Access, Booking and Choice Policy, appendix 1
advertisement

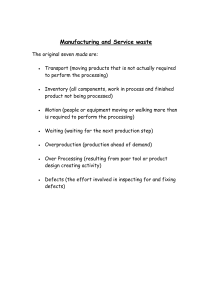
ROYAL NATIONAL ORTHOPAEDIC HOSPITAL NHS TRUST OPERATION GUIDANCE 2008-09 GENERAL Management of waiting lists Patients will be treated in order of their clinical need. Patients with similar clinical needs will be treated in chronological order. The Trust will meet/achieve national directives on outpatient, inpatient, day case and diagnostic waiting times (including cancer standards), adhering also to targeted volumes for the total number of patients waiting. iSoft Patient Manager (PAS) or linked systems must be used to administer all referrals and waiting lists. Patient information stored on all computer systems must be accurate and confirmed with patients on each attendance. All patients added to a waiting list will be either partially or fully booked. There will be a process of regular audit of waiting list management to ensure compliance with the policy and guidance Patients removed from the Trust waiting list in accordance with this policy may be reinstated where there is a sound clinical reason for doing so. This will only occur with prior agreement by the responsible consultant, clinical lead or general manager for the Division within which the specialty sites, and the service manager responsible for the specific waiting list. Patients who inform the Trust that they no longer wish to remain on the waiting list will have their request confirmed in writing. The GP and consultant will be notified in writing and will be given two weeks in which to reinstate the patient on the waiting list on clinical grounds and with the agreement of the patient. Children and known vulnerable adults will be discussed with the consultant. Patient records on PAS will be updated in real time. D:\533567122.doc 1 Cancellations or changes to appointments Reasons for cancellations or changes to appointments must be accurately recorded in PAS using either a drop down menu or free text. A clear audit trail for all changes must be available from the patient’s electronic record. Patient cancellations Patients who cancel their initial appointment will be given an alternative date at the time of cancellation. The patient must be informed that the cancellation is regarded as a self-rejected and will reset the start of the wait to the date on which the patient would have attended. If a patient cancels two reasonable offers, the patient is to be informed that this will result in removal from the waiting list. With 18 weeks the clock start date does not change if the patients cancel Cancellation by the Trust Patients that have been previously cancelled should not be cancelled a second time except in exceptional circumstances. All such cancellations must be authorised by the appropriate General Manager, and a plan for patient care agreed. If there are changes to patient appointments at short notice, the date of the rescheduled appointment must take account of clinical urgency Where patients have to be cancelled within six weeks, the clinical needs of the patients must be taken into consideration and the scheduler must discuss this with the clinician. Cancellation by a clinician A minimum of six weeks notice is required when a clinician requires a clinic/ list to be cancelled due to annual leave, study leave or other planned reasons. Any clinic/ list cancellations need to be approved and signed of by the relevant general manager or service manager using the Trust clinic cancellation pro forma and must be accompanied by a clinic/ theatre list indicating the timescales in which cancelled patients must be rebooked, having consulted the doctor/ nurse concerned about the clinical requirements. When clinics have to be unavoidably cancelled at short notice, immediate notification to the relevant general manager or service manager, nursing staff and outpatient managers/ schedulers (where D:\533567122.doc 2 appropriate) is essential. The head of outpatient/ inpatient scheduling must work with the relevant specialty general manager or service manager to arrange reprovision of the clinic/ list. Patients who do not attend their appointment New appointments All adult patients who do not attend their hospital appointment will be discharged back to GP care. Exclusions to this are: cancer patients and known vulnerable adults. All Paediatric patients who do not attend will have their notes reviewed by their clinician to determine the future care plan. If a patient disputes a discharge due to not attending their appointment, then the manager or supervisor for that area may, at their discretion, book a further appointment/ procedure for the patient. Follow Up appointments Patients are discharged unless the clinician requires otherwise. Transfers into/ out of Trust Patients who have had a private outpatient appointment, but have elected to have NHS inpatient treatment will be treated in the same way as patients who have had a NHS