Adrenaline may increase the effect of tricyclic antidepressants. Storage and shelf-life Sensitive to light, keep in box. Pregnancy and lactation Lidocaine has been used in large number of pregnant women. An increased incidence of malformations or direct or indirect harmful effects on the foetus have not been reported. Lidocaine is excreted in the breast milk, but there is generally no risk of Packages Cylinder ampoules 100 x 1,8 ml Self-aspiriting cylinder ampoules 100 x 1,8 ml 304 Monitored intravenous sedation with local anaesthesia for dental outpatients Appendicies PRILOCAINE CATALOGUE TEXT CITANEST OCTAPRESSIN 30 mg/ml + 0,54 microg/ml solution for injection toxicity and it is well tolerated. It is suitable as a routine localizing agent provided that local ischemia is not essential in the injected area. (Declaration) Prilocaine hydrochloride 20 mg, felypressin 0,54 microg, sodium chloride, water for injection to 1 ml. Felypressin is tissue friendly and it has a very low toxicity. Animal studies has shown that felypressin in low concentrations effects only capillars in veins when adrenaline and noradrenaline effect capillars both in veins and in arteries. The localizing effect of felypressin increases local anaesthesia without causing ischemia in the injected area. (Description) Citanest Octapressin contains local anaesthetic, prilocaine, and vasopressin analogue, felypressin. Felypressin has a local effect differently from adrenaline. Thus Citanest Octapressin gives an optimal local analgetic effect without any significant ischemia. Citanest Octapressin 30 mg/ml + 0,54 microg/ml solution has the same anaesthesia frequence, reaction time, distribution and potency of anaesthesia as Xylocain Adrenaline 20 mg/ml + 12,5 microg/ml solution has. Duration of infiltration anaesthesia is a little shorter when used Citanest Octapressin than when used Xylocain Adrenaline. Duration of mandibular anaesthesia is as long as when used Xylocain Adrenaline 20 mg/ml + 12,5 microg/ml solution. Citanest Octapressin has a low Indications (In dentistry) Infiltration anaesthesia, where there is no need for ischaemia in the injected area. Regional nerve block anaesthesia. Duration of infiltration anaesthesia in pulp is about 45 minutes. 305 Appendix I events (vertigo, drowsiness) may sometimes occur followed by moderate overdosage, or in connection with decreased tolerance. Usually in these cases there is no need for special treatment. Serious undesirable reactions in dental procedures are very rare but they may occur followed by clear overdosage, accidental i.v. injection or in connection with decreased tolerance. The nature of complications depends on the volume of the dose, the administration route and the status of the patient. Undesirable reactions are mainly CNS and/or cardiovascular reactions. CNS effects cause depression of the cerebral cortex and medulla oblongata. Cerebral cortex effects manifested in anxiety, drowsiness, blurred vision, difficulties to speak, agitation and at last tremor and convulsions. Medulla oblongata effects induce vomiting, paleness, cold sweat and finally apnoea (respiratory depression). Hypotension is a first sign of cardiovascular effect and it may occur after, concomitantly or also before CNS excitation. Myocardial depression may lead to cardiovascular collapse and possible cardiac arrest. Dosage Usually 1-2 ml (30-60 mg lidocaine chloride). Maximum dose 600 mg = 20 ml = 11 cylinder ampoules. Dose for children and debilatated have to be lower. Contraindications Hypersensitivity anaesthetic agents. to local Pregnancy and lactation Citanest Octapressin has been administered to a large number of pregnant women. An increased incidence of malformations or direct or indirect harmful effects on the foetus have not been reported. Prilocaine is excreted in breast milk, but there is generally no risk of affecting the child at therapeutic levels. It is not known whether felypressin is excreted in breast milk. Adverse events Undesirable reactions are very rare in the doses used in dental procedures. Allergic reactions. Allergic reactions (in the most severe instances anaphylatic shock) to local anaesthesia of the amide type are rare. When larger doses are used it may in some cases occur paleness in face due to the effect of Octapressin in veins and it is not a symptom of reduced blood pressure. Mild adverse Serious reactions have to be treated rapidly by ventilation, (resuscitation), administrating barbiturates, diazepam or muscular relaxants. 306 Monitored intravenous sedation with local anaesthesia for dental outpatients Appendicies Packages Methemoglobin. Increase of methemoglobin or clinical symptoms of methemoglobinemia has not been reported with recommended doses. However, methemoglobin may form when used high doses. Prilocaine 600 mg (= 11 cylinder ampoules) may increase methemoglobin level from about 1 % (normal value) to 4 - 6 %. Hemolysis does not follow this. Cylinder ampoules (clear) 100 x 1,8 ml Self-aspiriting cylinder ampoules 100 x 1,8 ml Cylinder ampoules have been hygienically packed in blisters. They are for single-use. Preparation does not contain preservatives. Discard residue. Special warnings ATC-code Studies has shown that there is no interaction between Citanest Octapressin and tricyclic antidepressants. N01BB04 Storage and shelf-life 3 years in room temperature. Avoid freezing. Sensitive to light, keep in box. Metal ions may dissolve e.g. from canules and syringes containing metal parts. Solution must not be kept long in contact with metal surfaces, since dissolved metal ions may cause severe local irritation (swelling) at the site of injection. 307 Monitored intravenous sedation with local anaesthesia for dental outpatients Appendicies 7.2 APPENDIX II QUESTIONS AND PATIENTS COMMENTS OF STUDIES 4 AND 5 309 Monitored intravenous sedation with local anaesthesia for dental outpatients Appendicies According to my patient files I have performed a dental procedure for you using sedative premedication. I am presently collecting scientific data concerning these procedures. Therefore I am asking you to please kindly fill in the enclosed questionnaire concerning your dental care, and return it to me in the enclosed envelope. I would appreciate it if you could answer the questions as soon as possible and return the questionnaire within a week The study is a part of my thesis “Premedication in Dental Care” supervised by Mr. Risto Kotilainen, Professor (oral surgery) and Mr. Matti Mattila, Docent (Anaesthesiology) in the University of Kuopio. The questionnaire will not reveal your name, nor is there any chance that your person would be disclosed at any stage of the study. This ensures that you can make your answers as honest as possible. The study material is divided into two patient categories: those who seeked this treatment mainly because of fear and those who were applied sedative medication because of the nature of the procedure. This is why there may be points in the questions that seem difficult or impossible to answer. In such a case you may simply ignore the question. You may write your answer next to the question if “yes/no” answers or the “tick the right box” method does not seem natural for a question. It is always possible to tick several boxes. In the “yes/no” alternatives, please strike out what is not appropriate. I want to thank you in advance for your trouble. Your help is invaluable in my work. Elimäki, 7th June 1993 Kari Luotio Dentist tel. 951-77126 P.S. If you have any questions, please do not hesitate to phone me. The best time to reach me is after 8 o’clock P.M. 311 Appendix II The first group of questions define the reasons which made you seek this method of treatment. 1. Primary division a. I wanted this treatment primarily because of fear b. I needed other treatment that was carried out in premedication c. Other alternative, which? _____________________________ If you chose alternative “b” in the first point, please do not answer the four following questions but continue directly from point 6. 2. Why did you seek treatment in premedication? a. I wanted my teeth treated within one appointment b. I am afraid of the pain involved in dental procedures c. I am afraid of local anaesthesia d. I have painful experiences of dentistry e. My dentist - patient relationships always end at the start f. Other reason, what? __________________________________ 3. What has been the main reason for the discontinuation of previous dentist patient relationships? __________________________________________ 4. Why did you not seek dental care in sleep (general anaesthesia)? a. I am afraid of anaesthesia b. Anaesthetic treatment is much more expensive c. No anaesthetic treatment was available d. Other reason, what? ___________________________________ 5. What was the real initiative for you this time as you seeked treatment? a. Another person’s recommendation of a dentist b. The pressure from my spouse or some other next of kin c. Disadvantageous changes in appearance d. Bad smell/taste in the mouth or in breath e. Pain, infection or other such symptom f. Other reason, what? ___________________________________ 312 Monitored intravenous sedation with local anaesthesia for dental outpatients Appendicies 6. What procedures were made this time? a. Denture or a traditional bridge b. A denture fitted in the jawbone c. Surgical procedure, e.g. extraction d. Filling e. Gingivitis treatment 7. How long time was it since your previous appointment to the dentist? __________ years 8. Did you at that time seek treatment because of toothache? Yes / no 9. Was the treatment then discontinued? (Please strike out what is not appropriate) Yes / no 10. When were your teeth last fully treated, or the treatment was finished? _______ years earlier The second group of questions deals with your socio-economic background and the answers should be given according to the situation you were in at the time of the treatment. 11. How old were you when the procedure was carried out? __________ years 12. Are you male / female (please strike out what is not appropriate) 13. Were you at that time a. married b. living together c. divorced d. single 313 Appendix II 14. How many children did you have at that time? __________ children 15. What was your education? a. Comprehensive school b. Vocational college c. College d. University 16. Did you then live a. in your own apartment b. in a rented apartment c. as a subtenant d. with your parents e. in another form of housing Did you then work 17. a. as an employee b. as private entrepreneur c. I was not working d. I was unemployed e. I was student 18. a. b. c. d. in a leading position in a supervisory position as a qualified worker as unskilled labour 19. What was your profession? ____________________________ 20. What was the level of income (rounded in the nearest thousand marks) of your family (the household you lived in at the time)? Gross earnings ca. _________ FIM/month 21. What was your personal level of income at that time? Gross earnings ca. _________ FIM/month 314 Monitored intravenous sedation with local anaesthesia for dental outpatients Appendicies 22. Did you have difficulties in covering the expenses of the treatment? Yes / no 23. Did you receive any reimbursements for the treatment costs from the National Pensions Institute? Yes / no How much? Some _______ % 24. Did you receive other reimbursements? Yes / no From where? _______________ How much? _______________ 25. Do you feel that this type of treatment should be a. Free of charge (100 % reimbursement) b. With nominal charge (90 % reimbursement) c. Partly reimbursed (50 %) d. Society should not participate in the costs of this type of treatment. 