Pediatric Pulmonology 27:423–427 (1999) Diagnostic and
advertisement
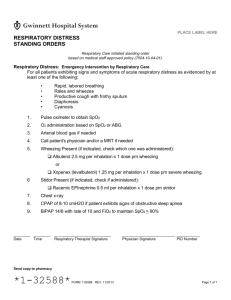
Pediatric Pulmonology 27:423–427 (1999) Diagnostic and Therapeutic Methods Relation Between Pulse Oximetry and Clinical Score in Children With Acute Wheezing Less Than 24 Months of Age Dolores Pavo´n, MD , 1 INT ROD UCT ION Jose Antonio Castro-Rodri´guez, Rubilar, MD,11and Guido Girardi, MD,1,2* Lilian MD Summary. The aim of this study was to determine the relation between transcutaneous hemoglobin oxygen saturation, measured by pulse oximetry (SpO2), and clinical score values in 138 infants (mean ± SD, 6.6 ± 5.5 months of age) with acute wheezing episodes presenting in a primary care outpatient setting. A single investigator evaluated the severity of the acute wheezing episodes by assigning a clinical score and was unaware of the SpOvalues. Another investigator measured SpO2values on all subjects. The mean (± SD) SpO22value was 98.2 ± 1.1% for children with clinical scores of 2–5 (n = 32); 95.4 ± 1.5% for those with scores of 6–7 (n = 82), and 92.9 ± 2% for children with scores of 8–10 (n = 24), ( P < 0.001 by Bonferroni’s multiple comparison, when all two-way comparisons were done for each pair of results). The clinical score showed a good correlation with SpO2(r = -0.76; 95% CI, -0.83 to -0.68). We conclude that if pulse oximetry is not available, it is advisable to include oxygen in the therapy of wheezy infants with clinical scores values 8. Pediatr Pulmonol. 1999; 27:423– 427. © 1999 Wiley-Liss, Inc. Key words: pulse oximetry; clinical score; wheezing; therapy; oxygen; bronchiolitis. score vs. SpO212in children under 2 years of age with acute wheezing. usefulness of clinical scores for the evaluation of the 13In Chile, wheezing is the most common cause of pediatric severity of acute wheezing episodes in infants has been shown visits to outpatient departments. Most of these visits occur at in several studies.4,5However, there are conflicting data in the a primary-care level where pulse oximetry is not readily literature.6This highlights the need for objective methods to available. We, therefore, designed the present study to evaluate the severity of these episodes. Hypoxemia is the correlate the clinical score used in Chile’s Acute Respiratory primary early feature resulting from the pathophysiological Infection National Programwith changes that occur in the children with airway obstruction, and it is an important marker of disease severity.Pulse 1Pediatric Pulmonology Unit, Department of Pediatrics, Exequiel Gonza´les oximetry is a simple noninvasive method, and it gives fast Co´rtes Children’s Hospital, University of Chile, Santiago, Chile. and fairly accurate assessment of arterial oxygen saturation.6,7 2Pediatric Pulmonary Section, Respiratory Sciences Center, University of Arizona, Tucson, Arizona. There have been contradictory results in previous studies which have tried to establish a correlation between clinical This work was presented in part at the American Lung Association/ scoring systems and the degree of transcutaneous hemoglobin American Thoracic Society International Conference, May 16–21, 1997, San oxygen saturation as measured by pulse oximetry (SpO2) in Francisco, CA. children.4,5,8,10–124,8,9Only one study compared a clinicalThese *Correspondence to: Jose Antonio Castro-Rodri´guez, M.D., Respiratory studies were conducted using patients of different ages, Center, Arizona Health Sciences Center, 1501 N. Campbell Ave., different respiratory diseases (e.g., pneumonia, bronchiolitis, Sciences Tucson, AZ 85724. E-mail: jacastro@resp-sci.arizona.edu or asthma), and different severities of disease (hospitalized vs. Received 31 August 1998; Accepted 15 December 1998. ambulatory subjects) and patients were evaluated by several observers. 