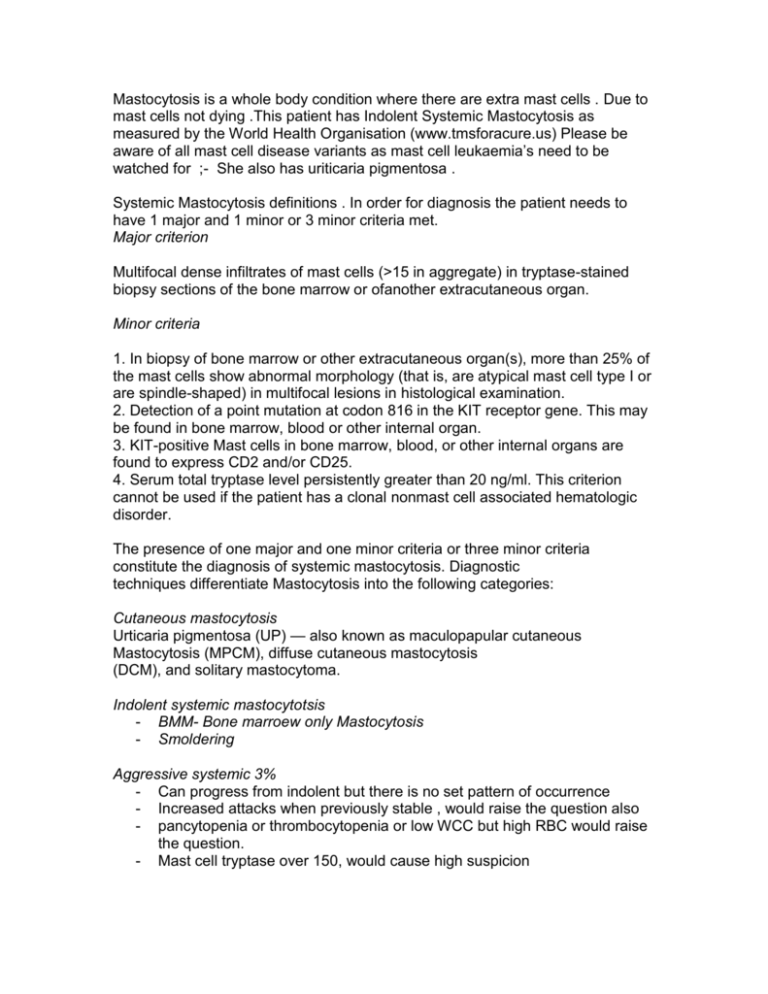
Mastocytosis is a whole body condition where there are extra mast cells . Due to
mast cells not dying .This patient has Indolent Systemic Mastocytosis as
measured by the World Health Organisation (www.tmsforacure.us) Please be
aware of all mast cell disease variants as mast cell leukaemia’s need to be
watched for ;- She also has uriticaria pigmentosa .
Systemic Mastocytosis definitions . In order for diagnosis the patient needs to
have 1 major and 1 minor or 3 minor criteria met.
Major criterion
Multifocal dense infiltrates of mast cells (>15 in aggregate) in tryptase-stained
biopsy sections of the bone marrow or ofanother extracutaneous organ.
Minor criteria
1. In biopsy of bone marrow or other extracutaneous organ(s), more than 25% of
the mast cells show abnormal morphology (that is, are atypical mast cell type I or
are spindle-shaped) in multifocal lesions in histological examination.
2. Detection of a point mutation at codon 816 in the KIT receptor gene. This may
be found in bone marrow, blood or other internal organ.
3. KIT-positive Mast cells in bone marrow, blood, or other internal organs are
found to express CD2 and/or CD25.
4. Serum total tryptase level persistently greater than 20 ng/ml. This criterion
cannot be used if the patient has a clonal nonmast cell associated hematologic
disorder.
The presence of one major and one minor criteria or three minor criteria
constitute the diagnosis of systemic mastocytosis. Diagnostic
techniques differentiate Mastocytosis into the following categories:
Cutaneous mastocytosis
Urticaria pigmentosa (UP) — also known as maculopapular cutaneous
Mastocytosis (MPCM), diffuse cutaneous mastocytosis
(DCM), and solitary mastocytoma.
Indolent systemic mastocytotsis
- BMM- Bone marroew only Mastocytosis
- Smoldering
Aggressive systemic 3%
- Can progress from indolent but there is no set pattern of occurrence
- Increased attacks when previously stable , would raise the question also
- pancytopenia or thrombocytopenia or low WCC but high RBC would raise
the question.
- Mast cell tryptase over 150, would cause high suspicion
-
Chemotherapy is used –Gleevac is the patient is ckit neg , as it doesn’t
work in ckit positive patients . Interferon in c kit positive patients
All other treatments are used to control symptoms
Notable facts
- There are mast cell leukemias which can occur .