315 Appendix II This page is an example to explain for you how to answer the questions in the following pages. Question: Was there any pain during the procedure? The purpose is that you imagine a scale where one end is marked by “the greatest imaginable pain” and the other end is marked by “not the slightest feeling of pain”. You would then think where in this scale your experience concerned would be situated. You will find vertical lines in the following pages and next to them words to help identify the feelings. To this scale you should insert a cross line or a cross at the point where you think your feelings would fit in. Model answer in words: “I faintly remember a slight pain towards the end of the treatment, but I cannot even remember what it was connected to.” You would then draw a cross somewhere between “no pain” and “slight pain”. Model answer drawn on the scale: Immense Severe Slight Insignificant (or none at all) 316 Monitored intravenous sedation with local anaesthesia for dental outpatients Appendicies The next group of questions deals with how you experienced the treatment itself. 26. Please insert a line to the scale below at places that in your opinion best describe your experience of the treatment. General impression of the treatment Satisfaction to treatment Wonderful Happy Pleasant Pleased Unpleasant Unsatisfied Objectionable Disappointed 27. Which procedures where made at that time? a. filling b. excavation c. scaling tartar from teeth d. surgery 28. If the procedure were to be made again, would it be done? a. in the same way, or with premedication b. conventionally with local anaesthesia c. even without local anaesthesia d. in sleep (general anaesthesia) 317 Appendix II 29. Could you recommend this method of treatment to others? Yes / no 30. Have you been able to personally make an appointment or make ordinary consultation calls to the dentist after this treatment? Yes / no 31. Please insert lines to the scale below at places that in your opinion best describe your sensations during treatment. Pain Fear Drowsiness Anxiety Confusion Immense Strong Slight Insignificant The last group of questions will deal with the consequences of the treatment. 32. Did you have any of the following symptoms between end of the dental procedure and falling asleep back home, and if yes, how much? a. Confusion ____________ b. Drowsiness ____________ c. Pain ____________ d. Headache ____________ e. Nausea ____________ f. Vomiting ____________ g. Other, what? __________________________ 318 Monitored intravenous sedation with local anaesthesia for dental outpatients Appendicies 33. After you woke up, did you have any of the following symptoms, and how much? a. Confusion ____________ b. Drowsiness ____________ c. Pain ____________ d. Headache ____________ e. Nausea ____________ f. Vomiting ____________ g. Other, what? __________________________ 34. Again, please draw a line that describes your general condition at the following stages: From end of treatment to falling asleep at night From the following morning to the following night Excellent Good Poor Miserable 319 During the week following treatment Appendix II 35. How many hours after the treatment did you consider yourself sleepy or confused? _____________ hours 36. What is your escort’s view on the above question? ____________ hours 37. What time did the procedure begin? At _____________ 38. What time did the procedure end? At _____________ 39. What time did you fall asleep after the procedure? At _____________ 40. What time did you then wake up? At _____________ 41. Did you consider yourself able to work the following morning? Yes / no 42. What is your escort’s / spouse’s view of the above? Yes / no 43. Did you consider yourself able to drive a car the following morning? Yes / no 44. What is your escort’s /spouse’s view of the above question? Yes / no 45. What do you think the symptoms you experienced came from? a. From the procedure itself b. From local anaesthesia c. From premedication d. Other, what? __________________________________ 46. What symptoms do you think followed the premedication? ________________________________________________________ ________________________________________________________ 47. How many months is it since the procedure was made? (Please answer in months, not in years) _____________ months 320 Monitored intravenous sedation with local anaesthesia for dental outpatients Appendicies Here I have reserved some space in case you would like to share your ideas on the procedures and your experiences. Please feel free to use also the back of the page when needed. ________________________________________________________ ________________________________________________________ ________________________________________________________ ________________________________________________________ ________________________________________________________ ________________________________________________________ Finally I have marked your medication below with a code. Your person will not be disclosed from this. do st fe mu xy ci 321 ta dg co Appendix II Answers to question 3: 1: 5: 6: 7: 9: 13: 14: 15: 16: 17: 19: 21: 22: 23: 26: 27: 29: 31: 35: 37: 39: 40: 41: 43: 44: 46: 48: 51: 52: 53: 94: 95: 96: 99: 102: 106: 108: Fear of pain Previous appointment 15 years earlier, fainting in the middle of the procedure, scolded by dentist in addition to all the pain Have not been allowed to seek treatment before pains Fear, getting bored of the many appointments Change of address Dentist’s lack of consideration, did not use enough anaesthetic Timidity Fear The dentist moved away from the district Moving away from the areas A long trip Fear Fear, fainting, nausea Fear Pain A renewing pain under old fillings Pain during treatment Lack of time, fear, financing Financial situation Fear Moving away from the area The previous dentist, Mr. Mönkkönen, discontinued his surgery Pain, fear Fear Fear I was afraid of pain the previous dentists had been harsh and hurt me Fear Too painful procedures Indifference, carelessness Fear Neglected teeth - carelessness, fear Cannot easily leave from work (long distances) Have not had so-called treatment plan before (now own financing) Extremely long intervals between treatments Poor result of treatment The patient - dentist relationship did not end but I changed dentist. Bad experiences 322 Monitored intravenous sedation with local anaesthesia for dental outpatients Appendicies Comments written at the end: Patient 1: Maybe (I will make a new appointment) if I will get toothache, but I do not think I will go to a dentist voluntarily. I’m really happy as my teeth were done in one single appointment. I recommend to all who are afraid of going to the dentist. Patient 2: My childhood experiences (of the dentist are) really bad. All milk teeth were excavated and that caused my present fear. I will recommend to all who suffer from fear of dentist. The procedure was so painless and, I think, a simple thing. Maybe next time I can agree to treatments without premedication, and to get all done at once is in my opinion a positive thing, and the fact that I was being informed all the time on what was being done in my mouth. Finally. With the school scale from 4 to 10 I give 10+ for my own experience! I was so pleased. I wish you a nice summer. Patient 5: (My) previous appointment (was) 15 years ago, fainting in the middle of procedure, I was scolded by the dentist in addition to all the pains (and this ended all my previous patient - dentist relationships). Patient 6: During the procedure (towards the end, if I can remember it correctly) I was cold and shaky. I don’t know if this would have been caused by end of effect of medication, the situation was remedied in due course. The pains I experienced afterwards were caused mainly by the many fillings done, and they were mild. 323 Appendix II Patient 7: (My earlier dentist - patient relationships were discontinued due to) fear, getting bored to the many appointments. I knew there were many large holes. I had gone through general anaesthesia many times in previous surgeries (so I did not wish general anaesthesia). I have shared my positive experiences on premedication, and many people have been interested in this. Even a stranger once called me and asked how he could get such a treatment and where. Patient 8: I did not feel the excavation. The surgery felt like milling, but I felt no pain. If I had known before what the procedure would be like, I would not have had to fear so much. Patient 12: I recommend to all who suffer from fear. Patient 13: I was pleased with the procedures and will recommend to others who are afraid of going to the dentist. Patient 14: I am pleased with the procedure and from my experience I can recommend this to others. Patient 16: Despite anticipating fear, the procedure was painless. The symptoms that followed were caused by the number of teeth that were being excavated. The pain killers I received were efficient. Patient 17: I have discussed dental care in premedication with another person who suffers panic disorders. Our experiences were similar, or the premedication takes away the feeling of pain (anaesthesia) but a strong mental anxiety remained. The need to escape - typical for a panic disorder patient - (you’ve got to get away) was immense. (The muscles were relaxed but not the mind.) Thinking about it afterwards, it was an unpleasant experience for me mentally. But I was very pleased with the result. 324 Monitored intravenous sedation with local anaesthesia for dental outpatients Appendicies Patient 19: The procedures I felt were very appropriate and pleasant. No unpleasant sideeffects. I warmly recommend this method of treatment for everyone. Patient 20: A sister of my late husband’s she cannot take pain either in connection with dental care, and therefore she cannot get herself to the dentist she has been very interested in this treatment of mine she is 30 years old. In my case this is the only method of treatment as far as oral treatment is concerned. Patient 21: The premedication was probably so mild that no symptoms followed the treatment. During the procedure the filling caused some pain, but not disturbingly. All in all the most pleasant dental appointment I’ve had. Patient 22: I think the procedure should have been done with less premedication. Is it possible that the tachycardia of the heart could be caused by anaesthesia? Also my blood pressure rose, whether this is normal I do not know. All in all a good experience as I felt no fear, the resulting drunkenness was a little unpleasant. This may be caused also because I have not felt well for a year. Patient 23: (answer to question 5) The advertisement that gave the image that fear and its causes are accepted, not underestimated. Also the feeling that people care. Patient 26: The procedures were painless and fast. Patient 29: If I had guessed this was so painless I would have had my teeth treated earlier. Patient 33: I am fully satisfied myself, and relieved of many years’ pain; fast and careless, even a pleasant experience. I recommend to people easily scared or with weak teeth. 