Evaluation of the Range of Safe, Effective and
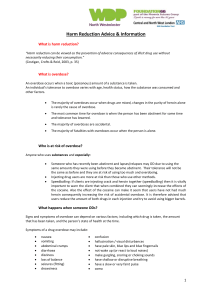
advertisement

Public Health Wales Safe, effective and cost effective interventions for IDUs and stimulant users Evaluation of the range of safe, effective and cost effective interventions aimed at injecting drug users, primary stimulant users and prevention of drug related overdose and death Authors: S.E Health Protection Team, National Public Health Service Date: 17/11/09 Version: 0e Status: Final Purpose and Summary of Document: This report provides a review of the international evidence on safe, effective and cost effective interventions aimed at injecting drug users; primary stimulant users and interventions aimed at reducing overdose and drug related deaths Publication/Distribution: For publication on Public Health Wales intranet and internet Author: Noel Craine, Josie Smith Date: 17/11/09 Status: Final Public Health Wales Safe, effective and cost effective interventions for IDUs and stimulant users Contents Executive Summary 3 1 Introduction 7 2 Methodology and focus 7 3 Areas of evaluation 8 3.1 Safe, effective and cost effective interventions for injecting drug users 9 3.1.1 Needle and syringe programs 9 3.1.2 Vending machines (needle / syringe dispensing machines) 12 3.1.3 Drug consumption rooms 15 3.1.4 Provision of harm reduction and safe injecting information 16 3.1.5 Blood borne virus management 17 3.1.6 Provision of injecting related health care 18 3.2 Safe, effective and cost effective interventions to meet the needs of stimulant users 19 3.2.1 Interventions to meet the needs of stimulant users 19 3.2.2 Substitute prescribing 20 3.2.3 Residential Rehabilitation 20 3.2.4 Contingency Management 20 3.2.5 Psychosocial interventions and brief interventions 21 3.2.6 Provision of equipment used in the consumption of stimulants 22 3.3 Safe, effective and cost effective interventions targeted at reducing overdose and drug related deaths 23 3.3.1 Provision of education and information relating to overdose 23 3.3.2 Prevention of overdose post-release from prison services 24 3.3.3 Identification and intervention of those at risk of suicide 24 3.3.4 Provision of Naloxone 25 3.3.5 Overdose and stimulant drug use 25 3.3.6 Drug treatment and overdose 25 3.3.7 Overdose and antidepressant and benzodiazepine prescribing 26 3.3.8 Local arrangements between Police and ambulance arrangements 26 3.3.9 Accident and Emergency department follow-up 26 3.3.10 Information dissemination via public health alerts 26 4 References 27 Author: Noel Craine, Josie Smith Date: 17/11/09 Status: Final Public Health Wales Safe, effective and cost effective interventions for IDUs and stimulant users Executive Summary The following broad areas for intervention were evaluated: a) Interventions for injecting drug users (IDUs) b) Interventions to meet the needs of stimulant users (including cocaine, crack, amphetamine and methamphetamine) c) Interventions targeted at reducing overdoses and drug related deaths This report is not a systematic review; rather it is a pragmatic summary of peer reviewed evidence. Lack of available peer review evidence does not necessarily indicate lack of effectiveness of an intervention The report focuses on interventions with the potential to reduce: - blood borne viral (BBV) transmission - drug overdose - bacterial infections - tissue damage due to injections - medical complications related to drug use INTERVENTIONS FOR INJECTING DRUG USERS (IDUS) Needle and syringe programmes (NSPs) There is compelling evidence that increasing the availability and utilisation of sterile injecting equipment by IDUs reduces HIV substantially There is no convincing evidence of any major unintended negative consequences NSPs are cost effective NSPs have additional and worthwhile benefits apart from reducing HIV infection among IDUs Pharmacies and vending machines increase the availability and probable utilisation of sterile injecting equipment by IDUs Vending machines can provide 24 hour availability and improve access in locations that are difficult to serve Participation in NSPs reduces injecting risk behaviours in IDUs e.g. sharing behaviours Prison based NSPs are feasible and can provide benefits in the reduction of risk behaviour and transmission of BBVs There is insufficient evidence to determine the impact of NSPs on hepatitis C infection in injecting drug users Bleach and other forms of disinfection are not supported by good evidence of effectiveness for reducing HIV infection Drug Consumption Rooms (DCRs) or Safe Injecting Facilities (SIFs) Author: Noel Craine, Josie Smith Date: 17/11/09 Status: Final Public Health Wales Safe, effective and cost effective interventions for IDUs and stimulant users DCRs may offer a unique and promising way to work with the most problematic users – to reduce the risk of overdose, improve their health and lessen the costs to society DCRs may contribute to a reduced incidence of hepatitis C Clarification required establishment of DCRs regarding the legal issues around the Hepatitis B (HBV) vaccination HBV vaccination is a key intervention in reducing the direct and indirect harms associated with injecting drug use IDUs should be vaccinated against HBV and vaccination should be prioritised by all substance misuse services including prison health care services Provision of harm reduction information and brief behavioural interventions (BBIs) There has been no systematic evaluation or review level evidence for the cost effectiveness of general, unstructured provision of information on harm reduction and safe injecting however high quality and up to date information should be provided within the full range of health care setting where there is contact with potential, current or ex drug users. BBIs are a potential means to facilitate behaviour change within the area of substance misuse e.g. in preventing HIV Evaluations of BBIs as an approach to risk reduction required research to determine both efficacy and effectiveness Peer delivered interventions may potentially play a role in risk reduction however further evaluation is required Blood borne virus management Dried blood spot testing as an alternative to venepuncture represents a highly effective means of diagnosis BBVs amongst current and ex injecting drug users and can be undertaken with a range of substance misuse services Treatment of BBVs in current and ex injecting drug users is effective and cost-effective (successful outcome of treatment depends on a number of factors) Diagnosis of BBVs in ex and current drug users can allow for information and behavioural lifestyle changes e.g. alcohol consumption that can have a major impact on disease progression INTERVENTIONS TO MEET THE NEEDS OF STIMULANT USERS (INCLUDING COCAINE, CRACK AND AMPHETAMINE Author: Noel Craine, Josie Smith Date: 17/11/09 Status: Final Public Health Wales Safe, effective and cost effective interventions for IDUs and stimulant users Evaluation of the Crack Treatment Delivery Model (CTDM) concluded that appropriate treatment can help reduce high levels of crack use and for those in treatment there are quantifiable health benefits Service users placed importance upon fast access to treatment as appropriateness of the service Dexamphetamine prescribing may influence drug use and increase treatment contact and retention. Drug free psychosocial interventions such as counselling, provided on a non-residential basis are the most cost effective option for clients with few complicating problems There is little understanding of how to prompt initial contact with treatment services. Once made, rapid intake, proactive reminders and practical help improve treatment uptake. Empathy and understanding amongst key workers is important in retention and outcomes Recognised psychotherapies delivered by professional psychologists perform no better that well structured drug counselling Cognitive behavioural approaches have an evidence base to support them and group therapy may be as effective as individual therapy Intensive residential rehabilitation may be appropriate for the most complex cases Evidence for the effectiveness of residential rehabilitation specific to stimulant dependence with the UK context is required Research specific to cocaine-dependent outpatients with depression and to amphetamine users suggested benefits from Motivational Interviewing In addition to injection, stimulants may be taken by snorting, smoking and ingesting orally. A recent review of non-injection drug use and hepatitis C infection identified gaps in research and concluded that the causal pathway to infection remained unclear however there is a theoretical possibility of BBV transmission from sharing crack pipes and other non injecting equipment. Provision of this equipment improves engagement Evaluation of the range of safe, effective and cost effective interventions targeted at reducing overdoses and drug related deaths The primary means to reduce overdose include: Engendering behaviour change around the risk behaviours that lead to overdose; this includes education around risks and more broadly, high standard and appropriately dosed drug treatment that ensures tolerance to opiates is maintained and that reduces injecting drug use. Responses and interventions to reduce the mortality rate associated with overdose once it has occurred e.g. training in resuscitation techniques, Author: Noel Craine, Josie Smith Date: 17/11/09 Status: Final Public Health Wales Safe, effective and cost effective interventions for IDUs and stimulant users local agreements with police to encourage witnesses to call an ambulance and the provision of naloxone to reverse the effects of opiate overdose Information dissemination via public health alerts to significant changes within drug supply that may influence overdose and to outbreaks of highly pathogenic bacterial infections. providing safe environments for drug use by individuals vulnerable to overdose e.g. via safe injecting facilities Education around overdose risks, and rapid admission into specialist drug treatment services for individuals who are likely to relapse into opiate use upon release from prison Substance misusers prone to suicide through deliberate overdose tend to enter treatment. Whilst in treatment the risk is modestly reduced and dropping out or being thrown out of treatment restores high risk Engaging drug users in treatment reduces drug related deaths, however treatment must be high quality and tailored to patient need with careful consideration of tolerance A quantitative evaluation of cocaine, crack cocaine and amphetamine use in relation to drug related death in the UK would provide valuable evidence in this area Data on overdose admission to accident and emergency (A&E) departments show high levels of recidivism amongst vulnerable individuals. This environment thus presents an opportunity for intervention, e.g. education and referral to specialist services, for those vulnerable individuals who are repeatedly overdosing and attending A & E services Author: Noel Craine, Josie Smith Date: 17/11/09 Status: Final Public Health Wales Safe, effective and cost effective interventions for IDUs and stimulant users Introduction 1 The purpose of this report is to provide a succinct review of the international evidence behind key health care interventions targeted at injecting drug users. The report will focus on interventions with the potential to reduce: blood borne viral transmission drug overdose bacterial infections tissue damage due to injections medical complications related to drug use The report will not examine the evidence base behind substitution treatment or psychosocial interventions for opiate substitution treatment. These two central health interventions targeting injecting drug users have been the subject of thorough review elsewhere (Gossop et al, 2001; Gossop, 2006; Campbell et al; 2007). 