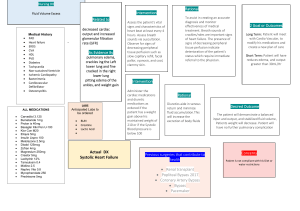
Patient has Diagnosis of Heart Failure
advertisement

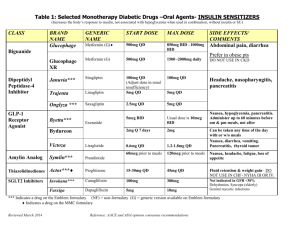
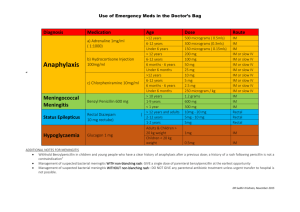
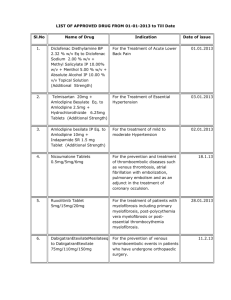
Therapy of Heart Failure Patient has Diagnosis of Heart Failure Pharmacological Management Fluid Retention Atrial Fibrillation Ace-Inhibitors Angiotensin II antagonists (ARB) Beta-Blockers and Ivabradine Aldosterone Antagonists Underlying Disorders Diastolic Heart Failure Referral to Clinic Removing excess fluid is an initial essential, aim to normalise JVP, and clear lungs. Frusemide 40-80mg daily common OP doses. Watch U/E, BP and symptoms. Controlling ventricular rate is also an initial essential, aim resting HR <70. Digoxin 0.0625mg / 0.125mg / 0.25mg od po depending on renal function especially used in acute setting. As OP preferably use bisoprolol 2.5mg / 5mg / 10mg. Once HR controlled usually stop digoxin. If beta-blocker fails in HR control continue / add digoxin. Remember anticoagulation for stroke prevention. Warfarin to be used in HF and AF unless contraindicated. Essential therapy in LV systolic dysfunction. Titrate dose upwards at approx 2-4 week intervals, usually ramipril 2.5mg / 5mg / 10mg po od. Watch U/E and BP. Use as alternative to ACE-I (usually cough), usually candesartan 4mg / 8mg / 16mg Beta-Blockers routinely indicated in systolic dysfunction, (both in AF and SR). eg: bisoprolol 2.5mg / 5mg / 10mg po od as tolerated. Control of heart rate also important. In SR, if resting HR >74bpm despite optimal beta-blocker, then add ivabradine 5mg bd po / 7.5mg bd po. Aim HR not >60 at rest. In AF ivabradine is contra-indicated: use betablocker +/- digoxin as needed. Moderate/severe LV systolic impairment: routinely add spironolactone 25mg od po. Watch U/E especially hyperkalaemia Use eplerenone 25mg od po if gynaecomastia, or within 3-14 days of acute MI Need therapy in their own right – for example hypertension control and diabetes. Secondary prevention for CAD: aspirin 75mg od and statin. Clopidogrel 75mg od for 1 year post acute coronary syndrome and/or stenting. Heart failure with normal ejection fraction. Diuretics and heart rate control as needed, together with therapy of underlying disorders, most commonly hypertension. No mandate for ACE-I, ARB, or aldosterone anatagonists, though often used empirically. All patients with heart failure should be referred to hospital clinic. [NICE 108]. All (new) patients with suspected heart failure refer via NTProBNP pathway via the ICE_Desktop application. Heart Failure Team Hampshire Hospitals Foundation Trust. V1 April 2012 Dr Barnaby Thwaites