A 25-year-old woman was admitted with a swollen left calf
advertisement

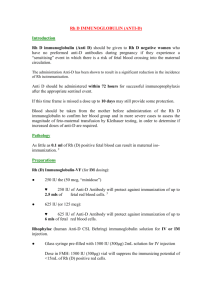
1 A 25-year-old Saudi woman was admitted with a swollen left calf. She had been taking an oral contraceptive pill containing 30 ug of oestrogen. There was no past, or family history of venous thromboembolism. A venogram demonstrated thrombosis up to the left iliac vein. The contraceptive pill was stopped. A coagulation screen was performed and found to be normal. Treatment was started with intravenous heparin. Two days later a citrated blood sample was taken and the results shown in Table. Question a a Interpret the results and offer possible explanations for the abnormalities. After six days of intravenous heparin the patient was started on warfarin and stabilised to give a prothrombin ratio of 2.5 International Normalised Ratio (INR). After three months a further citrated blood sample gave the results shown in Table. Questions b, c b Interpret these results. c How would you manage this patient now? Results from a citrated blood sample taken two months after stopping warfarin are shown in Table. Questions d, e d Interpret these results. e How would you manage this patient in future? 2 a The antithrombin III level is markedly reduced. This suggests congenital antithrombin III deficiency. However, heparin therapy itself can lower the level and may be the explanation. The protein C level is within the normal range, which extends down to levels that might be considered as pathological for other coagulation inhibitors. The protein C level increases with age, but levels in the region of 68% are within the normal age-specific range for a 25-year-old female.The free protein S level is reduced, probably due to the oral contraceptive. This and pregnancy are associated with lower concentrations. b The antithrombin III level is still reduced in the absence of heparin providing more evidence for congenital antithrombin III deficiency. The protein C and S levels are reduced. This is because both are vitamin K-dependent proteins and their concentrations fall in patients on warfarin. c Warfarin should be continued for a total of six months. A further citrated blood sample should be obtained two months after stopping warfarin. d The antithrombin III activity level remains low, but the antigen concentrate is normal. This patient therefore has type II antithrombin III deficiency. The protein C and S are now both normal. e It is necessary to consider whether or not this patient should be on long- term warfarin therapy. As she has only had a single deep vein thrombosis (DVT) that might have been precipitated by the oral contraceptive it would be reasonable to withhold war- farm. If, however, she develops a further DVT without provocation, there would be a stronger argument for starting long-term warfarin. The patient will need to be advised that there is an increased risk of developing a DVT if she becomes pregnant. During subsequent pregnancies she should receive subcutaneous heparin. There are no firm guidelines about the use of antithrombin concentrates in pregnancy. Although some would recommend starting regular infusions at 32 weeks’ gestation, others would give the concentrate just over the delivery period and continue it for several days after delivery until the patient is fully warfarinised. Warfarin should then be continued for six months. As antithrombin III deficiency is an autosomal dominant disorder, it is important to screen the patient’s parents and siblings for the deficiency. 3 A 31-year-old Saudi woman attends the Ante- natal Booking Clinic. She is 12 weeks pregnant. Her obstetric history is gravida 3 para 0. She received a transfusion of two units of blood 12 years ago following a major road traffic accident. Results of investigations were as follows: • group and screen A Rh-negative; antiD and anti-Kell present. Questions a—c a How do you explain the presence of the antibodies in the mother’s serum? b Is further testing indicated at this stage? c How regularly would you see the mother during the pregnancy? The mother is regularly reviewed during the pregnancy. Her anti-D levels are given in Table. Question d d At what stage is amniocentesis indicated? The results of serial amniocentesis are shown in Figure 109. Questions e, f e Should induction of labour be considered? f What further helpful result can amniocentesis provide which will assist your decision? 4 At birth: • the baby is found to be A Rh-positive; • direct Coomb’s test was positive on cord cells; •Hb9.8g/dl; • bilirubin 120 imol/l; • red cell eluate reveals anti-D and antiKell; • maternal screen reveals anti-D and anti-Kell. Questions g—i g Should the baby receive any further treatment? h Is the anti-Kell contributory to the haemolytic disease of the newborn? i Should the mother receive prophylactic anti-D? a The presence of the antibodies can be explained by the history of previous transfusion and previous pregnancies. b Further testing is indicated. Both mother and father should be genotyped and the anti-D antibody should be quantified. It is also possible in specialist centres to determine blood group at 12 weeks’ gestation by chorionic villous biopsy, or from 18 weeks onwards by fetal blood sampling. The haemolytic potential of the anti-D can be assessed by macrophage phagocytosis assay or an antibody-dependent cell-mediated cytotoxic assay, which appears to correlate more closely with clinical outcome than the anti-D level per Se. In this case, the genotype of the mother was rrkk and the genotype of the father was R2rkk. c The mother should be reviewed at monthly intervals. d Amniocentesis is indicated at 24 weeks’ gestation (i.e., when the anti-D is 4 lU/mi). It is worth noting that this baby may have an R2 phenotype, which is more susceptible to haemolytic disease than RI phenotype. e Induction of labour should be considered at 35 weeks. 5 f Amniocentesis can also determine the lecithin/sphingomyelin ratio, which should he greater than 2 for safe induction. g The Hb and bilirubin indicate that the baby should receive an exchange transfusion. h The anti-Kell is unlikely to be contributory to the haemolytic disease of the newborn, since both mother and father are Keli-negative. Unless there is a problem with paternity, the baby should also be Kell-negative. The Kell phenotype of the baby can be easily checked. The presence of the anti-Kell on the baby’s red cells is due to IgG placental transfer. i There is no point in administering anti-D immunoglobulin to the mother.