- Cutanious Mastocytosis can become indolent systemic
- may have enlarged liver and spleen
- GI tract may be affected
- Organs failing indicates smouldering . Which raises the question of need
for mast cell numbers to be reduced medically
- mediator release symptoms are common
- Grade of bone marrow inflatration is “ normally” lower than 5%
- Mast cells co express CD2 and CD25- with kit and contain the kit mutation
D816v
Single system mast cell conditions
-
Bladder, interstitial cystitis ,
Bowel mastocyctic enrocollitis.
Mast cells are known to be involved in the pathophysiology of migraines, MS
Mast cell tryptase.
In most patients with systemic Mastocytosis , the serum tryptase concentration
exceeds 20 ng/mL, but a normal level of tryptase does not rule out either
Mastocytosis or another mast cell activation disorder.
Mast cell tryptase measures mast cell load not symptom severity . Bone marrow
biopsies need to be done with care and analysed at specialist centres to ensure
accurate results . Because staining for mast cell tryptase is complex . Sedation
with benzodiazepines is used .
During investigation – taking mast cell measurements ( in blood ) on a normal
day and within 2 hours is vital . As tryptase is processed out of the body very
quickly .
Mast cell activation disorders .
These are new diagnosis’ – monoclonal mast cell activation syndrome and mast
cell activation syndrome introduced in Dec 2010 ( Akin et al 2010 ). This is being
diagnosed by some Mastocytosis specialists and not others . the alternate
diagnosis currently is angiodeama and urticaria
Monoclonal mast cell activation – has extra mast cells in the bone marrow but not
big enough to be defined as Mastocytosis. This is often tryptase negative . Bone
marrow biopsy is required for diagnosis .
Mast cell activation syndrome – has no extra mast cells , but the pts normal mast
cells behave badly, triggering easily. All the medications , symptoms and triggers
apply. This can be very complex to treat. Diagnostic criteria are being honed
down . Currently testing is for urine histamine and prostaglandins in urine . ( Akin
et al 2010 ).
Mast cell activation can be autoimmune- notably due to hashimotos thyroiditis –
seen more commonly in mast cell conditions (
) , adrenal,
lupus or amiloyd . Due to other immunoglobulin’s – IGG- myasthenia gravis
amongst others. Autoimmune conditions , even if not mast cell activating directly
act as a magnifier of any mast cell disease .
Other conditions which can present very similar to mast cell conditions arehereditary angiodeama , carciniod syndrome and pheocryocythoma .
In the absence of any known cause an idiopathic diagnosis ( all known causes
excluded ) will be made of specific symptoms – angiodeama, urticaria and or/
anaphylaxis .
Mast cells occur naturally in mucous membranes and connective tissue -skin,
eyes, ears, nose, mouth, lips, tongue, gums, throat, lungs, esophagus, stomach
and bowels thu to bottom , bladder, womb, prostate, heart, blood vessels
,nervous system, bone marrow and brain linings . The products from mast cells
travel in the blood and have effects on the nervous system. Histamine crosses
the blood brain barrier . Receptors are found all over the body .
In indolent systemic Mastocytosis the patient likely has extra mast cells all over
the body. When a patient has an infection mast cells migrate , but don’t die so
remain in those areas . Flares of cells can happen in any area of the body or
several areas . An example is in Breast , a mass can show one day and be gone
the next , this is where mast cells were active and have now settled . Any new
symptoms should be reviewed by the relevant specialty .
These are the symptoms caused by chemical released and receptor affected .
Symptoms in red = anaphylactiod reactions
Histamine receptor type 1 effects - receptors in skin , lungs , bladder , womb ,
eyes ,ears ,
Itching , Dermatographia ,hives ,Burning rashes ,Swelling – from 3rd spacing ,
fluid moving into tissues – by blood vessels being made porous allowing fluid to
move ,flushing – dry until shock ensues , enlarged lymph nodes , pale - dizzy Hypotension ( can go high on the way – compensated shock ) Fast heart –
patients are often tachycardic day to day , up to 200bpm then dropping when
hypovolemia ensues ( syncope /presyncope ) ,short of breath –from mildly
wheezy up to respiratory rate of 40 and lungs full of fluid, Throat close /stridor–
leading to respiratory arrest ,
Bone pain in any bone – causing severe debitating pain and increase in
symptoms , joint inflammation in any joint , recurrent infections ,Eye problems –
Dry , inflammation, can be uvetitis or a less identifiable cause of inflammation
Migraines – mast cell known to be involved ,Ringing ears - , sign of high overall
inflammation, Painful sinus' – swelling in enclosed spaces ,Over heating +++
,Poor cold tolerence ,Pain in intercostal spaces ( between ribs )
Histamine receptor 2 - digestive tract ,Abdominal pain – from swelling bowel ,
cramps , large , hard abdomen ,Diarrhea – or loose stools , pencil thin stools,
Urgency and frequency,Nausea,Vomiting, abdominal anaphylaxis GERD and
too much stomach acid ,Spasms of smooth muscles – all bladder , bowel ,
stomach , womb , chest wall , night sweats.
