11th Annual Conference – Women`s Health and Suicide
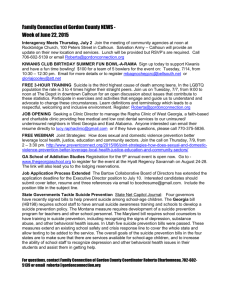
advertisement

11th Annual Conference Women’s Health and Suicide West County Hotel, Ennis 29th – 30th September, 2006 Board Members of the Irish Association of Suicidology President Mr. Dan Neville, T.D. Dail Eireann Chairperson Professor Michael Fitzgerald Consultant Psychiatrist Secretary Dr. John F. Connolly Consultant Psychiatrist Directors Dr. Justin Brophy Consultant Psychiatrist Dr. Anne Cleary Sociologist Mr. Michael Fahy ‘Solace’ Suicide Support Group Mrs. Mary Hutchinson Student N.I. Dr. Margaret Kelleher National Suicide Research Foundation Paul Kelly Console, Bereaved by Suicide Foundation Anne Kilgallen Public Health Consultant Prof. Kevin Malone Consultant Psychiatrist Mr Barry McGale Suicide Awareness Co-ordinator Ms. Eileen Williamson National Suicide Research Foundation Executive Officer – Ms. Josephine Scott Clerical Assistant – Ms. Angela Coleman THE IRISH ASSOCIATION OF SUICIDOLOGY AIMS AND OBJECTIVES The Association was founded in 1996 and among its aims and objectives are the following To facilitate communication between clinicians, volunteers, survivors and researchers in all matters relating to suicide and suicidal behaviour To promote awareness of the problems of suicide and suicidal behaviour in the general public by holding conferences and workshops and by communication of relevant materials through the media To ensure that the public is better informed about suicide prevention To support and encourage relevant research To encourage and support the formation of groups to help those bereaved President: Mr. Dan Neville, T.D. Chairperson: Prof. Michael Fitzgerald Consultant Psychiatrist Secretary: Dr. John Connolly Consultant Psychiatrist Conference Objectives To develop an understanding of the management of deliberate self harm Insight into the relationship of developmental factors and suicide Awareness of the growing problem of suicide in young women Welcome Note Dear Delegates The 11th Annual Conference of the Irish Association of Suicidology has as its theme “Women’s Health and Suicide”. The male to female differential in suicide rates holds in all countries suggesting that culturally defined gender roles and expectations may be important variables both across and within different societies. It varies from 1.1 in China to 6.7 to 1 in the Russian Federation. In European terms, Ireland ranks second to the Russian Federation having an overall male to female differential of 4.7 to 1 in 2002. In Ireland the total rate of female suicide has remained fairly constant since 1990. However, the number of young women aged 15 to 24 who have died by suicide has trebled from 1990 to 2004. Prior to 1980 the Irish female suicide rate was stable, at 2 deaths per 100,000, when there was a marked increase to a figure of 7 per 100,000 in 2001. A modest decrease in suicide rates in females over 65 years of age has been reported in Ireland since 1990, possibly due to improved attitudes toward retirement; improved social services; enhanced psychiatric care for older people; greater economic security and greater socio-political activism for the elderly (de Leo 1998) –suicide among the over-75s being an indication of inadequate support and poor medical care. In 2004, there were 5,850 episodes of self harm of women presenting at accident and emergency which was 37% higher than the male rate. There were 58 incidents of females self harming for each completed suicide. The figure for males was 13. The complexities and challenges of female suicide will be explored in depth during the course of the conference. The bereavement seminar which is presented in conjunction with CONSOLE, the suicide bereavement support organisation which was set up by families that experienced the grief on loosing a loved one through suicide, will take place on Saturday and will add to our knowledge of the traumatic experience of families of those who take their lives. It is now 10 years since the Irish Association of Suicidology was incorporated. It is a time to take stock and plan for the future development of the organisation. I welcome delegates’ views on this and look forward to ideas on how the association will contribute to suicidology into the future and to reflect on how it has met with its aims and objectives as set out in 1996. We welcome you to Ennis and I am confident that the conference will add to our knowledge of suicide and in particular in relation to women’s health and suicide. Dan Neville TD, President, Irish Association of Suicidology OPENING ADDRESS Ms. Brid Clarke CEO Mental Health Commission Thank you for the invitation to attend your 11th annual conference. This year is the 10th anniversary of the formation of the Irish Association of Suicidology (IAS). In these ten years, the Association has taken the lead in raising awareness about the incidence of suicide and factors that contribute to suicide and suicidal behaviour, in supporting groups and communities affected by suicide and in promoting research. This year’s conference on Women’s Health and Suicide will add to our knowledge and awareness of this important area. The Mental Health Commission was established in 2002 pursuant to Section 33 of the Mental Health Act 2001. The overarching statutory functions of the Mental Health Commission are twofold:- to promote, encourage, and foster the establishment and maintenance of high standards and good practices in the delivery of mental health services and To take all reasonable steps to protect the interests of persons detained in approved centres. I will be focusing in my address on certain aspects of our mental health services. The risk factors for suicide are multiple and typically people who die by suicide experience more than one risk factor. While acknowledging the prevalence of mental illness among those who die by suicide it is important to recognise that the vast majority of people with a mental illness will not die by suicide. Most persons with a mental health problem do not experience the life stresses or other risk factors that contribute to suicide risk or they receive appropriate support and interventions. In recognition of the fact that mental illness is an import factor that can predispose people to suicidal behaviour especially in western countries, the World Federation for Mental Health has designated the theme for this year’s World Mental Health Day – 10th October – as “Building Awareness – Reducing Risk: Mental Illness and Suicide”. This theme was picked in recognition that suicide is a key public health problem in many countries. The World Health Organisation estimates that there are one million deaths by suicide each year, representing 1.4% of the total global burden of disease. The World Federation of Mental Health has collaborated with the International Association for Suicide Prevention to jointly promote World Suicide Prevention Day which was held on September 10th and World Mental Health Day which will be held on October 10th. It is hoped that this collaboration will promote awareness, reduce stigma and promote service and policy advocacy. The Mental Health Commission, since 2003 has marked World Mental Health Day with a public seminar (free of charge) on the theme selected by the World Federation for Mental Health. This year’s seminar will have two key speakers: Mr. Dougie Paterson, National Operations Manager Choose Life National Strategy and Action Plan to prevent Suicide in Scotland. Theme: “Suicide Prevention in Scotland – Raising Awareness to Reduce Risk” Mr. Gareth O’Callaghan – Author and Broadcaster Theme: “Being Kind to your Mind” There is a greater awareness and consciousness of World Mental Health Day in Ireland and this is to be welcomed. To return specifically to the theme of this year’s conference, Women’s Health and Suicide, it is acknowledged that mental illness affects woman and men differently – some mental illnesses e.g. depression are more common in women. WHO estimated that 121 million people currently suffer from depression with 5.8% of men and 9.7% of women experiencing a depressive episode in any given year. The presentation of the illness varies between men and women and treatment outcomes also vary. Research studies have identified the risk and protective factors for mental health for women and how to improve treatment outcomes. We know that women are more likely to experience low social status, isolation and poverty. Frequently women have multiple roles as members of the workforce and assuming major responsibility for child care and caring for other family members. These factors can have an impact on women’s mental health. Research studies have also identified a number of areas which are important to ensuring positive outcomes for women availing of mental health services. One of the most important is ensuring the safety, privacy and dignity of the mental health service user. Mental health care in Ireland is generally provided in mixed sex environments. Access