2 Methodology and focus This report is not a systematic review; rather it is a pragmatic summary of peer reviewed evidence. To identify key research and evaluation existing publications of key UK and international professional bodies were examined to identify evidence reviews. Publications from World Health Organisation (WHO), The National Treatment Agency (NTA), the Advisory Council on the Misuse of Drugs (ACMD), the Scottish Executive, the Department of Health (DoH), and the National Institute for Health and Clinical Excellence (NICE) were reviewed. Where such review level evidence was not available peer reviewed journals were searched using the Medline database. It should be emphasised that the evaluation of health interventions targeting injecting drug use faces major methodological challenges that, to date, have restricted the quality of research evidence. Difficult to access populations, lack of control groups, lack of studies with sufficient statistical power, poorly defined outcome measures, lack of robust baseline data and regression to the mean all contribute in varying degrees to a lack of clarity in effectiveness and cost effectiveness studies. A lack of evidence should not be considered as evidence of in-effectiveness; thus biological plausibility and the other Bradford Hill causal criteria are used by some reviews for interpreting the data (see WHO, 2004 for a useful summary of these criteria). This report limits its focus to the areas of intervention listed below, in practice there is considerable overlap between these interventions, for example provision of harm reduction material and vending machines are part of needle and syringe programs (NSP). It is suggested that this evidence is considered alongside the comprehensive NTA paper ‘Treating drug misuse problems: evidence of effectiveness’ (Gossop, 2006). Author: Noel Craine, Josie Smith Date: 17/11/09 Status: Final Public Health Wales 3 Safe, effective and cost effective interventions for IDUs and stimulant users Areas of evaluation The following broad areas for intervention were evaluated: a) Interventions for injecting drug users b) Interventions to meet the needs of stimulant users (including cocaine, crack, amphetamine and methamphetamine) c) Interventions targeted at reducing overdoses and drug related deaths The degree to which the interventions discussed have been subjected to either systematic review or to primary research varies greatly. In addition, rigorous cost-effective appraisals of many of the interventions considered are rare. This is reflected in the following report and will be addresses in the second stage of this report process. Author: Noel Craine, Josie Smith Date: 17/11/09 Status: Final Public Health Wales 3.1 Safe, effective and cost effective interventions for IDUs and stimulant users Evaluation of the range of safe, effective and cost effective interventions for injecting drug users 3.1.1 Needle and syringe programs What are needle and syringe programs? Needle and syringe programs (NSPs) (also referred to as needle exchange programs) are programs that, in a range of situations and with different models of delivery, provide injecting drug users (IDUs) with sterile needles, syringes and other injecting related paraphernalia including sterile water, one use cookers, one use filters and citric acid / vitamin C. NSPs also incorporate and encourage the return and safe disposal of used injecting equipment. In the UK, NSPs are delivered via community pharmacies, Tier 2 and 3 drug services, hospital A&E departments and also by specialist mobile, outreach services, hostels and custody suites. What are the potential health benefits, and key roles of needle and syringe programs in community settings? The potential benefits and key roles of NSP are: Reducing the transmission of blood borne viruses; in particular HIV, hepatitis C (HCV) and hepatitis B (HBV) Reducing the occurrence of soft tissue skin infections around injecting sites by supporting increased hygiene in injection practices, and the provision of wound care management Education of IDUs on the risks of overdose, blood borne viral transmission, safe injecting practices and associated risks of injection including venous damage and deep vein thromboses Provision of vaccinations for hepatitis A, hepatitis B and tetanus Route for referral of IDUs into drug treatment services Education and information on sexual health and the provision of condoms Education on alternative routes of ingesting illicit drugs including smoking, and reducing move to injecting Break the cycle – a route transition intervention aimed at reducing the initiation of others into injecting What is the evidence for the effectiveness of needle and syringe programs? NSP programs have been recently subjected to three high standard evidence reviews: - World Health Organisation evidence for action technical paper (WHO, 2004) - NICE Needle Syringe Programme appraisal (NICE, 2008a) - Health Protection Scotland review of evidence (Palmeteer et al, 2008) The WHO review examined the effectiveness of NSPs in reducing HIV/AIDS among IDUs. The NICE review, ‘a review of reviews’, looked at reviews of the Author: Noel Craine, Josie Smith Date: 17/11/09 Status: Final Public Health Wales Safe, effective and cost effective interventions for IDUs and stimulant users effectiveness and cost effectiveness of NSPs for IDUs (NICE, 2008a), and an additional review of the qualitative evidence for NSP. The Scottish review carried out by Health Protection Scotland, was a ‘review of reviews’ of evidence for the effectiveness of harm reduction interventions in preventing hepatitis C transmission among injecting drug users (Palmateer et al, 2008). English language literature was systematically searched to identify reviews of the impacts of selected interventions on HCV transmission. These reviews have focused primarily on the impact of NSP on the transmission of infectious disease. The evidence presented here is a summary of the findings within these documents. What is the evidence for the effectiveness of needle and syringe programs in reducing HIV/AIDS in injecting drug users? The NICE review concluded that there was evidence to support the effectiveness of NSPs in reducing HIV infection among IDUs. There was evidence from 11 cost effectiveness analyses and one cost benefit analysis that, in terms of reducing HIV incidence and prevalence among IDUs, NSP are cost effective. The WHO review (which was examined within the NICE review of reviews) looked at evidence for NSP impact on HIV. Applying the Bradford Hill Causal Criteria (Hill, 1965) (and the additional criteria of cost effectiveness, absence of negative consequences, unanticipated benefits, feasibility of implementation and coverage, and special populations) as a framework to evaluate the effectiveness of needle and syringe programs in reducing HIV/AIDS in injecting drug users, the review concluded the following: There is compelling evidence that increasing the availability and utilisation of sterile injecting equipment by IDUs reduces HIV substantially There is no convincing evidence of any major unintended negative consequences Needle syringe programs are cost effective Needle syringe programs have additional and worthwhile benefits apart from reducing HIV infection among IDUs Bleach and other forms of disinfection are not supported by good evidence of effectiveness for reducing HIV infection Pharmacies and vending machines increase the availability and probable utilisation of sterile injecting equipment by IDUs (see section below on further detail regarding vending machines). Needle and syringe programs on their own are not enough to control HIV infection among IDUs Injecting paraphernalia legislation is a barrier to effective HIV control among IDUs. Note: This conclusion was made within the context of USA legislation in certain states in the USA What is the evidence for the effectiveness of needle and syringe programs in reducing HCV in injecting drug users? Author: Noel Craine, Josie Smith Date: 17/11/09 Status: Final Public Health Wales Safe, effective and cost effective interventions for IDUs and stimulant users The evidence for the effectiveness of NSP (and for other interventions) in reducing the transmission of HCV is less clear. It is now not possible, for ethical reasons, to carryout the type of intervention study that could demonstrate a causal effect of NSP on HCV incidence as NSP are already in place across the UK. The review level evidence, evaluated by the Scottish HCV action plan review, is insufficient to conclude that NSP are effective in reducing HCV incidence (Palmeteer et al, 2008). In addition there is insufficient evidence to conclude that NSP are cost effective in the prevention of HCV. In agreement with the Scottish Hepatitis C action plan review, the NICE review (NICE, 2008a) concluded that, from two systematic reviews that there was insufficient evidence to determine the impact of NSPs on HCV infection in IDUs. What is the evidence for the effectiveness of needle and syringe programs in reducing injecting risk behaviour? The NICE review (NICE, 2008a) concluded that there was evidence from one good quality and five moderate quality systematic reviews and meta-analyses that participation in NSPs reduces injecting risk behaviours in IDUs, in particular self reported sharing of needles and syringes, and frequency of injecting. The Scottish Hepatitis C