325 Appendix II Patient 34: I am a panic disorder patient. Dispite the premedication I was still anxious. Panic! The premedication during procedure was not strong enough? I was disappointed with the effects of premedication. It was not effective enough, that’s why I was afraid during the procedure. And had to take painkillers astonishingly many days, ca. one week. Then at first the pain was relieved. Next time I have a tooth excavated, I would like to undergo general anaesthesia. Patient 35: The experience of the procedure most positive, can recommend to others! Patient 36: In all ways a pleasant and polite experience! Patient 41: I recommend and have already recommended the treatment in question for my friends/relatives. I understand fear for dentist is very common. Patient 42: The procedure was a pleasant experience. I have recommended also for other “cowards”. Patient 43: A very good treatment cannot be blamed really good Patient 45: It was all over in one go, beautifully. Patient 46: In my opinion the use of a sedative or premedication is excellent for patients who are genuinely afraid of the pains experienced at the dentist’s, and afraid of the suspense which for me is very intense. My experiences at Mr. Kari Luotio’s surgery have been excellent. I think Mr. Luotio always shows personal consideration of the patient, and I could not imagine going to any other dentist. I recommend premedication also for others who suffer pain and fear, and I have told many people about it and many have asked for the place from me, where you may have it, even from other regions. A really good method of treatment. 326 Monitored intravenous sedation with local anaesthesia for dental outpatients Appendicies Patient 47: The procedure was quite pleasant the days that followed were awful the pain indescribable. Patient 48: A pleasant experience, at first I was a little scared. The fear went away after medication. Time just flied (3,5 hours). No consequences the following morning. Patient 50: It is a relief to know that there is such a possibility, if there will be other major procedures with anaesthesia. I was aware of what was happening and I recall our talks but I felt nicely like “who cares!”. Patient 51: Otherwise I’m most pleased to the procedure being done with premedication, but at some stage I felt a severe pain, fortunately only for a moment. Too little medication? I cannot remember a thing of the procedure, or it felt like general anaesthesia. I am pleased. Patient 54: Painkilling medication immediately (0-0,5 hours) after procedure, or even the first painkiller from the dentist! Patient 57: I am a worrier by nature all new things make me wonder. As I get to know them the suspense disappears. I felt quite calm before the procedure. Patient 58: There was no effect to the ability to work the next morning; the procedure as such was so large that it had an effect e.g. to the ability to speak and eat. Patient 62: No negative comments about premedication. Patient 64: The experience did not cause anxieties, even though one might think so at first. When needed I will recommend this also to others. 327 Appendix II Patient 65: I was prejudiced at first, that fitting the implant would be painful. I am surprised the procedure went quite painlessly in my opinion. Patient 70: “Through difficulties to victory!” Patient 73: By far the biggest problems were those caused by temporary loose dentures. Patient 75: The most unpleasant thing after the procedure was a quite marked swelling in the cheek on the side that was operated, and it lasted a few days. Patient 76: A week after the procedure I was more tired than usually, otherwise I felt really good. Patient 77: Taking the medicine caused quite a strong pain in the stomach. The results up to now are good. Patient 79: Drilling the denture into the jawbone was a suprisingly painless procedure. The only disadvantage here is a seemingly lengthy process. Patient 82: The experience was pleasant and painless, I did not need any painkillers. Healing was fast but due to the nature of my work 3 days off work was adequate. The stitches had melted some 9 days from procedure. I can recommend this to others!! THANK YOU! Patient 83: I am very pleased with the result. Patient 85: I have told about this to many people and I warmly recommend premedication in dental care. 328 Monitored intravenous sedation with local anaesthesia for dental outpatients Appendicies Patient 86: Through this procedure I have been greatly helped with my teeth. I am really happy that I found the person who committed himself to look after these teeth. Here in the country possibilities are very weak and getting information on this kind of treatment is quite difficult. I am disappointed with public dental care if their resources or skills run out. Continuation or advice for additional care are bleak. The only advice I have got was that we’ll wait and then fit in dentures. Patient 88: The experience of the operation was painless and pleasant. I felt calm and safe. I can recommend this to everyone. The resulting pains healed fast. Patient 92: I have been very pleased with the treatment given, and the general attitude. I have also recommended the treatment to my friends and openly told them what I have been able to. Patient 93: My best experience on a dentist appointment! Patient 96: You know for yourself “where you are” and may partly participate in the treatment. Feel quite calm during the procedure. Not confused after the procedure. Patient 97: During the two-hour operation I felt good. Time passed surprisingly quickly. Patient 98: If painkiller is injected in the vein during treatment the procedure is pleasant this was the case the first time. The second time, as far as I know, I did not receive a painkiller injection and the procedure was a little more painful. Patient 100: After the operation I felt a little drowsy, but the most annoying thing was only a somewhat “strange feeling” in the mouth. 329 Appendix II Patient 106: I sat with an open mouth for two hours but it seemed short, I felt no pain. I felt a little tipsy. It was an altogether nice experience. I sat in the chair with confidence and did not feel the anxiety I usually feel at the dentist’s. I can recommend (and have already recommended) the same treatment for others (if their wallet can take it). Patient 107: The treatment was a most pleasant experience, painless, and in today’s busy life a fine thing as you do not need to run back and forth to the dentist’s. This method of treatment should be increased, I mean more of these dentists who make procedures all in one time. Patient 108: I was pleased with the procedure, such a large “redecoration” done with suprisingly little pain. I felt no confusion and quickly recovered from the premedication. I can recommend it. 330 Monitored intravenous sedation with local anaesthesia for dental outpatients Appendicies 7.3 APPENDIX III PLETYSTOMOGRAFIC PULSE WAVE Published with permission of Datex 331 Monitored intravenous sedation with local anaesthesia for dental outpatients Appendicies CONTENTS 1 2 3 4 5 ARTERIAL FINGER CIRCULATION REGULATION OF ARTERIAL CIRCULATION REGISTRATION OF THE PULSE WAVE SHAPE AND COMPONENTS OF THE PULSE WAVE TYPICAL VARIATIONS IN THE PULSE WAVE DURING ANAESTHESIA 6 CONCLUSIONS BASED ON CHANGES IN THE AMPLITUDE OF THE PULSE WAVE DURING ANAESTHESIA 7 DIFFERENTIAL DIAGNOSIS 8 THE PLETHYSMOGRAPHIK WAVEFORM DISPLAYED BY DATEX-ENGSTROM MONITORS 9 BENEFITS OF THE PLETHYSMOGRAPHIC WAVEFORM 10 DETERMINATION OF THE PULSE WAVE 11 TREND DISPLAY 12 SUMMARY 333 Appendix III 1 ARTERIAL FINGER CIRCULATION Pulsatile blood flow causes distinct variations in the amount of blood in the vascular bed of the finger due to the relatively large number of arterioles near to the skin. the vascular bed of the finger with arterial blood. Photoelectric finger plethysmography registers the volume changes in arterial blood, and a positive deflection denotes blood volume increase at the place of measurement (finger). Pulsatile blood flow in the finger is the result of left ventricle contractions of the heart, which fill Fig. 1. The effect of blood volume changes on the plethysmogram. The diameter of the blood vessel increases when the local blood volume increases following heart contractions. 334 Monitored intravenous sedation with local anaesthesia for dental outpatients Appendicies 2 REGULATION OF PERIPHERAL ARTERIAL CIRCULATION Vasoconstriction is induced by sympathetic stimulation of the smooth muscle of the peripheral arterial bed. This results in a decrease in pulse wave amplitude (Fig. 2). lists some factors which affect vasodilatation and vasoconstriction. The decrease in pulse wave amplitude is very often related to discomfort, pain or other stress-related stimuli (Table 1). The effect of the sympathetic tone varies greatly in the individual. Fig. 3 Fig. 2. The effect of vasoconstriction and vasodilatation on pulse wave amplitude. 335 Appendix III Fig. 3. Factors influencing vasoconstriction and vasodilatation . Table 1. Typical discomfort and pain. causes of DISCOMFORT OR PAIN DURING ANAESTHESIA • Preoperative anxiety • Endotracheal intubation • Skin incision • Periods of superficial anaesthesia • Supefficial level of anaesthesia • Postoperative discomfort • Postoperative pain VASODILATATION Changes in the pulse wave amplitude during anaesthesia are normally related to neurogenic- or humorally-determined changes in the smooth muscular tonus of the arterial walls. • Anaesthetics • Sedation • Hypercarbia VASOCONSTRICTION • Fear • Pain • Low temperature • Hypovolemia • Hypocarbia 336 Monitored intravenous sedation with local anaesthesia for dental outpatients Appendicies 3 REGISTRATION OF THE PULSE WAVE Photoelectric plethysmography measures the absorption of incident light at an infrared wavelength (910 nm in Datex-Engstrom pulse wave oximeters). The absorption of infrared light is not significantly affected by changes in the oxyhemoglobin concentration, see Fig. 4, so changes in light absorption essentially reflect only changes in local blood volume. Fig. 4. Absorption coefficients of hemoglobin. Measurement is made optically with an infrared light source and a photo-sensitive detector which are attached to an appropriate part of the skin, normally to a finger. In the transmission method the detector is positioned opposite to the emitter, (Fig. 5) Fig. 5. Attachment of a finger probe. 