to women-only services and activities is very limited. Although some studies have advocated the development of single-sex units and single sex provision, exercising choice and ensuring the safety and dignity of women while availing of mental health services are recognised as effective strategies. Factors that protect women’s safety, privacy and dignity especially while receiving in-patient treatment include facilities/rooms that can be designated as access for women only during certain periods of time, bathroom facilities that are single-sex and appropriately located, providing information about the service in advance of admission and assigning responsibility for women’s safety, privacy and dignity to a senior staff member. Research studies both here and abroad have also reported on service users’ wish for choice in treatment interventions and choice of therapists. In the consultation process undertaken by the Mental Health Commission in 2004 to ascertain stakeholders’ views of what constitutes a quality mental health service, people availing of mental health services talked of the importance of having a choice and a range of treatment interventions. This included access to psychological, occupational and social care programmes as well as to medical care programmes, access to counselling, involvement with support groups and a holistic service which takes account of diet, social skills, education, work training. A recently published study commissioned by the Mental Health Commission from the Department of Applied Psychology, University College Cork, on the views of Adult Users of Public Sector Mental Health Services also echoed these views. We are moving from what has been called a paternalistic mental health service to one where service users are now advocating an active involvement in their own care and treatment programmes. Women have been to the forefront in expressing their wish to be listened to, be involved, be accepted as partners in their treatment. There is increasing evidence to support the recovery model within our mental health services. The recovery model emphasises personal growth, building self-esteem, autonomy, empowerment and having a meaningful role in society. The Association for Suicide Prevention has identified a number of strategies for suicide prevention which include improving mental health treatment and management. Mental health services in Ireland are facing a most significant period of change, with the commencement in full of the provisions of the Mental Health Act 2001 on 1st November 2006 and the implementation of the Government policy on mental health “A Vision for Change”. Mental health services will be based on the multidisciplinary team communitybased model with the service user central to the treatment programmes. The Mental Health Act introduces key protections for patients availing of mental health services, especially those who are involuntarily admitted. As you are probably aware, all people involuntarily admitted will have an automatic independent review of their admission. The review includes an examination by an independent consultant psychiatrist, appointment of a legal representative and a review of the admission order (or renewal order) by a three person mental health tribunal. These provisions bring Irish mental health law into conformity with the European Convention on Human Rights and Fundamental Freedoms. The Act also provides for the registration of all approved centres, the introduction of regulations for approved centres and rules for certain treatments. The Mental Health Act also places considerable emphasis on promoting quality and best practice in the mental health services. The Mental Health Commission will be rolling out the quality framework for the mental health services over the next few years, which will support continuous improvement in the quality of our mental health services. The quality framework will identify the essential attributes of a quality mental health service, describe how standards outlined in the framework can be attained and how these standards of care will be monitored and evaluated internally and externally. An exciting and challenging time faces us all in mental health services. To conclude, I wish to again acknowledge the work of the Association during the last ten years, wish you a successful and productive conference and look forward to ongoing partnership with the Association. Ms. Brid Clarke, CEO, Mental Health Commission, St. Martin’s House, Waterloo Road, Dublin 4 MICHAEL KELLEHER MEMORIAL LECTURE WOMEN AND SUICIDE ANNETTE BEAUTRAIS Principal Investigator, Canterbury Suicide Project, Christchurch School of Medicine Abstract Gender plays a glaringly predictive role in suicidal behaviour: In Western developed countries women are more likely to report suicidal ideation and suicide attempt while men are more likely than women to die by suicide. However, in a number of countries there are growing concerns that rates of suicide in females may be starting to increase, particularly amongst younger women. This trend suggests that suicidal behaviour in women should be a more significant focus for research and prevention than it has been thus far. Surprisingly little research to date has explored the risk, and protective, factors for suicidal behaviour in women. This paper examines the epidemiology of suicidal ideation, suicide attempt behaviour and suicide in women and explores the risk and casual factors which are associated with female suicidal behaviour. In particular, the role and contributions of exposure to childhood adversity (including sexual abuse), mental illness, marriage, pregnancy, postnatal depression, motherhood, social contact and support, substance abuse, domestic violence and personality disorders are discussed, particularly in the light of recent trends in suicidal behaviour among women. The implications of these findings for assessing, treating and managing suicide risk in women are examined. Implications for suicide prevention strategies are discussed. Prof. Annette Beautrais, Principal Investigator, Canterbury Suicide Project, Christchurch School of Medicine, PO Box 4345, Christchurch 8001, New Zealand CONSEQUENCES OF UNDER-TREATMENT OF PSYCHIATRIC ILLNESS DURING PREGNANCY AND THE POSTNATAL PERIOD: MATERNAL SUICIDE AND INFANTICIDE, DEPRESSION AND SUICIDE IN OFFSPRING VERONICA O’KEANE Head of Section Perinatal Psychiatry, Institute of Psychiatry, London Abstract I am a Perinatal Psychiatrist: a term that unfortunately many of you will not be familiar with because of the general absence of this specialty psychiatric service in Ireland. I run a service in London for the treatment of women with serious mental illness during pregnancy and in the first year following childbirth. This service is largely in-patient based: we have a 10-bed unit accepting referrals from all of the UK and we also run an out-patient clinic and an advisory service. An integral part of the service is to disseminate information to psychiatrists, GPs and obstetric colleagues about the identification and management of mental illness during the perinatal period. In this lecture I will address key issues in perinatal psychiatry: what psychiatric disorders occur during the process of reproduction? Are these disorders specific to this period? What are the treatments for these disorders? What are the consequences of these disorders for the mother and the family unit? What are the consequences of parental mental health problems for the developing baby and into adulthood? What are the consequences of parenteral mental ill-health on society at large and could this influence the rates of suicide? What service do we require in Ireland to address these problems? Psychiatric Disorders during the Perinatal Period Postpartum Psychosis Although suicide rates in women are significantly reduced compared to men, the risk of a serious mental illness and suicide is hugely increased during the period immediately following childbirth, known as the puerperium. This is largely because of the occurrence of a mental illness specific to the puerperium called Postpartum Psychosis. This is a rare disorder occurring in approximately one in a thousand live births. A family or personal of Bipolar Disorder predicts the onset of this psychosis but about half of these cases occur in women with no history of mental health problems. This dramatic illness was first formally described in the mid-19th century by Victor Marce, a French physician and the causes are generally attributed to hormonal fluctuations altering brain function, leading to a psychosis. If treated effectively, women make a rapid recovery and the psychosis completely resolves but if un- treated or under-treated, there is a high rate of suicide and infanticide. Before the introduction of modern medicines for the treatment of psychoses, there are accounts of women, such as the Mary Shelly (author of “Frankenstein”) who developed a puerperal psychosis and died of the consequences of this “malady” within a few years. In spite of the dramatic nature and frequently fatal consequences of this illness, I have never treated a woman who developed this illness for the first time who was aware of its existence. The identification of this illness appears to be subsumed under the generic catch-all title of “post-natal depression”, perhaps reflection the stigma surrounding serious mental illness. Perinatal Depression Depression is a spectrum disorder, and for this reason it is now operationally defined; that is, it is said to exist when a certain range of symptoms are present for a fixed period of time. Briefly a diagnosis of depression requires the presence, for at least the previous two weeks, of consistent lowering of mood or inability to experience pleasure, along with a fixed number of biological (disruption of sleep, appetite, motor activity, energy levels) or cognitive (reduced concentration, guilt or suicidal thoughts) symptoms. The definition of depression during the perinatal period does not differ from that of depression in general. Rates of depression in women in general are about twice to three times as high as men and are higher during, than outside, of reproductive years. Although rates of moderate depression do not appear to be increased during the post-natal period there is emerging evidence that some women are genetically vulnerable to developing a form of depression characterised by anxiey and/or obsessional symptoms following childbirth. The epidemiology of post-partum depression is similar to Post-partum Psychosis in that women with a past history of depression are the most vunerable group but some women will develop post-partum depression without any apparent vunerability factors, suggesting a hormonal-brain interaction causation. Although excellent studies published from the 1980’s onwards uncovered significant mood disorder during pregnancy, these findings have been largely ignored. Findings from the main studies examining mood symptoms and/or mood disorder during pregnancy and the postpartum period are consistent in their findings and demonstrate high levels of depressive symptoms, particularly from the second trimester of pregnancy through to the postpartum period. Whether these high levels of depressive symptoms in women during pregnancy are paralled by the occurrence of a specific pregnancy-related depressive disorder has not been examined but in my clinical I have treated many severe pregnancy-related depressions that remitted on delivery of the baby. What is certainly established beyond doubt is that the perinatal period is a time of increased risk for the development of mood disorder and that some of these disorders are specific to this period. In many ways the risk factors for developing depression during the perinatal period are similar to those outside of this periofd. In addition there are some specific risk factors relevant to this state. Depression must be viewed as a stress disorder which arises in response to external stresses and life events. Women will be individually susceptible both to developing depression in the context of general stress, and in response to the specific stressor of pregnancy and motherhood. Women who are socially vulnerable are more prone to becoming depressed: a fact that is consistent across all studies of depression regardless of age, gender or culture. Poverty, poor housing, exposure to violence or racism, unemployment, lack of education, and an unplanned pregnancy or an unsupportive or absent partner are specifically associated with pregnancy-related depression. Ethnicity is also an important issue in perinatal depression as in many cultures depression is not recognised as an illness or a disease and there is no language to describe these pathological emotional states. For example, African women tend to somatise their symptoms of depression and more commonly present with medical symptoms (e.g. pains in their stomachs), rather than a lowered mood state. It would appear that when depression is enquired after in a culturally sensitive way, that rates of depression are similar across diverse countries and cultures. An important point with regard to this is that women are more prone to becoming depressed when removed from their familiar environment and culture, which is clearly protective. Perinatal depression is similarly responsive to treatment as is depression outside of this period: approximately 70% of women respond to standard antidepressant medication. There has been limited experience with using antidepressants during pregnancy, but the evidence to date does not suggest that antidepressant use is associated with significantly higher rates of foetal malformation or complications of pregnancy. The problem with most of the studies examining antidepressant use during pregnancy is that they fail to take into account the fact that being depressed results in high levels of complications during pregnancy and poor baby outcome. Many women prefer to manage their depression with psychological therapies, and would appear to be as effective as medication for the milder forms of depression, but in general these therapies are not available. Consequence of Perinatal Mood Disorder There has been much emphasis placed on recognition and treatment of postpartum depression and this relates to the body of knowledge demonstrating that children born to women who suffer from postpartum depression are disadvantaged relative to their peers. They are disadvantaged in a range of areas including emotional development, intellectual development and they also have higher rates of childhood psychiatric disorders, such as conduct disorder and anxiety disorders. More recent follow-up studies of children born to women who were mildly depressed, and certainly anxious, during pregnancy indicate that at 4 years of age these children suffered more behavioural problems than their counterparts born to women who did not have significant psychiatric problems during pregnancy. A 16 year follow-up study of a group of 200 women and their babies from a deprived area of south London from my research group has demonstrated that all adolescents who were depressed at 16 years of age had a mother who suffered from depression: 74% of whom had perinatal depression whereas among the women who had never been depressed, none of their children became depressed. There is also strong evidence that depression during pregnancy is associated with preterm birth and/or low birth weight. My research programme is investigating the way that mental stress can influence fetal growth and baby outcome, through the action of stress hormones. Preterm birth and low birth weight are the leading causes of perinatal mortality and illness and are the leading costs of disease burden world wide across cultures. The role of psychosocial stress in determining baby outcome is being increasingly recognised. Not only is low birth weight and preterm delivery the leading cause of perinatal disease, it is also a significant determinant of adult health problems. Low birth weight is associated with a range of diseases in adulthood including high blood pressure, diabetes, ischaemic heart disease and major mental illness such as Schizophrenia and Bipolar Disorder. Low weigh at birth is also associated with death by suicide in adulthood. The Future In Ireland there is no means of identifying women who die by suicide as a consequence of perinatal mental illness. In the UK, however, the most recent “Confidential Enquiry into maternal deaths 1997-1999” has identified suicide as the second leading cause of maternal death after cardiac disease. The report also suggests that many of the unidentified deaths are likely to result from mental illness, making suicide the leading cause of maternal mortality. More generally, it is now established that the seeds for mental ill health are laid down before a baby is born and much of adult mental health is determined by parental mental health, particularly during the perinatal period. If we wish to address the public health problem of adolescent and adult suicide we need to target these high risk children, who could be easily identified by screening programmes during pregnancy and the postpartum. Lastly, there has been an increase in the deaths of children by their parents in Ireland in recent years: at least 18 children have died at the hands of their parents in this country since 2000. In many of these cases, the parents then took their own life. It would appear that many of these cases occurred because parents were psychotically depressed, believing that it was in the best interest of their children to die rather than live a life of disgrace, despair and eventual impoverishment. Experts call this “altruistic filicide”, a phenomenon that I have followed in the national press because of the absence of official information on the topic. Many of these case involved very young children with the onset of depression occurring during the peripartum period. A project to investigate