Brain receptor histamine effects- parathsesias to numbness, Nerve pain –
neurogenic – from histamine neurotransmitter role, Brain fog - mixed organic
brain syndrome – concentration poor , memory poor, agitation , word finding
problems , down thoughts, anger/rages
Prostaglandins ,Vasodilatation, ,flushing,headaches,smooth muscle spasms
,Hypotension from vasodilation ,Anxiety when you don't feel anxious , sometimes
pacing. Over time can lead to depression .
Lecotrines swelling of airways and all over,asthma type symptoms, larangeal and
pharangeal odeama with stridor ,
Serotonin –hunger, exaggeration of mood ,diarrhea ,sleepy in day but can't sleep
at night .
Heparin ,blood thinner so leads to bleeds,,oesteoprosis- from heparin drawing
calcium from the bones constantly, compression fractures , kidney stones. Mast
cell
Tryptase,-high cholesterol .
Mast cell activation happens easily through immunologic and non immunologic
mechanisms independent of IGE. Compliment traditional and alternative
pathways cause mast cell degranulation . alternative causes Smooth muscle
spasms, anywhere ,Flushing
Blood vessels become porus leaking fluid into tissues – note 2l can move before
swelling becomes visible .Activates mast cells
Mast cells can leak mediators or completely degranulate. Patients can have more
one symptom pattern or both .ANAPHYLAXIS is a real risk in Mastocytosis and
the patient should be counseled on and have to use of 2 epipens – epinephrine
0.3ml(1/100)IM auto injector . Suitable if over 30kg . Caution in coexisting known
cardiac arrhythmia . Symptoms in red are anaphylaxis symptoms . epipens
should be given and patient call 911 and have IV antihistamines H1 &h2 ,
steroids-200mg hydrocortisone, IV fluids- NOT dextran , nebualised albuterol .
High risk of needing ICU . EPIPEN’s can be given in succession after 5 minutes if
symptoms aren’t controlled or return .
These reactions are anaphylactiod as they are NOT IGE mediated . Immunologic
– compliment , immunoglobulin’s, physical known mast cell triggers, known drugs
and secretoguges – are responsible . Presentation can be typical or atypical the
same applies with the progression . The patient should be listened to at all times
.
Anxiety presents as a symptom from histamine and prostaglandins and should
not be disregarded but seen as a serious warning sign . Reactions can be
multiphasic or well controlled with 1 epipen . Each patient will react to different
triggers at varying severity depending on many factors, so no expectation of
progression should be used .
Treatment focus' on controlling as many symptoms as possible ;-) This is by
blocking histamine receptors and stopping mast cells putting the chemicals into
the blood . Different medications help different symptoms .These are the
treatments used in practice currently .
H1 blockade - drowsy making, The drowsy ones are stronger and work better
and have the ability to stabilizing mast cells, the drowsy side effect , if
experienced wears off after 2 weeks ,
Benadryl – USA ( not ceterizine ) 25mg-50mg doses. maximum 200mg
/24h.Hydroxyzine - 25 mg up to 4 times a day- Indication brain fog ,spasms and
overall control .
Clomtron 4mg up to 6 times a day, weak stabilsing mast cells ( for emergency 8mg )Ketitofen 1-2mg 3 times a day - stabilizes mast cells . Available in Canada ,
Italy and UK . Its a safe drug widely used with immense success ,Doxepin –
blocks H1 and H2 &stabilizes mast cells and is widely used . Some people don't
tolerate it .ONLY SAFE TRICYCLIC
,H1 blockade - Non drowsy Ceterizine hydrochloride - 10 mg once a day ( I take
2 doses )Fenofexidine ( Allegra ) 180mg once a day, common dose 2 times a
day some 3 )
H2 blockade – H2 receptor agonists -digestive system, Mouth to bottom,
ranitidine 300mg twice a day - drug of choice - has taken my bowel pain on a
daily movement much better , reduced frequency and bleeding .
PPI - proton pump inhibitors, Omeprazole , lansoprazole and the like to control
excessive stomach acid,
Lecotrine receptor agonists ( blocks )Singulair 10mg once a day ( i take 2 doses
as per doc off licence this is common,
Tylenol – plain no other drugs sailcilates 1g 4 times a day - reduces effects of
prostaglandins , Weak slaicilate so caution in saliclate sensitivity,
NSAIDS / ASprin cause mast cell activation so may not be tolerated but can lead
to consistent degranulation aiding symptom control . Not for patients with vinegar
as a trigger / known asthma or previous GI bleeds .