337 Appendix III the pulsating arterial blood, see Fig. 6. The plethysmographic pulse wave is derived from the intensity of the transmitted light. The total absorption of the incident light can be divided into components, which are equivalent to compartments in the substance: tissue, venous and arterial blood and the pulse added volume of Note: The pulse waveform reflects changes in blood volume and movements of the blood vessel walls, not changes in blood pressure. Fig. 6. Absorption of infrared light in thefinger. 338 Monitored intravenous sedation with local anaesthesia for dental outpatients Appendicies 4 SHAPE AND COMPONENTS OF THE PULSE WAVE The amplitude of the pulse wave is the most informative indicator of changes in circulation of the vascular bed. Other parameters, for example crest time and the dicrotic notch can also be identified from the pulse wave, see Fig. 7. The dicrotic notch is caused by the closing of the aortic valve. Fig. 7. Analysis of the peripheral pulse wave. 339 Appendix III 5 TYPICAL VARIATIONS IN THE PULSE WAVE DURING ANAESTHESIA Fig. 8 shows how the plethysmographic pulse wave amplitude changes during general anaesthesia. The following different phases can be identified, see Fig. 8: Following intubation, the patient is prepared for surgery. There are no strong external stimuli in this quiet phase, thus maximum vasodilatation can be seen. 1. Preanaesthetic phase 5. Skin incision The patient is afraid of the operation and the anaesthesia despite premedication. Relative vasoconstriction and hence a small pulse amplitude are normal during this phase. Skin incision is very strong stimulus which appears as a significant decrease in pulse wave amplitude with or without other changes in monitored parameters (for example increasing blood pressure and heart rate). 2. Induction During the induction phase, the patient loses consciousness, and marked vasodilatation causing a significant increase in pulse wave amplitude can be seen. This is partially due to the direct vasodilatatory effect of different anaesthetics. 6. Maintenance phase In most patients, the pulse wave amplitude recovers to its previous level in a short period of time. During the maintenance period, the pulse wave reacts to different surgical stimuli with minor reflectory decreases in amplitude. During a prolonged operation, the pulse wave amplitude may progressively decrease. 3. Laryngoscopy and intubation Laryngoscopy and endotracheal intubation are strong stimuli which cause sudden vasoconstriction and a decrease in the pulse wave amplitude. 4. Surglcal preparation phase 340 Monitored intravenous sedation with local anaesthesia for dental outpatients Appendicies 7. End of anaesthesia 8. Recovery The patient begins to regain consciousness and is more sensitive to the various stimuli during this phase - resulting in vasoconstriction and a decrease in the pulse wave amplitude. During recovery from anaesthesia, the pulse wave amplitude is often relatively low because the patient experiences postoperative pain and other discomfort. Fig. 8. Typical plethysmographic pattern during anaesthesia. 341 Appendix III 6 CONCLUSIONS BASED ON CHANGES IN THE AMPLITUDE OF THE PULSE WAVE DURING ANAESTHESIA The following conclusions can be made from the plethysmogram during anaesthesia (Note: the patient is basically healthy and the operation proceeds without any major complications): amplitude indicates anaesthesia. too light 4. Surgical preparation phase No significant conclusions can usually be made. 1. Preanaesthetic phase If the patient has a low pulse wave amplitude before anaesthesia, it may be an indication that the patient is scared of the operation and the premedication has been insufficient. 5. Skin incision Skin incision is one of the strongest stimuli during an operation. The strong reaction can be avoided by a booster dose of intravenous or inhalation anaesthetics before incision. 2. Induction Strong vasodilatation is very typical during the induction phase. This is due to a redistribution of circulation at the beginning of anaesthesia. Possible disadvantages can be counteracted by active infusion therapy. 6. Maintenance phase If the pulse wave amplitude stays low during the operation, it is normally an indication of light anaesthesia. Frequent changes in amplitude also indicate light anaesthesia in the absence of other influencing factors. 3. Laryngoscopy and intubation The sudden reaction to laryngoscopy and intubation is common even to a deep anaesthesia. It is not necessarily a sign of an unacceptable induction, but is reflectory in nature and normally recovers quickly. A slow recovery of A progressive, continuous decrease in pulse wave amplitude is usually due to a blood volume deficit (hypovolemia), decrease of body temperature or hyperventilation. Changes in the pulse wave amplitude should always be considered together with other variables in order to 342 Monitored intravenous sedation with local anaesthesia for dental outpatients Appendicies diagnose the real cause of any changes. 8. Recovery In the recovery room, the pulse wave amplitude can be used as a guide to better patient care. Vasodilatation is normally associated with a good quality of recovery and patient welfare. 7. End of anaesthesia A normal reaction to the various stimuli during this phase is vasoconstriction. 343 Appendix III 7 DIFFERENTIAL DIAGNOSIS Table 2. Relation of changes in the pulse wave to other parameters in various situations. Clinical Situation Pulse wave BP HR EtCO2 Peripheral temperature SpO2 Hypovolemia - Too light anaesthesia - Too deep anaesthesia - Hyperventilation - Hypoventilation () - Hypoksia - Parameter indicates increase indicates decrease constant or no significant change 344 Monitored intravenous sedation with local anaesthesia for dental outpatients Appendicies Correct interpretation of changes in the plethysmographic wave can only be made by simultaneous comparison with changes in the clinical signs and other monitored parameters. sensitivity of the pulse wave and the ECG to different clinical disturbances. The following table indicates the relation of other commonly monitored parameters to changes in the pulse wave in different situations. • ECG is one of the most commonly monitored physiological parameters. Table 3 compares the Table 3. Relative sensitivity of pulse wave and ECG to various disturbances. ECG (shape) DISTURBANCE PLETHYSMOGRAPHIC PULSE WAVE (amplitude) + - - Hypovolemia + - Hypercarbia + - Hypocarbia + - Too light anaesthesia +++ - Too deep anaesthesia +++ + Arrhythmia +++ - Low cardiac output + +++ Cardiac arrest +++ + Primary myocardial ischemia - + Hypoxia + indicateschange indicates no change +++ ++ + - 345 immediate reaction fast reaction slow reaction no reaction Appendix III 8 THE PLETHYSMOGRAPHIC WAVE DISPLAYED BY DATEXENGSTROM MONITORS Datex-Engstrom pulse wave oximeters measure oxygen saturation from the absorption of incident light at two wavelengths. In addition, they display the plethysmographic waveform on the screen. The scale of the pulse wave indicates the amplitude factor, and can be changed manually. The pulse rate, derived from the pulse wave, is displayed as a numeric value. As an example, Datex-Engstrom Capnomac UltimaTM has an integral video display, which gives both high resolution waveform display and comprehensive trend display capabilities. Fig. 9. Datex-Engstrom Capnomac UltimaTM with plethysmographic pulse wave display. 346 Monitored intravenous sedation with local anaesthesia for dental outpatients Appendicies 9 BENEFITS OF THE PLETHYSMOGRAPHIC WAVEFORM The plethysmogram is a diagnostically relevant parameter to monitor: The pulse wave also shows other abnormalities in heart function, eg arrhythmias. By inspecting the peripheral pulse wave, we can make conclusions about the importance of occasional arrhythmias. The waveform amplitude is related to changes in blood volume at the monitoring site The shape of the pulse wave and its amplitude give valuable information about the condition of the peripheral vascular bed. The pulse wave indicates changes in local, peripheral blood circulation better than any other parameter. Consecutive pulse waves readily show rapid, beat-to-beat changes in circulation. The effect of breathing can also seen from the waveform baseline fluctuation Changes in the plethysmogram reflect the effects of premedication, sedation and depth of anaesthesia The displayed waveform is an actual basis of the oxygen saturation measurement (SpO2). Thus the user can always check that the SpO2 measurement is not compromised by motion or other artefacts. The amplitude of the pulse wave is sensitive to stimuli provoking vasoconstriction, eg fear, pain, cold, hypocapnia, etc 347 Appendix III 10 DETERMINATION OF THE PULSE WAVE During start up, the optimum display range for the pulse wave is automatically set, the gain is then fixed. The user can, however, change the gain manually during operation to account for large changes in amplitude. Thus relative changes in peripheral circulation are accurately reproduced in the displayed waveform. Fig. 10. Derivation plethysmographic wave. of intensity (increase in absorption) is recorded as an upward deflection in the plethysmogram, see Fig. 10. This variation can be expressed as a percentage, which we call the amplitude factor: I I Amplitudefactor = max- min X 100 % Imax The amplitude factor reflects blood volume changes and can thus indicate the strength of perfusion in the measuring site. The smaller the amplitude factor is, the smaller the blood volume change, and vice versa. the Despite the obvious similarity of the waveform to the arterial blood pressure waveform, the pulse wave is not analogous to the blood pressure. Naturally, the pulse wave amplitude varies from patient to patient. The actual pulse wave is displayed as a mirror image of the intensity waveform, so that a decrease in 348 Monitored intravenous sedation with local anaesthesia for dental outpatients Appendicies 11 TREND DISPLAY Fig. 11. Changes in plethysmographic pulse waveform amplitude and SpO2 during open heart surgery. The patient underwent repair of a ventricular septal defect. After successful emergence from cardiopulmonary bypass, impaired function of the left ventricle resulted in a decrease in cardiac output, dramatic decrease in SpO2 and plethysmographic pulse wave amplitude (1). SpO2 decreased to 40 % and the patient experienced a cardiac arrest (2). During the successful cardiopulmonary resuscitation, sodium nitroprusside infusion was started (3). SpO2 improved rapidly due to vasodilatation, release of left ventricular overload and improved function of the left ventricle. 349 Appendix III display a trend is to select the amplitude value which corresponds to maximum vasodilatation as a 100 % reference value, and compare changes in amplitude with this (Fig. 12). This kind of approach gives a tool to compare the trends of different patients during anaesthesia and analyze typical phases and similarities between patients. Hardcopy trending of the monitored parameters gives a permanent, continuous record. A serial data output gives the numeric information every 10 seconds. Information is easy to process further with a personal computer and commercial spreadsheet and graphic software packages. An informative way to Fig. 12. Relative pulse wave amplitude changes of a patient during propofol short anaesthesia. 350 Monitored intravenous sedation with local anaesthesia for dental outpatients Appendicies 12 SUMMARY The plethysmographic waveform, displayed by all Datex-Engstrom pulse wave oximeters, is a valuable addition to parameters monitored in modern anaesthesia. Together with other clinical signs and parameters, it supplements the clinical picture of the patient condition and thus helps improve patient care and anaesthesia. The pulse wave is a rapid and sensitive indicator of various disturbances during anaesthesia. The long-term trend information gives an overall view of the course of the anaesthesia and is a valuable tool for teaching and research purposes. 351 Monitored intravenous sedation with local anaesthesia for dental outpatients Appendicies 7.4 APPENDIX IV COMMUNICATION BETWEEN PC AND OXIMETER 353 Monitored intravenous sedation with local anaesthesia for dental outpatients Appendicies The following list is a Q-BASIC program which allows the communication transferring from the Ohmeda pulse oximeter to the personal computer. The four first rows form the start file and rest of the list is the program itself. This program do not only collect the data from the equipment but allows the operator add comments between the data. The program is done by Juha Luotio and he has granted permission for its free use; it is also available in disk when requested from the author’s address. @echo off echo. echo starting MedCom... qbasic /run MedCom.Bas LET c = 0 LET g = 10 LET p = 0 CLS SCREEN 2 LOCATE 10, 30: PRINT "Pulse Oximeter" LOCATE 11, 30: PRINT "Communication" LOCATE 12, 33: PRINT "Program" LOCATE 25, 65: PRINT "Version 1.0" SLEEP 5 SHELL "a:" SHELL "cd\" CONST ESC = 27 kys: LOCATE 10, 20: INPUT "Where is pulse oximeter? In COM 1 or 2 "; h nimi: LOCATE 11, 20: INPUT "Give a name of the file: ", g$ IF g$ = "" THEN LOCATE 13, 20: PRINT "Incorrect file name": GOTO nimi COLOR 15 CLS LOCATE 7, 20: PRINT "To start the program press any key." LOCATE 9, 20: PRINT "DURING THE PROGRAM:" LOCATE 11, 20: PRINT "To add comments into the collected data press F1." LOCATE 12, 20: PRINT "To continue collection press ENTER." LOCATE 13, 20: PRINT "To exit from the program press ESC." LOCATE 14, 20: PRINT "To clear the screen durin program press F2." SLEEP 30 IF h = 2 THEN GOTO com2 355 Appendix III CLS COM(1) ON OPEN "COM1:1200,S,7,1,ASC,OP0,LF,RB500" FOR INPUT AS #1 OPEN g$ FOR OUTPUT AS #2 ON COM(1) GOSUB ComHandel WHILE INKEY$ <> CHR$(ESC) WEND COM(1) OFF CLOSE #2 CLS LOCATE 10, 20: PRINT "SYSTEM OF COLLECTION. PRESS ANY KEY" LOCATE 11, 20: PRINT "AND EXIT THE ''MEDCOM.BAS'' USING ''FILE''." SYSTEM com2: CLS COM(2) ON OPEN "COM2:1200,S,7,1,ASC,OP0,LF,RB500" FOR INPUT AS #1 OPEN g$ FOR OUTPUT AS #2 ON COM(2) GOSUB ComHandel WHILE INKEY$ <> CHR$(ESC) WEND COM(2) OFF CLOSE #2 CLS LOCATE 10, 20: PRINT "SYSTEM OF COLLECTION. PRESS ANY KEY" LOCATE 11, 20: PRINT "AND EXIT THE ''MEDCOM.BAS'' USING ''FILE''." SYSTEM ComHandel: LOCATE 9, 5: PRINT "Comments: " LET c = c + 1 INPUT #1, tieto$ IF c = 1 THEN LET j$ = tieto$ IF c = 2 THEN LET b$ = tieto$ IF c = 3 THEN LET x$ = tieto$ IF c = 4 THEN LET z$ = tieto$ IF c = 5 THEN LET s$ = tieto$ LOCATE 7, 5: PRINT "DATE; "; DATE$; " TIME; "; TIME$; ";"; tieto$; " ** CONNECTION......." PRINT #2, "; DATE; "; DATE$; "; TIME; "; TIME$; ";"; tieto$ 356 Monitored intravenous sedation with local anaesthesia for dental outpatients Appendicies LOCATE 1, 5: PRINT j$ LOCATE 2, 5: PRINT b$ LOCATE 3, 5: PRINT x$ LOCATE 4, 5: PRINT z$ LOCATE 5, 5: PRINT s$ KEY(2) ON: ON KEY(2) GOSUB Tyhjen SLEEP 1: KEY(1) ON: ON KEY(1) GOSUB kommentti RETURN kommentti: LET p = p + 1 LET g = g + 1 IF g >= 25 THEN RETURN LOCATE 9, 5: INPUT "Comments: ", komm$ IF komm$ = "X" OR komm$ = "x" THEN LET komm$ = "Xylocain adr. 1.8 ml" IF komm$ = "C" OR komm$ = "c" THEN LET komm$ = "Citanest Oct. 1.8 ml" IF komm$ = "D" OR komm$ = "d" THEN LET komm$ = "Dormicum (1mg/ml) 1 ml" IF komm$ = "O" OR komm$ = "o" THEN LET komm$ = "Oxygen 3 l/min" IF komm$ = "T" OR komm$ = "t" THEN LET komm$ = "Toradol 1 ml" IF komm$ = "F" OR komm$ = "f" THEN LET komm$ = "Fentanyl 0.5 ml" LOCATE g, 5: PRINT "COMM"; p; "; TIME = "; TIME$; " COMM = "; komm$ PRINT #2, "COMM"; p; "; TIME = "; TIME$; " COMM = "; komm$ IF g = 24 THEN LOCATE 25, 5: PRINT "NO MORE COMMENTS. PRESS ''F2'' TO CLEAN THE SCREEN" COLOR 15 RETURN Tyhjen: CLS LET g = 10 RETURN 357 Appendix IV Following list is an example of a real monitored and documented treatment period: 21.10.1994 12:43 name os the patient removed extraktioita (extractions) 21.10.1994 12:48 kanyl kesäajassa vieläkin (still in summer time) 21.10.1994 12:48 1 ml Dormicum 1mg/ml 21.10.1994 12:49 1 ml Dormicum 1mg/ml 21.10.1994 12:49 1 ml Dormicum 1mg/ml 21.10.1994 12:49 1 ml Dormicum 1mg/ml 21.10.1994 12:50 1 ml Dormicum 1mg/ml 21.10.1994 12:51 1,8 ml Citanest Octapressin 30 mg/ml + 0,54 21.10.1994 12:51 1,8 ml Citanest Octapressin 30 mg/ml + 0,54 21.10.1994 12:52 1,8 ml Citanest Octapressin 30 mg/ml + 0,54 21.10.1994 12:52 1,8 ml Citanest Octapressin 30 mg/ml + 0,54 21.10.1994 12:53 1,8 ml Xylocain adrenalin 20 mg/ml + 12,5 mcg/ml 21.10.1994 12:54 1,8 ml Xylocain adrenalin 20 mg/ml + 12,5 mcg/ml 21.10.1994 12:55 1,8 ml Xylocain adrenalin 20 mg/ml + 12,5 mcg/ml 21.10.1994 12:58 1,8 ml Xylocain adrenalin 20 mg/ml + 12,5 mcg/ml 21.10.1994 12:59 ex.., 13:01 8 hammasta pois ja proteesit nyt suussa ( 8 extractions done and prosthesis in the mouth) 21.10.1994 13:03 lanexat lähtee.. (the begin of flumazenil) 21.10.1994 13:04 5 ml meni ( total dose 0.5 mg) 13:11 kylmät sormet vaihdan anturin paikkaa ( Cold fingers. Changing of the place of the probe) 21.10.1994 13:13 loppu ..kan.pois (The end. Cannula removed) . :SaO2=--- PR=--- ** PROBE OFF PATIENT :SaO2=--- PR=--- ** PROBE OFF PATIENT :SaO2=--- PR=--- ** PROBE OFF PATIENT :SaO2=--- PR=--- ** PROBE OFF PATIENT :SaO2=--- PR=--- ** PROBE OFF PATIENT :SaO2=--- PR=--- ** PROBE OFF PATIENT WHAT? :SaO2=--- PR=-WHAT? :SaO2=--- PR=--- ** PROBE OFF PATIENT :SaO2=--- PR=--- ** PROBE OFF PATIENT :SaO2=--- PR=--- ** PROBE OFF PATIENT 358 Monitored intravenous sedation with local anaesthesia for dental outpatients Appendicies :SaO2=--- PR=--- ** PROBE OFF PATIENT :SaO2=--- PR=--- ** PROBE OFF PATIENT :SaO2=--- PR=--- ** PROBE OFF PATIENT :SaO2=--- PR=--- ** PROBE OFF PATIENT :SaO2=--- PR=--- ** PROBE OFF PATIENT :SaO2= 93 PR= 72 :SaO2= 93 PR= 71 :SaO2= 95 PR= 68 :SaO2= 97 PR= 71 :SaO2= 97 PR= 70 :SaO2= 96 PR= 70 :SaO2= 96 PR= 68 :SaO2= 95 PR= 69 :SaO2= 95 PR= 74 :SaO2= 95 PR= 75 :SaO2= 95 PR= 74 :SaO2= 95 PR= 75 :SaO2= 95 PR= 76 :SaO2= 95 PR= 76 :SaO2= 96 PR= 78 :SaO2= 95 PR= 79 :SaO2= 95 PR= 78 :SaO2= 95 PR= 78 :SaO2= 96 PR= 78 :SaO2= 95 PR= 80 :SaO2= 95 PR= 77 :SaO2= 96 PR= 74 :SaO2= 96 PR= 73 :SaO2= 96 PR= 74 :SaO2= 96 PR= 74 :SaO2= 95 PR= 77 :SaO2= 95 PR= 82 :SaO2= 95 PR= 79 :SaO2= 97 PR= 79 :SaO2= 98 PR= 79 :SaO2= 97 PR= 80 :SaO2= 96 PR= 80 :SaO2= 96 PR= 81 :SaO2= 97 PR= 78 :SaO2= 96 PR= 79 :SaO2= 96 PR= 79 :SaO2= 95 PR= 79 :SaO2= 95 PR= 79 :SaO2= 95 PR= 78 :SaO2= 95 PR= 79 :SaO2= 95 PR= 82 :SaO2= 96 PR= 82 :SaO2= 96 PR= 81 OHMEDA BIOX 3740 PULSE OXIMETER TREND DATA OUTPUT 12 SECONDS PER DATA POINT :SaO2=--- PR=--:SaO2= 96 PR= 69 :SaO2= 97 PR= 70 :SaO2= 96 PR= 74 :SaO2= 96 PR= 72 :SaO2= 97 PR= 75 :SaO2= 97 PR= 75 :SaO2= 97 PR= 80 :SaO2= 98 PR= 76 :SaO2= 99 PR= 74 :SaO2= 99 PR= 65 :SaO2= 98 PR= 67 :SaO2= 96 PR= 72 :SaO2= 95 PR= 73 :SaO2= 96 PR= 63 :SaO2= 97 PR= 62 :SaO2= 97 PR= 61 :SaO2= 96 PR= 60 :SaO2= 95 PR= 60 :SaO2= 95 PR= 66 :SaO2= 95 PR= 65 :SaO2= 95 PR= 66 :SaO2= 95 PR= 67 :SaO2= 95 PR= 70 :SaO2= 96 PR= 66 :SaO2= 95 PR= 70 12:50 10/21/94 359 12:55 10/21/94 13:00 10/21/94 Appendix IV :SaO2= 97 PR= 80 :SaO2= 97 PR= 80 :SaO2= 96 PR= 79 :SaO2= 96 PR= 79 :SaO2= 96 PR= 79 :SaO2= 94 PR= 78 :SaO2= 94 PR= 79 :SaO2= 94 PR= 77 :SaO2= 95 PR= 75 :SaO2= 95 PR= 75 :SaO2= 95 PR= 71 :SaO2= 95 PR= 70 :SaO2= 95 PR= 68 :SaO2= 94 PR= 72 :SaO2= 94 PR= 77 :SaO2= 94 PR= 77 :SaO2= 97 PR= 77 :SaO2= 97 PR= 78 :SaO2= 96 PR= 77 :SaO2= 97 PR= 72 :SaO2= 97 PR= 73 :SaO2= 97 PR= 83 :SaO2= 96 PR= 80 :SaO2= 96 PR= 80 :SaO2= 96 PR= 81 :SaO2= 96 PR= 79 :SaO2= 96 PR= 79 :SaO2= 96 PR= 78 :SaO2= 96 PR= 74 :SaO2= 96 PR= 76 :SaO2= 96 PR= 75 :SaO2= 96 PR= 74 :SaO2= 96 PR= 75 :SaO2= 95 PR= 76 :SaO2= 95 PR= 77 :SaO2= 94 PR= 75 :SaO2= 94 PR= 75 :SaO2= 94 PR= 74 :SaO2= 93 PR= 76 :SaO2= 93 PR= 78 :SaO2= 94 PR= 75 :SaO2= 95 PR= 72 :SaO2= 96 PR= 73 :SaO2= 95 PR= 75 :SaO2= 94 PR= 75 :SaO2= 94 PR= 78 :SaO2= 94 PR= 76 :SaO2= 94 PR= 75 :SaO2= 93 PR= 77 13:10 10/21/94 :SaO2= 94 PR= 73 :SaO2= 95 PR= 73 :SaO2=--- PR=--- PO :SaO2=--- PR=--- PO :SaO2=--- PR=--- PO :SaO2=--- PR=--- PO :SaO2=--- PR=--- PO :SaO2=--- PR=--- PO :SaO2=--- PR=--- PO :SaO2=--- PR=--- PO :SaO2=--- PR=--- PO :SaO2=--- PR=--- PO :SaO2=--- PR=--- PO :SaO2=--- PR=--- PO :SaO2=--- PR=--- PO :SaO2=--- PR=--- PO :SaO2=--- PR=--- PO :SaO2=--- PR=--- PO :SaO2=--- PR=--- PO :SaO2=--- PR=--- PO :SaO2=--- PR=--- PO :SaO2=--- PR=--- PO :SaO2=--- PR=--- PO :SaO2=--- PR=--- PO :SaO2=--- PR=--- PO 13:15 10/21/94 :SaO2=--- PR=--- PO :SaO2=--- PR=--- PO :** POWER ON ** :SaO2= 99 PR=214 ** PROBE OFF PATIENT :SaO2=--- PR=--- 13:05 10/21/94 ** PROBE OFF PATIENT 360 Monitored intravenous sedation with local anaesthesia for dental outpatients Appendicies 7.5 APPENDIX V CRTICAL THOUGHTS 361 Monitored intravenous sedation with local anaesthesia for dental outpatients Appendicies A year after the completion of the manuscript: Critical thoughts from one side and the other real world: the world is far too complicated for that. The syntheses are valid only under special conditions, devoid of chaotic components. If we do not complete the examinations with careful descriptions of reality as it is, we will soon believe in our theories rather than reality. The Methods: experiments against observation The experimental method of examination which at present is almost the sole method used in e.g. medicine, is of fairly young origin, since Galileo Galilei was claimed to have made the first experiments in the natural sciences. Until then, observation and deduction were the only methods used, as - rightly interrupting nature’s events with an experiment would have altered reality. A case in point of this alteration is my second extensive study; the Osfix implant study (www.osfix.sci.fi) where the test group consisted of healthy edentulous adults with a nonresorbed mandible... Unfortunately, patients in the real world, or those in my dental practice, rarely fulfil the criteria. Nevertheless, the treatment has to be made. Personally, I think the study plan approved by the Ethical Board and the Medical