consultation. Former private patients must be referred via their GP or their private patient consultant. Patients can be transferred to another provider by local arrangement. These patients must remain on the Trust waiting list until treated. Selection of patients is in accordance with the prevailing criteria. Waiting list monitoring Management of the waiting list will be routinely monitored as outlined in the appropriate procedure. Communication Communication with patients will be informative, clear and concise. The process of waiting list management will be transparent to the public, staff and commissioners of the service. This will include the patient being made aware of their responsibility to attend for treatment and to inform the Trust of any changes in their condition or social circumstances. D:\533567122.doc 3 When a patient attends the hospital the following information will be confirmed: o Confirmation of the patient’s address (including postcode) and referring general practitioner; o Patient’s telephone number (home, work and mobile) or a number through which they can be contacted; o Availability to come in at short notice (e.g. less than 72 hours) if an unexpected vacancy arises and if the patient has not been given an admission date; o Any special circumstances requiring longer notice than usual for admission (e.g. caring for elderly relative, transport arrangement); o Any dates when a patient will not be available for admission (e.g. booked holiday). o Ethnicity, if not already recorded. This information is expected to be provided by the GP or referring consultant for the first outpatient appointments. Patients will be given a date which is considered robust and unlikely to change. For written and verbal offers of an appointment or admission offer to be reasonable (with the exception of patients with suspected cancer), the following waiting time guidance will be followed: i) “For a written appointment or admission offer to a patient to be deemed reasonable, the patient is to be offered an appointment or admission date with a minimum of three weeks notice (21 days). ii) “In addition to the 3 weeks notice, for a verbal appointment or admission offer to a patient to be deemed reasonable, the patient is to be offered: for inpatient admission - a minimum of two admission dates for an outpatient appointment - an appointment on a minimum of two different dates. Where patients are offered dates with less than 21 days notice, the patient’s decision to decline the date must not be recorded as a self rejection. GPs and consultants must refer in line with specialty protocols where they exist. D:\533567122.doc 4 OUTPATIENTS Referrals Choose and Book Patients can be booked into outpatient clinics using the direct booking Choose & Book system (DBS). Directly booked patients will agree their appointment slot during, or immediately after, their GP appointment. A letter confirming their time and date of appointment is automatically generated by the national Choose and Book system. Paper referrals All paper referrals must be date-stamped on day of receipt into Trust, in order to indicate start of the outpatient wait. For the 18 week target, the start of journey is the date of referral from the GP whether that referral is directly to the Trust or via an external organisation the date of a consultant’s decision to commence a patient on a pathway when the patient converts their Choose and Book unique booking reference number (UBRN). Most referrals are made to a specific consultant. Where there is pooling, referrals are registered to the consultant with appropriate specialty/ subspecialty interest and the shortest wait. Where more than one clinician partakes in the same specialty/ subspecialty the referrals will be pooled and allocated to the clinician with the shortest wait. If a referral has been made and the special interest of the consultant does not match the needs of the patient, the consultant must transfer the referral to an appropriate colleague where such a service is provided by the Trust, and a letter to this effect sent to the GP or referring consultant. The 18 week clock start remains unaffected. If the referral is for a service that is not provided by the Trust, then the referral letter will be returned to the referring GP or consultant advising that patient needs to be referred elsewhere. Cancer Referrals To meet required NHS standards, suspected cancer referrals must be seen by a specialist within 14 days of their GP deciding that they need to be seen urgently and requesting an appointment. Referrals from GPs will comply with the referral guidelines for suspected cancers as agreed by the North London Cancer Network in D:\533567122.doc 5 January 2008. Referrals will be by referral protocol or must clearly identify the two-week rule/ cancer/ tumour. Appointments Outpatient appointments are classified into three groupings: o See within 2 weeks (Cancer 2 week rule referrals) o See within 