Benzodiazepines -These are drugs with the drug name ending in pam. these
help control stress and anxiety which is a known trigger .
Opiates . Are not advised , some people tolerate them . Tramadol is tolerated by
some patients. If opiates are used then 12hrly dosing is advised to reduce
fluctuations in drug level and pain as pain is a trigger .Bone pain can be major
and restrictive gat advice if this is needed .
Cholesterol – fenofibrate 160mg once a day. statins have interactions with H2
blockers Mast cell stabilization drugs - Gastrocrom / Nalcrom - sodium, cromlyn .
is poorly absorbed systemically 800mg aday is used to get 57mg into systemic
circulation . Has nasal, ocular and nebualised preparations . 6week course used
for mastocyctic enrocollitis . Stabilses mast cells leading to less total circulating
mediators .
Osteoporosis – vitamin d and calcium supplements as both are poorly absorbed .
Biphoshonates are used but have an increased bone pain and bleeding risk , A
mast cell stabilizer reduces total circulating heparin so reduces the loss of bone .
When the list of meds is exhausted . Immune modulation can be used , these
include methotrexate , cellcept , interferon. Gleevac is used in aggressive
systemic Mastocytosis and in smoldering when there is NO ckit muttaion on
cidon816 . Interferon is used in ckit positive patients . .Steroids were used and do
work , but have serious long term implications . So are favored for emergency
only as per anaphylaxis protocol .
EPIPENS – epinephrine 300mcg -0,3ml1/1000 is used by patient when
symptoms become life threatening. Anaphylaxis/ anaphylactiod reactions can
have atypical presentation and progression.
Triggers are anything which make mast cells split , spilling their contents .
The crucial fact to understand is the activation of mast cells is NOT IGE
mediated. Other immunologic processes – compliment , immunoglobulin’s,
physical triggers, known drugs , and secretoguges are responsible for this
process .
All of these processes are termed anaphylactiod, but this does not equal less
serious. Patients get anaphylaxis, which can be fast and typical or atypical in
presentation and the patient should be listened to regards symptom level at all
times.
Every patient is individual in their triggers and symptoms from triggers . Pts
should keep diaries to work out triggers . Also acknowledge all symptoms as
most will have early warning symptoms. There is always an exception of every
rule in Mastocytosis . This is the list from tmsforacure.org,
Alcohol-50% of pts ,Anesthetic agents- must be premeditated for ANY
anesthetic/invasive procedure ,Antibiotics - mycin antibiotics ,Bacteria or fungi,
Certain foods, Cold (temperature),Coloring, packers (fillers ) & flavoring in food
sand medications, Emotional upset, Environmental toxins, Exercise or exertion –
even minor ,Fatigue ,Fever ,Friction- from clothing ,Heat (temperature) – being
hot needing aircon/fans to maintain consistent core temperature ,Infection with
viruses, bacteria or fungi, Mold MSG,Narcotics,Perfumes, paint fumes
/diesel/gas/ bbq fuel,Pesticides,Plasma expanders (i.e. dextran), Tricyclic
antidepressants, beta blockers , metroclopamide , culvinic acid , caution heparin ,
ssri/ssni ( serotonin syndrome )as serotonin is high in many pts , Hormones in
women mid month and around menstruation ,Preservatives-sulphites and all
others, Room freshener sprays, Smells, Spices, Stress ++++ high trigger
,Sunlight, personal care products, home cleaning products ,CT contrast -
absolute NO Drugs – any drug can cause an anaphylactiod reaction.
metroclopamide , tricyclic antidepressants ( bar doxepin ) , beta blockers - have
contraindications that make them an absloute NO.
If a patient thinks it a trigger it is. Patients should be encouraged to consider all
possible triggers .
Foods- high histamine foods should be avoided . Foods can be tolerated one day
but not the next , once a food or trigger has caused symptoms it should be
avoided .Through the night 2am and early hours high histamine time naturally .
for high histamine foods, .http://www.iainfoctr.com/articles/histamine.php. This
site is comprehensively referenced and written by a patient ( masters level ) with
idiopathic anaphylaxis . Has discussion of non ige anaphylaxis , receptors and
symptoms , drug no’s, causes of anaphylaxis and 3rd spacing.
IGE allergies exist with Mastocytosis at the same rate as the general population20%. These get exaggerated by the presence of extra mast cells .
Desensitization injections are not advised in Mastocytosis . medication and
trigger avoidance is the key to stability, but patients will still experience variations
and being activated .
