Unit 11 Neonatal and Obstetrical Transfusion Practice – Part 2
advertisement

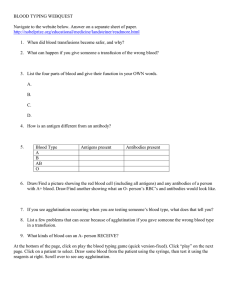
Unit 11 Neonatal and Obstetrical Transfusion Practice – Part 2 Terry Kotrla, MS, MT(ASCP)BB Laboratory Investigation During Neonatal Period Sample of cord blood obtained. Avoid contamination with Wharton’s jelly. Wharton’s jelly is a gelatinous substance which protects umbilical cord. If it contaminates blood it will coat cells and cause false positive in forward type. If false positive obtained wash thoroughly and repeat test. Laboratory Investigation During Neonatal Period Tube is labeled in delivery room with MOTHER’S information. Labeled as “Cord Blood” Her name Her ID number Date and time of collection which is the birth. Kept in blood bank for 7 days. Laboratory Investigation During Neonatal Period Antepartum, postpartum testing on mother. ABO, D and antibody screen on mother. During first prenatal visit. At hospital during delivery If screen positive,identify alloantibodies. Determine clinical significance of alloantibodies and notify physician if significant. If significant, follow with titers during pregnancy Laboratory Investigation During Neonatal Period Cord blood Determine ABO/D if indicated Some hospitals perform ABO/D on cordbloods of all group O mothers, if baby A or B then DAT is done. All cord bloods from D negative mothers must be typed, if D positive mother must receive RhIg False positive may occur (types as AB pos with pos D control) due to Wharton’s jelly, repeat on thoroughly washed rbc sample. Laboratory Investigation During Neonatal Period Cord blood May get false negative with anti-D when mother has immune anti-D and baby is D positive. Every D antigen site on the baby’s rbcs gets coated with maternal anti-D leaving no sites available for reagent anti-D to attach. Weak D test and D control will be STRONGLY POSITIVE as the immune anti-D is IgG and will react with AHG. Laboratory Investigation During Neonatal Period Cord blood DAT Some hospitals perform DAT on all cord bloods. Others will perform only if necessary, mom has clinically significant immune antibody. group O mother has A or B baby. Immune antibodies cause strongly positive DATs if infant is antigen positive. ABO is very, very weak. Laboratory Investigation During Neonatal Period Positive DAT and cord blood elutions Rarely performed any more. If mom is group O with negative antibody screen and baby is A or B comment “positive DAT probably due to maternal ABO antibodies”. It is possible to elute immune anti-A, -B or –A,B off any ABO incompatible baby regardless of results of DAT. Immune antibodies elution usually performed. Laboratory Diagnosis of ABO HDFN HDFN caused by ABO incompatibility is clinically mild, with jaundice most frequently developing within 24 hours of birth. Laboratory Diagnosis of ABO HDFN Profile - MEMORIZE T&S on mom – Mom group O, screen neg DAT on cord cells, weakly positive ABO/D type on cord cells is A or B Elution testing on cord cells – anti-A or –B &A,B eluted. Bilirubin on infant – 12 mg/dL or more Transcutaneous Monitoring Transcutaneous bilirubinometry screening tool for jaundice in well, full-term babies. If elevated blood test will be ordered. Leads to approximate 50% decrease in blood testing. Laboratory Diagnosis of ABO HDFN Profile - MEMORIZE H&H on infant – decreased. Infant peripheral smear – hypochromia, polychromasia, NRBCs and microspherocytosis. Reticulocyte count on infant – increased. Treatment of ABO HDFN Except in the extremely rare cases of severe HDFN produced by ABO incompatibility, phototherapy with UV light is the usual treatment. UV light converts bilirubin into nontoxic isomer photobilirubin, transported to liver. Photobilirubin rapidly excreted in the form of bile. Phototherapy – Light Therapy Isolette with UV lights Therapy uses blue light (420-470 nm) that converts bilirubin so it can be excreted in the urine and feces. Blinders protect baby’s eyes from damage that may lead to retinopathy Usually do not wear diaper. Can be done at home. Phototherapy – Bili Blanket Much more humane. Lightweight, fiberoptic pad delivers up to 45 microwatts of therapeutic light for treatment of jaundice while allowing infant to be swaddled, held and cared for by parents and hospital staff. Compact unit can be used for hospital and homecare. Bilirubin Degradation by Phototherapy Treatment of ABO HDFN The need for exchange transfusion is RARE. Risk of mistake being made and giving baby their own A or B type, triggers more hemolysis. Blood for exchange must be: Compatible with baby AND mother. D compatible with infant. “Other” Hemolytic Disease Uncommon, occurs in ~0.8% of pregnant women. Immune alloantibodies usually due to anti-E, -c, Kell, -Kidd or -Duffy. Anti-K disease ranges from mild to severe over half of the cases are caused by multiple blood transfusions is the second most common form of severe HDN Anti-M very rare Laboratory Diagnosis of Other HDFN Profile - MEMORIZE T&S on mom – antibody screen