2: Cardiovascular system
advertisement

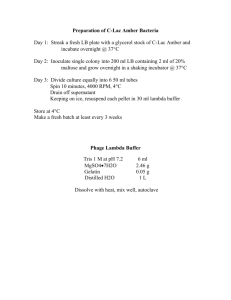
2: Cardiovascular system Please select a topic: 2.1 Positive inotropic drugs 2.2 Diuretics 2.3 Anti-arrhythmic drugs 2.4 Beta-adrenoceptor blocking drugs 2.5 Drugs affecting the renin-angiotensin 2.6 Nitrates, calcium-channel blockers, and system and some other antihypertensive other anti-antianginal drugs drugs 2.7 Sympathomimetics 2.8 Anticoagulants and protamine 2.9 Antiplatelet drugs 2.10 Myocardial infarction and fibrinolysis 2.11 Antifibrinolytic drugs and 2.12 Lipid-regulating drugs haemostatics 2.13 Local sclerosants Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default Amber 1 = Drugs with shared care agreement Amber 2 = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Drug & Therapeutics Committee Page 1 of 24 Date: 1.2.2012 2.1 Positive inotropic drugs Digoxin 62.5, 125, 250 microgram tablets Digoxin 250 micrograms/5ml elixir Digoxin 250 micrograms/ml injection Enoxamine 100mg/20ml injection (Emergency Drug Cupboard only) Digibind 38mg injection (restricted) Dose - Digoxin tablets 62.5micrograms, 125micrograms, 250micrograms; elixir 50micrograms/mL: rapid digitalisation, 1-1.5mg in divided doses over 24 hours; less urgent digitalisation, 250500micrograms daily (higher dose may be divided). Maintenance, 62.5-500micrograms daily. - Digoxin injection 250micrograms/mL: according to local guidance. - Enoxamine injection 100mg/20ml: see BNF - Digibind injection 38mg: see BNF Prescribing notes Digoxin is indicated for rate control in atrial fibrillation and symptomatic heart failure; it has no role in the prophylaxis of atrial fibrillation. For rapid rate control in atrial fibrillation, a loading dose of digoxin may be given intravenously or orally. Regular measurements of plasma digoxin concentrations are not usually required except to confirm toxic or sub-therapeutic levels, or to check compliance. Digoxin should be used with particular caution in the elderly and patients with renal impairment. Hypokalaemia predisposes to digoxin toxicity. Digoxin levels may be increased by drugs such as amiodarone, calcium channel blockers, quinine, hydroxychloroquine. Older Patients - Digoxin Loading and maintenance doses of digoxin should be adjusted according to renal function: age, sex and weight need to be considered. A lower maintenance dose (i.e. 62.5-125 micrograms daily) is usually adequate in older patients. Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default Amber 1 = Drugs with shared care agreement Amber 2 = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Drug & Therapeutics Committee Page 2 of 24 Date: 1.2.2012 2.2 Diuretics Thiazides and related diuretics Bendroflumethazide/Bendrofluazide 2.5mg, 5mg tablet Metolozone 5mg tablet Chlorothiazide 250mg/5ml and 100mg/5ml suspension Dose - Bendroflumethiazide tablets 2.5mg, 5mg: hypertension, 2.5mg daily. - Metolozone tablets 5mg: see BNF - Chlorothiazide suspension 250mg/5ml, 100mg/5ml: see BNF for Children Prescribing notes Allow 4 weeks for maximal antihypertensive effect of bendroflumethiazide. Bendroflumethiazide may be prescribed with furosemide (frusemide) for severe heart failure under hospital supervision; this must be carefully monitored. Loop diuretics Furosemide 20mg, 40mg, 500mg tablet Furosemide 20mg/5ml, 40mg/5ml liquid Furosemide 50mg/5ml injection Bumetanide 1mg, 5mg tablet Bumetanide 1mg/5ml liquid Bumetanide 1mg/2ml injection Dose - Furosemide tablets 20mg, 40mg, 500mg; liquid 20mg/5ml, 20mg/5ml: oedema, initially 40mg daily then adjusted according to response. - Furosemide injection 10mg/mL: slow intravenous injection, initially 20-50mg. Furosemide may be given by intravenous infusion at a rate not exceeding 4mg/minute. - Bumetanide tablets 1mg, 5mg; liquid 1mg/5ml: initially 1mg in the morning the adjusted according to response Prescribing notes Furosemide produces a dose-dependent diuresis within 1 hour if given orally or 30 minutes if given intravenously; duration of action, 6 hours. Furosemide 500mg tablets are scored and can be halved. Bumetanide may be an option in those patients that are not responding to furosemide (1mg bumetanide is equivalent to furosemide). Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default Amber 1 = Drugs with shared care agreement Amber 2 = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Drug & Therapeutics Committee Page 3 of 24 Date: 1.2.2012 Potassium-sparing diuretics Amiloride 5mg tablet Amiloride 5mg/5ml solution Dose - Amiloride tablets 5mg; oral solution 5mg/5ml: 5-20mg daily. Prescribing notes Amiloride is a weak diuretic with potassium-sparing properties, given with other diuretics if hypokalaemia is a problem; may take 2-3 days for full effect. Use with caution in renal impairment. Potassium-sparing diuretics such as amiloride are usually only necessary if hypokalaemia develops Aldosterone antagonists Eplerenone 25mg, 50mg tablet Spironolactone 25mg, 100mg tablet Spironolactone 50mg/5ml suspension Dose - Eplerenone tablets 25mg, 50mg: initially 25mg once daily, increased within 4 weeks to 50mg once daily. - Spironolactone tablets 25mg, 50mg, 100mg: heart failure in conjunction with ACE inhibitor, 25mg daily; higher doses may be needed in liver failure. Prescribing notes Spironolactone is an aldosterone antagonist used for oedema in hepatic cirrhosis or heart failure, and primary hyperaldosteronism. Spironolactone 25mg daily has been shown to reduce mortality in patients with severe heart failure receiving standard therapy including ACE inhibitors; renal function and electrolytes should be monitored. Use with caution in renal impairment. Eplerenone is to be used as an adjunct in stable patients with left ventricular dysfunction with evidence of heart failure following myocardial infarction (start therapy within 3-14 days of event). Eplerenone is an alternative aldosterone antagonist which may be prescribed for patients who develop gynaecomastia with spironolactone. Osmotic diuretics Mannitol 10%, 20% infusion polyfusor Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default Amber 1 = Drugs with shared care agreement Amber 2 = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Drug & Therapeutics Committee Page 4 of 24 Date: 1.2.2012 Older Patients - Diuretics All diuretics have the propensity to cause postural hypotension and thus collapse and falls in older patients. Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default Amber 1 = Drugs with shared care agreement Amber 2 = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Drug & Therapeutics Committee Page 5 of 24 Date: 1.2.2012 2.3 Anti-arrhythmic drugs Supraventricular arrhythmias Adenosine 3mg/ml injection Adenosine 30mg/10ml (Restricted/unlicensed) Dronedarone 400mg tablet Supraventricular and ventricular arrhythmias Amiodarone 100mg, 200mg tablet Amiodarone 150mg/3ml injection Amiodarone 300mg in 10ml prefilled syringe Atenolol 25mg, 50mg, 100mg tablets Atenolol 25mg/5ml syrup Atenolol 5mg/10ml injection Disopyramide 100mg capsule Disopyramide 50mg/5ml injection Flecainide 100mg tablet Flecainide 150mg/15ml injection Propafenone 150mg tablet Sotalol 40mg, 80mg, 160mg tablet Ventricular arrhythmias Lidocaine/Lignocaine 0.2% in 500ml infusion Lidocaine/Lignocaine 1% 10ml minijet Mexiletine 50mg capsules Dose Anti-arrhythmics are complex agents; intravenous injections or infusions should be given according to specialist advice. - Disopyramide capsules 100mg: orally 300-800mg daily in divided doses - Lidocaine injection 10mg/mL (1%), 20mg/mL (2%); infusion 1mg/mL (0.1%) and 2mg/mL (0.2%) in glucose 5%, 500mL. - Flecainide tablets 50mg, 100mg; injection 10mg/mL: orally, ventricular arrhythmias, 100mg twice daily; max 400mg daily, reduced after 3-5 days if possible; supraventricular arrhythmias, 50mg twice daily; max 300mg daily. - Atenolol tablets 25mg, 50mg, 100mg; syrup 25mg/5mL; injection 500micrograms/mL: orally, 50100mg daily. - Amiodarone tablets 100mg, 200mg; injection 50mg/mL: orally, 200mg 3 times daily for 1 week, then 200mg twice daily for 1 week, then usually 100-200mg daily thereafter. - Dronedarone tablets 400mg: orally, 400mg twice daily - Sotalol (with ECG monitoring and measurement of corrected QT interval) tablets 40mg, 80mg, 160mg: orally, initially 80mg daily in 1-2 divided doses increased every 2-3 days to 160-320mg Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default Amber 1 = Drugs with shared care agreement Amber 2 = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Drug & Therapeutics Committee Page 6 of 24 Date: 1.2.2012 daily in 2 divided doses; 480-640mg daily for life-threatening ventricular arrhythmias. - Verapamil tablets 40mg, 80mg, 120mg; m/r tablets 120mg, 240mg; m/r capsules 120mg, 180mg, 240mg; injection 2.5mg/mL: orally, supraventricular arrhythmias, 40-120mg 3 times daily for standard preparation; m/r verapamil, dose according to brand. See BNF. - Adenosine injection 3mg/mL. - Atropine injection 100micrograms/mL, 200micrograms/mL, 300micrograms/mL, 600micrograms/mL. - Digoxin tablets 62.5micrograms, 125micrograms and 250micrograms; elixir 50micrograms/mL; injection 250micrograms/mL. - Mexiletene