Patients can experience issues with packers and gelatin in medications .
Triggers can cross many areas – vinegar – cleaning products, personal care,
foods as an example
The coexistence of an autoimmune condition will act as a magnifier of
Mastocytosis as the immune system activates mast cells through autoimmune
processes .
Mastocytosis will effect every patient differently, in triggers, symptoms and ideal
treatment It has risk of serious disability . Disability benefits can be sought and
will be granted . All patients go through a greif process along the lines of Kubler
Ross model and it takes time for acceptance. Lifestyle adaptations can be
difficult to make and accept . Especially in respect to restricted diet . This is
ideally not medicated unless the patient is in significant distress.
Benzodiazepines help reduce emotional stress to alleviate it as a trigger. No
antidepressants are ideal in Masto / mast cell conditions . As serotonin is high in
many, but not all patients . measurement of chromatogranin a in blood can help
determine safety of serotonin modifying medications. Best done in series of at
least 3 as serotonin will depend on level of mast cell degranulation .
Histamine gives neuropsychiatric symptoms , in the form of mixed organic brain
syndrome (
) and prostaglandins make patients behave anxious
when they will often deny this.
About 20% of patients with systemic Mastocytosis work in paid employment ,
most often to maintain insurance ( USA). The loss of career and or previous
abilities can be very distressing for individuals . Support groups of other patients
provide valuable support and understanding. Patients have often suffered up to
10 years at diagnosis and many experience personal loneliness or social
loneliness/exclusion due to avoiding triggers and lack of understanding among
family and friends . Especially with multiple investigations not yielding any results
. As a result some patients are wary of new doctors as no previous doctor has
found out what is wrong / helped them . Patients also are likely to have clutch of
diagnoses – IBS, asthma ( not responding to normal treatments ) , fibromyalgia,
chronic fatigue syndrome , migraines . POTs and Ethers danlos are been
researched for their connection to mast cell disease .
The ckit mutation occurs after conception so is not inherited in systemic
Mastocytosis but in uriticaria pigementosa when appearing in children can be
passed on.
The risk of anesthetics and invasive procedures should not be underestimated .
Premedication MUST be given .
This link has the Anesthetic guide , or you can email me josieevans@yahoo.co.uk
WHAT YOU SHOULD KNOW ABOUT ANESTHESIA – IT COULD SAVE YOUR
LIFE
Nancy Gould and Regis (Gigi) Park
INTRODUCTION
Surgery is a stressful experience. For a patient with mast cell disease, that stress is compounded
by the possibility of complications including anaphylaxis, cardiovascular collapse, increased
bleeding and even death. Therefore, general anesthesia is considered a high-risk procedure in
patients with mast cell disease. It is critical that all members of the patient’s operating team take
proper precautions before, during, and after surgery to protect against
potentially life-threatening mast cell activation
.
PLANNING FOR SURGERY SHOULD BEGIN AS SOON AS THE NEED FOR
SURGERY ARISES
It is imperative that good communication is established between the patient, referring physician,
surgeon, anesthesiologist, nurses, and all others involved in the patient’s care before, during, and
after surgery. The surgeon must be aware of the patient’s mast cell disease and inform themselves
of the measures necessary to keep the patient as free of symptoms as possible. Additionally, the
patient should contact the anesthesiologist assigned to their care as soon as possible after surgery
has been scheduled. Both regional and general anesthetics can cause lifethreatening
complications. An experienced anesthesiologist is aware of medications known to cause mast cell
degranulation and medications that stabilize mast cells. If the patient is satisfied that their
anesthesiologist fully understands the importance of planning around the mast cell disease, it will
go a long way toward calming the patient, which in turn may reduce mast cell mediator release.
Symptoms should be as well-controlled as possible in the days prior to surgery. The patient
should carefully avoid known triggers of mast cell activity and should take their medications as
prescribed. Those medications include H1 and H2 histamine receptor blockers such as Allegra
(H1) and Zantac (H2). A mast cell stabilizer such as disodium cromoglycate or ketotifen, and
medications targeting other mast cell mediators should be taken regularly if they are
part of the patient’s normal drug regimen.
The patient’s complete medication list should be reviewed by the surgical team prior to surgery
and any necessary medication changes should be thoroughly discussed with the patient. For
example, if the patient regularly takes a
medication in the family known as beta blockers for blood pressure or heart rate abnormality, a
change to another drug should be considered well before surgery is scheduled. Beta blockers are
generally avoided in people with mast cell disease undergoing surgery because they interfere with
an important natural control of mast cell activation. These drugs may also interfere with the use
of epinephrine, which may be required if the patient has a major release of mast cell mediators
resulting in low blood pressure during surgery. Other drugs that may interfere with control of
blood pressure during surgery must be carefully reviewed by the patient’s physician before the
surgery. It may be necessary to perform a “graded challenge” procedure in the hospital under the
supervision of an allergist and an anesthesiologist for certain medications if there is no history of
exposure to that medication. This procedure usually starts with scratching the skin with a small
amount of medication followed by injection of increasing amounts with careful monitoring after
each injection. Resuscitation equipment and drugs including epinephrine must be readily
available during the procedure.