Board distorts reality! Of course there remains a lot to be said about ancient and medieval observational philosophy, but rejecting clinical observation in the favour of an experimental method (basing the examination on exclusion and randomization) may be parallelled with emptying the baby out with the bathwater. The fact that observation seldom leads to a great synthesis is mainly due to the lack of counterpart for the synthesis in the This is why in my most important study I have wanted to observe my patients without test arrangements, i.e. to observe the treatment as such, and - as was noted in the study plan submitted to the faculty, the treatments had already been made and therefore there seemed to be no sense in applying for a permission from the Ethical Board. Thus there was no study plan when monitoring the patients, but there was an access to various monitors for observing the patient’s well-being, and the sedation accounts are based on the data stored on discs by these monitors, complemented with comments on medication in the data flow. This is not a question of making online information to be used in studies, but carefully following up sedation which is routine in my dental practice. Examining the stored-up information (the disc is part of the “patient information card”) retrospectively and making conclusions from the examinations - either combining similar treatment procedures or by 363 Appendix V statistical means with multi-analysis of variance, has created the science. index exist, could upcoming problems be predicted from this? A most intriguing facet concerning my method was the observation material in the work observing anesthesia made for medical students, as the experimental thinking (time schedule - division into groups) that has saturated the university also crept in my work although I had planned to remain an observer. In an afterthought; if I had known from the beginning what will happen, I would have either completed a plan with randomizations and applied for a permit from the Ethical Board, or made the work in my dental clinic on real patients which are solely given local anesthetics, not sedated. The local anesthetics given to dental students only seemed a perfect occasion to “have the job well done”. Later on in the Holter study I had gained knowledge: I made a dental student in the university operating theatre to ask the morning patient if he/she would carry an extra monitor for 24 hours. I thus prevented the ordinary staff from distorting the patient group. The same question was placed for all patients coming to my dental practice for a sedation, until the 23 registrations had been completed (incidentally, only one denied). I thus have two different groups, as they are, in my work. Of course no firm conclusions may be made from these kind of groups - only indicative ones. The purpose of my method is not to firmly prove anything - that I leave to others - but to bring up previously unknown issues; could it be thus, could such an 364 Monitored intravenous sedation with local anaesthesia for dental outpatients Appendicies mathematical system, which additionally affects our emotions, but the notion on what music should be like, is tied to time, place and social reference group. Also the assumption that there is so-called superior and inferior art reveals the social ties within art. Furthermore, art clearly contains an end in itself. Science, Art and Dentists In my outlook on life I define science (and inevitably also its cousin, art) as follows: -Science is a method whereby awareness obtains information on the outside reality. Humans are part of this concrete reality as biological creatures with a basic instinct to survive and reproduce. Our awareness is rising from this basis as an interdepencency through our social network. This network gives us a notion of ourselves, of others and of reality. This is, however, only a notion. It is not necessarily connected to reality, it is an agreement made by our social network. Yet science is undisputably an interdependency between awareness and reality, with an exterior goal. This goal is further clearly divided into two: to an attempt to understand reality, and to an attempt to informatively affect the reality, the latter being often referred to as engineering skills or, in case of medicine, clinical knowhow. The experimental method again has been one of the most brilliant means of getting clear of the disturbance caused by our collective consciousness and reach the first goal. But overemphasizing the experiment will lead into a massive problem: science is thus limited into a structure between experiment and awareness... If we agree on the above, I cannot resist making a couple of conclusions which will greatly irritate our awareness: 1.Scientific reports are works of art, since they are socially tied, selfpurposeful products comparable to a painting. The new, disease resistent grain is the product of scientific work, a report thereof is a work of art... 2.The branches of science that do not fall into the natural sciences, e.g.psychology, are pure art, as no reality exists as an object of their study. They bear no difference to committed art. The polarization of the professioninto unpractial experimentalists who have created their own, introvert academic culture, and into practical dentists, who have to zigzag through traditions, marketing and study results - has created a blind faith to the former being somewhat better representatives of science. They are not. Dentistry is part of the medical sciences and this reveals on which grounds the treatment should be based. Treatment is no less scientific than making experiments. It is a question of difference in outlook on -Art again is the processing of awareness, emotions and the above mentioned social agreement both in individual and collective consciousnesses; music is a logical, 365 Appendix V life: even an university researcher may believe and create sheer nonsense in his everyday life. The scientific outlook on life is no more anchored into researchers than to practical doctors. Both are equally a part of the scientific world, or they are not. The book in your hand attempts, however, to be a friendly gesture from practice towards academic culture. I broke the pattern into pieces small enough for the clinicist to read one at a time. This is why the book contains so much repetition, but then again if you have read the item “Patients and methods” in Part 1, there is no need to read them again in the sections thereafter. My aim has been to repeat the most essential points at least three times, as repetition still is the path to learning. Furthermore, the book can be read in three ways: 1) browsing bold prints, abstracts and clinical conclusions; 2) reading only the parts interesting for the reader, e.g. the patients’ experiences; 3) thoroughly going into the whole works. Thus I have considered the practical needs of a professional, yet aimed at waking an initial interest, then further introducing to them the interesting issues, and finally starting a process that leads to learning. This form has aroused an enormous opposition in the pre-examiners - hardly any criticism has been expressed on the subject itself - and, surprisingly enough, a year after the manuscript was completed, I came across a book (Dryden and Vos 1994) in which I could read that in my form-opposing attitude I might still be right. The readability of this book This book would probably be more readable for those living in academic culture, if it would obey the conventional dissertation pattern, but I have intently wanted to break that pattern (where form sometimes replaces contents), as I am writing of my observations to a dentist who is making clinical work. The possibilities of a clinicist to allocate his time are absolutely such that I know not of any clinicist colleague who would have read even one dissertation from cover to cover! The reason is not in the “ignorance” of the clinicists, but the fact that most dissertations make you wonder if anyone, save the pre-examiners and the opponent, ever read them. What an effort, and usually a waste of time. This issue cannot be justified by the traditional outline of a monography. 366 Monitored intravenous sedation with local anaesthesia for dental outpatients Appendicies The academic world seems at first sight most respectable, but a closer examination will reveal it pompous, authoritarian, domineering and offensive. 367 Monitored intravenous sedation with local anaesthesia for dental outpatients Appendicies REFERENCES Acosta F, Diaz J, Moreno J, Fuente T, Contreras RF, Sansano T, Bueno FS, Robles R, Ramirez P, Parrilla P 1995 Relationship between beta-endorphin release and surgical stress in orthotopic liver transplantation. Transplant Proc 27: 2303 Bachmann B, Biscoping J, Adams HA, Sokolovski A, Ratthey K, Hempelmann G 1988 Plasma concentrations of lidocaine and prilocaine following infiltration anesthesia in otorhinolaryngologic surgery. Laryngol Rhinol Otol Stuttg 67:335-339 Baka-een GS, Al Shanableh JS, Armouti AN, Abdel-Hadi OF 1987 Intravenous sedation in dental surgery. Middle-East J Anesthesiol 9: 193-197 Barker I, Butchart DG, Gibson J, Lawson JI, Mackenzie N 1986 I.v. sedation for conservative dentistry. A comparison of midazolam and diazepam.Br J Anaesth Apr, 58 (4) 371-377 Baxendale BR, Vater M, Lavery KM 1993 Dexamethasone reduces pain and swelling following extraction of third molar teeth. Anesthesia 48: 961-964 Berg JC, Miller R, Burkholter E 1991, Clinical value of pulse oximetry during routine diagnostic and therapeutic endoscopic procedures, Endoscopy 23: 328-330 Berge TI, Boe OE 1994 Predictor evaluation of postoperative morbidity after surgical removal of mandibular third molars. Acta Odontol Scand 52: 162-169 Berge TI, Gilhuus Moe OT 1993 Per and post operative variables of mandibular third molar surgery by four general practitioners and one oral surgeon. Acta Odontol Scand 51: 389-397 Berggren U 1984 Dental Fear and Avoidance: A study of etiology, consequences and treatment. Dissertation 1984 Bernstein DA. Anxiety management. In: Graighead WE, Kazdin AE, Mahoney MJ. Behavior modification. Principles, issues and applications. Hougren Miffin Co 1976. van-der Bijl P, Roelofse JA, Joubert JJ, van Zyl JF 1991 Comparison of various physiologic and psychomotor parameters in patients sedated with intravenous lorazepam, diazepam, or midazolam during oral surgery. J Oral Maxillofac Surg 49 672-678 369 References Billman GE, Schwartz PJ, Gagnol JP, Stone HL 1985 The cardiac response to submaximal exercise in dogs susceptible to sudden cardiac death. J Appl Physiol 59:890-897 Bilotta JJ, Floyd JL, Waye JD 1990 Arterial oxygen desaturation during ambulatory colonoscopy: predictability, incidence, and clinical insignificance. Gastrointest Endosc 36 (3 Suppl): 5-8 Bland JM and Altman DG 1995 Calculating correlation coefficients with repeated observations: Part 1-correlation within subjecst. BMJ 310:446 Bonazzi M, Riva A, Marsicano M, Prampolini