infanticide and filicide in Ireland involving Barnardos, the National Children’s Office and the Central Mental Hospital, and commenced by Dermot Aherne in his capacity as Minister for Social, Community and Family Affairs some years ago has been abandoned because of internal difficulties. In addition to perinatal mental health service deficits, this official denial of the phenomenon of infanticide, filicide and maternal death is leaving our children vulnerable to an ongoing cycle of mental ill health and possible suicide. Relevant website (created by a research worker in my team with personal experience of perinatal depression): http://www.pregnancy-depression-help.com/index.html Book: “Psychiatric Disorders in Pregnancy: Obstetric and Psychiatric Care” Eds, O’Keane V, Marsh M, Seneviratne G. Martin & Dunitz: Feb 2006. Dr. Veronica O’Keane, Senior Lecturer, Perinatal Section, Institute of Psychaitry, London SE5 8AF WOMEN AND SUICIDE FROM A WOMEN’S HEALTH PERSPECTIVE ANNIE DILLON National Women’s Council Abstract This presentation examines women’s mental health from a gendered perspective taking account of women’s continued inequality, the impact on women’s mental health and women’s experience of suicide and deliberate self-harm. Women’s particular experience including diversity of women is highlighted in the context of mental ill health and treatment and their own preferences are put forward. Firstly some background information on NWCI is presented. National Women’s Council of Ireland (NWCI) The NWCI was founded as the Council for the Status of Women (CSW) in 1973 following a recommendation by the Report of the First Commission on the Status of Women. The name was changed to the National Women’s Council of Ireland in 1996. NWCI is a Non-Government Organisation located within the Community & Voluntary sector and is the national representative organization for women and women's groups in Ireland. There are currently over 160 women's organisations and groups from all parts of Ireland affiliated to the NWCI. It is estimated that the NWCI represents over 300,000 women through its combined affiliate membership. NWCI Work on Women’s Health Policy and Issues Since its foundation NWCI has worked on women’s health issues and policy, e.g. in 1995 NWCI was appointed by the Department of Health and Children to undertake wide ranging consultation with members on the Green Paper on women’s health and subsequently made significant contribution to the development of the Government’s Women’s Health Policy ‘A Plan For Women’s Health 1997-1999’ Currently NWCI collaborate with our members to inform policy based on their work and experience including e.g. NWCI annual pre-budget submission and other submissions1 such as to the Mental Health Commission on Recovery Model (Mar. 06) NWCI have participated in Partnership through the Community and Voluntary (C&V) Strand and also participate in the National Economic and Social Forum (NESF), most recently in relation to the NESF Mental Health & Social Inclusion Project Team. Work of NWCI Affiliate Members on Women’s Health2 Many NWCI member organisations work on women’s health at a variety of levels including service provision, advocacy and lobbying: Locally and Regionally e.g. Provision of services such as counselling, mental health promotion, well women services and adult education in response to local women’s needs (Organisations include Longford Women’s Link, Letterkenny Women’s Centre, North Leitrim Women’s Centre) 1 For NWCI Submissions see http://www.nwci.ie/publications.html#3 For further information on the work of NWCI and NWCI affiliate members see: www.nwci.ie and http://www.nwci.ie/membership.html 2 Provision of community development approaches to health, health education, primary health care projects (Organisations include Pavee Point, Cáirde, Clondalkin Women’s Network Women’s Health Forum) Nationally, e.g. Bodywhys and Action Breast Cancer In September 2006 NWCI published aReport ‘Women’s Health in Ireland; Meeting International Standards’. The report recommends that policy take account of gender, including the health impacts of women’s continued inequality, women’s diversity and particular health needs and experience of ill health. Health Impacts of Women’s Continued Inequality ‘Women’s Health is inextricably linked to their status in society. It benefits from equality and suffers from discrimination’3 The WHO notes that the impact of gender on health is determined by women’s subordinated status in society.4 The UN Convention on the Elimination of Discrimination Against Women (CEDAW) stresses the broad range of risks to mental health to which women are disproportionately susceptible as a result of gender discrimination, violence, poverty, armed conflict, dislocation and other forms of social deprivation.5 In Ireland, women continue to experience economic inequality. The gender pay gap persists, with women currently earning 14% less than men. The Institute of Public Health has noted that for women the gender pay gap is a pathway to poverty and ill health.6 An increasing number of people living in poverty are working. In 2004, 6.2% of women working were at risk of poverty in comparison to 7.2% of men. In 2004, 23% of women were at risk of falling below the 60% poverty line in comparison to 18% of men. Women aged 65 and older have a 45% risk of being below the 60% poverty line in comparison to 34% of men. Lone parents, the majority women, have a 42% risk of living on an income below the 60% poverty line. Women do not have equal access to social welfare allowances, defined within the system as ‘qualified adults’; which also affects the level of state pensions. As a result of women’s ascribed roles, women undertake the majority of unpaid care work, which can have an impact on women’s mental health. While there is limited data available in Ireland, there is evidence to suggest that unpaid care work negatively impacts women’s mental health, including through lack of sleep, increased anxiety, lack of social life and higher rates of illness generally7. Overall women’s continued unequal position means that more women experience poverty, a determinant, which negatively effects mental and physical health. 3 4 WHO (1998) World Health Report WHO Europe (2001) Strategic Action Plan For Women In Europe 5 http://www.un.org/womenwatch/daw/cedaw/recommendations/recomm.htm#recom24 6 IPHI (2005) Health Impacts of Employment, A Review 7 Canadian Women’s Health Network Impact of Violence and Sexual Abuse on Women’s Mental Health It is increasingly recognised that violence against women is a major contributor to the burden of mental and physical ill health experienced by women.8 According to the WHO9 women who have been exposed to violence are at greater risk to developing a range of health problems including stress, anxiety, depression, pain syndrome, phobias and medical symptoms. An overview of studies on domestic violence and depression in women found an average prevalence rate of 47.6%.10 In Ireland the SAVI Report (2002) found that of the 42% of women who have experienced sexual abuse or violence over their lifetime, including child sexual abuse, 25% reported symptoms consistent with a diagnosis of Post Traumatic Stress Disorder (PTSD) at some time in their lives following and as a consequence of their experience of sexual violence. Those who had experienced sexual violence were significantly more likely to have used medication for anxiety or depression or to have been a psychiatric hospital in-patient than those without such experiences. For example, those who had experienced attempted or actual penetrative sexual abuse were eight times more likely to have been an in-patient in a psychiatric hospital than those who had not been abused. A Canadian study suggests that the impact of violence, abuse and trauma on women’s mental health is not generally taken account by treatment services. When it is recognised, as a causative factor a biomedical treatment approach is the norm.11 Women’s Mental Health Women have a particular experience of mental ill health, and therefore specific mental health needs. In 1997 the Government acknowledged that mental health services did not meet women’s needs.12 Women’s mental health is affected by various factors relating to women’s inequality and multiple discriminations in Irish society. In order to respond to women’s experience and needs, mental health provision requires a gendered approach to both policy and service provision as highlighted in the recent report by the Women’s Health Council,13 borne out by the WHO’s acknowledgement that gender is a determinant of mental health14 and recommended by NWCI (2006). With recent developments in the area including the work of the Mental Health Commission NWCI hope that the situation will soon improve. Women’s Experience of Mental Ill Health. 