PRECAUTIONS TAKEN IN THE HOURS PRIOR TO SURGERY WILL HELP THE
PATIENT GO
INTO SURGERY IN THE BEST POSSIBLE CONDITION
For pre-operative control of anxiety and the reduction of mast cell activity, drugs in the valium
family (diazepam, midazolam, lorazepam) are usually effective. Some procedures require the
patient not to take anything by mouth including medications after midnight of the night before the
surgery. In this case, H1 and H2 blockers should be administered intravenously prior to the
surgery. The use of corticosteroids, such as prednisone, has also been suggested although there is
no evidence that the short-term use of steroids reduces the ability of mast cells to
release the chemicals contained in their granules. However, corticosteroids may reduce the extent
of other inflammatory reactions that result from mast cell activation. A tube may be inserted into
an artery and attached to a device allowing the anesthesiologist to vigilantly monitor
blood pressure without having to periodically inflate a blood pressure cuff. In addition, a tube is
inserted into a vein and securely taped in place, with intravenous (IV) fluids running to keep the
patient well-hydrated in all surgeries involving general anesthesia or conscious sedation. This
tube will also make it possible to immediately administer any emergency medications that may be
needed. In the operating room, the patient should not be allowed to become either too cold or
over-heated. Warm blankets should be used, and all IV fluids should be warmed before they are
given. In addition, there should be a minimum of noise and bustle around the patient prior to the
administration of the anesthetic in order to reduce the possibility of anxiety-triggered mast cell
mediator release.
EMERGENCY SURGERY
An emergency situation may arise in which a person with mast cell disease requires immediate
surgery. Wearing a MedicAlert bracelet could be a life-saver if this happens. Inscriptions vary
depending upon the patient’s specific needs, but generally include the patient’s diagnosis and
drug sensitivities. Emergency response team members can
access more detailed information 24 hours a day, 7 days a week from the MedicAlert organization
by dialling the toll-free number on the bracelet. MedicAlert is a non-profit organization serving
patients world-wide. There are nominal membership and annual fees with financial assistance
available for those in need. For more information,
please visit www.medicalert.org or dial 888-633-4298 within the U.S. or 209-668-3333 from
outside the U.S.
Alternatively, there are several companies that manufacture and inscribe medical identification
jewellery. These products are available on the internet and are also carried by some jewellery
stores and pharmacies. It may be wise to select jewellery which provides space for a miniature
version of the patient’s medical history (often supplied by
the manufacturer as part of the cost) in addition to the inscription. Although these companies do
not have a 24 hour information center, they do not require membership or annual fees and may be
preferable for some patients. It may also be helpful for mast cell patients to carry with them at all
times emergency information, written on their physician’s letterhead, which contains a list of
current medications and other instructions for treatment in the event of severe symptoms.
DURING SURGERY
Constant attention from the anesthesiologist is required for the safety of a patient with mast cell
disease during surgery, as some of the early symptoms of mast cell mediator release such as
flushing, hives, and early signs of obstructed breathing can be masked by the surgical drapes
covering much of the patient’s skin and by the use of an airway tube during anesthesia.
Should anaphylaxis occur during surgery, the drug thought to be responsible should be
discontinued immediately and epinephrine should be administered. Airway support with 100%
oxygen, IV replacement fluids to compensate for dilated blood vessels, H1 and H2
antihistamines, bronchodilators, and corticosteroids may also be given.
Continuous IV epinephrine and other “vasopressor drugs” may be necessary to keep blood
pressure from falling.
However, it is important to keep in mind that not all hypotensive episodes during surgery are due
to mast cell degranulation and anaphylaxis. A serum tryptase level obtained during the
hypotensive episode and its comparison with pre-surgery or “baseline” level may be helpful to
determine whether the episode is due to mast cell degranulation.
DRUGS
Records from prior surgeries should be examined and drugs tolerated in those procedures should
be preferred if possible. Prior to the administration of any drugs associated with surgery, it is
important that an IV is running, that
epinephrine is available for immediate intramuscular (IM) or IV administration, and that
emergency equipment is
easily accessible in case of an adverse reaction.
IV preparations without preservative should be used.