capsules 50mg: see BNF Prescribing notes Amiodarone may cause corneal microdeposits, thyroid dysfunction, pneumonitis, peripheral neuropathy and hepatotoxicity. Liver-function and thyroid-function tests should be performed before treatment, and 6 monthly thereafter; chest X-ray should be done before treatment. Patients receiving amiodarone should avoid exposure of the skin to direct sunlight or sun lamps; a sunscreening product providing SPF 25 should be applied if amiodarone is prescribed. Amiodarone interacts with many drugs. There is a potential for drug interactions to occur for several weeks (or even months) after treatment with it has been stopped. Sotalol may cause atypical VT (torsades de pointes); it should be given with extreme caution with drugs known to prolong the QT interval e.g. erythromycin, chloroquine, haloperidol, lithium, tricyclic antidepressants, chlorpromazine. It should not be used for angina, hypertension, thyrotoxicosis or secondary prevention after myocardial infarction. Sotalol should be avoided in patients on diuretics or with hypokalaemia. For patients prescribed dronedarone, liver function tests should be performed: o Prior to treatment o On a monthly basis for six months o At months 9 and 12, and periodically thereafter With dronedarone if alanine transaminase (ALT) levels are elevated to ≥3 x upper limited of normal (ULN), levels should be re-measured within 48 to 72 hours. If ALT levels are confirmed to be ≥3 x ULN after re-measurement, dronedarone treatment should be withdrawn. Patients on dronedarone should be advised to contact healthcare professionals immediately in case of signs or symptoms of liver injury. Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default Amber 1 = Drugs with shared care agreement Amber 2 = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Drug & Therapeutics Committee Page 7 of 24 Date: 1.2.2012 2.4 Beta-adrenoceptor blocking drugs Atenolol 25mg, 50mg, 100mg tablets Atenolol 25mg/5ml syrup Atenolol 5mg/10ml injection Bisoprolol 1.25mg, 2.5mg, 3.75mg, 5mg, 10mg tablet Esmolol 100mg/10ml Esmolol 2.5g/250ml (ITU only) Labetolol 50mg, 100mg tablet Labetolol 5mg/ml injection Metoprolol 5mg/5ml injection Metoprolol 25mg/5ml suspension Metoprolol 50mg, 100mg tablet Nebivolol 5mg tablet Propranolol 10mg, 40mg tablet Propranolol 10mg/5ml and 80mg/5ml SF solution Propranolol 1mg/ml injection Propranolol M/R 80mg, 160mg capsule Sotalol 40mg, 80mg, 160mg tablet (For use in the treatment of heart failure only) Dose - Atenolol tablets 25mg, 50mg, 100mg; syrup 25mg/5mL: 25-100mg daily according to response. - Bisoprolol tablets 1.25mg, 2.5mg, 3.75mg, 5mg, 7.5mg, 10mg: stable, chronic heart failure, 1.25mg daily for 1 week, increased, if well tolerated, to 2.5mg daily for 1 week, then 3.75mg daily for 1 week, then 5mg daily for 4 weeks, then 7.5mg daily for 4 weeks, then 10mg daily maintenance. - Labetolol tablets 50mg, 100mg: see BNF - Metoprolol tablets 50mg, 100mg, suspension 25mg/5ml: see BNF - Propranolol tablets 10mg, 40mg, 80mg, 160mg: thyrotoxicosis (adjunct), anxiety tachycardia, 10-40mg 3-4 times daily. Anxiety with symptoms such as palpitations, sweating, tremor, 40mg once daily increased to 40mg 3 times daily if necessary. Migraine prophylaxis, essential tremor: initially 40mg 2-3 times daily, maintenance 80-160mg daily. Prescribing notes Bisoprolol is second-line for patients intolerant of atenolol in hypertension. Bisoprolol is first choice beta-blocker for stable, chronic heart failure initiated under specialist supervision. Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default Amber 1 = Drugs with shared care agreement Amber 2 = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Drug & Therapeutics Committee Page 8 of 24 Date: 1.2.2012 Beta-blockers may cause bronchospasm; avoid in patients suffering asthma. If a beta-blocker is required, a cardioselective beta-blocker should be selected, initiated at a low dose and the patient closely monitored. Sotalol is only used as an anti-arrhythmic. Propranolol is indicated for treatment of migraine, anxiety, thyrotoxicosis and essential tremor. 2.5 Drugs affecting the renin-angiotensin system and other antihypertensive drugs Vasodilator antihypertensive drugs Hydralazine 25mg tablet Hydralazine 20mg injection Minoxidil 5mg tablet Sodium nitroprusside 50mg/5ml injection Centrally acting antihypertensive drugs Methyldopa 125mg, 250mg, 500mg tablet Moxonidine 200 microgram, 300 microgram, 400 microgram tablet Clonidine 25 microgram and 100 microgram tablet Clonidine 150 microgram/ml injection Alpha-adrenoceptor blocking drugs 1st Choice Doxazosin 1mg, 2mg, 4mg tablet Doxazosin 4mg XL, 8mg XL tablet Alternatives Prazosin 1mg tablet Terazosin 2mg, 5mg tablet Dose - see BNF Prescribing notes Doxazosin is a third-line agent in the treatment of hypertension. It should be used with caution in patients with heart failure or impaired left ventricular function. Doxazosin may cause postural hypotension and first dose hypotension. Treatment should be initiated at the lowest dose possible. Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default Amber 1 = Drugs with shared care agreement Amber 2 = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Drug & Therapeutics Committee Page 9 of 24 Date: 1.2.2012 Angiotensin-converting enzyme inhibitors Captopril 12.5mg, 25mg tablet Enalapril 2.5mg, 5mg, 10mg tablet Lisinopril 2.5mg, 5mg, 10mg, 20mg tablet Perindopril 2mg, 4mg tablet Ramipril 1.25mg, 2.5mg, 5mg, 10mg capsule Dose - see BNF Prescribing notes ACE inhibitors are useful alternatives for hypertension when thiazides and beta-blockers are contra-indicated, not tolerated or fail to control blood pressure. For heart failure the dose of the ACE inhibitor should be titrated to a 'target' dose (or to the maximum tolerated dose if lower). See BNF. Urea and electrolytes should be checked within 1 week of commencing therapy. Enalapril should be prescribed once daily for hypertension. Ramipril should be prescribed as a once daily dose. Patients who have been initiated on twice daily dosing should be switched to an equivalent once daily dose/ Angiotensin-II receptor antagonists Candesartan 2mg, 4mg, 8mg, 16mg and 32mg tablets Irbesartan 75mg, 150mg tablet Valsartan 40mg, 80mg and 160mg capsules Dose - Candesartan tablets 2mg, 4mg, 8mg, 16mg, 32mg: recommended dose is 4-32 daily. See BNF. - Irbesartan tablets 75mg, 150mg, 300mg: recommended dose is 150-300mg once daily (in haemodialysis or in elderly over 75 years, initial dose of 75mg once daily may be used). See BNF. - Valsartan capsules 80mg, 160mg: 40mg-160mg daily. See BNF Prescribing notes Angiotensin-II receptor antagonists should be reserved for patients who develop a persistent cough with ACE inhibitors. Urea and electrolytes should be checked within 2 weeks of commencing therapy and after any change in dose. Losartan is available as a generic product and is less expensive currently than the other angiotensin-II receptor antagonists. Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default Amber 1 = Drugs with shared care agreement Amber 2 = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Drug & Therapeutics Committee Page 10 of 24 Date: 1.2.2012 Miscellaneous Phenoxybenzamine 10mg capsules Phentolamine 10mg/ml injection Guanethidine 10mg/ml injection (Theatres only) Iloprost nebules 10microgram/ml (Critical Care Only) Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default Amber 1 = Drugs with shared care agreement Amber 2 = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Drug & Therapeutics Committee Page 11 of 24 Date: 1.2.2012 2.6 Nitrates, calcium-channel blockers, and other anti-anginal drugs Nitrates Glyceryl trinitrate 400 microgram/dose spray Glyceryl trinitrate 2mg, 3mg, 5mg buccal m/r tablet Glyceryl trinitrate 5mg, 10mg skin patch Glyceryl trinitrate 5mg/5ml injection Isosorbide mononitrate 10mg, 20mg tablet Isosorbide dinitrate 10mg, 20mg tablet Isosorbide dinitrate 25mg/50ml injection Dose - Glyceryl trinitrate spray 400micrograms per puff; sublingual tablets 300micrograms, 500micrograms: sublingually, 300microgram-1mg repeated as required. - Glyceryl trinitrate buccal tablets m/r 2mg, 3mg, 5mg: treatment of angina, 2mg as required (1mg in sensitive patients), increased to 3mg if necessary; prophylaxis 1-3mg 3 times daily; 5mg in severe angina. Unstable angina (adjunct), up to 5mg with ECG monitoring. Congestive heart failure, 5mg 3 times daily, increased to 10mg 3 times daily in severe cases. Acute heart failure, 5mg repeated until symptoms abate. - Isosorbide mononitrate tablets 10mg, 20mg:: 20 - 40mg twice daily (10mg twice daily in those who have not previously received nitrates); up to 120mg daily in divided doses if required. - Isosorbide dinitrate tablets 10mg, 20mg: see BNF Prescribing notes To reduce the risk of nitrate tolerance, isosorbide mononitrate should be given twice daily 6-8 hours apart. Long-acting and transdermal nitrate preparations are significantly more expensive than standard formulations. A cost-effective branded long-acting preparation should be prescribed only for patients who have a problem with compliance. Glyceryl trinitrate (GTN) intravenous injection may be given when sublingual or buccal GTN is ineffective in patients with chest pain due to myocardial infarction or severe ischaemia, and in treatment of acute left ventricular failure. Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default Amber 1 = Drugs with shared care agreement Amber 2 = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Drug & Therapeutics Committee Page 12 of 24 Date: 1.2.2012 Calcium-channel blockers Amlodipine 5mg, 10mg tablet Diltiazem 60mg M/R tablets (Tildiem® Diltiazem 120mg, 240mg, 180mg, 300mg and 360mg s/r capsule (Viazem XL®) Diltiazem 200mg M/R capsules (Tildiem LA®) Lercanidipine 10mg tablets Nifedipine 5mg, 10mg capsule - Instant release formulation Nifedipine 10mg, 20mg s/r tablet (Adalat retard®) - 12 hourly formulation Nifedipine 10mg, 20mg m/r capsules (Coracten SR®) - 12 hourly formulation Nifedipine 30mg and 60mg XL capsules (Coracten XL®) - 24 hourly formulation Nimodipine 30mg tablet, 10mg/50ml injection Verapamil 40mg, 80mg,120mg tablet Verapamil 120mg s/r capsule Verapamil 40mg/5ml SF solution Verapamil 2.5mg/ml injection Dose - Amlodipine tablets 5mg, 10mg: hypertension or angina, initially 5mg once daily; max. 10mg once daily. - Diltiazem m/r tablets 60mg, 90mg, 120mg; m/r capsules 60mg, 90mg, 120mg, 180mg, 200mg, 240mg, 300mg, 360mg: dose according to brand. See BNF. - Verapamil tablets 40mg, 80mg, 120mg; m/r capsules 120mg: dose according to brand. See BNF. Prescribing notes Nifedipine m/r is first choice calcium-channel blocker for hypertension. The brand of different calcium-channel blockers should be specified since different formulations may have different clinical effects. The most cost-effective brand should be prescribed. Sudden withdrawal of calcium-channel blockers may exacerbate angina; withdraw if ischaemic pain occurs or worsens after starting treatment. Nifedipine should not be given without a beta-blocker for angina. Short-acting formulations of nifedipine capsules have been associated with large variations in blood pressure and reflex tachycardia; they are no longer recommended for angina or hypertension. Diltiazem is first choice calcium-channel blocker for angina if a beta-blocker cannot be used; it is also given for hypertension. It has less negative inotropic effects than verapamil and significant myocardial depression is rare. Use caution if given with beta-blockers due to risk of bradycardia. The most cost-effective brand should be prescribed. Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default Amber 1 = Drugs with shared care agreement Amber 2 = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Drug & Therapeutics Committee Page 13 of 24 Date: 1.2.2012 Verapamil is used for angina, hypertension and arrhythmia; it reduces cardiac output, slows the heart rate and may affect atrioventricular conduction. It may produce heart failure, exacerbate conduction disorders, and high doses may cause hypotension. It should not be used with beta-blockers. Other Anti-anginal drugs Nicorandil 10mg, 20mg tablet Ivabradine 5mg, 7.5mg tablets Dose - see BNF Prescribing notes Nicorandil is used when other anti-anginal drugs are insufficient; they have similar efficacy to other anti-anginal drugs in controlling symptoms but there is little evidence regarding their efficacy in combination with other anti-anginal drugs. Ivabradine is approved for use, on the initiation of a cardiologist, chronic stable angina in patients for whom heart rate control is desirable and also have a contra-indication or intolerance of beta-blockers and rate limiting calcium channel blockers. Peripheral vasodilators and related drugs Cinnarizine 75mg capsules Pentoxyfilline 400mg tablets Naftidrofuryl 100mg capsules Prescribing notes Patients suffering intermittent claudication should be advised to exercise and stop smoking. First-line management of Raynaud's phenomenon includes avoiding exposure to cold and stopping smoking. Peripheral vasodilators are of limited value. Cilostazol, pentoxifylline and inositol are not recommended for the treatment of intermittent claudication. Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default Amber 1 = Drugs with shared care agreement Amber 2 = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Drug & Therapeutics Committee Page 14 of 24 Date: 1.2.2012 2.7 Sympathomimetics Inotropic sympathomimetics Dobutamine 250mg/20ml injection Dopamine 200mg/5ml injection Dopexamine 50mg/5ml injection Isoprenaline 2.25mg/2ml injection (unlicensed) Vasoconstrictor sympathomimetics Ephedrine 30mg/ml injection Metaraminol 10mg/ml injection Noradrenaline/Norepinephrine 2mg/ml injection Phenylephrine 10mg/ml injection (ITU only) Cardiopulmonary resuscitation Adrenaline/Epinephrine 100 micrograms/ml(1:10,000) minijet Adrenaline/Epinephrine 100 micrograms/ml(1:10,000) injection Dose - See BNF for dosing recommendations. - Adrenaline injection 100micrograms/mL: during cardiopulmonary resuscitation (CPR), 1mg (10mL) intravenously flushed with saline, and repeated every 3 minutes. - Dobutamine strong sterile solution,12.5mg/mL and 50mg/mL. - Dopamine sterile concentrate, 40mg/mL and 160mg/mL; intravenous infusion, 400mg or 800mg in 250mL glucose 5%. - Noradrenaline acid tartrate injection 2mg/mL (equivalent to noradrenaline base 1mg/mL). Prescribing notes Low dose dopamine induces vasodilatation and increases renal perfusion; higher doses (more than 5micrograms/kg/min) produce vasoconstriction and may exacerbate heart failure. Inotropic and vasoconstrictor sympathomimetics should preferably be used only in the intensive care setting with invasive haemodynamic monitoring. Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default Amber 1 = Drugs with shared care agreement Amber 2 = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Drug & Therapeutics Committee Page 15 of 24 Date: 1.2.2012 2.8 Anticoagulants and protamine Parenteral anticoagulants Fondaparinux 2.5mg syringe (Haematology advice only) Standard heparins Heparin 20000units/20ml, 5000units/5ml injection Heparin 5000 units/0.2ml (Calciparine®) Heparin 50 units/5ml (Hepsal®) Low molecular weight heparins Enoxaparin 20mg, 40mg, 60mg, 80mg, 100mg and 150 mg pre-filled syringe Tinzaparin 20000 units/ml (2ml) vial Tinzaparin 20000 unit/ml pre-filled syringes (10000, 14000, 18000, 40000 units) Tinzaparin 10000/ml pre-filled syringes (3500, 4500 units) Dose - See BNF for dosing recommendations. - Standard heparin 1000units/mL, 20 000units/20mL. - Enoxaparin 100mg/mL (0.2mL, 0.4mL, 0.6mL, 0.8mL and 1mL syringes); 150mg/mL (0.8mL, 1mL syringes). - Tinzaparin 10,000 units/mL (0.25mL, 0.35mL, 0.45mL syringes or 2mL vial) or 20,000 units/mL (0.5mL, 0.7mL, 0.9mL syringes or 2mL vial). Prescribing notes See Trust “Unfractionated Heparin Dosing Guidelines”. See Trust Thrombophylaxis guidelines on use of LMWHs. Treatment with standard heparin is continued until no longer required, or until warfarin takes effect (at least 3 days). Heparin is monitored using activated partial thromboplastin time (APTT) to give a patient/control ratio of 1.5-2.5. Low molecular weight heparin does not require APTT monitoring; if necessary, anti-factor Xa can be monitored. Heparins may induce two types of thrombocytopenia: the first, usually develops within 1-4 days of initiation, is acute, usually mild, and may resolve spontaneously. The second type has an immunological basis and is more serious: it usually occurs after 7-11 days, or more quickly in previously exposed patients, and is often associated with serious thromboembolic complications or bleeding. Serial platelet counts should be measured if heparin is given for longer than 5 days (or sooner if previously exposed), and heparin stopped if thrombocytopenia develops. Lepirudin injection will be discontinued in the UK from 1st April 2012. Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default Amber 1 = Drugs with shared care agreement Amber 2 = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Drug & Therapeutics Committee Page 16 of 24 Date: 1.2.2012 Epoprostenol Epoprostenol 500 microgram vial Oral anticoagulants Warfarin 1mg, 3mg and 5mg tablets Phenindione 10mg, 25mg and 50mg tablets Dabigatran 75mg capsules Dabigatran 110mg and 150mg capsules Dose - Warfarin tablets 500micrograms (white), 1mg (brown), 3mg (blue), 5mg (pink): induction dose 10mg daily for 2 days, then adjusted according to INR. A lower induction dose may be required by some patients; see BNF for details. Prescribing notes See Trust “GUIDELINES FOR WARFARIN- INDUCTION and MAINTENANCE DOSES” The warfarin dose is adjusted according to the international normalised ratio (INR). The target INR should be clearly identified at initiation of therapy, and measured daily or on alternate days initially, then at longer intervals (depending on response) then up to every 12 weeks. Indication and duration of treatment should be clearly recorded at initiation of treatment; the patient-held anticoagulant treatment booklet should be used. See BNF for details. The plasma half-life of warfarin is 35 hours; a steady anticoagulant effect is