211-RH-Typing - The Indian Immunohematology Initiative
advertisement

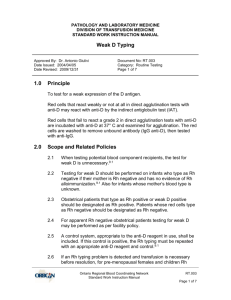
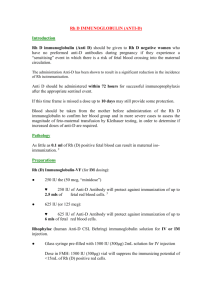
Procedure number: 211 (Blood Bank Name and address) Page 1 of 4 Subject: Rh Typing RH TYPING PURPOSE To determine the Rh type of blood donors and recipients. PRINCIPLE Due to its high immunogenicity and the ability of anti-Rh to cause severe hemolytic disease of the fetus or newborn (HDFN), after A and B, the Rho(D) antigen is the most important blood group in transfusion practice. Errors in correct Rh designation of blood donors or recipients can result in severe HDFN, so correct interpretation, recording, and transcription of results is of utmost importance. The reagents typically used for determination of the Rh-type of donors and patients are commercially prepared blends of monoclonal IgM anti-Rho(D) and polyclonal IgG anti-D, in relatively low protein diluents. Because a strong potentiating diluent is not needed with these reagents, a negative ABO typing tube will serve as a negative control (to detect non-specific agglutination of test RBCs heavily coated with auto- or alloantibody) so an additional negative control tube is only required when the patient is group AB (and Rh positive). When the latter is the case a control (Rh control) using 6% albumin or patient seum/plasma is tested along with the anti-D. Check the manufacturer’s package insert to verify what type of Rh control is required. Commercial anti-D reagents correctly identify over 90% of all Rh-positive red cell samples. Rh positive red cells which do not react in direct agglutination tests (“immediate spin”) with such reagents, but which will react when an indirect antiglobulin test (IAT) is employed are considered to have a variant of the D antigen termed "weak D" (previously “Du”). The “weak D test” is an IAT using a polyclonal IgG-containing anti-D reagent. If other anti-D sera are used in a special case, the manufacturer's instructions must be followed. Blood donors who appear Rh negative on initial testing must have a weak D test since mis-classification of a donor with a weak form of the Rh antigen could lead to anti-D formation in a true Rh negative recipient of such weak D RBCs. Similarly, a weak D fetus could immunize his or her mother, so umbilical cord blood workups should include a weak D test. However, if weak D patients having a transfusion are misclassified as Rh negative, the only harm that will result is the unnecessary use of Rh negative RBCs. Finally, the weak D test may be very weakly positive (<2+) in Rh negative women at delivery when there is a massive fetal maternal hemorrhage. In such a case a Kleihauer–Betke test should be done to detect fetal RBCs. Some patients with weak D typing results lack a portion of the D antigen (“partial D) and can become immunized to the portions of the antigen they lack. This is an issue for pregnant women, women of childbearing age, and girls, since such antibodies can rarely cause HDFN. Identification of partial D patients requires special reagents or genetic methods, so it may be best to treat such patients as Rh negative with respect to transfusion and Rh immune globulin administration. Note however that some partial D RBCs will NOT have a weak D phenotype. Rh (and ABO) typing on patients is recorded on a Patient Blood Bank Record form and filed indefinitely. Donor Rh (and ABO) typing is recorded on the Blood Donor Processing Record and transcribed to the Blood Donor Record. POLICIES (See also General Rules for Serologic Testing, procedure #201) 1. A weak D test must be performed on all donors who appear Rh-negative or demonstrate weak reactivity (<2+) on initial testing. Confirmatory testing does not require a weak D test. 2. A weak D test is also performed on all umbilical cord blood samples when the initial immediate spin reaction is negative or demonstrates weak reactivity (IS reaction <2+). A weak D test is not required for patients having pre-transfusion testing or for prenatal patient investigations. Procedure number: 211 (Blood Bank Name and address) Page 2 of 4 Subject: Rh Typing 3. For new patients without a previous blood type the ABO and Rh type must be repeated, including preparation of a new RBC suspension. 4. An Rh control tube is required for group AB, Rh positive individuals. 5. A DAT is required for individuals who test negative or demonstrate weak reactivity (< 2+) with anti-D at immediate spin, but who have a positive weak D test. MATERIALS AND SPECIMENS See General Guidelines for serologic testing, procedure # 201 Patient Blood Bank Record, appendix 210.1 PROCEDURE Rh typing is ordered with ABO testing in routine cases. 1. Prepare a 3-5% suspension of the red cells to be tested (See procedure #202). 2. Properly label a 10x75 or 12x75 mm test tube. 3. Place one drop of antiserum to the tube marked anti-D. (If the patient or donor is group AB, also place one drop of 6% albumin, patient/donor serum/plasma, or other appropriate Rh control reagent as defined by the manufacturer in a second tube marked "control" as outlined in procedure #210). 4. Add one drop of the cell suspension to be tested to the tube(s). 