Action Plan review (Palmeter et al, 2008) concluded that there is evidence to suggest that NSP are effective in reducing self reported reductions in injecting risk behaviour, this relates primarily to reductions in sharing behaviour. What is the evidence for needle and syringe programs in prison settings? With very high rates of incarceration amongst IDUs the role of prisons in addressing blood borne viral hepatitis is potentially very important. A survey of eight prisons in England and Wales suggested that hepatitis viruses were transmitted in the prison context (Weild et al, 2000). A review of research on prison based syringe exchange programs (operating in Switzerland, Germany and Spain) indicated that needle and syringe exchange in prisons is feasible and can provide benefits in the reduction of risk behaviour and the transmission of blood borne viruses (Dolan et al, 2003). Research in Scotland has revealed that HCV transmission can occur within the prison context (Champion et al, 2004). Following an HIV outbreak at HMP Glenochil in 1993, the Scottish Prison Service introduced several preventative measures to reduce transmission of blood borne viral transmission; these include bleach for sterilisation, counselling, detoxification and drug behaviour management programs (Taylor et al, 1995; Champion et al, 2004). What is the evidence for the effectiveness of needle and syringe programs in reducing the occurrence of soft tissue skin infections? As with blood borne viral transmission there has been no systematic evaluation of the impact of NSP on injection site infections. With the current distribution of NSP in the UK such an evaluation is unlikely. What is the evidence for the effectiveness of needle and syringe programs as sources of education on overdose, blood borne viral transmission, safe injecting practices and associated risk of injections? Author: Noel Craine, Josie Smith Date: 17/11/09 Status: Final Public Health Wales Safe, effective and cost effective interventions for IDUs and stimulant users NSPs should provide, in addition to clean injecting equipment; education on overdose, blood borne viral transmission, safe injecting practices and associated risk of injections. The NTA review of NSP in England in 2005 (Abdulrahim et al, 2006) reported that the majority of Drug Action Team (DATs) had at least one specialist NSP that provided face to face harm reduction advice, and referral to structured treatment. However around a half did not provide a service offering HCV or HBV testing (Abdulrahim et al, 2006). A pilot needle exchange data collection project, undertaken by NPHS in 2008, established that harm reduction information was routinely provided in the voluntary and statutory sector needle exchange services but to a far less extent in community pharmacy based outlets (NPHS, 2009). There is no research evidence to inform the effectiveness of these educational interventions as provided by NSP on blood borne viral transmission or other injection related infections. What is the evidence for the effectiveness of needle and syringe programs in the provision of hepatitis B vaccination? The effectiveness of HBV vaccination is well established. Recommendations for its use and target groups are covered in Immunisation against infectious disease (Department of Health 2006). It is clear that NSP can facilitate HBV vaccination, however the contribution of NSP to HBV vaccination has not be subject to systematic review in Wales. The NTA review of NSP in England in 2005 (Abdulrahim et al, 2006) reported wide variation in the provision of onsite HBV immunisation. What is the evidence for the effectiveness of needle and syringe programs in as a route for referral of IDUs into drug treatment services? It is rational to assume that NSP can provide a route for referral of IDUs into drug treatment services. The extent to which this occurs is unclear in the UK. NSPs are provided within pharmacy settings and also within drug treatment service settings. The pilot needle exchange data collection project (NPHS, 2009) established that signposting to specialist drug services occurred regularly in the voluntary and statutory sector needle exchange services but to a far less extent in community pharmacy based outlets. 3.1.2 Vending machines (Needle / syringe dispensing machines) What are needle and syringe dispensing machines? Needle / syringe dispensing machines (NDM) have been used since 1988 as an established part of the blood borne virus prevention in injecting drug user populations (Leicht, 1993). Syringe vending machines are NDMs where the contents are sold. The definition of NDM is broader and includes machines with free or token accessed dispensing. NDM are designed to provide 24 hour access to sterile injecting equipment (needles and syringes) and safe disposal of used equipment. There are a number of countries within Europe utilising NDM alongside more traditional needle exchange programmes. Outside of Europe NDM have been used in Australia (115 machines) and New Zealand (4 machines) (Islam et al, 2007). All forms of sterile injecting equipment distribution have the potential to increase the amount of discarded needles and syringes, however, drug related litter prevention is addressed by the placing of Author: Noel Craine, Josie Smith Date: 17/11/09 Status: Final Public Health Wales Safe, effective and cost effective interventions for IDUs and stimulant users a disposal bin in the close vicinity of the vending machine. There is currently a vending machine in operation in Southampton. What are the potential health benefits of needle and syringe dispensing machines? NDM are designed to support, not replace, existing pharmacy or drug service based needle exchanges services. NDM are designed for use by all injecting individuals including those who do not, or will not, access pharmacy or drug service based needle exchange services. The reasons for this may include: young age; being responsible for children, early on in injecting career; unwillingness to identify themselves as part of an injecting community, inject infrequently; fear of breach of confidentiality by needle exchange staff. NDM can also provide sterile injecting equipment in locations where it is not feasible to provide pharmacy or drug service needle exchange provision. What is the evidence for the effectiveness of needle and syringe dispensing machines? Measuring the impact of NDM on the transmission of blood borne viruses is, for logistic and ethical reasons, unlikely to be achieved in the short term. NDM are generally introduced as part of a package of interventions (e.g. pharmacy based needle exchange, methadone programs etc) aimed at reducing drug related harm. Disease incidence studies with sufficient power to measure the impact of interventions on the transmission of blood borne viruses amongst drug injectors are by nature large and thus costly. Separating out the effects of individual components of an intervention and controlling for confounding effects in studies of disease incidence is a major challenge. The majority of published research on the efficacy of NDM is therefore limited to evaluations of temporal and spatial levels of use, perceptions of NDM, potential problems e.g. safe disposal of used equipment associated with NDM, and cost effectiveness. Two key review documents have examined the evidence base for NDM; In 2004 a World Health Organisation Evidence for Action Technical Paper addressed NDM within a wider appraisal of the effectiveness of sterile needle and syringe programming in reducing HIV/AIDS among injecting drug users (WHO, 2004) and Islam and Conigrave (2007) examined the advantages and disadvantages of syringe vending machines in light of available evidence. The WHO report (WHO, 2004) examined the wider effectiveness of the sale of needles and syringes from pharmacies and vending machines in preventing HIV infection among IDUs. The report examined nine studies that looked at the effect of pharmacy sales and syringe vending machines on risk outcomes and HIV sero-prevalence among IDUs and concluded that there was sufficient evidence to fulfil: strength of association replication of findings specificity of association temporal sequence biological plausibility coherence of evidence reasoning by analogy cost effectiveness Author: Noel Craine, Josie Smith Date: 17/11/09 Status: Final Public Health Wales Safe, effective and cost effective interventions for IDUs and stimulant users absence of negative consequences feasibility of implementation expansion and coverage special populations However there was insufficient evidence to fulfil: biological gradient experimental evidence unanticipated benefits No indeterminate or negative studies were identified for either pharmacy sales or vending machines. Whilst the application of the criteria was to the wider effectiveness of the sale of needles and syringes from pharmacies and vending machines the report identified that: a) syringe vending machines can provide 24 hour availability and improve access in locations that are difficult to serve b) the introduction of vending machines in an open prison in Hamburg resulted in a significant reduction in needle sharing c) no evidence was found that increased pharmacy sales or vending machines have caused non-IDUs to become users d) primary users of vending machines were more likely to be younger, less likely to be in drug maintenance treatment and less likely to share needles and syringes (Obadia et al, 1999). The literature and international experience of syringe vending machines was reviewed by Islam and Conigrave (2007). This review identified a number of advantages and disadvantages associated with this intervention. The advantages cited were: a) Off peak and increased after-hour access to sterile injecting equipment that matches patterns of drug use and availability b) Increasing geographic reach; reducing the distance between IDU and sterile equipment c) Access in areas where it is not possible to establish staffed outlets d) Non-stigmatised access to sterile equipment and access for individuals who do not wish to be ‘seen as IDUs’ e) Anonymity, privacy and confidentiality Machines have also been used within prisons in Germany and Switzerland. Research from France reported that users of machines reported less sharing of syringes in the previous six months than users of pharmacies, and a little more than users of staffed needle exchanges (Moatti et al, 2001). However machine users reported reduced sharing of paraphernalia compared to pharmacy users. (Note: without randomised control trials such data is, due to potential confounding, difficult to interpret). The main