Drugs to avoid include ethanol, dextran, and non-steroidal anti-inflammatory drugs (NSAIDs)
such as ibuprofen
and toradol (unless the patient is already successfully taking a drug in this family), polymyxin B,
amphoteracin B,
quinine, dextromethorphan, α-adrenergic blockers, β-adrenergic blockers, and anticholinergic
drugs as well as
drugs mentioned in specific categories below.
Local anesthetics – True allergic reactions to local anesthetics resulting from mast cell
degranulation are thought
to be rare. Skin testing and graded challenge protocols have been published and may be
administered by an allergist
prior to the surgery if questions arise regarding the safe use of a local anesthetic in a patient. If
possible,
preservative-free local anesthetic should be used in these tests, as the preservative often present in
local anesthetics
can cause a mast cell reaction. In general, local anesthetics in the “ester” group should be
avoided. This group
includes procaine, chloroprocaine, tetracaine, and benzocaine. Anaphylactic reactions to local
anesthetics in the
“amide” group are rare. This group includes lidocaine, mepivacaine, prilocaine, bupivacaine,
levobupivacaine, and
ropivacaine.
Muscle relaxants - Muscle relaxants are the most likely group of the anesthetic drugs to cause
anaphylaxis.
Succinylcholine, D-tubocurarine, metocurine, doxacurium, atracurium, and mivacurium are more
likely to cause a
severe reaction than rocuronium or the so-called nondepolarizing muscle relaxants such as
pancuronium or
vercuronium. Some studies have reported increased numbers of anaphylactic reactions to
rocuronium, however, so
it may not be appropriate as the first choice for patients with mast cell disease.
Induction drugs - These are medications given to initiate anesthesia. It is rare for mast cell
activation to occur in
response to the use of propofol, ketamine, or the benzodiazepine drugs such as midazolam.
Inhaled anesthetics - Sevoflurane is an inhibitor of mast cell activation and is less likely to cause
liver damage
than other inhaled anesthetics in this family.
Opiates and opioids - Oral opioid drugs for pain relief may be tolerated by some mast cell
disease patients, but
their use should be approached with caution, beginning with very small doses. All drugs in this
category are
capable of causing mast cell mediator release.
SUMMARY
Surgery for a person with mast cell disease involves exposure to drugs and conditions that may
trigger extensive
mast cell degranulation. It should be emphasized that it is often impossible to predict or avoid the
risk of adverse
events which may occur in surgery due to the administration of drugs and the procedure itself.
The risk can be
reduced, though, if the mast cell disease is brought to the attention of everyone involved in the
patient’s care and
measures are taken to reduce the possibility of mast cell mediator release. Careful planning is
important, beginning
from the time a need for surgery has been defined and continuing through the immediate preoperative period,
anesthesia, surgery, and recovery. The choice of drugs is of major importance, and the
anesthesiologist, the
surgeon, the nursing staff, the patient’s physician, and the patient should form a working team to
ensure that
surgery presents the fewest possible dangers for the patient.
Neither The Mastocytosis Society nor the authors intend that this information replace
medical advice
given by the patient’s doctor. Patients are encouraged to consult with their doctor
regarding medications
and procedures related to surgery.
REFERENCES
Hazards in operative management of patients with systemic mastocytosis; HW Scott Jr, WCV
Parris, PC Sandidge,
JA Oates, LJ Roberts II; Annals of Surgery, May 1983;197(5):507-514
Anesthetic management of systemic mastocytosis: experience with 42 cases; WCV Parris, HW
Scott, and
BE Smith; Anesthesia and Analgesia (1986)65:S117 (Abstract)
Urticaria Pigmentosa: An anesthetic challenge; Eric P Greenblatt, Linda Chen; Journal of Clinical
Anesthesia,
March/April 1990;2:108-115
Mastocytosis: Perioperative considerations; VA Goins; AORN Journal December
1991;54(6):1229-1238
Anesthesia in a patient with malignant systemic mastocytosis using a total intravenous anesthetic
technique;
A Borgeat and YA Ruetsch; Anesthesia and Analgesia (1998);86:442-444
Treatment of systemic mast cell disorders; AS Worobec; Hematology/Oncology Clinics of North
America (June
2000);14(3):659-687
Treatment of mastocytosis: pharmacologic basis and current concepts; G Marone, G Spadaro, F
Granata,
M Triggiani; Leukemia Research, July 2001;25:583-594
Mastocytose: Anesthésie générale par rémifentanil et sévoflurane; L Auvray, B Letourneau, M
Freysz; Ann Fr
Anesth Réanim 2001;20:635-638 (article in French)
Mastocytosis: Current concepts in diagnosis and treatment; L Escribano, C Akin, M Castells, A
Orfao,
DD Metcalfe; Annuals of Hematology (2002);81:677-690
Anaphylaxis during the perioperative period; DL Hepner and MC Castells; Anesthesia and
Analgesia
2003;97:1381-1395
The authors wish to thank Cem Akin MD, PhD, for his review of this article.