4 weeks (Urgent referrals) o See within the maximum allowable time limit (all other patients) In all cases, patients are to be allocated outpatient slots in a chronological order. During 2008-9, the Urgent referral category will disappear as the maximum waiting time decreases to 5 weeks. Clinic management Clinic templates will be reviewed annually by the general manager and lead clinician. Templates should reflect expected performance as laid out in the Service Level Agreement with the lead PCT and good clinical practice; in line with National agreements and guidelines. Clinics should not be overbooked, except in exceptional circumstances and with the agreement of the general manager and consultant. Blocked clinics will be created in PAS to allow rescheduling of patients who have had to be cancelled at short notice. It is anticipated that as waiting times decrease these should only be used infrequently. D:\533567122.doc 6 DAY CASES AND IN-PATIENTS Patients will only be added to the ‘live’ waiting list if they are medically fit for surgery and can attend (with reasonable notice – see below) for surgery within the maximum waiting time specified within the national guidance and annual SLA agreed with the Lead PCT. Additions to waiting lists Summary of criteria for addition to waiting lists Only add patients to a Waiting List when they have accepted consultant advice for elective treatment. Only add patients who are ready to come in on the date the decision to add to the list is made. Do not add patients if they have weight to lose or gain. Do not add patients if they are unfit. Do not add patients if they are not ready for the surgical phase of treatment, unless they fit the criteria of an addition to the planned waiting list. Do not add patients where there is no serious intention to admit them: o because they are not ready to be treated, for example, because they are pregnant at the time that the decision to add to the list is made o because of the rules of this policy o because of procedural restrictions, e.g. clinically prohibited procedures o Second opinion Patients Listed for more than one procedure Where more than one procedure will be performed at one time by the same surgeon, the first procedure will be added to the waiting list with additional procedures noted. Where different surgeons working together will perform more than one procedure at one time, the patient will be added to the waiting list of the consultant surgeon for the priority procedure with additional procedures noted. Where a patient requires more than one procedure performed on separate occasions by different (or the same) surgeons the scheduler will seek guidance from the relevant consultants as to the order in which the patient will be treated. If the later Decision To Admit (DTA) is the highest priority procedure to be undertaken, then the waiting list episode relating to the earlier DTA will be suspended - NB no suspensions with 18 weeks immediately D:\533567122.doc 7 with a review date allowing enough time for the patient to be treated and recover from the procedure (the maximum 60 day suspension rule will not apply in this case, but a note will be made on the patient’s record to review within 6 months) If the earlier DTA is the highest priority procedure to be undertaken, then the waiting list episode relating to the later DTA will be suspended NB no suspensions with 18 weeks from the date of the TCI for the highest priority procedure with a review date allowing enough time for the patient to recover from this procedure (the maximum 60 day suspension rule will not apply in this case, but a note will be made on the patient’s record to review within 6 months). If the DTA for both procedures are made at the same time, then the lowest priority procedure to be undertaken will be treated as a “planned” procedure and so will go onto the planned waiting list. Bilateral procedures - initial surgery on one side at first admission and subsequent admission for a second side. The patient will be added to the waiting list for the first side and put on a planned list for the second procedure. Structure of Inpatient/ Day Case Waiting Lists To aid both the clinical and administrative management of the waiting list, the lists are sub-divided into the following: o Active Waiting Lists - consists of patients awaiting admission who are available to come in. o Suspended/Deferred Waiting Lists – patients who are already on the waiting list but become unsuitable for admission for clinical or social reasons. o Planned Waiting Lists - patients who are waiting to be recalled to hospital for a further stage in their course of treatment or investigation. Examples include: D:\533567122.doc ‘Check’ endoscopic procedures The second procedure for bilateral operations Removal of screws/metal work Age/growth related surgery Investigation/treatment sequences. 