Policy and Procedure Framework
advertisement

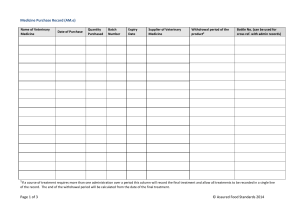
Western Health Alcohol Withdrawal Procedure code: Effective date: Last review date: December 2007 Next review date: Policy: Sub-section: 1. Overview To inform clinical staff of the procedure to effectively manage patients/consumers who are identified at risk of alcohol withdrawal in hospital. 2. Responsibility Nurse Unit Managers Head of Unit Department Heads Clinical staff 3. Authority Head of Unit - Addiction Medicine 4. Applicability Medical staff and Nursing staff in clinical areas 5. Associated Procedures/Instructions In support of this procedure, the following Manuals, Policies, Instructions, Guidelines, and/or Forms apply: Name: Alcohol Withdrawal Scale (AWS). Number: 6. Procedure Detail 6.Overview Any patient who may be at risk to develop Alcohol Withdrawal Syndrome while in hospital should be identified and offered appropriate management. 6.1 Alcohol Withdrawal Risk A patient might have one or more of the following characteristics: Drinks on five or more days each week, Consumes six or more drinks (alcoholic beverage in standard drinks) per day (NB especially elderly & patients with significant liver disease). A past history of alcohol withdrawal syndrome and/or DT (Delirium Tremens). Patient has a current diagnosis of alcohol dependence syndrome (i.e. 'alcoholic'). 6.2 Management in hospital Authorisation Authority: Date: Page 1 of 6 Once a patient at risk has been identified, the medical officer should prescribe appropriate doses of Thiamine, Multivitamins and prophylactic Diazepam for both symptom relief and to minimise the risk of withdrawal complications. Nursing staff should refer to the Alcohol Withdrawal Scale (AWS) as a guide to patient treatment response and to guide them about the potential need for additional medication (eg, Further Diazepam dosing etc.) Prompt institution of treatment usually attenuates the duration and severity of the Alcohol Withdrawal Syndrome. Alcohol withdrawal syndrome in all hospitalised alcoholics is lik ely to be more severe, especially when there is a co-existing medical or surgical illness (i.e. Fever, sepsis, pain, and other stressors). Liaison with the Drug & Alcohol Service is recommended especially in cases of severe of otherwise complicated Alcohol Withdrawal reactions 6.3 Nursing Assessment A patient identified at risk of Alcohol Withdrawal syndrome should be commenced on an Alcohol Withdrawal Scale (AWS). The patient is to be assessed utilising the AWS: o Upon admission o 1 hour after the loading doses o 4 hourly thereafter for 24 hours o HMO review daily for continuation of AWS The time of assessment & the score must be documented on the AWS. A score of 6 or more indicates a significant alcohol withdrawal response and should prompt a dosing with diazepam. 6.4 Treatment All patients should receive Thiamine supplementation (eg. 100mg daily or more) and have any electrolyte abnormality (hypokalemia & hypomagnesemia are quite common) corrected. The treatment for Alcohol Withdrawal may sometimes only require supportive nursing care but in hospitalised alcoholics, there is more likely to be a requirement for pharmacotherapy to treat withdrawal symptoms. Furthermore, the use of pharmacotherapy (i.e. usually benzodiazepines like Diazepam etc) early as “prop hylaxis” can reduce the risk of the Alcohol Withdrawal Syndrome’s progression and development of complications eg. Seizures, delirium etc. Diazepam is provided in one of two ways: o Firstly as “Symptom-Triggered” which means a dose is given according to the AWS score (eg. >6 gets 20mg Diazepam) or according to any “prn” provision made on the drug chart (eg. Diazepam 5 – 10mg prn) which is determined by patient request and nursing assessment; o The second way of providing Diazepam in Alcohol Withdrawal is to utilise this drug for “Prophylactic” benefit i.e. a loading dose of 60mg (or more) given early but after the blood alcohol level has fallen below 0.1gm% [< 22mmol] and as three sequential doses of 20mg 1 2hours apart; any further doses are given when the AWS score exceeds 6. The latter process continues for 24 hours after which time, the HMO needs to review the patient. Any patient who scores 9 or more ( = severe) should always receive 20mg and further doses as required until their score falls consistently below 6. A maximum dose of 120mg Diazepam is considered appropriate for most patients however there may be rare exceptions (eg. patient dependent upon alcohol plus high regular doses of diazepam/other benzodiazepines): in such circumstances, consultation with Addiction Medicine is highly recommended. Precautions: One hour after any dose of diazepam, the patient needs to be assessed for any signs of respiratory compromise. If signs of respiratory compromise are identified, withhold any further doses and contact the treating unit. Code and title of procedure Authorisation Authority: Page 2 of 6 Date: 6.5 