Answers
advertisement

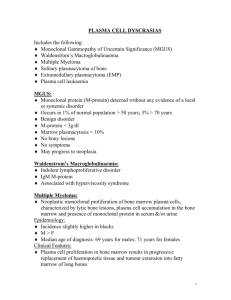
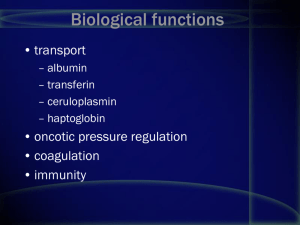
Small Group Case # 8: Thursday, September 19, 2002. HEMATOLOGY/ONCOLOGY 1 HEMATOLOGY/ONCOLOGY A 78 year-old-man presented to the emergency room for acute loss of vision in the left eye. Ophthalmic examination in the E.R suggested retinal vein thrombosis. On further evaluation patient described progressive tiredness and bone pain in the spine and hip. He also described two back-to-back episodes of upper respiratory bacterial infections. Physical examination revealed a pale white elderly man with purpura on the legs and arms. No enlargement of the lymph nodes or spleen was noted. A CBC showed the following values: WBC Neutrophil Eosinophil Basophil Lymphocytes Monocytes = 7.8 x 109/L = 63% = 2% =1 = 30% = 4% RBC Hb/Hct MCV MCHC MCH Platelets RDW = 3.67 x 1012/L = 9.8 g/dL / 24 = 89 fL = 30 g/L = 26.7 pg = 352 x 109/L = 14 Review of the peripheral blood smear showed pink, hyaline proteinaceous material and normochromic normocytic red cells. No abnormal circulating cells were seen. The reticulocyte count was 2%. A total serum protein was found to be 10.8 g/dl. Q1. What other tests would you like to do at this point and why? 1. Serum and urine protein electrophoresis 2. Serum immunofixation 3. PT and PTT 4. Skeletal survey Multiple small osteolytic lesions were found in the spine and hip bones. A serum protein immunofixation after electrophoresis showed the following results: Small Group Case # 8: Thursday, September 19, 2002. HEMATOLOGY/ONCOLOGY 2 Q2. What would you like to do next in your diagnostic evaluation and why? Serum paraprotein quantitation, serum calcium, bone marrow biopsy and aspiration with cytogenetics. Flow cytometry or immunohistochemistry if diagnosis is in question. Serum -2 microglobulin and C-reactive protein for prognostication. Examination of the bone marrow biopsy showed the following cells on an aspirate Q3. Describe the complete immunophenotype and the best markers to identify these cells CD138+, CD38+, best marker is cytoplasmic immunoglobulin light-chain evaluation by immunohistochemistry or flow cytometry. Other markers are CD56+, CD45-, CD20-, CD19-, Q4. Describe this disease with respect to the following 1. General features 2. Various clinical presentations 3. Pathophysiology 4. Diagnostic criteria 5. Course General features: Most common malignant plasma cell dyscrasia. A disease of adults (usually > 60 years). Not seen in children. Refractory to treatment in most cases. Small Group Case # 8: Thursday, September 19, 2002. 3 HEMATOLOGY/ONCOLOGY Various clinical presentations and pathophysiology: Bone pain BONE DESTRUCTION Hypercalcemia IL-1 IL-6 Release of cytokines Anemia Marrow infiltration IL-6 Multiple myeloma MONOCLONAL PROTEIN IMMUNE DEFICIENCY Renal failure Amyloidosis Hyperviscosity Infection Diagnostic criteria: 1 major + 1 minor criteria or 3 minor criteria Major criteria: 1) Plasmacytoma on tissue biopsy 2) Marrow plasmacytosis (>30%) 3) Monoclonal protein a) IgG >3.5 g/dl b) IgA >2 g/dl c) Light-chains only (Bence-Jones proteins) > 1 g/dl Minor criteria: 1) Marrow plasmacytosis 10-29% 2) Monoclonal protein that is less than that required in major criteria 3) Lytic bone lesions 4) Decrease in uninvolved (non-clonal) immunoglobulins a) IgM <50 mg/dl b) IgA < 100 mg/dl c) IgG < 600 mg/dl