8 Suspended Waiting List Suspended patients will not count as waiting for statistical purposes. Any periods of suspension will be subtracted from the patient’s total time on the waiting list for Körner returns. No single suspension period may exceed 60 days. In the event that a patient will remain either clinically or socially unavailable for a period of greater than 60 days the patient must be removed from the waiting list and returned to the referring general practitioner. This terminates the patient’s period of wait, with any subsequent referral regarded as a new episode of care (therefore constituting a new decision to admit). Types of suspension Suspension for Social Reasons (always linked to a clock pause) Some patients may not be available for admission due to social/personal reasons, e.g. holidays, work commitments. In order for a social suspension to be considered, notification of unavailability must be made in advance of any offer of admission. Any other circumstance will be considered a self-deferral. Suspension for Clinical Reasons Patients who, following a clinical assessment, are deemed medically unfit to be admitted will be clinically suspended or removed from the waiting list if this period of unavailability will be more than 60 days. Offer Rejections & Patient Cancellations Patients who cancel their admission date or decline a reasonable offer (i.e., within 21 days notice as per national guidance) of an admission date will be considered to have self rejected. In this event the patient's current date on waiting list (CDOL) will be adjusted to the date of self rejection (national guidance allows the CDOL to be adjusted to the admission date or the offer date, but the Trust has adopted a practice that ensures that patients do not wait longer than is necessary). The patient must be given a re-arranged date at the time of deferral. If a patient self rejects more than once then they should be removed from the waiting list. In the case of children and known vulnerable adults, the consultant must be consulted with, it is their decision whether the patient is removed from the waiting list or not. (anyone - does this read okay) D:\533567122.doc 9 Clock Pauses A clock may be paused only where a decision to admit has been made, and the patient has declined at least two reasonable appointment offers for admission. The clock is paused for the duration of the time between the earliest reasonable offer and the date from which the patient makes themselves available again for admission. Patients Admitted and Discharged with Treatment Cancelled If the patient is admitted to hospital but their treatment is cancelled for non-clinical reasons and discharge to their place of residence, a new TCI date must be agreed within 28 days of the cancelled appointment/ operation date. If the patient rejects this offer, then every reasonable attempt should be made to admit the patient at their convenience. Escalation In the event that emergency pressures compromise planned admissions, each clinical team must, on a daily basis, review its admission list and only prioritise patients: o Whose care meets NCEPOD category 3 (urgent); this includes cancer patients; o Who will exceed the maximum waiting time permitted; o Who have been cancelled on the day of admission and need to be treated within 28 days. If, after prioritisation the number of patients across all specialties exceeds capacity, the Clinical Director: Clinical Support Services will agree which patients will be admitted after discussion with the consultants or specialist registrar. D:\533567122.doc 10 DIAGNOSTIC PROCEDURES To ensure a procedure is accurately recorded and coded as Diagnostic, and reported in the diagnostic return, the referral form must be accurately completed to identify whether the procedure to be performed is diagnostic or therapeutic. If the procedure is both Diagnostic and Therapeutic, the diagnostic box on the form must be ticked as the priority to ensure the procedure is monitored to meet the diagnostic waiting time and reported in the diagnostic return. If the box is not ticked, then the form must be returned to the referring clinician for clarification. D:\533567122.doc 11 18 WEEK REFERRAL TO TREATMENT GUIDANCE By December 2008 all patients will be required to be treated or discharged within 18 weeks from the time a provider receives notice of the patients referral or the date of a consultant’s decision to start the clock. Or when the patient converts their Choose and Book unique booking reference number (UBRN). Their clock will continue until the patient is given, or admitted for, a definitive treatment or is discharged. There may be clock stops and starts along the way. A referral made to the wrong clinic or specialist and has to be re-referred, will not stop the clock. There are no suspension periods in the 18 week pathway. Further information about Clock Starts, Clock Pauses and Clock Starts can be obtained from the 18 week website “The 18 week rules suite - National Clock Rules”. D:\533567122.doc 