Copyright 2010. The Mastocytosis Society, Inc. All Rights Reserved.
Valerie M. Slee, Chair, Board of Directors
23 Camelot Dr. Shrewsbury, MA 01545 • Phone: 508-842-3080 • Fax: 508-842-2051 •
E-mail:chairman@tmsforacure.org • Web: www.tmsforacure.org
The Mastocytosis Society • P.O. Box 731 • Brenham, TX 77834
Medical Emergency Response Plan
for Systemic Mastocytosis, Mast Cell Activation, and Anaphylaxis
If the patient presents with flushing, rash, hives, swelling, abdominal pain, nausea,
vomiting,
shortness of breath, wheezing or hypotension, respond with the following:
Administer
• Epinephrine 0.3 cc of 1/1000 and repeat 3x at 5-minute intervals if BP < 90 systolic (0.1
cc
for children under 12)
• Benadryl (Generic: diphenhydramine) 25-50 mg (12.5-25 for children under 12) orally,
intramuscular or intravenously every 2—4 hours or Atarax (Generic: hydroxizine) 25mg
(12.5 mg for children under 12) orally every 2—4 hours
• Solu-Medrol (Generic: methylprednisolone) 120 mg (40 mg for children under 12)
IV/IM
• Oxygen by mask or nasal canula 100%
• Albuterol nebulization
Call 911 and take the patient to the closest Emergency Room.
Pre-medication for major and minor procedures and for radiology procedures
with and without dyes:
• Prednisone 50 mg orally (20 mg for children under 12) 24 hours and 1—2 hours prior to
surgery
• Benadry1 (Generic: diphenhydramine) 25-50 mg orally (12.5 mg for children under 12)
or
Atarax (Generic: hydroxizine) 25 mg orally, 1 hour prior to surgery
• Zantac (Generic: ranitidine) 150 mg orally (20 mg for children under 12) 1 hour prior to
surgery
• Singulair (Generic: montelukast) 10 mg orally (5 mg for children under 12) 1 hour prior
to
Surgery
Drugs to be avoided:
• Aspirin and non-steroidal anti-inflammatory medications
• Morphine, codeine derivatives
• Vancomycin
Recommend: Tylenol
The Mastocytosis Society thanks Dr. Mariana Castells for this emergency protocol.
I am a degree nurse of 15 years , who now has idiopathic angiodeama and
anaphylaxis , of highly suspected mast cell origin . I have researched in detail for
myself and for other patients .
Worldwide specialists on systemic Mastocytosis ;- They accept referral for
patients with systemic Mastocytosis
Cem Akin, M.D., PhD
Brigham and Women’s Hospital
1 Jimmy Fund Way,
Smith Building Room 626D
Boston , MA 02115
Chestnut Hill, MA 02467
Email: cakin@partners.org
Phone:
617-732-9850
Fax: 617-525-1310
Mariana Castells, M.D., Ph.D.
Brigham and Women’s Hospital
1 Jimmy Fund Way,
Smith Building Room 626D
Boston , MA 02115
Email: mcastells@partners.org
Phone:
617-732-9850
Fax: 617-525-1310
Larry Schwartz, M.D., Ph.D.
Internal Medicine: Rheumatology, Allergy, and Immunology
Virginia Commonwealth University
P.O. Box 980263
1250 East Marshall St.
Richmond, VA 23298
Phone:
804-828-9685
Fax: 804-828-0283
Email: lbschwar@vcu.edu
Philip Askenase, MD, Chief Section of Allergy and Clinical Immunology
Department of Internal Medicine
Yale University School of Medicine
333 Cedar Street
New Haven CT 06520
Email: philip.askenase@yale.edu
Tel
203-785-4143
Fax 203-785-3229
Theoharis Theoharides, M.D., Ph.D.
Professor of Pharmacology and Internal Medicine
Tufts University School of Medicine
136 Harrison Avenue
Boston, MA 02111
Email: Theoharis.Theoharides@Tufts.edu
Phone:
617-636-6866
Fax: 617-636-2456
Srdan Verstovsek, M.D., Ph.D. / Associate Professor
Leukemia Department
MD Anderson Cancer Center
1515 Holcombe Blvd, Unit 428
Houston, TX 77030
Email: sverstov@mdanderson.org
Phone:
713-792-7305
Fax: 713-794-4297
Dr. Leonard Bernstein, M.D.
Bernstein Allergy Group
8444 Winton Road
Cincinnati, OH 45231
Phone:
513-931-0775
Fax: 513-984-1096
Email: bernstil@email.uc.edu