disadvantage cited by the review was that vending machines keep injecting drug users away from important health contact. This lack of contact Author: Noel Craine, Josie Smith Date: 17/11/09 Status: Final Public Health Wales Safe, effective and cost effective interventions for IDUs and stimulant users potentially deprives injectors of information, education and communication. Staffed exchanges can be the first point of contact for health services with some injectors facilitating access into treatment and for the most vulnerable contact with primary health care. This issue may be overcome if distribution of tokens for the vending machines is facilitated by substance misuse or health services. What evidence exists for the cost effectiveness of needle and syringe dispensing machines? There is no evidence to inform estimates of the cost effectiveness of vending machines. The potential impact of needle and syringe exchange is limited by the access and attractiveness of these services to potential clients; vending machines can increase this access to a broader range of IDUs and extend the time when sterile equipment is available. They can offer anonymous and confidential provision. Vending machines however do not offer contact between IDU and health staff. They potentially have a role to supplement NSP provision in specific circumstances but should not replace NSP. NDM could provide clean equipment to steroid injectors; steroid use is on the increase in Wales, many steroid users do not wish to access drug services and exchanges aimed at opiate and stimulant injectors. Any NDM should be accompanied by tamper proof needle and syringe disposal facilities. Realistic objectives should be set for the evaluation of any NDM introduced in Wales. 3.1.3 Drug consumption rooms What are drug consumption rooms? Drug consumption rooms (DCRs, also known as supervised injecting rooms or medically supervised injecting centres) are legally sanctioned facilities that allow injecting drug users to self-administer illicit drugs in an environment that can support a reduction in the risk of blood borne viral transmission, injection site infections, drug overdose and public order concerns. These facilities have trained medical personnel present at all times to supervise, but physically not assist, injectors. There were, as of 2006, approximately 65 DCRs in operation in eight countries around the world but there are none in the UK. An independent working group, set up by the Joseph Rowntree Foundation, examined the evidence for the development of DCRs in the UK. The group concluded that DCRs offered ‘a unique and promising way to work with the most problematic users – to reduce the risk of overdose, improve their health and lessen the costs to society…’ and recommended the piloting and evaluation of DCRs in the UK (Independent Working Group, 2006). Guidance on standards for the establishment and operation of DCRs in the UK has recently been published outlining and addressing the legal issues (Hunt, 2008). A review of the evidence of primary prevention interventions for HCV among IDUs found only one evaluation of a DCR that studied anti-HCV seroconversion as an outcome. Overall the review concluded that it was plausible that DCR could contribute to a reduced incidence of HCV (Wright and Tompkins, 2006). Author: Noel Craine, Josie Smith Date: 17/11/09 Status: Final Public Health Wales Safe, effective and cost effective interventions for IDUs and stimulant users 3.1.4 Provision of harm reduction and safe injecting information What information on harm reduction and safe injecting is offered and what formats have been evaluated? Information on harm reduction and safe injecting is currently offered in a range of settings across Wales. The manner in which this information is provided, both verbal, written or visual (DVD/film) will vary across the country from general provision of information to structured intervention. To our knowledge the impact of this information upon disease transmission, risk behaviour or client knowledge has not been systematically evaluated. Despite these limitations, high quality and up to date information should be provided within the full range of health care settings where there is contact with potential, current or ex drug users. There is no review level evidence for the cost effectiveness of the general, unstructured provision of information on harm reduction and safe injecting. Brief behavioural interventions (BBIs) are a potential means to facilitate behaviour change within the area of substance misuse. BBIs have been shown to have a role in preventing HIV (Fishbein, 2000). A recent study from Australia compared a BBI for reducing hepatitis C risk practices among injecting drug users to a standardised educational intervention (Tucker et al, 2004). The study reported that both the intervention and control group reported significant reductions in risk behaviour however the brief intervention did not show evidence of being more effective. The range of interventions that can be considered as BBI is extensive; likewise the potential targets for intervention, for example reduction of risk behaviour, reduction of viral transmission, reduction in injecting frequency etc. Evaluations of BBI as an approach to risk reduction require research to determine both efficacy and effectiveness. Peer delivered interventions can potentially play a role in risk reduction (Aitken et al, 2002). However further evaluation is needed on how such interventions can best be delivered to reduce disease incidence. Hepatitis B vaccination is a key intervention in reducing the direct and indirect harms associated with injecting drug use. Recommendations for its use and target groups are covered in Immunisation against infectious disease (DoH, 2006). Injecting drug users should be vaccinated against HBV and vaccination should be prioritised by all substance misuse services including prison health care services. Evidence from NPHS research with injecting drug users in Wales indicated that of a sample of 700 current IDUs, 71% had been in prison on at least one occasion and that the majority of IDUs had received HBV vaccination within the prison setting (NPHS, 2006). In addition research from Scotland demonstrated the potential increase in uptake of HBV vaccination that can be achieved with a prison based vaccine program; with prison vaccination contributing significantly to coverage measured in community settings (Hutchinson et al, 2004). 3.1.5 Blood borne virus management Author: Noel Craine, Josie Smith Date: 17/11/09 Status: Final Public Health Wales Safe, effective and cost effective interventions for IDUs and stimulant users The management of chronic hepatitis B, hepatitis C and HIV should be carried out by specialist clinicians (gastroenterologists, hepatologists and infectious disease specialists) and primary care. Guidelines for treatment of chronic HBV infection have been issued by the NICE. NICE has made recommendations for the use of adefovir dipivoxil and peginterferon alfa-2a to treat chronic hepatitis B (NICE, 2006b). These recommendations do not apply to people who are also infected with hepatitis C or D, or HIV. More recently Entecavir has been approved for treatment of Hepatitis B (NICE, 2008b). The effectiveness of HBV vaccination is also well established for HBV prevention in those infected with hepatitis C and HIV NICE guidelines support the use of combination therapy for treatment of HCV positive individuals with mild, moderate or severe liver disease, patients may require ongoing support throughout the treatment process (NICE, 2006a). Changes in lifestyle, in particular in relation to alcohol consumption can have a major impact on disease progression. Treatment of acute infection is in the UK relatively uncommon, acute infections are largely asymptomatic and with current levels of diagnostic infections many acute infections will be missed. With improvements in diagnosis of infection, possible with the adoption of dried blood spot testing across Wales it is likely that more acute infections may be detected. A recent review of treatment of acute HCV infection (Wiegand et al, 2008) concluded that acute HCV can be successfully treated and highlighted the need for further research into this important area. HIV treatment can be managed by Highly Active Anti Retroviral Treatment (HAART) within specialist clinical settings. Diagnostic testing is an essential step on the pathway to treatment. Research in South Wales showed that testing rates amongst IDUs was low (NPHS, 2006) A pilot study in North West Wales has demonstrated the effectiveness of dried blood spot testing as an alternative to venepuncture testing amongst IDUs (DBS is much easier among individuals with poor vein access) (Craine et al, 2008). In the study there was an approximately seven fold increase in testing by DBS when compared to venepuncture testing in the previous year. Recent research from Ireland reported that structured clinical guidance for GPs increased screening for HCV (Cullen et al 2006). There is little evidence in the UK for the effectiveness or otherwise for awareness raising among those who may have in the past put themselves at risk of blood borne viral hepatitis infection. However, a recent Health Technology Assessment (Castelnuovo et al, 2006) concluded that: a) Case finding for hepatitis C in former injecting drug users is likely to be considered cost-effective by NHS commissioners b) Improvements in treatment would improve cost effectiveness c) Case finding is likely to be most effective when targeted at people with more advanced HCV disease Screening for HCV in the prison setting is possible, however early evaluation of a screening project in HMP Dartmoor reported low uptake of screening and a high attrition rate through the screening process (Horne et al, 2004). Research Author: Noel Craine, Josie Smith Date: 17/11/09 Status: Final Public Health Wales Safe, effective and cost effective interventions for IDUs and stimulant users into optimising both screening of prisoners and subsequent follow-up of infected individuals is urgently needed. Screening of pregnant women is routinely undertaken for HIV and HBV however testing for HCV is currently by consent. 