1–3The © 1999 Wiley-Liss, Inc. 424 Pavo´n et al. TABLE 1—Modified TAL’s Clinical Score1 Respiratory rate 0 40 30 None2 None None SpO2values in a group of young children with acute wheezing Abbreviations PaCOPartial pressure of carbon dioxide in arterial blood PaO22Partial pressure of oxygen in arterial blood SpO2Transcutaneous episodes seen in a primary care setting. hemoglobin oxygen saturation MATERIALS AND METHODS In this cross-sectional study we evaluated 138 children (age range, 1–24 months) who presented with acute wheezing episodes to a single primary care center in Santiago (545 m above sea level), from July to November 1995 (winter–spring and the respiratory syncytial virus season). We did not distinguish between asthma and bronchiolitis. All children had a chest film. Children with a clinical and/or radiological diagnosis of pneumonia, pulmonary or cardiac congenital malformations, chronic pulmonary disease, malnutrition, or a history of prematurity were excluded. The study was approved by the local Ethics Committee, and verbal consent of each parent was obtained. 1The patients were accompanied by their mothers at all times. After a period of adjustment for at least 5 min, and with the child quiet, not crying, without fever, and breathing room air only, one investigator (L.R.) evaluated the severity of the acute wheezing episodes using a modified Tal’s clinical score(the modification was only in the respiratory frequency according to age;1314see Table 1). Respiratory frequency was determined by observation of the thoracic movement over a full minute. The degree of accessory muscle use was based on the degree of intercostal or subcostal retraction. According to the policy of Chile’s Acute Respiratory Infection National Program, infants with clinical scores of 11–12 must be referred immediately for hospitalization and, therefore, were not included in the present study.We recently determined that infants with a clinical score of 11–12 constituted no more than 3% of all wheezing infants (G. Girardi, unpublished observations). Simultaneously, and without knowing the result of the clinical score, another investigator (D.P.) measured SpO2 with a pulse oximeter (Omheda Biox 3740, Louisville, CO) using a pediatric probe placed on the big toe, with infant quiet, awake, and in natural light. The maximum SpO2was recorded after a period of at least three satisfactory sweeps of the pulse wave were recorded (corroborating that the cardiac frequency of the oximeter coincided with the simultaneously taken heart rate by auscultation). For this study, we defined hypoxemia as a SpO2value 91%. The data were analyzed with the EpiInfo v.5.1 (CDDWHO) program. Student’s t-test was used to test the significance of r or the difference between two means. Bonferroni analysis was used for evaluations of multiple comparisons and multiple regressions (Stata v.5.0, Corp., TX). Statistical significance was considered when P 0.05. Score RESULTS One hundred thirty-eight infants (88 male, 50 female) with a mean (± SD) age of 6.6 ± 5.5 months (range, 1–24 months) were included in the analysis. For the entire population (n 4 138), the mean (± SD) SpO2value was 95.6 ± 2.3%, and the clinical score value (mean ± SD) was 6.4 ± 1.4. The mean (± SD) SpO2value was 98.2 ± 1.1% in children with a score of 2–5, 95.4 ± 1.5% in those with a score of 6–7, and 92.9 ± 2% in children with a score of 8–10, (P < 0.001 by Bonferroni’s multiple comparison, when all two-way comparisons were done for each pair of results; Table 2). When we divided the population into three age groups (<3, 3–5, and 6 months of age), SpO2 values were still significantly different based on the clinical score in each age group (P < 0.001 by Bonferroni’s multiple comparison, when all two-way comparisons were done for each pair of results; the only exception was (per min) Wheezing CyanosisAccessory muscle use<6 mths 6 mths with stethoscope Perioral with crying + 2 56–70 46–60 Inspiration and expirationwith stethoscope Perioral at rest ++ 3 >70 >60 Audible withoutstethoscope Generalized at rest +++ 1 41–55 31–45 End expiration 1 14Score: mild, 5; moderate, 6–7; severe, 8–10; very severe, 11–12. Derived from Martínez et al.,with the addition of an age-appropriate respiratory rate score. 