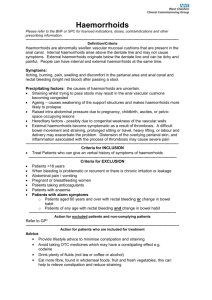
HAEMORRHOIDS (PILES) DURING & AFTER PREGNANCY
advertisement
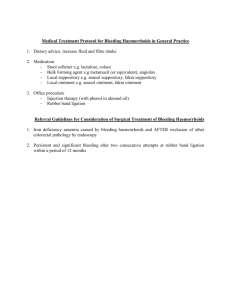
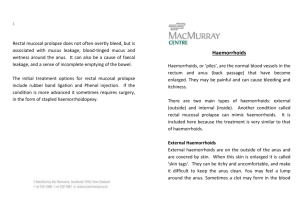
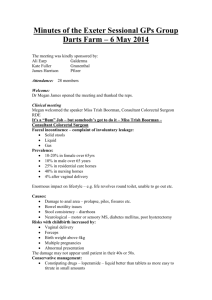
HAEMORRHOIDS (PILES) DURING & AFTER PREGNANCY Few people talk about one of the most common problems experienced during pregnancy – haemorrhoids. Also known as piles, haemorrhoids are thought to affect more than half of people in the Westernised world, and large percentage of pregnant women. Determining how many people are affected is not always easy, because haemorrhoids are one of those subjects people prefer to keep to themselves. While haemorrhoids are more irritating than dangerous, it is important to have a doctor confirm that any symptoms you have (such as rectal bleeding) are indeed caused by haemorrhoids, and not by a more serious condition. The most likely to develop haemorrhoids include Westernised people who eat a lowfibre diet, the elderly, pregnant women, those chronically straining with constipation, people with heavy lifting jobs and those who are overweight. What are Haemorrhoids? Haemorrhoids (piles) are swollen, congested and enlarged (but normally present) blood vessels in and around the anus and lower rectum that stretch under pressure. Veins inside or around the opening of the anus (back passage). They can be described as “varicose veins” of the rectum. These blood vessels lie just below the surface of the anus lining, and may cause pain, irritation and itching and may even bleed slightly. The blood from haemorrhoids is bright red in colour, and may show up on the stool or toilet paper after a bowel movement. Sometimes, haemorrhoids develop ulcers/sores and produce mucous which may be seen on toilet paper. Sufferers may feel as if they have a lump or bump hanging down from the anus. Haemorrhoids can occur just inside the rectum (internal haemorrhoids), making them undetectable to you, they may prolapse or protrude outside the rectum (protruding haemorrhoid), or may appear as a lump under the skin in the area of the rectum (external haemorrhoids). Haemorrhoids that protrude through the anus may cause continual discomfort and difficulty in cleaning the area. Excessive straining, itching or rubbing around the anus can cause bleeding and irritation in the affected area. Haemorrhoids can make proper cleaning of the area difficult, resulting in skin irritation and even infection. It is important for haemorrhoid sufferers to take extra care to wipe the area clean with soap and water and dry thoroughly after every bowel movement. Many anorectal problems, including fissures, fistulae, abscesses, or irritation and itching (pruritus ani), have similar symptoms and are incorrectly referred to as haemorrhoids. Signs and Symptoms of piles . Anal itching and irritation . Pain when sitting, or when passing a motion . Bright red blood on the stool, or toilet paper or even in the toilet bowl . Sensation of a tender or hard lump in the anal region Why do they Occur? Haemorrhoids develop when increased pressure causes the blood vessels in the anal region to become dilated and stretched, and then to protrude through the walls of the anal region. The blood in these swollen vessels may even clot and so form a firm lump or nodule. Piles containing clots are particularly likely to bleed. Haemorrhoids Why are They More Common During Pregnancy? During pregnancy, women may develop haemorrhoids for several reasons: . The increasingly heavy uterus (womb) puts pressure on the veins taking blood from the lower body to the heart. When the walls of these veins are weakened by increased blood pressure, the results can be a bulging blood vessels such as a varicose vein or haemorrhoids. . The hormone progesterone, which is produced during pregnancy, relaxes the walls of the veins, causing them to swell. . Progesterone also slows down the digestive system, increasing the pregnant woman’s tendency to become constipated. When she strains to pass a hard stool, added pressure is put on the blood vessels in the rectal area. . Iron supplements, which may be needed during pregnancy, may cause constipation. This also results in straining during bowel movements. . As the uterus grows, it can press on the bowel and slow down the passage of stool, resulting in straining during bowel movements. After Pregnancy In some cases, the haemorrhoids that develop during pregnancy shrink after delivery, causing no further symptoms. However, some women develop haemorrhoids for the first time after delivery. This is because of the immense pressure put on the weakened blood vessel walls during the straining of labour and delivery. Women may find that they have haemorrhoids, or even painful varicose veins in their vaginal and perineal area, after delivery. Constipation may also develop after delivery, due to the effects of pain-killers, or due to reluctance to pass