8 Victorian Health Promotion Foundation (2004) The Health Costs of Violence, Measuring the burden of disease caused by intimate partner violence. Melbourne, VicHealth: Victorian Health Promotion Foundation. www.women.vic.gov.au 9 WHO (2000) Women’s Mental Health An Evidence Based Review. Geneva, WHO. http://www.who.int/mental_health/media/en/67.pdf 10 Golding, J (1999) Intimate Partner Violence as a Risk Factor for Mental Disorder: A Meta Analysis 11 Morrow. M (2002) Violence & Trauma in the lives of women with serious mental illness. http://www.bccewh.bc.ca/PDFs/violencetrauma.pdf 12 DoH&C (2007) A Plan For women’s Health 1997-1999 13 WHC (2005) Women’s Mental Health, Promoting a Gendered Approach to Policy & Service Provision. 14 WHO (2001) Gender Disparities in mental health. The UN Convention on the Elimination of Discrimination Against Women (CEDAW) stresses the broad range of risks to mental health to which women are disproportionately susceptible as a result of gender discrimination, violence, poverty, armed conflict, dislocation and other forms of social deprivation. There are significant gender differences in the experience of mental illness. For example: Depression, including postnatal depression is considered the most common form of mental illness amongst women. Eating disorders are more common among women and women are more likely to be diagnosed with anxiety related disorders and post-traumatic stress than men. Suicide and Deliberate Self Harm (DSH) It is well established that suicide is less common amongst women than men although in Ireland the Central Statistics Office (CSO) has noted that the overall female rate is increasing with the rate of suicide amongst young women more than doubled during the 1990’s. Deliberate Self Harm (DSH) is higher amongst women than men, peaking amongst 15-19 year old girls (more than twice that of boys).A recent Canadian report15 notes that women who self harm have frequently experienced family disruption and trauma in their lives. The onset typically occurs in adolescence and often linked to childhood abuse and violence including sexual abuse. This report draws on research, which suggests that, the relationship between self-harm and suicide is contested with self harm seen as a coping mechanism for dealing with emotional pain and distress while suicidal acts are viewed as oriented toward ending pain. The report notes that those who self-harm may still be at risk of suicide and recommends particular women centred responses including: Community Services including crisis intervention Education including to reduce stigma Treatment that includes a woman centred therapeutic approaches, peer support Overall a non-punitive responses and harm reduction are recommended Policy development, that is women centred, focused on causes rather than behaviours and research to establish prevalence, evaluate interventions etc. Women’s Experience of Treatment In relation to treatment women are generally more likely to be prescribed psychotropic drugs by their GPs, while men are more likely to be referred for specialist treatment.16 Women with experience of mental ill health have expressed concern to the NWCI about the use of medication and the lack of availability of services such as counseling and therapy.17 This concern is borne out by a recent Canadian review, which indicates that women are more likely to be prescribed psychotropic drugs such as SSRIs rather than the 15 Prepared by the Canadian Centre on Substance (2006) Abuse 'Self Harm Among Criminalized Women' Available from www.ccsa.ca 16 WHC (2005) ibid. 17 NWCI (2004) In From The Margin use of non-drug methods such as counseling, support, nutrition and exercise.18 Women mental health service users have identified further issues to the NWCI19 including: The gender specific experience of mental ill health Stigma attached to mental ill health, lack of optimism and the impact of long term medication The need for a person centred approach to treatment and mental health promotion The lack of availability of services such as counseling and self help groups. Through NWCI membership women have also raised the need for more holistic and empowering options such as counselling and support groups needs. Promoting a Gendered Approach In conclusion NWCI believe that in order to respond to women’s experience and needs, including in the area of Suicide and Deliberate Self Harm, mental health provision requires a gendered approach to both policy and service provision as recognized in the recent report by the Women’s Health Council and borne out by the WHO’s acknowledgement that gender is a determinant of mental health. We stress that ‘Womencentred’ includes involving women, particularly those who experience mental ill health and is responsive to needs and recognises diversity. Finally in relation to Suicide and Deliberate Self Harm NWCI acknowledges the need for further developments particularly services which target young women. Ms. Annie Dillon, NWCI, 9 Marlborough Court, Marlborough St. Dublin 1. Tel: 01 8898472. e-mail: annied@nwci.ie Tel: 01 878 7248. E-mail: info@nwci.ie Website: www.nwci.ie Chairperson: Anne Cleary - Comments Session 2 of the programme consisted of two papers. The first paper, given by Dr. Veronica O’Kane examined the health consequences of under-treatment of psychiatric illness during pregnancy and the postnatal period. Dr. O’Kane’s job title – that of Perinatal Psychiatrist - is, as yet, unusual and her talk began with a moving story of a tragedy which underlined the need for this specialisation and the screening of pregnant women for psychiatric symptoms. This need is crucial in the context of certain forms of psychiatric illness – notably bipolar disorder – when screening may save lives. More generally the identification of psychiatric symptoms has hugely positive repercussions for both mother and children. The service which Dr. O’Kane provides in a special unit attached to the Maudsley Hospital in London is unique in the UK and not available in 18 Currie, Janet (2005) The Marketization of Depression: The Prescribing of SSRI, Antidepressants to Women. Women and Health Protection., Canada http://www.whp-apsf.ca/pdf/SSRIs.pdf 19 NWCI In From the Margin Project (2002/4), Feedback from Schizophrenia Ireland Women’s Group Ireland. She therefore sees part of her role as disseminating information on this area of need to other clinicians. The discussion which followed focused on the need to publicly identify this problem and to provide appropriate care for such women. The second paper examined suicide from a women’s health perspective and was delivered by Annie Dillon of the National Women’s Council of Ireland. Using a women’s health policy context the speaker reviewed issues relating to suicide and parasuicide in Ireland and addressed prevention in the context of locally based groups. The fact that the NWCI represents approximately 300,000 women through a network of women’s clubs underlines the preventive potential of this organisation. Ms Dillon emphasised the need to understand women’s health in a socio-economic context and this approach underlines a recent report on women’s health from the Council. Economic factors have a major influence on women’s health and women they are also affected by gender-specific difficulties. Thus women have specific mental health needs and these need to be addressed to prevent distress, mental illness and suicidal behaviour. BORDERLINE PERSONALITY DISORDER: COMPLEXITY AND CHALLENGE FOR SUFFERER AND SERVICE ANGELA MOHAN Consultant Psychiatrist, St. Vincent’s Hospital, Dublin Abstract This presentation will cover some of the complexities and challenges in the diagnosis management and treatment of women with borderline personality disorder. It aims to highlight the particular suffering of women with this condition which is poorly understood and the difficulties experienced by their families and society. The high incidence of self harming behaviours and the links with completed suicide will be explored. Some suggestions for a more compassionate understanding, treatment frameworks and service development will be discussed. Borderline Personality Disorder is a uniquely challenging mental health problem. It is difficult to define, is separate from mental illness but is commonly associated with it. The cause is unclear. It lacks specific treatments. It causes much suffering for the individual, their family and society. It challenges the health service providers due to the dramatic and demanding presentations, the social rule breaking, the intense emotions stirred, the disruption and the sense of powerlessness evoked in others. There are also high maintenance costs of the individuals involved, as they are high users of health services often with questionable benefit. There is high morbidity, general ill health and high mortality with suffers dying from accidents and physical ill health as well as having a rate of suicide of one in ten. These clients are damaged and damaging, challenged and challenging. Diagnosis While not considered mental illness, personality disorders are defined in ICD-10 (WHO, 1992), as deeply ingrained and enduring