Case study 3 - NHS Education for Scotland
advertisement

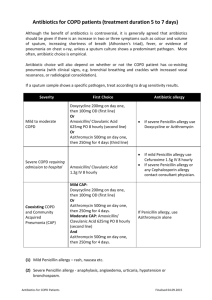
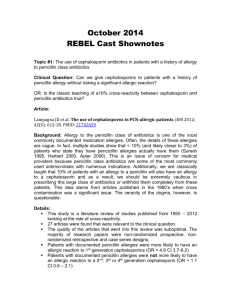
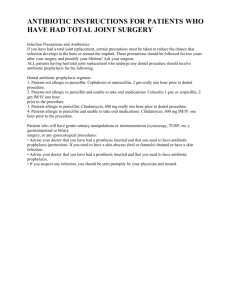
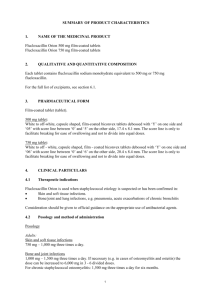
NES Core course Case study on Skin and Soft Tissue Infection (SSTI) A 70 year old lady presents to your Pharmacy with a prescription for: Flucloxacillin capsules 500mg QDS for 7 days She tells you that she fell last week whilst out walking and had sustained a small cut to her leg. Today, the area around the cut is red, hot, swollen and painful. PMH: Epilepsy Current medication: Carbamazepine 400mg BD Dyspepsia Lansoprazole 30mg mane Penicillin allergy 1) Do you think an antibiotic is indicated for this patient? Yes, there are clear signs of an infection i.e. red, hot, swollen, painful A cut to the skin means the primary defence has been breached which has exposed the patient to an infection. Antibiotics will be necessary to stop the infection from spreading. 2) Is flucloxacillin an appropriate choice for cellulitis? The most likely organisms to cause cellulitis are Staphylococcus aureus and Streptococcus pyogenes (Strep A) Flucloxacillin would be appropriate as it is has activity against these two organisms. It also has good tissue penetration. Flucloxacillin has a very narrow spectrum of activity only covering Staphylococcus aureus and streptococci therefore it will cause minimal disruption to the natural bowel flora and so has low risk for CDAD This is not a severe cellulitis (i.e. is not rapidly spreading, only covers a small area, no signs of systemic infection) therefore oral therapy with a single agent would be appropriate. If the patient is afebrile and healthy other than the cellulitis then flucloxacillin maybe used as a single agent. If the patient is febrile or shows other signs of a systemic infection then they may need admission for IV therapy (follow local guidelines). 3) Is flucloxacillin an appropriate choice for this patient? The patient has a penicillin allergy, therefore flucloxacillin is not appropriate. Check whether patient has a true penicillin allergy. What is a penicillin allergy? -1- Symptoms of true penicillin allergy are anaphylaxis, bronchospasm, urticaria, rash occurring 1 to 72 hours after taking the penicillin; it is not likely to be due to the penicillin if occurs > 72 hours. Gastrointestinal sideeffects or a minor rash (i.e. non-confluent, non-pruritic rash restricted to a small area) are not an allergic reaction. Pharmacists have an educational role to play here. Less than 20% of people who report a penicillin allergy actually have a true allergy when skin tested. By labelling somebody with a penicillin allergy you are possibly excluding them from a range of potentially life saving drugs i.e. all penicillins, cephalosporins, carbapenems. 4) What antibiotic would you recommend? Need an oral agent that is not a beta lactam that has good Staphylococcus aureus and Streptococcus pyogenes cover. Clarithromycin is a suitable alternative for treatment of cellulitis in patients with penicillin allergy. Clarithromycin interacts with carbamazepine; it can increase carbamazepine levels and possibly lead to toxicity, therefore should be avoided. From Tegretol® SPC: “Co-administration of CYP 3A4 inhibitors may result in increased carbamazepine plasma concentrations which could induce adverse reactions e.g. dizziness, drowsiness, ataxia, diplopia” – these are obviously undesirable effects in elderly. Clindamycin also has good S. aureus and S. pyogenes cover, and is suitable in penicillin allergy. You call the GP, who confirms the patient has a true penicillin allergy and agrees that flucloxacillin and clarithromycin are inappropriate and issues a prescription for: Clindamycin capsules 300mg QDS for 7 days 5) What, if any are your concerns? Patient is > 65 years and clindamycin is highly associated with Clostridium difficile associated diarrhoea (CDAD) in this patient group. The benefit of effective treatment of her cellulitis may outweigh the risk of CDAD. 4 days later the patient returns to the pharmacy. She tells you that her leg does seem to be improving and asks to purchase Imodium® tablets as she has had terrible diarrhoea for the last 24 hours. 6) What advice would you give to the patient? Stop clindamycin immediately and make urgent appointment to see GP. Consider speaking to the GP yourself. -2- Do not sell Imodium® or any other antimotility drugs. Theoretical risk of precipitating toxic megacolon by slowing the clearance of C. difficile toxin from the bowel. Rehydration is essential – maintain fluids and suggest use of Dioralyte® or similar if symptoms severe. Good hand hygiene and environment cleaning is very important. Advise to wash hands with soap and water. Do not sell alcohol hand gel. 7) What advice would you give to the GP? Clindamycin is highly associated with CDAD so you have advised patient to stop treatment. Send a stool sample to microbiology lab for culture but do not wait for the results before starting metronidazole. Assess the need for further antibiotics. If they are still required for the cellulitis use the most narrow spectrum antibiotic possible e.g. doxycycline. First line treatment for non severe C. difficile is metronidazole 400mg tds for 10 -14 days Review the need for PPI as this may also be a factor in development of CDAD. Consider stopping if not required acutely. References: 1) Health Protection Agency: Management of Infection Guidance for Primary Care for Consultation and Local Adaptation. Amended March 2009. 2) Tegretol® Summary of Product Characteristics. 3) Scottish Antimicrobial Prescribing Group: Guidance to Optimise Antimicrobial Use and Reduce Clostridium difficile Associated Disease in Scottish Hospitals, July 2008. -3-