stool because of pain in the vaginal and perineal areas. This ultimately results in a vicious cycle of straining during bowel movement, avoiding bowel movements because of pain, worsening constipation and consequent straining. This constant straining can cause new haemorrhoids to develop. Minimising Haemorrhoids Because haemorrhoids are worsened by constipation and the resultant straining during bowel movements, the most important step towards minimising haemorrhoids is to avoid constipation. Drink plenty of fluids and increase your fibre intake to improve bowel function. Cut down on processed foods. You could also try a soothing sitz bath to clean the area and soothe the irritated skin. Use a specially-designed sitz bath that fits over the toilet, or simply sit in a bath of warm or ice-cold water for 10 to 15 minutes, three or four times a day. Alternative remedies containing witch hazel can also be used, to clean the rectal area and help to reduce the swelling. If a haemorrhoid is extremely painful after a bowel movement, you could try applying an ice pack to the area for a few minutes. Creams can suppositories can help to reduce swelling, inflammation and itching. Treatments are usually available in topical cream for external haemorrhoids or suppository form for internal haemorrhoids. Fibre supplements may also be useful, to reduce constipation. Do Not strain when attempting to pass a motion, and don’t linger on the toilet because it puts pressure on the area. In addition do not scratch or wipe vigorously – or the condition may well worsen. Do Kegel exercise daily: Tense the muscles around your vagina and anus and hold for eight to 10 seconds before releasing and relaxing. Repeat 25 times. Not only will these increase circulation in the rectal area and strengthen the muscles around the anus (thereby decreasing the chance of haemorrhoids), but they also strengthen and tone the muscles around the vagina and urethra, which aids in postpartum recovery. Avoiding sitting or standing for long stretches of time during your pregnancy. If your job involves sitting, get up and move around for few minutes every hour or so. At home, lie on your left side when sleeping, reading, or watching TV to take the pressure off rectal veins and help increase blood return from the lower half of your body. Medical Treatment Consult your doctor if you notice any changes in bowel movements or rectal bleeding, as these could be symptoms of more serious conditions. The doctor may examine the anus and rectum to look for swollen blood vessels that indicate haemorrhoids. The doctor may also perform a digital rectal examination with a gloved finger, to check for abnormalities. Examinations may also be done using an anoscope or proctoscope (fibre-optic devices that a doctor passes through the anus to examine the inside of the bowel). If haemorrhoids are diagnosed, the initial treatment will focus on relieving the symptoms. Treatment might include sitting in warm water several times a day, applying a topical haemorrhoid cream or using suppositories, and increasing the amount of fibre in the diet. If these measures do not relieve the symptoms, further treatment may be needed. Whilst much depends on the severity of the piles and where they are situated, procedures that are commonly used to treat haemorrhoids include: . Rubber band ligation – which a rubber band is placed around the base of the haemorrhod. The band cuts off circulation, and the haemorrhoid withers away within a few days. . Infrared coagulation – in which the haemorrhoid is burnt off using a special infrared device. . Sclerotherapy – in which a chemical solution is injected around the blood vessels to shrink the haemorrhoid. . Haemorrhoidectomy – in which the haemorrhoids are surgically removed. Avoiding Constipation . Exercise regularly, as this helps to keep bowel movements regular. . Drink plenty of water – up to two litres a day . Increase your intake of fibre. Fibre holds water and allows for the formation of softer, bulkier stools that can pass through the colon more rapidly. Wheat bran, cereals, whole wheat, fresh vegetables and fresh and dried fruit are good sources. If this does not help, ask your doctor about a fibre supplement. . A dessertspoonful of linseed (readily available at most supermarkets) which has been soaked in a glassful of water overnight and swallowed first thing in the morning, every morning, is highly recommendable for those who are readily inclined to become constipated . Try to move your bowels at the same time every day. Do not ignore the urge to move your bowel, as this can worsen constipation. . Do not use laxatives, unless your doctor prescribes them. Some laxatives cause dangerous dehydration and electrolyte imbalances. In addition, your body may come to depend on laxatives for bowel movement, and lose the ability to pass a stool unaided. Haemorrhoids like this are very painfull