3.1.6 Provision of injecting related health care; bacterial infections, vein damage and deep vein thromboses Injecting drug use carries with it the risk of blood borne viral transmission via sharing of contaminated equipment as addressed in previous sections, and problems associated with bacterial infections, vein damage and deep vein thromboses (DVTs). Wound care for bacterial infections may be addressed, depending on the severity of the problem, within a range of health care settings ranging from acute hospital settings for severe manifestations through to clinics within drug services for more straight forward cases. DVTs will require attention within acute hospital settings. The extent to which drug services can address the problems associated with injecting will reflect the clinical resources available to services. Services must however be able to spot serious problems and rapidly refer individuals to specialist services for treatment. We are aware of no systematic evaluation of interventions aimed at bacterial infections, vein damage and deep vein thromboses within a UK context. Author: Noel Craine, Josie Smith Date: 17/11/09 Status: Final Public Health Wales Safe, effective and cost effective interventions for IDUs and stimulant users 3.2 Assess the range of safe, effective and cost effective interventions to meet the needs of stimulant users (including cocaine, crack, amphetamine and methamphetamine) 3.2.1 Interventions to meet the needs of stimulant users What interventions are indicated for the treatment of stimulant users? There is only limited research data on the efficacy of treatment interventions for the treatment of stimulant users. Nonetheless drug services are faced increasingly with the challenge of providing treatment for stimulant use amongst individuals both with and without opiate dependency. Crack use: The most detailed evaluation currently available to guide the treatment of crack cocaine use in the UK context is the NTA and DoH National Evaluation of Crack Cocaine Treatment and Outcomes (NECTOS) study (Weaver et al, 2007). This study drew on the experiences of services providing specialist interventions for crack cocaine use in the UK. This evaluation concluded that specialist crack treatment services are relatively new and do not have an established evidence base. The report identified a need to implement and evaluate promising interventions that are appropriate to crack and stimulant use in the context of opiate substitution therapy. In the absence of a wide research evidence base the development of specialist services should continue on the basis of emerging best practice. A further recent study evaluated the implementation of the Crack Treatment Delivery Model (CTDM) across 11 cities and 13 services in England (Arnull et al, 2007). This model was developed by the NTA as part of the response to the National Crack Action Plan (NTA, 2002). The model was designed in line with NTA models of care and Drug and Alcohol National Standards (DANOS). The CTDM aimed to disseminate best practice in the engagement, retention and treatment of crack users and involved; training for managers and staff; a manual of practice materials; guidance about service specifications; other frameworks for service delivery; two days consultancy support for each site. The study concluded that: a) Services adapted existing resources to their needs b) Staff who adopted and adapted materials were most positive about the pilot c) Managers and stakeholders were less engaged d) The appropriateness of the service was important to users (particularly women and those from BME groups) e) Service users placed importance upon fast access to treatment The implications of the findings were that appropriate treatment can help reduce high levels of crack use and for those in treatment there are quantifiable health benefits. The CDTM is elaborated in detail within the evaluation report (Arnull et al, 2007). The NTA produce a resource pack for treatment providers on treating crack and cocaine use (NTA, 2003). Author: Noel Craine, Josie Smith Date: 17/11/09 Status: Final Public Health Wales Safe, effective and cost effective interventions for IDUs and stimulant users 3.2.2 Substitute prescribing Substitute prescribing for stimulant, primarily amphetamine, use is a contentious procedure (Gossop, 2006a); limited evidence exists as to its effectiveness. Research has suggested that dexamphetamine prescribing may influence drug use and increase treatment contact and retention (McBride et al, 1997; Shearer et al, 2001). It has been suggested that treatment should be time limited and restricted to heavy and problematic primary stimulant users (Flemming, 1998). Although amphetamine prescribing occurs, research is needed to robustly evaluate its effectiveness. 3.2.3 Residential Rehabilitation One USA study reported limited evidence for the impact of residential programs on crack users who had no pressing reason to enter residential as opposed to non-residential rehabilitation (e.g. lacked housing). The study found that intensive day programs matched outcomes from residential rehabilitation at a potentially lower cost (Greenwood, 2001). In addition, there is some evidence to suggests benefits from residential rehabilitation in the treatment of cocaine dependence (Hubbard et al, 1997). Evidence for the effectiveness of residential rehabilitation specific to stimulant dependence within the UK context is required. 3.2.4 Contingency management Contingency management (CM) interventions offer tangible reinforcements to individuals in treatment for substance misuse who abstain from using drugs or who meet other objectively determined goals (Sindelar et al, 2007). One example of CM is the provision of vouchers for retail goods given in return for the production of drug-free urine samples. The majority of research on CM has been carried out in the USA, the roll of CM in the UK drug treatment context has not been subjected to the same degree of attention. Recent research from the USA suggests that CM treatment is associated with a reduction in HIV risk behaviour, especially injecting risk behaviour in cocaine using patients on methadone maintenance treatment (Hanson et al, 2008). The primary beneficial effects reported were apparent three months after CM ended. Similarly, recent research suggests CM that may be beneficially in the treatment of methamphetamine, however CM should be a component of a wider treatment package and not a treatment offered alone (Roll, 2007). There is no trial level evaluation for the impact of CM on amphetamine use. In evaluating the impact of CM on stimulant use there are a number of variables that may impact on the effectiveness, and cost effectiveness, (Sindelar, 2007; Petry et al, 2004), with the magnitude of the reinforcement influencing the outcome (Higgins et al, 2007a). A meta-analysis of CM for treatment of substance misuse disorders carried out in 2006 (Prendergast et al, 2006) concluded that CM was among the more effective approaches in promoting abstinence during the treatment of substance use disorders. CM was seen to improve the ability of clients to remain abstinent thus improving use of other clinical interventions. Author: Noel Craine, Josie Smith Date: 17/11/09 Status: Final Public Health Wales Safe, effective and cost effective interventions for IDUs and stimulant users Note: A text book examining in detail contingency management (Contingency Management in Substance Misuse Treatment) has been recently published (Higgins et al, 2007b). In addition Contingency management has been reviewed by Gossop (2006). 3.2.5 Psychosocial interventions and brief interventions In a review of evidence of effective treatment for cocaine and crack dependence, the NTA (2002) concluded that: Drug free psychosocial interventions such as counselling, provided on a non-residential basis are the most cost effective option for clients with few complicating problems There is little understanding of how to prompt initial contact with treatment services. Once made, rapid intake, proactive reminders and practical help improve treatment uptake. Empathy and understanding amongst key workers is important in retention and outcomes Recognised psychotherapies delivered by professional psychologists perform no better that well structured drug counselling Cognitive behavioural approaches have an evidence base to support them and group therapy may be as effective as individual therapy Intensive residential rehabilitation may be appropriate for the most complex cases The range of psychosocial interventions and brief interventions summarised below are reviewed in greater detail in the NTA publication ‘Treating drug misuse problems: evidence of effectiveness’ (Gossop, 2006) from which much of this summary on psychosocial interventions is drawn. Methodologically conducting research on psychosocial interventions can be challenging; interventions may have more than one component and may be provided alongside other treatments (e.g. substitution treatments) it may also be difficult to control for the quality of the intervention and skills of practitioners providing interventions. Motivational Interviewing (MI): Research has suggested that MI can be beneficial within the context of drug use; a recent meta-analysis found that MI frequently improved outcomes both as a stand alone treatment and as an adjunct to other treatment (Hettema et al, 2005). However improved outcomes were not consistently seen and effectiveness was variable. Research specific to cocaine-dependent outpatients with depression and to amphetamine users suggested benefits from MI (Daley et al, 1998; Baker et al, 2001) Cue exposure: Evidence for the effectiveness of cue exposure treatments for drug dependence is lacking (Conklin and Tiffany, 2002; Gossop, 2006). Relapse prevention: Relapse prevention (RP) aims to prevent lapses into drug use after abstinence using a range of techniques that include cognitive and behavioural interventions. A review of controlled trials concluded that there is some support for relapse prevention in the treatment of drug dependence (Carroll, 1996). Outcomes may be influenced by participant preference and by underlying psychological distress of patients (Brown, 2002). A study comparing Author: Noel Craine, Josie Smith Date: 17/11/09 Status: Final Public Health Wales Safe, effective and cost effective interventions for IDUs and stimulant users group vs. individual treatments in outcomes amongst cocaine dependent patients reported no difference between the groups with improvements in addiction severity, craving and coping behaviours reported for both individual and group treatments, however RP was no more effective than other active treatments (Schmitz, 1997; Gossop, 2006). 