F, Speranza R, Andriolli A, Laveneziana D 1994 (Trazodone versus flunitrazepam in premedication in day care surgery). Minerva Anestesiol 60: 115-121 Bouvy-Berends EC, Makkes PC 1990 (Anesthesiological support for special dental care). Anesthesiologie in de Bijzondere tandheelkunde. Ned Tijdschr Tandheelkd 97: 490-493 Breier T 1992 (Anxiolysis vs. intravenous conscious sedation during maxillary fracture splinting in local anaesthesia). Anxiolyse versus Analgosedierung bei der Kieferbruchschienung in Lokalanasthesie. Dtsch Zahnarztl Z 47: 50-53 Cantin RY, Poole A, Ryan JF 1986 Malignant hyperthermia. Oral Surg Oral Med Oral Pathol 62: 389-392 Casteel HB, Fiedorek SC, Kiel EA 1990 Arterial blood oxygen desaturation in infants and children during upper gastrointestinal endoscopy. Gastrointest Endosc 36: 0016-5107. Castillo J, Bogdanovich A, Valero R, Nalda MA 1990 Efecto de la premedicacion anestesica intravenosa con diacepam y fentanil sobre la saturacion arterial de oxigeno. Estudio pulsioximetrico. (Effect of intravenous anesthetic premedication using diazepam and fentanyl on the arterial oxygen saturation. A pulse oximetric study). Rev Esp Anestesiol Reanim 37: 142-145 Charlton D, Herbeau C, Renouard F 1991 (Ambulatory vigil anaesthesia for implant surgery). Interet de l'anesthesie vigile ambulatoire en chirurgie implantaire. J Parodontol 10: 235-237 Cioffi GA, Chernow B, Glahn RP, Terezhalmy GT, Lake CR 1985 The hemodynamic and plasma catecholamine responses to routine restorative dental care. JADA 111:67-70 370 Monitored intravenous sedation with local anaesthesia for dental outpatients Appendicies Clark MS, Lindenmuth JE, Jafek BW, Fryer GE Jr, Goldberg JR 1991 Reversal of central benzodiazepine effects by intravenous flumazenil. Anesth Prog 38: 12-16 Clark MS, Silverstone LM, Coke JM, Hicks J 1987 Midazolam, diazepam, and placebo as intravenous sedatives for dental surgery. Oral Surg Oral Med Oral Pathol 63: 127-131 Clark RN, Rodrigo MR 1986 A comparative study of intravenous diazepam and midazolam for oral surgery. J Oral Maxillofac Surg 44: 860-863 Cooper SA, Quinn PD, MacAfee K, McKenna D 1991 Reversing intravenous sedation with flumazenil. Oral Surg Oral Med Oral Pathol 72: 2-9 Coulthard P, Rood JP 1992 An investigation of the effect of midazolam on the pain experience. Br J Oral Maxillofac Surg 30: 248-251 Daublander M, Roth W, Lipp M 1992 Effects of different lidocaine sprays for topical anesthesia on cardiovascular parameters and oxygen saturation. Anesth Pain Control Dent 1:161-166 Davenport RE, Porcelli RJ, Iacono VJ, Bonura CF, Mallis GI, Baer PN 1990 Effects of anesthetics containing epinephrine on catecholamine levels during periodontal surgery. J Periodontal 61: 553-8 Davies CA, Sealey CM, Lawson JI, Grant IS 1990 Reversal of midazolam sedation with flumazenil following conservative dentistry. J Dent 18: 113-118 Dionne RA, Snyder J, Hargreaves KM 1994 Analgesic efficacy of flurbiprofen in comparison with acetaminophen, acetaminophen plus codeine, and placebo after impacted third molar removal. J Oral Maxillofac Surg 52: 919-24 Dolan EA, Murray WJ, Immediata AR, Gleason N 1988 Comparison of nalbuphine and fentanyl in combination with diazepam for outpatient oral surgery. J Oral Maxillofac Surg 46: 471-473 Dolci G, Ripari M, Pacifici L, Umile A 1993 (Analgesic efficacy and the tolerance for piroxicam beta cyclodextrin compared to piroxicam, paracetamol and placebo in the treatment of postextraction dental pain). Minerva Stomatol 42: 235241 Dryden G and Vos J 1994 Oppimisen vallankumous. WSOY 1997 (The Learning Revolution, Jalmar Press, California) Dundee JW 1990 Fantasies during sedation with intravenous midazolam or diazepam. Med Leg J 58: 29-34 371 References Eastwood DW 1992 Digital nerve blocks and pulse oximeter signal detection (letter). Anesth Analg 74:931 Edelman RJ, Mark J, Watts FN, Williams G 1992 Anxiety, Theory, Research and Intervention in Clinical and Health Psychology. In: Willey Series in Clinical Psychology 207-229 Edmunds DH Rosen M 1989 Management of anxiety in dental practice in the UK. Br Dent J 166: 253-255 Farrel TG, Odemuyiwa O, Bashir Y, Cripps TR, Malik M, Ward DE, Camm AJ 1992 Prognostic value of baroreflex sensitivity testing after acute myocardial infarction. Br Heart J 67:129-137 Faucett J, Gordon N, Levine J 1994 Differences in postoperative pain severity among four ethnic groups. J Pain Symptom Manage 9: 383-389 File SE, Pellow S, Skelly AM, Nelson IA. 1986 Amnesic and anxiolytic effects of intravenous diazepam in dental anxiety. Int Clin Psychopharmacol 1: 66-73 Fiset L, Milgrom P, Weinstein P, Getz T, Glassman P 1985 Psychophysiological responses to dental injections. JADA 111:578-583 Frabetti L, Checchi L, Finelli K 1992 Cardiovascular effects of local anesthesia with epinephrine in periodontal treatment. Quintessence Int 23:19-24 Franccoise M, Gouyon JB, Mercier JC 1996 Hemodynamics and oxygenation changes induced by the discontinuation of low dose inhalational nitric oxide in newborn infants. Intensive Care Med 22:477 -481 Gallon P, Walton GM, Rood JP 1992 Cardiopulmonary performance following changes in position and the administration of intravenous Diazemuls. J Dent 20: 211-214 Ghoneim MM, Dembo JB, Block RI 1989 Time course of antagonism of sedative and amnesic effects of diazepam by flumazenil. Anaesthesiology 70: 899904 Gortzak RATh, Abraham Inpijn L, Peters G 1992a Non invasive 27-hour blood pressure registration including dental checkups in some dental practices. Clin Prev Dent 14: 5-10 372 Monitored intravenous sedation with local anaesthesia for dental outpatients Appendicies Gortzak RATh, Oosting J, Abraham-Inpijn L 1992b Blood pressure response to routine restorative dental treatment with and without local anesthesia. Oral Surg Oral Med Oral Pathol 73: 677-681 Hardeman JH, Sabol SR 1990 Goldwasser MS. Incidence of hypoxaemia in the postanesthetic recovery room in patients having undergone intravenous sedation for outpatient oral surgery (see comments). J Oral Maxillofac Surg 48: 942-944 Heinze J, Rohrbach M 1992 Pramedikation bei Retrobulbaranasthesie. Ein blutgasanalytischer Vergleich von Flunitrazepam sublingual und Midazolam intravenos. (Premedication in retrobulbar anesthesia. A blood gas analysis comparison of sublingual flunitrazepam and intravenous midazolam). Anaesthetist 41: 673-679 Hempenstall PD, Campbell JP 1986 Bajurnow AT, Reade PC, McGrath B, Harrison LC. 1986 Cardiovascular, biochemical, and hormonal responses to intravenous sedation with local analgesia versus general anaesthesia in patients undergoing oral surgery. J Oral Maxillofac Surg 44: 441-446 Himuro H, Imai F, Satoh K, Aono K 1989 Arrhythmia during extraction of the third molars under intravenous sedation. A case report of postoperative tetralogy of Fallot. Fukuoka Shika Daigaku Gakkai Zasshi 16: 495-500 Hinzmann CA, Budden PM, Olson J 1992 Intravenous conscious sedation use in endoscopy: does monitoring of oxygen saturation influence timing of nursing interventions? Gastroenterol Nurs 15: 6-13 Hirota Y, Hori T, Kai K, Matsuura H 1992 Effects of epinephrine and norepinephrine contained in 2% lidocaine on hemodynamics of the carotid and cerebral circulation in older and younger adults. Anesth Pain Control Dent 1:143151 Hirsch JA, Bishop B 1981 Respiratory sinus arrhythmia in humans: how breathing pattern modulates heart rate. Am J Physiol 241:1620-1629 Hook PC, Lavery KM 1988 New intravenous sedative combinations in oral surgery: a comparative study of nalbuphine or pentazocine with midazolam. Br J Oral Maxillofac Surg 26: 95-106 Hosie HE, Brook IM, Nimmo WS 1988 Comparison of sedation with temazepam by mouth and diazemuls i.v. for dental surgery. Variability in absorption may influence clinical effect. Br J Anaesth 60: 18-23 Hupp JR, Becker LE 1988 Intensity and duration of amnesia from intravenous midazolam given for sedation. J Conn State Dent Assoc 62: 80-85 373 References Jann MW, Fidone G, Gorday M, Rostedt RR 1987 Butorphanol as a dental premedication in the mentally retarded. Oral Surg Oral Med Oral Pathol 63: 403407 Johnstone M 1976 Adult preoperative medication. Anaesthesia rounds N:o 10, (monograph) Kamath MV, Fallen EL 1993 Power spectral analysis of HRV: a non.invasive signature of cardiac autonomic functions. Crit Rev Biomed Eng 21: 245-311 Kaufman E, Heling I, Rotstein I, Friedman S, Sion A, Moz C, Stabholtz A 1994 Intraligamentary injection of slow release methylprednisolone for the prevention of pain after endodontic treatment. Oral Surg Oral Med Oral Pathol 77: 651-654 Keckeis A, Hofmockel R 1994 (Mixtures of different local anesthetics for subaxillary plexus anesthesia). Anaesthesiol Reanim 19: 32-36 Keeffe EB, O-Connor KW 1990 1989 A/S/G/E survey of endoscopic sedation and monitoring practices. Gastrointest Endosc 36: 13-18 Kent G 1984 Anxiety, pain and type of dental procedure. Behav Res Ther 22: 465-469 Kent G 1985 Memory of dental pain. Pain 21: 187-194 Kingon AM 1990 Intravenous sedation and patient response to minor oral surgery experience of 408 cases. Dent Update 17: 340-343 Kitney RI, Rompelman O 1977 Analysis of the human blood pressure and thermal control systems 1977 In Perkins J (ed) Biomedical Computing. Pitman Medical 49-50 Kleiger RE, Miller JP, Bigger JT Jr, Moss AJ and The Multicenter Post Infarction Researc Group 1987 Heart rate variability: a predictor of mortality following acute myocardial infarction. Am J Cardiol 59: 256-262 Kleinhauz M, Eli I 1993 When pharmacologic anesthesia is precluded: The value of hypnosis as a sole anesthetic agent in dentistry. Special Care in dentistry 13: 15 Knoll-Kohler E, Frie A, Becker J, Ohlendorf D 1989 Changes in plasma epinephrine concentration after dental infiltration anesthesia with different doses of epinephrine J Dent Res 68: 1098-1101 Krochak M, Rubin JG 1992 An overview of the treatment of anxious and phobic dental patients. Compend Contin Educ Dent 14: 604-614. 374 Monitored intravenous sedation with local anaesthesia for dental outpatients Appendicies Laskin DM 1984 Diagnosis and treatment of complications associated with local anesthesia. Int Dent J 34: 232-237 Lefevre B 1991 Local anaesthesia with intravenous analgesia as an alternative to general anaesthesia for medically compromised patients undergoing oral surgery. A retrospective study of sixty-two cases. SAAD Dig 8: 12-18 Lemasney NJ, Holland T, Mullane DO, O'Sullivan UR 1989 The etiology and treatment of needle phobia in the young patient- a review. J JR Dent Assoc 35: 2023 Lind LJ, Mushlin PS, Schnitman PA 1990 Monitored anaesthesia care for dental implant surgery: analysis of effectiveness and complications. J Oral Implantol 16: 106-113 Lowe T, Brook IM 1991 Oxygen saturation during third molar removal with local anaesthetic alone and in combination with intravenous sedation. Br Dent J 171: 210-211 Lundgren S 1988 Intravenous or rectal administration of sedatives in outpatient oral surgery. Acta Anaesthesiol Scand Suppl 88: 24-26 Luotio K, Mattila MAK, Kotilainen RM 1993 Introduction of a new patient monitoring system during dental procedures: Pulse oximetry. Oral Surg Diagn 4: 29-33 Luotio K, Ryhänen JM, Kotilainen R, Vainio M 1996 Cardiovascular effects of lidocaine and prilocaine used separately and in combination. 