patterns of behaviour manifesting themselves as inflexible responses to a broad range of personal and social situations. They represent either extreme or significant deviations from the way the average individual in a given culture perceives, thinks, feels and relates to others. They are frequently, but not always, associated with various degrees of subjective distress and problems in social functioning and performance. Borderline personality (BPD) is categorised under the group of emotionally unstable, borderline type characterised by disturbed self-image, aims and preferences, chronic emptiness, intense unstable relationships, self-destructive behaviour. (*3 criteria) This disorder is grouped in the ‘Cluster B’ group of personality disorders. Incidence The incidence varies according to the study but there is general agreement that severe forms of the disorder occur in 1% of the population. There is a four times greater incidence in females (Gunderson, 2001). Clinical Features The core features are of unstable mood with frequent shifts sometimes within minutes or hours. Depression is common but mostly of a reactive type. There is frequently a state of emptiness. Patients describe this as feeling ‘blank’ or ‘being like a zombie’. They are frequently bored and crave company. There is what is described as ‘a morbid fear of abandonment’ and intense anxiety at separation. These unpleasant feelings are so distressing that clients often use binge eating, substance misuse, engage in kleptomania, promiscuity and self-cutting to relieve and break the cycle. There are frequent episodes of intense rage and anger directed towards others as in aggressive outbursts or towards themselves often resulting in self-harm. With the frequent shifts from one mood state into another, the identity disturbance can be understood, resulting in difficulties in interpersonal functioning and in work and occupational functioning. Impulsivity is marked with recurrent threats, repeated overdoses and self-cutting, running away and aggressive acting out. There is frequent co morbidity with other types of personality disorders, dysthymia, major depression, substance misuse, eating disorders, anxiety disorders and psychotic disorders. The repeated presentations to the A+E or the psychiatric services of these patients in crisis either considering self harm or having cut themselves or taken an over dose leads often to a negative rejecting and even hostile reaction. It is not unusual for those with the most severe disorders to present up to 10 or 15 times a year in such a crisis. Doctors and psychiatrists regularly describe these behaviours and patients as “wilful” “manipulative” and “attention seeking”. Sometimes these patients are treated as if they are deliberately trying to make life difficult for services and that their behaviours are under their full voluntary control. There are no studies, which fully explain the motivation for the behaviours (Browne, 2002). There appears to be a mixture of motivations, which can vary between patients, and between the same patients on different occasions. One of these is the relief from unbearable feeling of dysphoria. Patients describe a build of inner tension, which is immediately dissipated, on cutting or on swallowing a foreign body. This may be due to the release of brain endorphins, which help regulate other brain chemicals (Leibenluft, 1987). Patients may be dissociating during the episodes as they describe a lack of pain even during deep cutting. Other patients want to punish them selves or distract themselves and some may indeed be motivated to illicit care and attention. Patients with this condition are frequently admitted to acute wards in psychiatric hospitals. After the first few days of admission as the crisis is resolving, destructive dynamics (splitting) get played out where the patient manages to set other patients and the staff against them and against each other, creating confusion and crisis. The admission becomes counterproductive and the patient is frequently hastily discharged feeling rejected and abandoned. The patient self harms to relieve the distress or to gain support or attention, again repeating the cycle. Causes This is a disorder where both nature and nurture have roles to play. There is a strong association with sexual and physical abuse (Fonagy, et al 1997) but a great many with childhood abuse do not present in this way. Several studies have shown the strong association between personality disorder and child hood adversity (Fonagy et al, 1997)(Johnston et al, 1999). There is also evidence of a genetic component (Torgersen, 2000) but the size of the contribution is unclear. Family members of patients with borderline personality disorders frequently have high rates of personality disorders-not just BPD. Other biological factors may be involved as the neuroendocrine function may be damaged by chronic stress or trauma). There also may be neurotransmitter dysfunction resulting in impulsivity and affective instability (Sarkar, 2006). Self Harm and Suicide Risk It has been described that there is “chronic” suicidal risk with borderline patients and the risk becomes more “acute” with even slight interpersonal or environmental stressors. There is a relatively low level of completed suicide given the number of attempts. Others have described the high rate of self-injurious behaviour as the “behavioural specialty” (Gunderson, 2001) of borderline personality disorder and this tendency as “multiple suicide attempts of low lethality”. However the risk of completed suicide doubles after a suicide attempt (Gunderson, 2001) .The risk of suicide increased with comorbid major depressive disorder, with comorbid substance misuse and when there is co existing antisocial personality disorder (APA Guidelines, 2001) The higher risk with co morbid substance abuse maybe accounted for by impaired judgement and even low suicidal intent can combine to produce a fatal outcome. Personality disorders are estimated to be present in more than 30% of individuals who die by suicide, about 45% of individuals who make suicide attempts (Haw, 2001), and around 50% of psychiatric outpatients who die by suicide. In clinical populations, the rate of suicide of patients with borderline personality disorder is estimated to be between 8% and 10%, a rate far greater than that in the general population (Oldham, 2006). However, since 60%–70% of patients with borderline personality disorder make repeated suicide attempts, unsuccessful suicide attempts are far more frequent than completed suicides in patients with borderline personality disorder The risk factors most readily recognized by clinicians include a history of multiple suicide attempts, especially those with high potential lethality, and the presence of significant, persistent substance misuse. Despite the ability to identify meaningful risk factors in patients with borderline personality disorder, we cannot with certainty predict future completed suicidal behaviour in an individual patient. Impulsivity has been shown to be related to suicidal behaviours (Brodsky, 1997). In a major prospective study, affective instability the criterion most strongly related, in BPD, to both suicidal behaviours and suicide attempts (Yen, 2004). It is interesting that this is more of a predictor for suicidal behaviour than major depressive disorder. This suggests that reactive mood shifts associated may account for suicidal behaviours more so than negative mood Ways of Understanding BPD Freud’s concept of personality development proposes that early traumas disrupt personality development and the patient becomes fixed at an immature level. Melanie Kline suggests that there is regression to a stage of the infant within the first months of life, with the use of primitive defences such as splitting where the sufferer separates and divides people sharply in their mind into good and bad and projects these states out to others. There is lack of the integration, which characterised more mature states of development. I will spend some time describing Cognitive Analytic Therapy as this gives a framework for the understanding of this condition, which I find useful in my practice. Cognitive Analytic Therapy (Ryle, 1991) holds the theory that the mind is socially formed and the infant learns about relationships and the social values and customs through an intense intimate relationship with the chief carer usually the mother. Observational experiments on neonates only a few minutes old have concluded that the infant is primed to relate from birth and both responds to the mother and elicits responses. The early relationships are internalised into the child’s mind .The child learns two roles, the role of the caretaker and the role of the care receiver. These roles are seen to be connected as the poles of a reciprocal relationship. The child is then able to apply either of these roles in any future relationship either with another person or to themselves. In other words, a baby