2 If wheezes not audible due to a minimal air entry, consider score 3. Pulse Oximetry and Wheezing 425 by Clinical Score and Age Group1 C SpO2 l T o t a l < 3 m o n ti h s 3 – 5 m o n t h s 6 m o n t h s X ± S D n X ± S D n X ± S D n nX ± S D n 2–5 98.2 ± 1.1 32 98.1 ± 1.2 14 98.8 ± 1 i4 98.0 ± 1.1 14 6–7 95.4 ± 1.6 82 95.0 ± 1.4 18 95.5 ± 1.6 31 95.4 ± 2.4 33 8–10 92.9 ± 2 24 93.5 ±c0.7 2 92.0 ± 2.3 7 93.2 ± 3.8 17 a for each set of pairs in each age-group and the total group, SpO2for all pairs was 1When all two-way comparisons were done l for Bonferroni’s multiple comparisons); the only exception was in the <3 months significantly different (P < 0.001 corrected age group between those children with clinical score 6–7 vs. 8–10 (P 4 0.15). s c o r e TABLE 3—Correlation (r) Between the Components of the group, in which there was no difference Clinical Score vs. SpO2 TABLE 2—Average SpO2 in the <3 months age in the clinical scores of 6–7 vs. 8–10, P 4 0.15, Table 2). Clinical score r* Components The correlation coefficient between total clinical score and Cyanosis -0.38 Respiratory rate -0.41 Wheezing -0.52 Accessory muscles use SpO2was r 4 -0.76 (P < 0.0001; 95% CI, -0.83 to -0.68). The -0.55 Total score: -0.76 correlation of each component of the clinical score and *P < 0.0001, for all components and total score. SpO2was also significant (P < 0.0001): wheezing r 4 -0.52, cyanosis r 4 -0.38, accessory muscle use r 4 -0.55, and respiratory frequency r 4 -0.41 (Table 3). Age did not influence this correlation (data not shown). In the more severely affected patients (clinical score 8–10), the correlation between SpOand clinical score was r 4 -0.57 (P 4 0.004). The linear regression model between SpO22and clinical score was y 4 103.5147–1.2421x (Fig. 1). A clinical score 8 had 100% sensitivity, 86.4% specificity, and 100% negative predictive value to detect hypoxemia (SpO291%). DISCUSSION The clinical score originally described by Tal et al.1 has been used in many clinical trials.3,15–17In the present study, using a modified Tal’s clinical scorein a large number of infants with acute wheezing without pneumonia, we demonstrated a good correlation (r 4 -0.76; 95% CI, -0.83 to -0.68; P < 0.0001) between our modified Tal’s score and SpO2144,5. The correlation was maintained in all three age groups (<3, 3–5, and 6 months), and remained significant (r 4 -0.57, P 4 0.004) in infants with severe wheezing (clinical score 8–10). The good correlation found in our study was due, in part, to the fact that only one investigator evaluated the clinical score in all patients, in contrast to other studies where there were several observers with wide variations in scoring between them.We also used a selected population defined as outpatients up to 2 years of age with acute exacerbation of wheezing and without pneumonia, instead of a population with a wide age range,4,55,9and with different types 6,9,10and severities of respiratory illness. A clinical score similar to that applied in the present study was used in 71 pediatric asthmatic outpatients (mean ± SD, 10 ± 2.6 years of age), in whom a strong Fig. 1. Correlation between clinical score and SpO2. correlation (r 4 -0.7, P 0.001) between asthma severity and SpO2was demonstrated.128showed a poor correlation between SpOHowever, in other studies using different methodologies in the assessment of clinical severity of disease, contradictory results appeared. For example, using a different clinical score, Alario et al.2 9and acute wheezing episodes (r 4 -0.36, P 0.01) in 74 infants (mean age, 16.1 months; range, 1–36 months). In contrast, Dawsonshowed a good correlation (r 4 -0.76, P 0.0001) in 41 hospitalized asthmatic children (mean age, 5.5 years; range, 3–13 years) between the same parameters. Studies of children with different respiratory diseases have given variable results. Wang et al. could not demonstrate a significant correlation (r 4 -0.04) between SpO2and a clinical score similar to the one we used, in 58 infants hospitalized for pneumonia 426 Pavo´n et al. 3use such testing in the evaluation of acute wheezing. Therefore, disease severity is usually established on clinical 4(mean age, 12.3 months) and bronchiolitis (mean age, 6.6 grounds. months). 13In Chile, most children with acute wheezing episodes are A single clinical sign will not be very indicative of severity treated in a primary-care setting.Due to inadequate resources, of airway obstruction, but a combination of signs may provide many of those centers do not have pulse oximetry available to more valid information, considering the complex relationship determine the need to add oxygen to bronchodilator therapy. between the pathophysiological and the clinical features of If pulse oximetry is not available, we conclude that it is acute asthma. Our study showed a better correlation when it advisable to include oxygen in the therapy of any infant with considered the clinical score as a whole, instead of each an acute wheezing episode who has a clinical score 8. isolated element of the score (Table 3). Margolis et al. took Using our criteria may result in a few infants receiving 27 elements of a clinical score in 312 infants with acute lower oxygen unnecessarily, but on the other hand, all hypoxemic respiratory tract infection (mean age 4 months, 87% children will be identified. bronchiolitis) and could not demonstrate a correlation with hypoxemia (SpO25<95%). However, when they used a group of five clinical characteristics, the sensitivity was 88%, the ACKNOWLEDGMENTS specificity was 90%, and the negative predictive value was We thank Dr. Asher Tal, M.D. (Ben-Gurion University of the Negev, Israel), and Dr. Mark A. Brown, M.D. 80%. (Respiratory Sciences Center, University of Arizona), for their advice and critical reviews. As in other studies,we found that respiratory frequency had one of the lowest correlations (r 4 -0.41, P < 0.0001) with SpO25. In contrast, in children with pneumonia, the correlation between respiratory rate and SpO2 2 REFERENCES or PaO2 was good.10,11 2 . than PaO2.18 7 , 1 9 2. Abara S, Girardi G, Mun˜oz R, Varas R, Maggiolo J, Reyes M. Manejo del sindrome bronquial obstructivo agudo del lactante en una sala de pre-hospitalizacio´n. Enf Respir Cir Torac 1990;6:192– 197. 3. Mallol J, Barrueto L, Girardi G, Munoz R, Puppo H, Ulloa V, Toro O, Quevedo F. Use of nebulized bronchodilators in infants under 1 year of ag analysis of four forms of therapy. Pediatr Pulmonol 1987;3:289–303. 4. Wang E, Milner R, Navas L, Maj H. Observer agreement for respiratory signs and oximetry in infants hospitalized with lower respiratory infection Am Rev Respir Dis 1992;145:106–109. 5. Margolis P, Ferkol T, Marsocci S, Super DM, Keyes LL, McNutt R, Harrell FE. Accuracy of the clinical examination in detecting hypoxemia i infants with respiratory illness. J Pediatr 1994;124: 552–560. 6. Kerem E, Canny G, Tibshirani R, Reisman J, Bentur L, Schuh S, Leviso H. Clinical-physiologic correlations in acute asthma of childhood. Pediatr 1991;87:481–486. 7. Connett GJ, Lenney W. Use of pulse oximetry in the hospital management of acute asthma in childhood. Pediatr Pulmonol 1993;15:345–349. 8. Geelhoed G, Landau L, Le Soue¨f P. Evaluation of SaO2as a predictor outcome in 280 children presenting with acute asthma. Ann Emerg Med 1994;23:1236–1241. 9. Dawson K. The asthma clinical score and oxygen saturation. Aust Clin Rev 1991;11:20–21. 