74.th general session and exhibition of the international association for dental research (IADR) March 1317, San Francisco, CA, USA Luotio K, Ryhänen JM, Kotilainen R, Hyppönen T 1997 Soft tissue anaesthesia with lidocaine, prilocaine and their combination. 74.th general session and exhibition of the international association for dental research (IADR), San Francisco, CA, USA Luyk NH, Zacharias M, Wanwimolaruk S 1992 Bolus dose with continuous infusion of midazolam as sedation for outpatient surgery. Int J Oral Maxillofac Surg 21: 172-175 Malliani A, Pagani M, Lombardi F et al. 1991 Cardiovascular neural regulation explored in the frequency domain. Circulation: Research Advaced Series 84: 482492 375 References Marsch SCU, Skarvan K, Schaefer HG, Paganoni R, Castelli I and Scheidegger D 1994 Prolonged decrease in heart rate variability after elective hip artroplasty. Brit J Anaesth 72: 643-649 Matthews RW, Malkawi Z, Griffiths M J, Scully C 1992 Pulse oximetry during minor oral surgery with and without intravenous sedation. Oral Surg Oral Med Oral Pathol 74: 537-543 Mattila MAK, Koski EM, Lukin S 1990 The effect of postoperative pain on pulse wave amplitudes. 8th European Congress of Anaesthesiology, Warsaw September 9-15, Abstr. 4/5.1-2. Mattila MAK, Kurki T, Malinen S 1989 Interpreting the plethysmographic pulse wave. Appliguide, Datex Mattila MAK 1990 Pulse wave oximetry and capnography in monitoring depth of anaesthesia. in book, Memory and Awareness in Ana- esthesia, ed. Bonke B, Fitch W, Millar K. Swewts & Zeitlinger, Amsterdam/Lisse 350-352. McKee CC, Ragland JJ, Myers JO 1991 An evaluation of multiple clinical variables for hypoxia during colonoscopy. Surg Gynecol Obstet 173: 37-40 Meyer FU 1987 Haemodynamic changes under emotional stress following a minor surgical procedure under local anesthesia. Int J Oral Maxillofac Surg 16: 688694 Meyer FU 1990 Influence of emotional stress and vasoconstrictor agents on heart rate and blood pressure. Dtsch Zahnarztl Z 46: 832-834 Mihm FG, Halperin BD 1985 Non-invasive detection of profound arterial desaturation using a pulse oximetry device. Anaesthesiology 62: 85 -87 Milam SB, Bennett CR 1987 Physostigmine reversal of drug-induced paradoxical excitement. Int J Oral Maxillofac Surg 16: 190-193 Miller RI, Bullard DE, Patrissi GA 1989 Duration of amnesia associated with midazolam/fentanyl intravenous sedation. J Oral Maxillofac Surg 47: 155-158 Milgrom P and Weinstein P 1993 Dental fears in general practice: New guidelines for assessment and treatment. Int Dent J 43: 288-293 Montebugnoli L, Pelliccioni GA, Borghi C 1990 Effects of vasoconstrictors during local anesthesia. Dent Cadmos 58: 62-71 376 Monitored intravenous sedation with local anaesthesia for dental outpatients Appendicies Nishida T, Taniguchi A, Tanigami H, Hagihira S, Yoshiya I 1996 (Anesthetic management of a patient complicated with restrictive cardiomyopathy for gastrectomy). Masui 45: 1265-1268 Noshima S, Morita N, Kobayashi Y, Hayashi D, Okamura K, Takahashi T, Kobayashi T, Enoki T, Esato K 1997 Surgical stress and the development of complications in relation to polymorphonuclear leukocyte elastase (PMNE) levels. Surg Today 27: 135-139 O Boyle CA, Barry H, Fox E, McCreary C, Bewley A 1988 Controlled comparison of a new sublingual lormetazepam formulation and i.v. diazepam in outpatient minor oral surgery. Br J Anaesth 60: 419-425 Osborne GA, Rudkin GE, Jarvis DA, Young IG, Barlow J, Leppard PI 1994 Intra operative patient controlled sedation and patient attitude to control. A crossover comparison of patient preference for patient controlled propofol and propofol by continuous infusion. Anesthesia 49: 287-292 Pagani M, Lombardi F, Guzzetti S, et al. 1986 Power spectral analysis of a beatto-beat heart rate and blood pressure variability as a possible marker of sympathovagal interaction in man and conscious dog. Circ Res 159: 178-193 Pan PH, Gravenstein N 1994 Intraoperative pulse oximetry: frequency and distribution of discrepant data. J Clin Anesth 6: 491-495 Pateromichelakis S 1992 Circulatory and respiratory effects of lidocaine administered into the rat maxillofacial circulation. J Oral Maxillofac Surg 50: 724727 Pietri S, Seguin JR, d Arbigny PD, Culcasi M 1994 Ascorbyl free radical: a noninvasive marker of oxidative stress in human open-heart surgery. Free Radic Biol Med 16: 523-528 Poon KS, Chang WK, Chen YC, Chan KH, Lee TY 1995 Evaluation of stress response to surgery under general anesthesia combined with spinal analgesia. Acta Anaesthesiol Sin 33: 85-90 Read Ward G 1990 Intravenous sedation in general dental practice--why oximetry? (see comments). Br Dent J 1990 5: 168, 9: 368-369 Comment in: Br Dent J 169:6. Reed MJ, Requa Clark B, Shultz RE 1989 Undergraduate education in the use of intravenous conscious sedation for dentistry. J Dent Educ 53: 273-276 377 References Rodrigo CR, Rosenquist JB, Cheng CH. 1990 Cardiac dysrhythmias with midazolam sedation. Anesth-Prog Jan-Feb, 37: 20-23 Rodrigo MR, Clark RN 1986 A study of intravenous sedation with diazepam and midazolam for dentistry in Hong Kong Chinese. Anaesth-Intensive-Care Nov, 14: 404-411 Rodrigo MR, Rosenquist JB 1988 Effect of conscious sedation with midazolam on oxygen saturation. J Oral Maxillofac Surg Sep, 46: 746-750 Rosenbaum NL, Hooper PA 1988 The use of flumazenil as an antagonist to midazolam in intravenous sedation for dental procedures. Eur J Anaesthesiol Suppl 2: 183-190 Sakurada S, Shido O, Yamamoto K, Sugimoto N, Kobayashi T, Nagasaka T 1995 Effect of digital nerve blockade on heat-induced vasoconstriction in the human finger. J Appl Physiol 78: 746-749 Salonen M, Forssell H, Schenin M 1988 Local dental anesthesia with lidocaine and adrenaline. Effects on plasma catecholamines, heart rate and blood pressure. Int J Oral Maxillofac Surg 17: 392-414 Saumet JL, Leftheriotis G, Dittmar A, Delhomme G, Degoute CS 1986 Skin blood flow changes in anaesthetized humans: comparison between skin thermal clearance and finger pulse amplitude measurement. Eur J Appl Physiol 54: 574-577 Schachter S, Singer J 1962 Cognitive, social and psycological determinants of emotional state. Psychol Rev 69: 379-399 Schwartz PJ, Billman GE, Stone HL 1984 Autonomic mechanisms in ventricular fibrillation induced by myocardial ischemia during exercise in dogs with a healed myocardial infarction: An experimental preparation for sudden cardiac death. Circulation 69: 780-790 Shepherd SR, Sims TN, Johnson BW, Hershman JM 1988 Assessment of stress during periodontal surgery with intravenous sedation and with local anaesthesia only. J Periodontol 59: 147-154 Van Sickels JE, Tiner BD 1992 Cost of a genioplasty under deep intravenous sedation in a private office versus general anesthesia in an outpatient surgical center.J Oral Maxillofac Surg 50: 687-690 Simcock P R, Raymond G L, Lavin M J, Whitley C L 1994 Combined peribulbar injection and blunt cannula infiltration for vitreoretinal surgery. Ophthalmic Surg 25: 232-235 378 Monitored intravenous sedation with local anaesthesia for dental outpatients Appendicies Skelly AM, Girdler NM, File SE 1992 The use of temazepam elixir in surgical dental sedation: a comparison with intravenous midazolam. Br Dent J 172: 153-157 Slater JP, Goldstein DJ, Ashton RC Jr, Levin HR, Spotnitz HM, Oz MC 1995 Right to left veno arterial shunting for right sided circulatory failure. Ann Thorac Surg 60: 978-985 Sugiyama A, Kaneko Y, Ichinohe T, Koyama T, Sakurai S, Nakakuki T 1991 Usefulness of the pulse oximeter as a respiratory monitor during intravenous sedation. Bull Tokyo Dent Coll Feb, 32: 19-26 Tay DH, Omar S, Low TC 1991 Is sedation without desaturation possible? Singapore Med J 32: 329-231 Taylor E, Ghouri AF, White PF 1992 Midazolam in combination with propofol for sedation during local anesthesia. J Clin Anesth 4: 213-216 Temper KK and Barker SJ 1986 Pulse oximetry and oxygen transport. In: Pulse Oximetry ed. Payne JP and Severinhouse JW. Springer-Verlag Berlin Heidelberg Thomson PJ, Coulthard P, Snowdon AT, Mitchell K 1993 Recovery from intravenous sedation with midazolam the value of flumazenil. Br J Oral Maxillofac Surg 31: 101-103 Tremper KK, Hufstedler S, Zaccari J, Schaefer R, Asrani R, Sangh M, Roohk V, LaMendola R 1985 Pulse oximetry and transeutaneous PO2 during hemorrhagic and normotensive shock in dogs. Anaesthesiology 61: AI63 Tsirlis A and Iakovidis D 1989 Arterial pressure variation following an intravenous and submucous injection of local anesthetic solutions with vasoconstrictor. Odontostomatol Proodas 43: 347-356 Tsuji H, Venditti FJ Jr, Manders ES, Evans JC, Larson MG, Feldman CL, Levy D 1994 Reduced heart rate variability and mortality in elderly cohort. The Framingham Heart Study. Circulation 90: 878-883 Tucker MR, Ochs MW, White RP-Jr. 1986 Arterial blood gas levels after midazolam or diazepam administered with or without fentanyl as an intravenous sedative for outpatient surgical procedures. J Oral Maxillofac Surg Sep, 44: 688-692 Tuutti H 1986 Hammashoitopelko lapsilla ja nuorilla. Dissertation, University of Kuopio, Finland 379 References Töyry JP, Niskanen LK, Mäntysaari MJ, Länsimies EA, Uusitupa MIJ 1996 Occurrence, predictors, and Clinical Significance of autonomic neuropathy in NIDDM. Diabetes 45: 308-315 Vassend O 1993 Anxiety, pain and discomfort associated with dental treatment. Behav Res Ther 31: 659-666. Veit S, Muser HG, Bottcher E, Bruckner JB 1993 Signs of a severe myocardial ischemia following peritonsillar infiltration with ornipressin. Anesthesist 42: 320323 Visco DM, Tolpin E, Straughn JC, Fagraeus L 1989 Arterial oxygen saturation in sedated patients undergoing gastrointestinal endoscopy and a review of pulse oximetry O Del Med J 61: 533-542 Walton GM, Rood JP, Snowdon AT, Rickwood D 1993 Ketorolac and diclofenac for postoperative pain relief following oral surgery. Br J Oral Maxillofac Surg 31: 158-160 White CS, Dolwick MF, Gravenstein N, Paulus DA 1989 Incidence of oxygen desaturation during oral surgery outpatient procedures. J Oral Maxillofac Surg 47: 147-149Wilson S 1990 Conscious sedation and pulse oximetry: false alarms? Pediatr Dent 12: 228-232 Wilson, Braunwald 1991 Isselbacher et al. (ed). Harrison's Prinsiples of Internal Medicine, Mc Graw Hill: 1021-1023 Yelderman M, New W 1983 Evaluation of pulse oximetry. Anaesthesiology 59: 349-352 Zacharias M, Luyk NH, Parkinson RT 1992 Oxygen saturation during intravenous sedation using midazolam. N Z Dent J 88: 94-96 Zacharias M, Thyne GM, Luyk NH 1993 Local anesthesia during surgery: when is the best time to give it? Anesth Pain Control Dent 2: 9-12 Zoller B, Zoller J. 1992 (The use of different conscious sedation procedures in ambulatory dental surgery). Einsatz verschiedener Analgosedierungsverfahren in der ambulanten zahnarztlichen Chirurgie. Dtsch Zahn Mund Kieferheilkd Zentralbl, 80: 97-100 380