is POSITIVE Immune antibody identified. DAT on cord cells is positive, strength varies. Elution testing on cord cells Test eluate against panel, specificity of antibody should be same as maternal antibody. If ABO incompatible test A and B cells as well. Bilirubin is determined and evaluated. CBC and reticulocyte determined and evaluated. Treatment of Other HDFN May be diagnosed prenatally. Depending on antigen strength on baby’s cells and other variables disease ranges from mild to severe. MOST cases require phototherapy. RARELY exchange transfusion necessary. Blood must be compatible with baby & mother. Lack all antigens to which she has antibodies. Rh (anti-D) Hemolytic Disease Early 1930’s classic observations of kernicterus, hydrops fetalis and anemia termed erythroblasosis fetalis. 1938 suggested the cause was transfer of immune antibodies, incorrectly assumed fetal hemoglobin was target. With discovery of D antigen led researchers to correctly identify the cause. Immunization to D Antigen Immunization to D depends on dose of D pos rbcs and ability to respond to the antigen. One third of individuals are non-responders. Two types of responders Differ in terms of type and quantity of anti-D. Hyperresponders produce extremely high titers of both IgM and IgG anti-D Immunization to D Antigen Caused by exposure to D pos rbcs through transfusion or pregnancy with D pos fetus. Subsequent exposure, such as pregnancy with D pos fetus, elicits secondary immune response. Characterized by ↑ titers of IgG anti-D. Immunization to D Antigen Immunization to D Antigen Was noted in 1943 that ABO incompatibility between mother and fetus reduced chance of immunization to D. Maternal ABO antibodies present naturally. Cause destruction of A or B cells before her immune system has chance to recognize D antigen as foreign. Anti-D (Rh) HDFN If the current pregnancy is the immunizing event seldom clinical signs of HDFN. Primary immune response – IgM If progression to IgG DAT will be positive. Antibody titer not high enough to cause severe hemolysis. If this is first pregnancy and HDFN is severe MUST have had previous exposure. Anti-D (Rh) HDFN Maternal IgG anti-D destroy fetal D positive red blood cells Baby's responds to hemolysis by trying to make more red blood cells very quickly in the bone marrow and the liver and spleen. Results in anemia. Anemia limits the ability of blood to carry oxygen to baby's organs and tissues. Organs enlarge - hepatosplenomegaly. New red blood cells released prematurely from bone marrow and are unable to do the work of mature red blood cells. As the red blood cells break down, bilirubin is formed. Babies unable to get rid of the bilirubin. Builds up in the blood (hyperbilirubinemia ) and other tissues and fluids of the baby's body resulting in jaundice. The placenta helps get rid of some of the bilirubin, but not all. Prenatal Diagnosis of Anti-D HDFN Detectable antibody titer rarely observed before 28 weeks if THIS is the immunizing event. Usually detectable at 35th week or later. Titer low. Subsequent pregnancy with D pos fetus Anti-D titer of 16 or ↑ with previous affected child or 64 without history indicates affected fetus. Amniocentesis performed at 24-28 weeks OR 6-8 weeks prior to previous fetal loss to assess fetal status. Complications During Pregnancy Severe anemia with enlargement of the liver and spleen When these organs and the bone marrow cannot compensate for the fast destruction of red blood cells, severe anemia results and other organs are affected. Hydrops Fetalis This occurs as the baby's organs are unable to handle the anemia. The heart begins to fail and large amounts of fluid build up in the baby's tissues and organs. A fetus with hydrops is at great risk of being stillborn. Hydrops Fetalis Anti-D (Rh) Clinical Presentation Varies from mild jaundice and anemia to hydrops fetalis (with ascites, pleural and pericardial effusions) Chief risk to the fetus is anemia. Extramedullary hematopoiesis due to anemia results in hepatosplenomegaly. Risks during labor and delivery include: asphyxia and splenic rupture. Postnatal problems include: Asphyxia Pulmonary hypertension Pallor (due to anemia) Edema (hydrops, due to low serum albumin) Respiratory distress Coagulopathies (↓ platelets & clotting factors) Jaundice Kernicterus (from hyperbilirubinemia) Hypoglycemia (due to hyperinsulinemnia from islet cell hyperplasia) Infant Laboratory Findings Mom - T&S will reveal positive antibody screen. Anti-D is the commonest form of severe HDN. The disease varies from mild to severe. May have additional Rh antibodies present, i.e., anti-C or anti-E. Infant - Vary with severity of HDN and include: Anemia Hyperbilirubinemia Reticulocytosis (6 to 40%) ↑ nucleated RBC count (>10/100 WBCs) Thrombocytopenia Leukopenia Positive Direct Antiglobulin Test Hypoalbuminemia D negative blood type Smear: polychromasia, anisocytosis, no spherocytes Blood Smear Polychromasia Anisocytosis Increase NRBCs no spherocytes End of Unit 11- Part 2