12 step programs: 12 step programs as used by narcotics anonymous and alcoholics anonymous within the context of group treatment are based on an abstinence model. There has been little systematic evaluation of the effectiveness of 12 step treatments. However existing research suggests that such approaches may be effective for cocaine dependence (Weiss et al, 2005). Brief interventions: Recent research from Australia has reported benefits in terms of amphetamine abstinence after brief cognitive behavioural intervention with regular amphetamine users (Baker, 2001). Evidence for the effectiveness of brief cognitive behavioural interventions specific to stimulant dependence within the UK context is needed. Acupuncture: A systematic review concluded that there is no evidence to support the use of acupuncture to treat cocaine dependence (Mills et al, 2005). 3.2.6 Provision of equipment used in the consumption of stimulants The provision of safe injecting equipment for the injection of stimulants is supported by the evidence presented in section 3.1 on NSP. However in addition to injection, stimulants may be taken by snorting, smoking and ingesting orally. A recent review of non-injection drug use and hepatitis C infection identified gaps in research and concluded that the causal pathway to infection remained unclear (Scheinmann et al, 2007). Preliminary research has demonstrated the presence of HCV viral RNA on a used crack pipe collected from one of 51 street collected crack pipes, indicating the theoretical possibility of HCV transmission from crack pipes (Fisher, 2008). Providing crack users with pipes to prevent HCV transmission has been suggested, however we know of no robust evaluation of the intervention in terms of reduction of the risk of blood borne viral transmission. Similarly the virological plausibility of intranasal transmission has been suggested by the finding that blood and HCV RNA present in the nasal secretions and drugsniffing implements of HCV-infected intranasal drug users recruited in New York City (Aaron et al, 2008). The epidemiological significance of these findings remains unknown. Provision of equipment for the consumption of stimulants is not backed up by robust research evidence on the impact of the intervention on disease transmission. However, arguably such interventions may improve engagement in services. Properly evaluated studies with clearly defined outcome measures are required. Author: Noel Craine, Josie Smith Date: 17/11/09 Status: Final Public Health Wales Safe, effective and cost effective interventions for IDUs and stimulant users 3.3 Evaluation of the range of safe, effective and cost effective interventions targeted at reducing overdoses and drug related deaths The interventions discussed below require multi-agency partnership and joint working practices to be effectively addressed and the challenges sit beyond the boundaries of any one organisation. For more detailed analysis of these issues readers are directed to a very thorough and recent review of the literature on reducing drug users’ risk of overdose produced by the Scottish Government which highlights recommendations to reduce drug related death (Rome et al, 2008). Reduction in overdose death: The primary cause of illicit drug use related overdose death in the UK is due to respiratory suppression in heroin (or other opiate) overdose. This may be in combination with alcohol and benzodiazepines. Risk of overdose is increased amongst individuals with reduced or low tolerance to opiates, e.g. after a period of detoxification due to rehabilitation or imprisonment, and patients in the first few weeks of methadone substitution (Strang, 2006). The UK Advisory Council on the Misuse of Drugs (ACMD) published a report drawing on international evidence and highlighting the increase in drug related death seen in the UK (ACMD, 2000). The report concludes that the primary means to reduce overdose are: Engendering behaviour change around the risk behaviours that lead to overdose; this includes education around risks and more broadly, high standard and appropriately dosed drug treatment that ensures tolerance to opiates is maintained and that reduces injecting drug use. Responses and interventions to reduce the mortality rate associated with overdose once it has occurred; such as education around the appropriate responses when an overdose is witnessed, training in resuscitation techniques, local agreements with police to encourage witnesses to call an ambulance and, potentially the provision of naloxone to reverse the effects of opiate overdose. Information dissemination via public health alerts to significant changes within drug supply that may influence overdose and to outbreaks of highly pathogenic bacterial infections. Potentially by providing safe environments for drug use by individuals vulnerable to overdose for example via safe injecting facilities (see section on drug consumption rooms above). 3.3.1 Provision of education and information relating to overdose Education for drug users targeting overdose can influence both self preservation and mutual preservation (Best et al, 2001). The DoH have provided detailed guidance for drug action teams in England on providing resuscitation training for drug users (Gillies, 2002). This guidance highlights the importance of targeting all drug users, but especially those at most risk of overdose. These include people leaving prison, detoxification or residential rehabilitation, homeless people and those not in contact with mainstream Author: Noel Craine, Josie Smith Date: 17/11/09 Status: Final Public Health Wales Safe, effective and cost effective interventions for IDUs and stimulant users services. In addition poly drug users and homeless users are at increased risk and long term users may become complacent about the risks. Individuals on opiate substitution should also be targeted. Health care staff with contact with drug users should also be trained. The guidance recommends that in each area at least 12 sessions a year should be held. The aim of training should provide participants with the necessary basic knowledge and skills to respond effectively, appropriately and confidently to a drugs overdose. Encouraging witnesses to stay with the casualty until medical help arrives is important; remaining with a casualty may help prevent choking or provide sensory stimulation influencing the progression of the overdose (Best et al, 2002). Administration of CPR has been associated with improved clinical outcomes in overdose (Dietze et al, 2002). Such interventions are more likely when witnesses have received information on how to prevent or revive a casualty (Pollini, 2006). A number of areas in the UK have engaged in projects addressing overdose risk: The Scottish Government has funded a critical incidents national training officer to provide initiatives directed at overdose; in Greater Manchester the North West Ambulance Service has been involved in training (Rome et al, 2008), in Merseyside a multi-component campaign using social marketing to reduce overdose was commissioned by local police, ambulance, the NHS and DAATs. The project ‘Lifeguard: Act Fast Save a Life’ involved local capacity building, a mass media campaign and training for professionals and drug users (HIT, 2009) 3.3.2 Prevention of overdose post-release from prison services Drug users leaving prison services are at an elevated risk of overdose due to relapse to opiate use following a loss of tolerance (Darke et al, 1996; Seaman et al, 1998; Neale, 2000). The period immediately following release provides an opportunity for interventions to reduce risk. Education around overdose risks, and rapid admission into specialist drug treatment services for individuals who are likely to relapse into opiate use upon release is important. This requires substantial resources and proactive communication between prisonbased health care, CARAT services and drug misuse services in the community to meet the scale of need presented by opiate users in Wales. 3.3.3 Identification and intervention of those at risk of suicide via overdose Deliberate overdoses among heroin users are difficult to distinguish from accidents (Farrell et al, 1996). Among drug using populations the prevalence of underlying mental health problems and feeling of hopelessness that may be associated with overdose (ACMD, 2000; Farrell et al, 1998; Best et al, 2001). Best and colleagues reviewed a range of evidence on non-accidental overdose and concluded that substance misusers prone to suicide tend to enter treatment, whilst in treatment the risk is modestly reduced and that dropping out or being thrown out of treatment restores high risk (Best et al, 2001). 3.3.4 Provision of Naloxone Author: Noel Craine, Josie Smith Date: 17/11/09 Status: Final Public Health Wales Safe, effective and cost effective interventions for IDUs and stimulant users There have been calls, from leading researchers and clinicians in the UK, to roll out and evaluate the impact of the provision of ‘take home’ naloxone for opiate users on opiate overdose death (Strang, 2006). Naloxone is a safe and effective opiate antagonist that rapidly reverses the respiratory suppression of heroin overdose. Early anecdotal evidence from the USA suggests that naloxone offers a potential benefit in risk reduction relating to opiate overdose (Strang, 2006). Whilst there is a persuasive argument for making naloxone widely available and ‘take home’ there has from some quarters been a call for caution (Ashworth, 2006). Recent UK research has provided support for the provision of overdose training and ‘take home’ naloxone (Strang et al, 2008). The research concluded that overdose management training, which included ‘take home’ naloxone, may reduce drug related deaths. Further research is urgently needed to evaluate the impact of a widespread roll out of this intervention. Several ‘take home’ naloxone pilots have taken place in England and in Scotland (Rome et al, 2008); initial results from a Lanarkshire pilot and a Glasgow pilot show naloxone has been appropriately used. In England, Salford DAT, Wiltshire DAAT and North West Ambulance Service have been involved in trials. Formal evaluation of these trials is to our knowledge yet to be published. Naloxone demonstration trials are to be undertaken in Wales from April 2009. There is a planned trial funded by the Medical Research Council to examine the effectiveness of providing naloxone on release from prison to prevent heroin-related overdose; the trial should start in late 2008. 