achieved after about one week. If immediate anticoagulation is required, heparin must be given concomitantly. There are many clinically important interactions with warfarin; clinicians are strongly advised to consult BNF before prescribing. Vitamin K (phytomenadione) can be given to reverse the effects of warfarin but takes 6-12 hours to become effective. Immediate reversal of the anticoagulant effect of warfarin may be achieved with fresh frozen plasma or prothrombin complex concentrate; see BNF for details. Specialist haematological advice should be sought. Dabigatran is approved for use in hip and knee replacement surgery for prophylaxis of venous thromboembolism. Warfarin will continue to be the first line drug of choice for prevention of stroke in patients with non-valvular AF but Dabigitran be considered for patients with a warfarin allergy or an absolute contra-indication to warfarin (Dabigatran may also be contra-indicated in some of these indications). Please note that a bleeding risk that would lead to a contraindication to warfarin would also contra-indicate to Dabigatran. Older Patients - Warfarin Warfarin should be used with caution in patients with confusion or a tendency to fall. Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default Amber 1 = Drugs with shared care agreement Amber 2 = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Drug & Therapeutics Committee Page 17 of 24 Date: 1.2.2012 Protamine Protamine 50mg/5ml injection Prescribing notes Protamine sulphate reverses the effects of standard heparin, but only partially reverses the effects of low molecular weight heparins. Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default Amber 1 = Drugs with shared care agreement Amber 2 = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Drug & Therapeutics Committee Page 18 of 24 Date: 1.2.2012 2.9 Antiplatelet drugs Aspirin 75mg and 300mg dispersible tablets Aspirin 75mg and 300mg e/c tablets Aspirin 150mg suppositories Clopidogrel 75mg tablets Dipyridamole 50mg/5ml suspension Dipyridamole 200mg s/r capsules Prasuguel 5mg and 10mg tablets Tirofiban 12.5mg/50ml injection Dose - Aspirin dispersible tablets 75mg, 300mg: prophylaxis of cerebrovascular disease or myocardial infarction, initial loading dose of 150-300mg, then 75mg daily. - Clopidogrel tablets 75mg: for acute coronary syndrome, 75mg once daily for up to 12 months in combination with aspirin. An initial loading dose of clopidogrel 300mg is recommended. - Dipyridamole SR capsules 200mg: for secondary prevention of ischaemic stroke and transient ischaemic attacks (used alone or combination with aspirin) 200mg capsule twice daily. - Prasugrel tablets 5mg, 10mg: (with aspirin) initially 60mg as a single dose then body-weight over 60kg, 10mg once daily or body-weight under 60kg or over 75 years, 5mg once daily. - Tirofiban injection 12.5mg/50ml: see BNF Prescribing notes The e/c formulations of aspirin are not recommended. Dipyridamole m/r or low dose aspirin may be used with warfarin for prophylaxis of thromboembolism due to prosthetic heart valves. Patients with proven intolerance to aspirin may be prescribed clopidogrel to prevent further events in stroke, myocardial infarction or peripheral vascular disease. Aspirin and clopidogrel may be prescribed concomitantly for acute coronary syndrome for up to 12 months, after which clopidogrel is discontinued. Hospital specialists may prescribe clopidogrel for up to 3 months to prevent coronary artery stent occlusion. The combination of dipyridamole and clopidogrel has not been adequately evaluated and is therefore not recommended. There is a clinically significant interaction between clopidogrel and omeprazole making clopidogrel less effective. If concomitant use of clopidogrel and a proton pump is necessary, then lansoprazole would be an appropriate choice. Prasugel in combination with aspirin 75mg is an option for treatment acute coronary syndrome undergoing PCI. Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default Amber 1 = Drugs with shared care agreement Amber 2 = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Drug & Therapeutics Committee Page 19 of 24 Date: 1.2.2012 2.10 Myocardial infarction and fibrinolysis Alteplase 20mg and 50mg injection Streptokinase 1.5million and 250000 unit injection Tenecteplase and 50mg injection (a) acute myocardial infarction First choice: tenecteplase Prescribing notes Thrombolysis is effective if given as soon as possible after acute myocardial infarction; urgent transfer to hospital is essential. Tenecteplase has the advantage of availability as a single, weight adjusted, intravenous bolus injection. It can also be used in patients who have ever received streptokinase, suffered a recent streptococcal infection or developed a hypersensitivity reaction to streptokinase. If severe bleeding occurs, the fibrinolytic should be discontinued; coagulation factors and/or tranexamic acid may be required. (b) acute ischaemic stroke First choice: alteplase Prescribing notes Alteplase must be used in strict accordance with detailed protocols in a specialist acute stroke unit. Treatment must be started within 3 hours of onset of symptoms and after exclusion of intracranial haemorrhage by means of appropriate imaging techniques. Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default Amber 1 = Drugs with shared care agreement Amber 2 = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Drug & Therapeutics Committee Page 20 of 24 Date: 1.2.2012 2.11 Antifibrinolytic drugs and haemostatics Etamsylate 500mg tablets Tranexamic acid 100mg/ml injection Tranexamic acid 500mg tablets Factor VIIa 1mg and 5mg injection (Novoseven®) Prothrombin complex 250unit and 500unit injection (Beriplex®) Dose - Tranexamic acid tablets 500mg; injection 100mg/mL: orally, menorrhagia (initiated when heavy bleeding has started), 1-1.5g 3-4 times daily for 3-4 days. Slow intravenous injection: local fibrinolysis 0.5-1g 3 times daily. - Other products: see BNF or product literature Prescribing notes The manufacturer recommends regular eye examinations and liver function tests when tranexamic acid is used long-term for hereditary angioneurotic oedema; however, the BNF states that the need for regular eye examinations during long-term treatment is based on unsatisfactory evidence. Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default Amber 1 = Drugs with shared care agreement Amber 2 = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Drug & Therapeutics Committee Page 21 of 24 Date: 1.2.2012 2.12 Lipid-regulating drugs Anion-exchange resins Colestyramine 4g sachets Fibrates Bezafibrate 200mg tablets Bezafibrate 400mg m/r tablets Ciprofibrate 100mg tablets Fenofibrate MR 160mg tablets Prescribing notes Fibrates have been less well tested in clinical trials. They are mainly of benefit in those with mixed hyperlipidaemia and low HDL cholesterol. Statins Atorvastatin 10mg, 20mg, 40mg and 80mg tablets Pravastatin 10mg, 20mg and 40mg tablets Simvastatin 10mg, 20mg and 40mg tablets Rosuvastatin 5mg, 10mg and 20mg tablets Dose - Atorvastatin tablets 10mg, 20mg, 40mg, 80mg: hyperlipidaemia, 10-80mg at night - Simvastatin tablets 10mg, 20mg, 40mg, 80mg: hyperlipidaemia, 10-80mg at night; coronary heart disease, initially 20mg at night, max 80mg at night. - Pravastatin tablets 10m, 20mg, 40mg: see BNF - Rosuvastatin tablets 5mg, 10mg, 20mg: see BNF Prescribing notes Lowering cholesterol is associated with reduced mortality and morbidity in patients at high and moderate risk of, or with established, cardiovascular and cerebrovascular disease. Pravastatin is less likely to interact with other drugs than atorvastatin or simvastatin and may be preferred in certain situations, such as in patients receiving warfarin, digoxin or ciclosporin. Generic simvastatin is substantially lower cost than other lipid lowering agents. Caution should be exercised when prescribing other drugs with statins. Simvastatin and atorvastatin interact with many drugs including azole antifungals, macrolide antibiotics, amiodarone, verapamil, grapefruit juice and warfarin. See BNF for full list of interactions. Caution should be exercised when prescribing simvastatin 80mg daily due to the increased risk of adverse effects. Other Ezetimibe 10mg tablets Omacor capsules Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default Amber 1 = Drugs with shared care agreement Amber 2 = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Drug & Therapeutics Committee Page 22 of 24 Date: 1.2.2012 Dose - Ezetimibe tablets 10mg: 10mg once daily. - Omacor capsules: see BNF Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default Amber 1 = Drugs with shared care agreement Amber 2 = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Drug & Therapeutics Committee Page 23 of 24 Date: 1.2.2012 2.13 Local sclerosants Ethanolamine oleate 5% injection Sodium tetradecyl sulphate 0.5%, 1% and 3% injection Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default Amber 1 = Drugs with shared care agreement Amber 2 = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Drug & Therapeutics Committee Page 24 of 24 Date: 1.2.2012