12 DEFINITIONS For the purposes of this guidance, the following terms have the meanings given below: Attendance & Clinic Outcomes This is the process, following an outpatient attendance, of ensuring that the correct outcome is recorded on PAS. Active Waiting List Patients awaiting elective admission for treatment and are currently available to be called for admission. Booked Patients Patients awaiting elective admission who have been given an opportunity to negotiate a date. These patients form part of the active waiting list. C&B Direct Booking System Patient booked through Choose & Book at the GP surgery and given an appointment at that time. Day Cases Patients who require admission to the hospital for treatment and will need the use of bed but who are not intended to stay in hospital overnight. Did Not Attend (DNA) Patients who have been informed of their admission date (inpatients/day cases) or appointment date (outpatients) and who without notifying the hospital did not attend for admission/ OP appointment. First Appointment This is the first chronological appointment with a specific clinician. Follow up Appointment The patient has been seen in outpatients by the same clinical team within the same pathway, then it is a ‘Follow-Up’ appointment Full Booking Fully booked patients are those whose admission date is negotiated at the time of the decision to operate Inpatients Patients who require admission to hospital. New Referral This is the first outpatient referral at this hospital to a clinician, even if the consultant has already seen the patient as an admitted patient Outpatients Patients referred by a general medical practitioner, general dental practitioner, another consultant, optometrist or other for clinical advice or treatment provided in an ambulatory setting. D:\533567122.doc 13 Partial Booking Partially booked patients are those who are added to a waiting list and contacted prior to their expected admission/attendance date and invited to negotiate a date. Planned Admissions Patients who are to be admitted as part of a planned sequence of treatment or investigation. They may or may not have been given a firm date. Pooled waiting list Specialties/ subspecialties where more than one clinician performs the service will be considered as one waiting list. Referrals will be allocated to the clinician with the shortest wait. Self-rejections Patients who, on receipt of reasonable offer(s) of admission, notify the hospital that they are unable to come in. Suspended Waiting List A list of patients awaiting elective admission who are currently unsuitable for admission due to some underlying medical or social reason. D:\533567122.doc 14 WAITING TIME STANDARDS IN 2007/ 08 There will be a maximum wait from GP referral to first treatment (18 RTT) of 18 weeks from December 2008. Within this, there are stage of treatment maximum targets that state that no patient will wait longer than: The National stages for 2008/ 09 are that no patient will wait longer than: o 13 weeks for an outpatient appointment o 26 weeks for inpatient or day surgery treatment o 6 weeks for a diagnostic test. The Trust also has milestones for stage of treatments, which are: o 5 weeks for first outpatient appointment o 11 weeks for inpatient or day surgery treatment D:\533567122.doc 15 LIST OF PROCEDURES SUPPORTING THIS GUIDANCE WL(OP)1 – Procedure for Registering and Adding Patients to the Out Patient Waiting List WL(OP)2 – Procedure for Booking Routine Paper Based Outpatient Appointments WL(OP)3 – Procedure for Booking Urgent Paper Based Outpatient Appointments WL(OP)4 – Procedure for Booking Cancer Outpatient Appointments in the Sarcoma Unit (Stuart) WL(OP)5 – Procedure for Cancelling Outpatient Appointments and Clinic: (a) hospital initiated cancellation and (b) Patient initiated cancellation WL(OP)6 – Process for limiting number of clinics throughout year/ ensuring less than 52 are booked (Siobhan) WL(OP)7 – Procedure for Recording Outpatient Outcomes (AADs) Attendance and Disposal WL(OP)8 – Checking MDS from third party i.e. tertiary WL(OP)9 – Sending MDS WL(IP)9 – Procedure for adding patients to the Trust Waiting List WL(IP)10 – Procedure for suspending Patients on Inpatients / Day Case Waiting List WL(IP)11 – Procedure to record TCI (to come in date) WL(IP)12 – Procedure for cancelling and rebooking a TCI (to come in) date WL(IP)13 – Procedure for dealing with cancellations: (a) Hospital Initiated Cancellation and (b) Patient Initiated Cancellation WL(IP)14 – Procedure for dealing with rejections WL(IP)15 – Procedure for dealing with Theatre Review WL(IP)16 – 28 Day cancellation and rebooks (Kim) D:\533567122.doc 16 WL(Dx)17 – Procedure for booking OPD Procedures (Pauline) WL(Dx)18 – Procedure for Ensuring Patients are Correctly Coded for Diagnostic Procedures (Pauline) WL(WLM)19 – Procedure for managing and auditing waiting lists WL(WLM)20 – Escalation of breaches and potential breaches D:\533567122.doc 17