3.3.5 Overdose and stimulant drug use The epidemiology of drug related death due to stimulant use is poorly described. There has been a suggestion that cocaine use by injecting drug users may be associated with an increased risk of non-fatal opioid overdose although a causal link has not been demonstrated (Oliver et al, 2007; Taylor et al, 1996; Ochoa et al, 2003). A quantitative evaluation of cocaine, crack cocaine and amphetamine use in relation to drug related death in the UK would provide valuable evidence in this area. 3.3.6 Drug treatment and overdose The role of opiate substitution treatment in reducing drug related death is well established (Ward et al, 1999). Substitution treatment can prevent the loss of tolerance to opiates within patients who are likely to relapse into opiate use after periods of reduced tolerance. Engaging drug users in treatment saves lives, however treatment must be high quality and tailored to patient need with careful consideration of tolerance. Drug treatment has been addressed elsewhere in detail (Gossop, 2006). 3.3.7 Overdose and antidepressant and benzodiazepine prescribing Author: Noel Craine, Josie Smith Date: 17/11/09 Status: Final Public Health Wales Safe, effective and cost effective interventions for IDUs and stimulant users Opiate users who are prescribed benzodiapines are at elevated risk of overdose due to the respiratory depressive effects of both substances (Best et al, 2001) and as such caution and patient education is required. Antidepressant prescribing, in particular tricyclic antidepressants, may influence risk of fatal opiate overdose (Best et al, 2001; Darke et al, 2000). 3.3.8 Local arrangements between police and ambulance arrangements Concerns of police involvement in overdose related to illicit drugs may be in certain instances a disincentive to the calling of an ambulance to a drug overdose (Tobin et al, 2005). In response to this problem some UK police forces areas have been involved in developing protocols regarding police attendance at overdose incidence. For example the Greater Manchester Police in 2002 implemented what has been termed the ‘Manchester Protocol’ for the attendance of police at overdose. The Greater Manchester Police supported the Greater Manchester Ambulance Service in their policy of not notifying the police of potential drug overdose incidents unless there were exceptional circumstances. This policy was designed to reduce the number of drug related deaths by encouraging overdose casualties to access emergency treatment without fear of police attendance (Chief Constable’s Order, 2002/04). Where fatalities occur, all drug related deaths are subject to a Coroner’s inquest and must be fully investigated (GMP, 2003). Likewise, Nottinghamshire Police and the East Midlands Ambulance Service and local DAATs have set up arrangements, similar protocols have been established in Kirklees, Leicestershire, and Avon and Somerset (Rome et al, 2008). These schemes have to our knowledge yet to be formally evaluated. 3.3.9 Accident and Emergency department follow-up Data on overdose admission to accident and emergency department show high levels of recidivism amongst vulnerable individuals (Best et al, 2001; Ryan, 2000; Ghodse et al, 1986). This environment thus presents an opportunity for intervention, for example education and referral to specialist services, for those vulnerable individuals who are repeatedly overdosing and attending A & E services. WAG are currently commissioning research in Wales on near misses or non-fatal overdoses including a literature review and meta-analysis of such interventions 3.3.10 Information dissemination via public health alerts Providing accurate, rapid and well-disseminated information to at-risk populations in relation to changes in drug composition that are likely to impact upon overdose risk is vital in reducing overdose and outbreaks of highly pathogenic bacterial infections. A greater understanding is needed of how best messages concerning drug composition should be provided (Rome et al, 2008). Author: Noel Craine, Josie Smith Date: 17/11/09 Status: Final National Public Health Service for Wales Safe, effective and cost effective interventions for IDUs and stimulant users References Abdulrahim D et al. (2006). Findings of a survey of needle exchanges in England. London: National Treatment Agency. Available at: http://www.nta.nhs.uk/publications/documents/nta_nes1_needle_exchange_survey.pdf [Accessed 13th Feb 2009] Advisory Council on the Misuse of Drugs. (2000). Reducing drug related deaths. London: The Stationery Office; 2000 Aitken CK, Kerger M and Crofts N. (2002). Peer-delivered hepatitis C testing and counselling: a means of improving the health of injecting drug users. Drug Alcohol Rev 21: pp.33-37 Ashworth AJ. (2006). Emergency naloxone for heroin overdose: beware of naloxone's other characteristics. BMJ 333: p.754 Arnull E et al. (2007). An evaluation of the crack treatment delivery model. Available at: http://www.nta.nhs.uk/publications/documents/nta_an_evaluation_of_the_crack_treatment_d elivery_model.pdf [Accessed 13th Feb 2009] Baker A, Boggs T and Lewin T. (2001). Randomised controlled trial of brief cognitivebehavioural interventions among regular users of amphetamine. Addiction 96: pp.1279-87 Best D et al. (2002). Peer overdose resuscitation: multiple intervention strategies and time to response by drug users who witness overdose. Drug Alcohol Rev 21: pp. 269-74 Best D et al. (2001). Overdosing on opiates. Drug and Alcohol Findings 5: pp.5-18 Brown TG et al. (2002). Process and outcome changes with relapse prevention versus 12Step aftercare programs for substance abusers. Addiction 97: pp.677-89 Campbell A et al. (2007). The international treatment effectiveness project. Implementing psychosocial interventions for adult drug misusers. London: The National Treatment Agency for Substance Misuse. Available at: http://www.nta.nhs.uk/publications/documents/nta_itep_implementing_psychosocial_interven tions_for_adult_drug_misusers_rb34.pdf [Accessed 13th Feb 2009] Carroll KM. (1996). Relapse prevention as a psychosocial treatment approach: A review of controlled clinical trials. J Consult Clin Psychol 4: pp.46-54 Castelnuovo E et al. (2006). The cost-effectiveness of testing for hepatitis C in former injecting drug users. Health Technol Assess 10 (32) Champion JK et al. (2004). Incidence of hepatitis C virus Infection and associated risk factors among Scottish prison inmates. Am J Epidemiol 159: pp.514-9 Conklin C and Tiffany S. (2002). Applying extinction research and theory to cue exposure addiction treatments. Addiction 97:pp.155- 67 Craine N et al. (2008). Improving blood-borne viral diagnosis; clinical audit of the uptake of dried blood spot testing offered by a substance misuse service. J Viral Hepat 16: pp.219-22 Cullen W et al. (2006). Hepatitis C infection among injecting drug users in general practice: a cluster randomised controlled trial of clinical guidelines’ implementation. Br J Gen Pract 56: pp.848-56 Daley D et al. (1988). Increasing treatment adherence among outpatients with cocaine dependence: results of a pilot study. Am J Psychiatry 155: pp. 1611-13 Darke S, Ross J and Hall W. (1996). Overdose among heroin users in Sydney, Australia: Prevalence and correlates of non-fatal overdose. Addiction 91(3): pp.405-11 Author: Noel Craine Version: 0c Date: 23/02/09 Page: 27 of 32 Status: Draft Intended Audience: APoSM National Public Health Service for Wales Safe, effective and cost effective interventions for IDUs and stimulant users Darke S and Ross J. (2000). The use of antidepressants among injecting drug users in Sydney Australia. Addiction 95(3): pp.407-17 Department of Health. (1999). Drug misuse and dependence: guidelines on clinical management . London: DoH. Available at: http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidan ce/DH_4009665 [Accessed 13th Feb 2009] Department of Health. (2006). Immunisation against infectious disease 2006. The Green Book. London: DH. Available at: http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidan ce/DH_079917 [Accessed 13th Feb 2009] Dietze P, Cantwell K and Burgess S. (2002). Bystander resuscitation attempts at heroin overdose: does it improve outcomes? Drug Alcohol Depend 67: pp.213-18 Dolan K, Rutter S and Wodak AD. (2003). Prison-based syringe exchange programmes: a review of international research and development. Addiction 98: pp.153-58 Farrell M et al. (1996). Suicide and overdose among opiate addicts. Addiction 91: pp.321-23 Farrell M et al. (1998). Substance misuse and psychiatric comorbidity: an overview of the OPCS national psychiatric morbidity survey. Addict Behav 23: pp.909-18 Fishbein M. (2000). The role of theory in HIV prevention. AIDS Care 12: pp.273-8 Fischer B et al. (2008). Hepatitis C virus transmission among oral crack users: viral detection on crack paraphernalia. Eur J Gastroenterol Hepatol 20: pp.29-32 Flemming P. (1998). Prescribing amphetamine to amphetamine users as a harm reduction measure. International Journal of Drug Policy 9: pp.339-44 Ghodse H et al. (1986). A comparison of drug-related problems in London accident and emergency departments 1975-1982. Br J Psychiatry 148: pp.658-62 Gillies C. (2002). Preventing overdose. Guidance for drug action teams on providing resuscitation training for drug users. London: DoH. Available at: http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidan ce/DH_4007051 [Accessed 13th Feb 2009] Gossop M, Marsden J and Stewart D. (2001). NTORS after five years (National Treatment Outcome Research Study): Changes in substance use, health and criminal behaviour in the five years after intake. London: National Addiction centre. Available at: http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidan ce/DH_4084908 [Accessed 13th Feb 2009] Gossop M. (2006). Treating drug misuse problems: evidence of effectiveness. London: National Addiction Centre. Available at: http://www.nta.nhs.uk/publications/documents/nta_treat_drug_misuse_evidence_effectivenes s_2006_rb5.pdf [Accessed 13th Feb 2009] Greenwood GL. 2001. Relapse outcomes in a randomised trial of residential and day drug abuse treatment. Journal of Substance Abuse Treatment 20: pp.15-23 Greater Manchester Police. (2003). Drug strategy. Available at: http://www.gmp.police.uk/mainsite/0/6F868640E1096CAC80257104004281D4/$file/DrugsStr ategyopt.pdf [Accessed 13th Feb 2009] Hanson T et al. (2008). Contingency management reduces drug-related human immunodeficiency virus risk behaviors in cocaine-abusing methadone patients. Addiction 103: pp.1187-97 Author: Noel Craine Version: 0c Date: 23/02/09 Page: 28 of 32 Status: Draft Intended Audience: APoSM National Public Health Service for Wales Safe, effective and cost effective interventions for IDUs and stimulant users Hettema JE et al. (2005). Motivational interviewing. Annu Rev Clin Psychol 1: pp.91-111 Higgins S et al. (2007a). Effects of varying the monetary value of voucher-based incentives on abstinence achieved during and following treatment among cocaine-dependent outpatients. Addiction 102: pp.271-81 Higgins ST, Silverman K and Heil SH. eds. (2007). Contingency management in substance abuse treatment. New York: Guildford Press. Higgins S et al. (1991). A behavioral approach to achieving initial cocaine abstinence. Am J Psychiatry 148: pp.1218-24 HIT campaigns portfolio 2009. Available at: http://www.hit.org.uk/campaigns.asp?id=25l [Accessed 13th Feb 2009] Hill AB. (1965). The environment and disease: association or causation? Proceedings of the Royal Society of Medicine 58: pp.295–300. Available at: http://www.edwardtufte.com/tufte/hill [Accessed 13th Feb 2009] Health Protection Agency. (2008). Prison hepatitis B vaccination programme monitoring reports. London: HPA. http://www.hpa.org.uk/webw/HPAweb&Page&HPAwebAutoListName/Page/1203582653813? p=1203582653813 [Accessed 10th Feb 2009] Horne JA et al. (2004). Screening for hepatitis C virus in the Dartmoor prison population: an observational study. J Public Health 26: pp.372-5 Hubbard RL et al. (1997). Overview of one-year outcomes in the Drug Abuse Treatment Outcome Study (DATOS). Psychol Addict Behav 11: pp.279-93 Hunt N. (2008). Guidance on standards for the establishment and operation of drug consumption rooms in the UK. York: Joseph Rowntree Foundation. Available at: http://www.jrf.org.uk/bookshop/eBooks/2266-drugs-services-standards.pdf [Accessed 18th Dec 2008] Hutchinson S et al. (2004). Sudden rise in uptake of Hepatitis B vaccination among injecting drug users associated with a universal vaccine programme in prisons. Vaccine 23: pp.210-14 Islam M and Conigrave KM. (2007). Syringe vending machines as a form of needle syringe program: advantages and disadvantages. Journal of Substance Use 12: pp.203 - 12 Leicht A. (1993). Characteristic and HIV-infection of users of syringe vending-machines and exchanging programs in Berlin/Germany. International Conference on Aids, Berlin, Germany, 6 June 1993. (abstract no. PO-D17-3931). Available at: http://gateway.nlm.nih.gov/MeetingAbstracts/ma?f=102207233.html [Accessed 13th Feb 2009] McBride AJ et al. (1997). Amphetamine prescribing as a harm reduction measure: a preliminary study. Addiction Research 5: pp.95-112 Mills EJ et al. (2005). Efficacy of acupuncture for cocaine dependence: a systematic review and meta-analysis. Harm Reduct J 2: p.4. Available at: http://www.pubmedcentral.nih.gov/picrender.fcgi?artid=1079914&blobtype=pdf [Accessed 13th Feb 2009] Moatti JP et al. (2001). Multiple access to sterile syringes for injection drug users: vending machines, needle exchange programs and legal pharmacy sales in Marseille, France. Eur Addict Res 7; pp.40-5 Author: Noel Craine Version: 0c Date: 23/02/09 Page: 29 of 32 Status: Draft Intended Audience: APoSM National Public Health Service for Wales Safe, effective and cost effective interventions for IDUs and stimulant users National Institute for Health and Clinical Excellence. (2006a). Peginterferon alfa and ribavirin for the treatment of mild hepatitis C. TA1206. London: NIHCE. Available at: http://www.nice.org.uk/Guidance/TA106 [Accessed 13th Feb 2009] National Institute for Health and ClinicaI Excellence. (2006b). Adefovir dipivoxil and peginterferon alfa-2a for the treatment of chronic hepatitis B. 2006 London: NIHCE Available at: http://www.nice.org.uk/Guidance/TA96 [Accessed 13th Feb 2009] National Public Health Service for Wales. (2006). Incidence of HCV, HBV and HIV in South Wales. Final report on the South Wales blood borne viral hepatitis incidence study 2004 – 2006. Cardiff: NPHS. Available at: http://www2.nphs.wales.nhs.uk:8080/BloodBorneVirusesDocs.nsf/7c21215d6d0c613e80256f 490030c05a/c966d33343dac12180257355004c7fff/$FILE/Incidence%20of%20blood%20bor ne%20viral%20hepatitis%20in%20injecting%20drug%20users%20in%20South%20Wales.pd f [Accessed 13th Feb 2009]] National Institute for Health and ClinicaI Excellence. (2008a). Needle and syringe programmes: review of effectiveness and cost effectiveness (revised full report October 2008) NIHCE Available at: http://www.nice.org.uk/Guidance/PHG/Wave15/7. [Accessed 13th Feb 2009] National Institute for Health and ClinicaI Excellence. (2008b). Entecavir for the treatment of chronic hepatitis B. TA153 London: NIHCE. Available at: http://www.nice.org.uk/Guidance/TA153 [Accessed 13th Feb 2009] Neale J. (2000). Methadone, methadone treatment and non-fatal overdose. Drug Alcohol Depend 58: pp.117-24 National Treatment Agency for Substance Abuse. (2002).Treating cocaine/crack dependence. London: NTA. Available at: http://www.nta.nhs.uk/publications/documents/nta_treating_crack_cocaine_2002_rip1a.pdf [Accessed 13th Feb 2009] National Treatment Agency for Substance Misuse and Conference on Crack and Cocaine. (2003). Treating crack and cocaine misuse: A resource pack for treatment providers. (Draft ) Available at: http://www.nta.nhs.uk/areas/crack_cocaine/docs/nta_crack_resource_pack_draft_feb_2003.d oc [Accessed 13th Feb 2009] Obadia Y et al. (1999). Syringe vending machines for injection drug users: an experiment in Marseille, France. Am J Public Health 89: pp.1852 – 54 Ochoa K et al. (2003). Risk behaviour for heroin-related overdose: The experiences of young injecting drug users. J Addict Dis 22: p.14A Oliver P, Forrest R and Keen J. (2007). Benzodiazepines and cocaine as risk factors in fatal overdoses. 2007. Research briefing 31. Available at: http://www.nta.nhs.uk/publications/documents/nta_rb31_benzos_cocaine_in_fatal_op ioid_overdose.pdf [Accessed 13th Feb 2009] Palmateer N et al. (2008). Evidence for the effectiveness of harm reduction interventions in preventing hepatitis C transmission among injecting drug users: A review of reviews. Summary. Glasgow: Health Protection Scotland. Available from: http://www.hepcscotland.co.uk/pdfs/p-Evidence-for-the-Effectiveness-of-Harm-Reductionreview-EXECUTIVE%20SUMMARY-2008-05.pdf [Accessed 13th Feb 2009] Pollini RA et al. (2006). Response to overdose among injection drug users. Am J Prev Med 31(3): pp.261-4 Author: Noel Craine Version: 0c Date: 23/02/09 Page: 30 of 32 Status: Draft Intended Audience: APoSM National Public Health Service for Wales Safe, effective and cost effective interventions for IDUs and stimulant users Petry NM et al. (2004). Prize reinforcement contingency management for treating cocaine users: how low can we go, and with whom? Addiction 99: pp.349-60 Prendergast M et al. (2006). Contingency management for treatment of substance use disorders: A meta-analysis. Addiction 101:pp.1546–60 Rockwell R et al. (1999). Geographical proximity, policy and utilisation of syringe exchange programmes. AIDS Care 11: pp.437–42 Roll JM. (2007). Contingency management: an evidence-based component of methamphetamine use disorder treatments. Addiction 102(Suppl 1): pp.114-20 Rome A, Shaw A and Boyle K. (2008). Reducing drug users' risk of overdose. Edinburgh: The Scottish Government Available at: http://www.scotland.gov.uk/Publications/2008/10/30132711/19 [Accessed 12th Feb 2009] Ryan J. (2000) Drug related deaths in the community: a preventative role for accident and emergency departments? Journal of Accident and Emergency Medicine 17: pp.272-273 Sagiv A et al. (2008). Intranasal transmission of hepatitis C virus: virological and clinical evidence. Clin Infect Dis 47: pp.931–34 Scheinmann R et al. (2007). Non-injection drug use and Hepatitis C Virus: A systematic review. Drug and Alcohol Dependence 89: pp.1-12 Schmitz JM et al. (1997). Relapse prevention treatment for cocaine dependence: group versus individual format. Addict Behav 22: pp.405-18 Seaman SR, Brettle RP and Gore SM. (1998). Mortality from overdose among injecting drug uses recently released from prison: database linkage study. BMJ 316: pp.426-28 Shearer J et al. (2001). Pilot randomised controlled study of dexamphetamine substitution for amphetamine dependence. Addiction 96: pp.1289-96 Sindelar JL, Elbel B and Petry NM. (2007). What do we get for our money? Costeffectiveness of adding contingency management. Addiction 102: pp. 309-16 Strang J et al. (2008). Overdose training and take-home naloxone for opiate users: prospective cohort study of impact on knowledge and attitudes and subsequent management of overdoses. BMJ 103: pp.1648-57 Strang J. (2006). Emergency naloxone for heroin overdose. BMJ 333: pp.614-5 Taylor A et al. (1995). Outbreak of HIV infection in a Scottish prison. BMJ 310: pp.289-92 Taylor T, Frischer M and Goldberg D. (1996). Non-fatal overdosing is related to polydrug use in Glasgow BMJ 313: pp.1400-01 Tobin KE, Davey MA and Latkin CA. (2005). Calling emergency medical services during drug overdose: an examination of individual, social and setting correlates. Addiction 100: pp.397404 Tucker T et al. (2004).Randomized controlled trial of a brief behavioural intervention for reducing hepatitis C virus risk practices among injecting drug users. Addiction 99: pp.115766 Ward J, Hall W and Mattick RP. (1999). The role of maintenance treatment in opioid dependence. Lancet 353: pp.221-26 Weaver et al. (2007). National evaluation of crack cocaine treatment and outcome study (NECTOS) A multi-centre evaluation of dedicated crack treatment services. London: NTA. Available at: http://www.nta.nhs.uk/publications/documents/nta_nectos_national_evaluation_crack_cocain e_treatment_and_outcome_study.pdf [Accessed 13th Feb 2009] Author: Noel Craine Version: 0c Date: 23/02/09 Page: 31 of 32 Status: Draft Intended Audience: APoSM National Public Health Service for Wales Safe, effective and cost effective interventions for IDUs and stimulant users Weild AR et al. (2000). Prevalence of HIV, hepatitis B and hepatitis C antibodies in prisoners in England and Wales: a national survey. Commun Dis Public Health 3: pp.121-6 Wiegand J et al. (2008). Treatment of acute hepatitis C: the success of monotherapy with (pegylated) interferon. J Antimicrob Chemother 62: pp.860-65 Weiss RD et al. (2005). The effect of twelve-step self-help group attendance and participation on drug use outcomes among cocaine-dependent patients. Drug and Alcohol Dependence 77: pp.177-84 World Health Organisation. (2004). Effectiveness of sterile needle and syringe programming in reducing HIV/AIDS among injecting drug users. Geneva: WHO . Available at: http://www.unodc.org/documents/hiv-aids/EFA%20effectiveness%20sterile%20needle.pdf [Accessed 13th Feb 2009] Wright Nat and Tompkins CNE. (2006). A review of the evidence for the effectiveness of primary prevention interventions for Hepatitis C among injecting drug users. Harm Reduction Journal 3;27 Available at: http://www.harmreductionjournal.com/content/pdf/1477-7517-327.pdf [Accessed 13th Feb 2009] Author: Noel Craine Version: 0c Date: 23/02/09 Page: 32 of 32 Status: Draft Intended Audience: APoSM