who has experienced caring and nurturing will be able, throughout their life to be in a caring and nurturing relationship with others and will be able to care and nurture itself. When one is in one pole or role of the reciprocal relationship the other pole or role is invited from others. Usually psychologically healthy people have a large range of roles and they can move smoothly between these roles. The damaged child who has been the subject of abuse is usually limited to a small number of harsh reciprocal roles e.g. abusing to abused victim and abandoning to abandoned The abuse hinders the development of reflective capacity (Ryle, 1991) and the client switches abruptly between mood states. This is often then how they relate to them selves and others. They abuse themselves in many ways, as has been described, but they also by their actions invite abuse and neglect from others. These individuals also have the victim role, which invites the other to be in a rescuing or be ideally caring. So on a ward some staff can be invited into the ideally caring role and others can be invited into the rejecting abusive role and this can change from day to day and hour to hour. This can cause the splitting between staff, which reflects the chaotic destructive inner world of the client. The role of Cognitive Analytic Therapy is to bring to the client’s awareness their roles and how they operate and help to them integrate the different parts of their inner worlds. This is usually done through diagrams to draw out the patterns and to help them develop new ways of dealing with their lives. The diagram can also help staff to avoid colluding in the invited roles. Another way of understanding BPD is that there is a failure of regulation of emotions resulting from insecure attachments to carers in childhood (Sarkar, 2006). This hypothesis is gaining ground. It combines a psychotherapeutic understanding with a biological model. I will go into this in more detail. Emotions and affects have been described as bodily experiences as a result of an external or internal cues (Damagio, 1994) The states are expressed through the autonomic nervous system, the endocrine system and the sensory and motor responses e.g. speech and through behavioural reactions. The systems in the body are linked together in a complex arrangement and the whole system is in a delicate balance designed to assist the human in survival behaviours. Humans are a uniquely social group and each individual requires a long time to become independent from others. The capacity to regulate emotions is advantageous to interpersonal functioning and to fostering higher levels of social adaptation. Animal research (Suomi, 1999) has shown the links between the animal’s temperament and the social environment and the development of the brain’s architecture. A distressed infant has a raised level of noradrenalin, the fight/ flight/freeze hormone. Crying elicits the care of the caretaker and when the baby is soothed the parasympathetic nervous system is recruited and this brings the baby’s hormone system into balance. The primary care giver has acted to regulate affects. In earliest infancy from around two months of age there are short intense bursts of interaction of between the child and carer centred on feeding changing bathing and holding. These critical interactions set the scene for the development of cognition and interpersonal development. The right side of the brain is involved in regulating the autonomic system and the right brain is also involved in the social and biological functions of attachment. Any experience disrupting development at this critical time is likely to impact on the development of this regulating system and lead to difficulties with emotional regulation throughout life. Children around the age of 5 have learned to regulate their own emotions internally and do not now need an adult carer for this. When there has been insecure attachment between a child and caregiver the emotional regulatory system is not functioning. Slight signals or cues in the environment can switch on an alarm response, which had difficulty being managed or contained. With very overwhelming response the person can switch rapidly into ‘freeze’ mode as in a dissociated state or there could be rapid cycling between states with depression and fear (fright) and intense switches into aggression (fight) which can be directed towards others and towards the self. Treatment and Management of Borderline Personality Disorder The main plank of treatment is psychotherapy. However the research into what works is still at an elementary stage. Dialectic behavioural therapy, a type of cognitive therapy with skills training in affect management using mindfulness, has shown promising results on a reduction of self harming behaviours. This needs an especially trained team and team support (Blennerhassett 2005). In a funded study with the National Institute of Mental Health (NIMH) has found that Dialectical Behaviour Therapy (DBT) reduced suicide attempts by half compared with other types of psychotherapy available in the community in patients with borderline personality disorder (Linehan2006). This study showed that DBT also excelled at reducing use of emergency room and inpatient services and more than halved therapy dropout rates compared to the mostly traditional approaches. Psychodynamic psychotherapy has also been shown to be helpful as well as Cognitive Analytic Therapy and Interpersonal Therapy. Group therapy and therapeutic communities (Dolan, 1999) and psychotherapy day hospital care (Bateman and Fonagy, 1999) have demonstrated value and benefit. Psychotherapy especially relational therapy probably acts to contain emotion, acting through the ventral precortex of the brain (Sarkar, 2006). Medication can also be of benefit when targeted to specific symptoms. The newer antidepressants, SSRIs, can help with impulsive aggression and anxiety symptoms and low dose antipsychotic medication can help with perceptual distortions. Anticonvulsants can help with mood stabilisation and with aggression. Managing the suicidal behaviours is given the first priority and is commonly undertaken by setting up a safety contract with the therapist .The patient is supported and encouraged to contact the therapist (in the case of DBT by phone on 24 hr basis) but at least to contact a day hospital or A+E before acting on an impulse to self harm. The therapy sessions are used to work through triggers and to explore and seek alternative ways of coping. The role of inpatient hospital admission is controversial (Paris, 2002). The consensus is emerging that hospitalisation is best avoided apart from brief stays which are sometimes required for acute suicidal crisis. This may include discharge before the threats of self- harm have subsided. It helps to balance the risk if the psychiatrist knows the patient’s form over a long period is psychologically minded and has a good therapeutic relationship with the patient. It can help also if the patient is referred to a day psychotherapy service and if they have a therapy session within a few days of discharge. Community day treatments with assertive outreach will most likely be the model of service delivery in future for this group (Links, 1998). In recent years there are increasing efforts to understand the pathology and the treatments in borderline personality. This coupled with encouraging reports of positive results from a number of studies of psychotherapy treatments is changing the views of service deliverers .In Ireland a number of teams have been trained in DBT and in CAT (White, 2006) but there are no Irish dedicated psychotherapy day hospitals or therapeutic communities serving this patient group. These services will probably develop in time as the evidence base strengthens and hopefully these patients will have more comprehensive humane and compassionate treatment. References available from IAS Dr Angela Mohan, St Vincent’s Hospital, Fairview, Dublin 3. BRAIN, GENDER AND SUICIDALITY MICHAEL FITZGERALD Henry Marsh Professor of Child and Adolescent Psychiatry, Dublin Abstract This talk focuses on brain gender and suicide. It puts particular emphasis on the major organic differences between male and female brains. It puts forward ‘an amygdale theory’ of suicide. It also examines the psychological differences between males and females and how these impact on suicide. This paper focuses on brain gender and suicide. It puts particular emphasis on the major biological differences between male and female brains. It describes the “amygdale theory” of suicide. It also examines the psychological differences between males and females and how these impact on suicide. In Ireland in 2005 there were 19 female suicides and 360 male suicides. The suicide rate of females in Ireland has increased for 2/1000,000 in 1980 to 7/100,000 in 2001. Differences between Male and Female Suicide: Male and Female Brains: The male brain has a larger coupus callosum that is the linkage