10. Reynolds EOR. Arterial blood gas tensions in acute disease of lower respiratory tract in infancy. Br Med J [Clin Res] 1963;i: 1192—1195 11. Madico G, Gilman R, Jabra A, Rojas L, Hernandez H, Fukuda J, Bern C Steinhoff M. The role of pulse oximetry. Its use as an indicator of severe respiratory disease in Peruvian children living at sea level. Arch Pediatr Adolesc Med 1995;149:1259–1263. 12. Alario A, Lewander W, Dennehehy P, Seifer R, Mansell A. The relation between oxygen saturation and the clinical assessment of Respiratory frequency is more dependent on PaCO Accessory muscle utilization is a very useful parameter in evaluating the severity of airway obstruction and in predicting the need for oxygen supplementation.198We also found that the degree of accessory muscle use (i.e., degree of intercostal or subcostal retractions) had the best correlation with hypoxemia (r 4 -0.55, P < 0.0001). In contrast, Mulholland et al.did not find a correlation between this sign and SpO2, perhaps due to more severe airway obstruction in their population. We found that a clinical score 8 had a sensitivity of 100%, specificity of 86.4%, and negative predictive value of 100% in diagnosing hypoxemia (SpO91%). The definition of hypoxemia (by SpO225,8,11Geelhoed et al.) in the literature is arbitrary, with suggested “cutoff ” values ranging between 90 and 95%.demonstrated that an initial value of SpO2891% (in room air) is a good predictor for poor outcome in children (mean age, 6.3 years; range, 1.0–14.5 years) with acute asthma (sensitivity, 100%; specificity, 84%). In our study, the precise duration of hypoxemia was not determined. In several studies, SpO2and PaCO2were the best indicators of the need for aggressive oxygen therapy, rather than PaO The aim of the present study was to determine whether hypoxemia by SpO132(as an index of ventilation/perfusion abnormalities in infants with acute wheezing) could be identified using an established clinical score performed as part of the Chilean Acute Respiratory Infection National Program.20Arterial blood gases and pulmonary function measures are rarely performed to objectively assess disease severity in wheezy children.There are usually no resources for most primary-care physicians to 1. Tal A, Bavilski C, Yohai D, Bearman J, Gorodischer R, Moses S. Dexamethasone and salbutamol in the treatment of acute wheezing in infants. Pediatrics 1983;71:13–18. Pulse Oximetry and Wheezing 427 acutely wheezing infants and children. Pediatr Emerg Care 1995; 11:331–334. 13. Astudillo P, Girardi G, Mancilla P, Aranda C. Hospitalizacion abreviada en 13,099 lactantes con sindrome bronquial obstructivo agudo. Rev Chile Enf Respir 1994;10:290. 14. Marti´nez R, Maggiolo J, Girardi G, Mora F, Carren˜o V, Mascaro´ J. Frecuencia respiratoria en lactantes y preescolares sanos y con infeccio´n respiratoria aguda. Enf Respir Cir Torac 1990;6:134– 140. 15. Lin Y-Z, Hsieh K-H. Metered dose inhaler and nebuliser in acute asthma. Arch Dis Child 1995;72:214–218. 16. Mallol J, Munoz R, Puppo H, Ulloa V, Toro O, Girardi G, Barrueto L. Effects of nebulized fenoterol, associated with ipratro- pium or steroids, on the heart rate of infants under one year of age with acute wheezing. Pediatr Pulmonol 1987;3:83–85. 17. Mallol J, Barrueto L, Girardi G, Toro O. Bronchodilator effect of fenoterol and ipratropium bromide in infants with acute wheezing: use of MDI with a spacer device. Pediatr Pulmonol 1987;3:352– 356. 18. Kerem E. Why do infants and small children breathe faster? Pediatr Pulmonol 1996;21:65–68. 19. Mulholland E, Olinsky A, Shann F. Clinical findings and severity of acute bronchiolitis. Lancet 1990;335:1259–1261. 20. Canny GJ, Reisman J, Healy R, Schwartz C, Petrou C, Rebuck A, Levison H. Acute asthma: observations regarding the management of a pediatric emergency room. Pediatrics 1989;83:507–512.