Discharge Follow up The patient should always be referred to Drug & Alcohol service to follow up care post discharge regarding their alcohol consumption and suffering of a Withdrawal reaction whilst in hospital. Consideration should be given to the initiation of relapse prevention/anti -craving medication prior to discharge (i.e. Naltrexone; Acamprosate) for any patient who has required treatment for alcohol withdrawal. Guidance may be obtained by contacting the Addi tion Medicine HMO via switchboard. PROCEDURE Refer to Alcohol Withdrawal Scale (AWS) attached. FURTHER INFORMATION Sample medication sheets available on 1 West NUM Ward 1 West Approval Head of Addiction Medicine 7. References Sullivan, J.T.; Sykora, K.; Schneiderman, J.; Naranjo, C. A; and Sellers, E. (1989). Assessment of alcohol withdrawal: The revised Clinical Institute Withdrawal Assessment for Alcohol scale (CIWA-AR). Br J Addict 84:1353-1357. Foy, S. Mc Kay, S. Ling S., Bertram and Sadler. (2006). Clinical use of a shortened alcohol withdrawal scale in a general hospital. Internal Medicine Journal.36, 150-154. 8. Document History Number of revisions: Issue dates: 9. Sponsor Jenny Walsh - Divisional Director Medicine/COGS/Aged Care 10. Approval Authority Head of Unit - Addiction Medicine 11. Authorisation Authority Clinical Governance Code and title of procedure Authorisation Authority: Page 3 of 6 Date: The Alcohol Withdrawal Scale (AWS) This protocol should be used in all patients withdrawing from alcohol. INITIAL ASSESSMENT Drinking history Previous withdrawal episodes / complications Current level of intoxication/withdrawal Blood Alcohol Level (B.A.L.) Is the patient in a state of alcohol withdrawal or at high risk of developing severe withdrawal symptoms? (See below) YES Diazepam titration regimen NO Observe 2-4 hourly as B.A.L. falls to zero and subsequent 24 hours Alcohol withdrawal pharmacotherapy Diazepam Titration Regimen: 1. Without a loading dose: if uncomplicated withdrawal in the past or history uncertain a. If AWS > 6 use diazepam 10-20mg PO hourly and monitor hourly. b. If AWS< 6 observe 4 hourly. Diazepam 5-10mg up to q.i.d., p.r.n. may be used for mild symptom relief. c. Cease protocol if AWS < 10 for 24 hours following last diazepam dose. Diazepam is not usually necessary for more than 3 days. 2. With a loading dose: If at high risk of severe withdrawal symptoms (past history of seizures, delirium hallucinations or other severe withdrawal reactions OR if AWS > 6 before BAL <0.1%). In addition to the above use: a. Diazepam 20mg when B.A.L. <0.1% or AWS > 6 (which ever is the sooner) followed by: b. Diazepam 20mg every hour until withdrawal symptoms settle and patient is lightly sedated. Do not give once patient is sedated. Reassess the patient before administering more than 60mg. Consult with Addiction Medicine Physician before using more than 12 0mg. c. Gradually taper diazepam over 3-5 days Code and title of procedure Authorisation Authority: Page 4 of 6 Date: ALCOHOL WITHDRAWAL SCALE USERS REFER TO NURSING GUIDELINES WHERE AVAILABLE N AM E: U.R. No: Address D.O.B. D AT E: DR: W A R D :(per axilla) Temperature D A T E T I M E Bradma Label 1) 37.0 – 37.5C 2) 37.6-38.0C 3) Greater than 38.0C Pulse (beats per minute) 1) 90-95 3) 101-105 5) 111-120 2) 96-100 4) 106-110 6) Greater than 120 Respiration rate (inspiration per minute) 1) 20 –24 2) Greater than 24 Tremor (arms extended, fingers spread) 0) No tremor 2) Not visible – can be felt fingertip to fingertip 4) Moderate with arms extended 6) Severe even with arms not extended Sweating (observation) 0) No sweat visible 2) Barely perceptible, palms moist 4) Beads of sweat visible 6) Drenching sweats Visual disturbances (photophobia, seeing things) 0) Not present 2) Mild sensitivity (bothered by the lights) 4) Intermittent visual hallucinations (occasionally sees things you cannot) 6) Continuous visual hallucinations (seeing things constantly) Clouding of sensorium (“What day is this? What is this place?”) 0) Oriented 2) Disorientated for date by no more than two days 4) Disorientated for date 6) Disorientated for place (re-orientate if necessary) Quality of contact 0) 2) 4) 6) In contact with examiner Seems in contact, but is oblivious to environment Periodically becomes detached Makes no contact with examiner Agitation (your observation) 0) 2) 4) 6) Normal activity Somewhat more than normal activity Moderately fidgety and restless Pacing, or thrashing about constantly Thought disturbances (flight of ideas) 0) No disturbance 2) Does not have much control over nature of thoughts 4) Plagued by unpleasant thoughts constantly 6) Thoughts come quickly and in a disconnected fashion Alcohol withdrawal scale regime – NOTE CHANGE IN SCORE 1 Score 4th hourly routinely 2 If greater than 6 score 2nd hourly 3 If greater than 9 score hourly TOTAL Code and title of procedure Authorisation Authority: Page 5 of 6 Date: Code and title of procedure Authorisation Authority: Page 6 of 6 Date: