Autoimmune skin diseases in dogs and cats
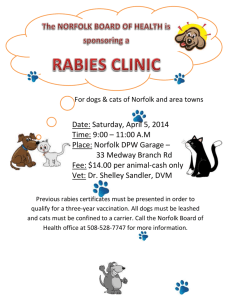
advertisement
Autoimmune skin diseases in dogs and cats Glen Burkett BVSc. Dip ACVD Animal Dermatology and Allergy Estero, FL Definition: a condition where the immune system fails to tolerate self and mounts an immune response, involving antibodies or lymphocytes, which affects the structure or function of the skin. Types: 1. Pemphigus a. Foliaceus b. Erythematosus c. Vegetans d. Vulgaris e. Paraneoplastic 2. Subepidermal blistering diseases a. Acquired junctional epidermolysis bullosa (AJEB) b. Bullous pemphigoid (BP) c. Bullous systemic lupus erythematosus type 1 (BSLE-1) d. Linear IgA disease e. Mixed AISBD f. Mucous membrane pemphigoid (MMP) 3. Lupus erythematosus (LE) a. Systemic (SLE) b. Discoid (DLE) c. Vesicular cutaneous (VCLE) d. Exfoliative cutaneous (ECLE) 4. Alopecia areata 5. Linear IgA pustular dermatosis 6. Cryoglobulinemia and Cryofibrinogenemia 7. Graft vs. Host disease 8. Canine Uveodermatological Syndrome (Vogt-Koyanagi- like syndrome) The 2 most common autoimmune skin diseases seen in dogs and cats are pemphigus foliaceus and discoid lupus erythematosus. The rest of this article will only discuss these diseases. Pemphigus foliaceus (PF) Pemphigus is crusting and pustular disease seen in dogs, cats, horses and goats. Autoantibodies target and breakdown desmosomes between keratinocytes. As a result, the keratinocytes become 1 Tri- County C.E. Conference March 22, 2015 detached from one another, also known as acantholysis. Recognizing these acantholytic keratinocytes is important in diagnosing this disease. Signalment Mainly middle age to older dogs and cats are affected but PF can be seen at any age. Males and females equally affected. Akitas and Chows are the most likely breeds to get this disease. Causes Most cases are idiopathic. Drug induced pemphigus has been documented in humans and the following drugs have been suspected in dogs: cephalexin, amoxicillin-clavulanic acid, ampicillin, trimethoprim-sulfonamide and cimetidine. Promeris (metaflumizone-amitraz), Certifect (fipronil-amitraz-methoprene) and Vectra 3D (dinotefuran-pyriproxyfen-permethrin) have been documented as causes in dogs. Ultraviolet light is a potential trigger for pemphigus and cases do appear to worsen in the summer. Foods, especially those containing the thiol group (e.g. onions and garlic) and infection can induce pemphigus in humans. It is unknown if these could be a trigger in dogs and cats. Clinical signs Typical lesions are large, fragile pustules that quickly rupture to form crusts. Lesions are bilateral and symmetrical with the face and ears being involved in more than 80% of cases. Footpads can be involved with fissures, crusts and peeling of the pads. Purulent material can be seen around nailbeds in cats. Cats also frequently have crusts around the nipples. The condition may wax and wane with some patients being febrile and depressed during outbreaks. It may or may not be pruritic. Diagnosis Distribution and appearance of the lesions help to make a tentative diagnosis. Cytology of pustules or from under crusts should show acantholytic cells with neutrophils and often eosinophils. Biopsies of intact pustules show subcorneal pustules with acantholytic cells. Indirect immunofluorescence identifies circulating autoantibodies but is highly variable. Direct immunofluorescence identifies epidermal IgG but this is not specific to pemphigus. Routine CBC and serum chemistry typically shows a moderate to marked neutrophilia. Treatment Glucocorticoids Oral prednisone or prednisolone is commonly used in dogs, at 2.2-4.4 mg/kg every 24 hours for 7-14 days. If no new pustules or crusts are seen after this period the dose can be tapered. There is no set protocol for this but it must be done slowly over a 30-40 day period to achieve a maintenance dose of 1mg/kg every other day. If the patient is still doing well, the dose can be further reduced over the next 30 days to 0.5mg/kg every other day. Monotherapy alone with corticosteroids seem to be effective for 40% of PF cases in dogs. Those that have a 75% improvement by day 7 seem to have a more favorable outcome just with corticosteroids. 2 Tri- County C.E. Conference March 22, 2015 Oral predNISone is not recommended in cats, due to it’s lower bioavailabity in this species. PredNISOLone, is a better choice and is dosed 2.2-4.4mg/kg every 24 hours. Alternative glucocorticoids include triamcinolone 0.6-2mg/kg/day, or methylprednisolone 1.8-3.5mg/kg every 24 hours with tapering after 7-14 days. If a relapse occurs, or poor response is seen in the first 2 weeks, then additional immunosuppressive drugs are needed. Azathioprine The starting dose of azathioprine is 1.5-2.5mg/kg orally daily. Azathioprine can take 3-8 weeks to have an effect. Once the disease is in remission, the azathioprine should be decreased to every other day. Adverse reactions include leukopenia, anemia and thrombocytopenia. Vomiting, diarrhea, hepatotoxicosis and acute pancreatitis can also occur. CBC’s and serum chemistries are advised every 2-3 weeks during the first 3 months of therapy then every 6 months. Available in a 50mg tablet only. Not recommended in cats due to very high risk of severe myelosuppression. Chlorambucil Dosed at 0.1-0.2mg/kg every 24-48 hours. Side effects include myelosuppression, vomiting and diarrhea but these are less likely seen than with azathioprine. Blood monitoring as with azathioprine is still recommended. This drug can also take several weeks to have an effect. Available as a 2mg-coated tablet that limits it’s use to cats and small dogs. Cyclosporine The modified (microemulsion) form of cyclosporine may be useful when combined with other immunosuppressive drugs. In dogs success has been seen using cyclosporine initially at 510mg/kg/day with 2.5-5mg/kg ketoconazole in conjunction with glucocorticoids or glucocorticoids and azathioprine. It can take several weeks to have an effect. Glucocorticoids, in some cases, may be eventually tapered off completely and the other drugs reduced to every 2-3 days for maintenance. In one study, 6/6 cats treated with cyclosporine 5mg/kg/day along with glucocorticoids were able to eventually wean off glucocorticoids completely and stayed maintained on cyclosporine alone. Other drugs Tetracycline or doxycycline plus niacinamide combination, mycophenolate mofetil, cyclophosphamide, injectable gold salts, dapsone and intravenous immunoglobulins have all been tried to treat and manage pemphigus. Discoid lupus erythematosus (DLE) Autoantibodies in this disease are directed at the dermoepidermal junction. This leads to deeper lesions than seen with pemphigus. Signalment Usually a disease of young to middle aged dogs. Collies, German Shepherds, Shelties, Siberian Huskies and German Shorthaired Pointers seem at higher risk for developing this. 3 Tri- County C.E. Conference March 22, 2015 Causes UV light appears to be an important exacerbating factor for DLE. Clinical signs Clinical signs, in dogs, are usually limited to the face and include depigmentation and ulceration of the nasal planum, lips, and periocular area. Crusting is often present on the bridge of the nose and inner pinnae. Crusts and ulcers may also be found on the distal limbs, footpads and perianal area. DLE is very rare in cats. Nasal involvement is less prominent and lesions commonly involve the face and ears. Diagnosis This is based on clinical appearance plus histopathology. The depigmentation of the nasal planum is accompanied by swelling so that the nose loses is normal cobblestone appearance and looks shiny. Histopathology reveals lichenoid or hydropic interface dermatitis along the dermoepidermal junction. It may be difficult in some cases to differentiate between this disease and mucocutaneous pyoderma based on histopathology. Direct immunofluorescence reveals immunoglobulin deposits at the dermoepidermal junction. ANA should be negative. Treatment Many cases of DLE are mild so aggressive immunosuppressive drugs may not be needed. Topical Glucocorticoids Topical glucocorticoids alone can sometimes be the only treatment needed for milder case of DLE. Generally start with a potent form such as betamethasone dipropionate ointment 0.05%, or fluocinonide cream 0.05%. Use daily for 7 days then every other day for 7 days before switching to a lower potency formulation such as triamcinolone cream 0.1% or 2% hydrocortisone two the three times weekly or less. Daily use of strong topical steroids past 2 weeks will lead to localized atrophy, alopecia and pyoderma. Percutaneous absorption or ingestion may also cause iatrogenic Cushings in dogs and diabetes mellitus in cats. Topical Tacrolimus Tacrolimus 0.1% cream twice daily initially, then tapered based on response, has been useful in cases of DLE. May cause a pruritic or burning sensation during the first few days of application. Brand name Protopic is very expensive but good responses have also been seen with compounded (and cheaper) versions. Systemic glucocorticoids For more severe cases oral glucocorticoids are needed. These should be dosed as for pemphigus. Niacinamide with tetracycline or doxycycline Tetracycline has several anti-inflammatory properties. Niacinamide (NOT NIACIN) inhibits mast cell degranulation and phosphodiesterase. The combination of these drugs has been used in various autoimmune diseases. However clinical response can take 2-3 months. Tetracycline may be difficult to get now so doxycycline has been substituted for it. The dose of doxycycline is 5- 4 Tri- County C.E. Conference March 22, 2015 10 mg/kg every 12 -24 hours. Dogs weighing less than 10kg receive 250mg niacinamide every 8 hours. Dogs greater than 10kg received 500mg every 8 hours. Side effects are generally related to GI upset. Discontinuing the niacinamide often resolves this. Once remission is seen the frequency can be reduced. Other medications as listed for pemphigus are generally not needed for DLE as cases tend to be less severe. 5 Tri- County C.E. Conference March 22, 2015