5. Mix, then centrifuge at the proper speed and time for the serofuge in use. 6. After centrifugation, examine for agglutination, and record the reactions in the column labeled anti-D. 7. If the immediate spin reaction is positive (2+ or greater), document your interpretation. If the immediate spin reaction is negative (or < 2+), document the reaction strength and continue with the weak D test if appropriate (see policies). If the patient/donor is AB pos, an Rh control with 1 drop of 6% albumin or patient serum/plasma and 1 drop of RBC suspension is required as part of the ABO grouping procedure. Weak D Testing Weak D RBCs are demonstrated by increasing the sensitivity of hemagglutination testing by using an antiglobulin test phase after incubation of the cells with anti-D serum. Therefore, red cells already sensitized with immunoglobulin (a positive DAT) will be agglutinated and are not suitable for weak D testing. 1. Incubate for 15-30 minutes at 37oC the test tube which, at immediate spin, was negative with anti-D. 2. Wash the tube 4 times with saline. This can be performed manually or in the automatic cell washers. 3. After the final wash, add 1-2 drops of monospecific anti-human IgG serum to the tube(s) and mix. 4. Centrifuge at the appropriate speed for the serofuge in use. 5. After centrifugation, examine the tube(s) for macroscopic agglutination. Record and interpret the reactions. Procedure number: 211 (Blood Bank Name and address) Page 3 of 4 Subject: Rh Typing 6. If the reaction is now positive, perform a DAT on the test cells (see procedure #215). 7. Add one drop of check cells (CC) to any tube which gave a negative reaction. 8. Centrifuge, read and record the results for CC. 9. Interpret the results as listed below. Repeat Testing for New Patients If the patient has never had a previous Rh (and ABO) typing at this institution repeat Rh typing must be done as follows. A weak D test is not required for patients who are negative on immediate spin testing. 1. Discard the previously used RBC suspension. Verify the patient identifiers on the primary and plasma tubes. Then prepare a new RBC suspension (see procedure #202). 2. Label a new 10x75 or 12x75 mm test tube from the ORIGINAL patient specimen. 3. Resolve any discrepancies between initial and repeat results. INTERPRETATION OF RESULTS The commercial sera are prepared to give a 2+ to 4+ reaction with the anti-D either after immediate spin or a weak D test, and negative reaction (O) with any controls needed. Further investigation and testing is necessary for any test that does not result in a 2+ to 4+ reaction. Immediate Spin Interpretation: Anti-D Rh control Interpretation Comment +* 0 Rh positive 0 0 Rh negative Continue with weak D test + + Invalid Test See discrepancies (below) *If the strength of reaction with the test cells is not 2+ or greater, perform a weak D test on the cells. Interpretation of the weak D TEST Anti-D (AHG) DAT Interpretation + 0 Rh positive 0 Not tested Rh negative + + Invalid Test Comment See discrepancies (below) If the weak D test result is not 2+ or greater, repeat the test with a different manufacturer's anti-D reagent. If the weak D test reaction with the second anti-D reagent is also weaker than 2+ or non-reactive, refer the problem to a supervisor or a blood bank physician. Procedure number: 211 (Blood Bank Name and address) Page 4 of 4 Subject: Rh Typing Discrepancies and problems 1. Improper and inadequate washing of the red cell suspension may cause pseudoagglutination due to the presence of serum macromolecules in the suspension. This should cause a positive control as well. 2. The presence of strong autoagglutinins in the patient's or donor's serum may cause agglutination. Proper washing and the control are designed to prevent or detect this problem. 3. Antibody coating of the red cell (positive DAT) can cause a false positive reaction, particularly in the weak D test. A DAT will detect this occurrence. 4. A false negative reaction may be seen due to the "blocking phenomenon". This occurs most commonly in HDFN due to anti-D. Since the red cell's antigen sites are heavily coated with maternal antibody, they may not react with the antiserum. 5. False positive or negative reactions may occur in the Rh test due to many of the technical errors and conditions listed in procedure #201. 6. RBCs that react with one manufacturer’s anti-D reagent but not with another may have a partial D antigen. Resolution 1. If transfusion is required before resolution of discrepant results, issue Rh negative RBCs or whole blood. 2. If the immediate spin results are invalid due to a positive Rh control, repeat the test using a new suspension of RBCs washed twice with warm saline. 3. If the weak D test results are invalid due to a positive DAT and a weak D determination is necessary, treat the patient's RBCs with chloroquine or glycine-EDTA (see procedures #259 or 260), and repeat the DAT. if the DAT is negative the weak D test can be repeated. 4. Patients with weak D reactions less than 2+ are to be reported as Rh positive, but should be transfused with Rh negative cellular components pending serologic and clinical evaluation. In particular, patients who react with one manufacturer’s anti-D reagent but not with another may have a partial D antigen. Notify a supervisor or blood bank physician. 5. Donors with weak D test reactions less than 2+ are labeled as Rh positive. Adopted Reviewed Reviewed Reviewed Reviewed Reviewed Reviewed Reviewed Reviewed Reviewed Reviewed Reviewed