structure between the right and left hemispheres. There is therefore more information passing between the right and left sides of the brain in females. Females use more of their brain to accomplish tasks. The female brain peaks in size at 11 ½ years while the male peaks in size at 14 ½ Years. The female brain matures faster than the male brain. There is an exception in that, boys mechanical and spatial reasoning matures four to eight years earlier in boys than girls. Female brains are 8% smaller but are more integrated and more connected up. In the female brain digust is processed by the left amygdale while in the male it is the right amygdale. The amygdale is the part of the brain that processes fear, hate, love and anger. It is involved in emotional processing. It is involved in a very quick form of emotional processing. A slower form of emotional processing is when the amygdale connects with the prefrontal cortex which is the executive part of the brain. These connections are more elaborated in females and this is the reason why the female brain is more connected up. This gives a protective factor to females in relation to completed suicide. Females also have better connections between amygdale and language centres of the brain. In addition female brains have less white matter in their brains that is the white myelin sheets of nerve fibres under the microscope. Language is also more bilaterally processed in female brains. In females the hippocampus is larger than in males. The hippocampus deals with learning and memory. Very importantly female hippocampal cells are less damaged by chronic stress in females than in males and it is possible that sex hormones play a role here. In mice and we have to be careful in extending these differences to humans there are 12,000 genes which behave differently in females than in males. Females have 11% more nerve cells in the area of the brain devoted to emotion and memory. This appears to be protective against suicide. It is going too far to say that men are ‘construction failures’. Female babies are exposed to much less testosterone in the later stages of pregnancy. This fact leads to better eye contact and earlier language development. Neuropsychological Factors: Because of the above females have much greater capacity for empathy and have much better verbal skill. From a purely human interpersonal point of view they are more advanced evolutionarily than males. They have better social intelligence. They are better at communication and care taking. They prioritise family over work even if working both inside and outside the home. They are better at reading body language and nonverbal behaviour, better at emotional processing, more interested in people than objects and they engage in less crime and physical aggression. They are better at seeing textures, colours and have a better sense of smell. At the same time women have twice as much depression as men and engage in self harm or attempted suicide far more commonly than men. Increasing Rates of Female Suicide: It would appear that the increasing rates of female suicide are due to environmental factors as the female brain would not change over the course of 20 years to any significant degree. The factors related to increased suicide in females appear to be alcohol particularly binge drinking, relationship breakdown, bullying in the workplace, abuse of drugs, lack of social support, copycat situations. The Need for Gender Specific Treatments for Men and Women in Relation to Self Harm and Attempted Suicide: It is important now that we begin to develop gender specific treatments for self harm and attempted suicide based on the above differences in male and female brains. It is critical that Psychotherapists are fully aware of the structural biological and neurochemical differences between male and female brains in their treatment. If they are not aware of this they will have greatly reduced capacity to be empathic and to understand the sex specific issues of their clients. References available from IAS Prof. Michael Fitzgerald, Ballyfermot, Child and Family Centre, Ballyfermot Road, Dublin 10 WORKING WITH YOUNG WOMEN WHO SELF HARM – THE SCOTTISH EXPERIENCE PAT LITTLE Development Manager (young people) Penumbra Abstract Penumbra is a leading Scottish Voluntary Organisation working in the field of mental health. Since 1994 Penumbra has pioneered community based mental health projects for young people. Penumbra provides an extensive range of person centred support services for young people with mental health problems and a diversity of support needs and issues throughout Scotland. Penumbra has been working in the field of self-harm, particularly with the 16-25 year age group over a period of several years. In 2001 Penumbra published a report on a piece of research carried out in Edinburgh with young people who self-harm called “No harm in Listening” that detailed gaps in the current service provision. At present Penumbra run 6 projects across Scotland funded by Choose Life (Scottish Executive National Strategy for Suicide Prevention) to tackle self-harm issues. Many have experience of both self-harm and attempted suicide. Penumbra’s aims to provide people who self-harm with a safe and non-judgemental environment in which they can explore their feelings and worries in confidence. Structure of Presentation I plan to cover Penumbra’s work with young people and then go on to look at working with young women who self-harm exploring: What is it? Why do they do it? What are their needs? What are the issues for agencies and workers? Young people’s experiences About Penumbra Penumbra is a leading Scottish Voluntary Organisation (NGO) working in the field of mental health. It provides a extensive range of person centred support services for adults and young people. It also campaigns to raise awareness of mental health issues, promotes the Recovery approach and is part of an anti stigma campaign called see me. Since 1994 Penumbra has been providing community based support services for 16-25 year olds and in recent years increasingly working with all secondary school ages. During this time Penumbra has become the leading agency in Scotland working with young people who self-harm. Between 30-50% of the young people coming to our mainstream projects self harm. In 1998 in conjunction with the British Medical Association in Scotland we organised an Open Space conference to highlight experiences of young people who self harm, their parents, carers and friends, and professionals who come into contact with them. In 2001 we published an Action Research Report carried out with young people in Edinburgh who self harm called “No Harm in Listening”. This involved testimonies of young people’s experiences of self harm- what led them to do it, what types of self-harm they used, what they got from it, what were their experiences of services and finally what types of support services they wanted to see developed. In the past two years Penumbra has developed 6 dedicated Self Harm Projects funded by local Choose Life groups- Choose life is the equivalent of the Irish Reach Out- tackling suicide agenda. The main aims of these projects are to : Offer support and advice to young people who are engaging in self harming behaviour Provide advice and support to carers, families and friends Provide information, training, support, advice and consultancy to professionals in contact with young people who self harm Provide individual and group support which explores underlying issues leading young people to self-harm Engage with young people and provide services that listen to and respond to their perceived support needs Educate the general public in relation to self harm in order to reduce stigma experienced by people who self harm Penumbra’s Learning in Working with Young People who Self Harm The history of Penumbra’s work with young people goes back to 1994 around the time when there was a huge increase in young people being referred and admitted to psychiatric hospitals in Scotland. What became clear was that the more young people came into hospital the more people recognised that adult services could not meet the needs of the growing numbers of young people being admitted to adult wards. The Scottish Borders Local Authority asked Penumbra to examine what was going on in their local area and to think about developing services which young people might use. Penumbra set up a Drop-in service for young people and began to advertise a community support service for young people affected by mental health issues. Over the next few years through working with young people who came to the project we began to develop a knowledge and expertise of working with this group. Some the significant lessons learned were: Many of the young people had severe problems to deal with Very few had single issues with most having a range of problems Most had histories of deteriorating health and could clearly remember where things had started to go wrong for them Most were reluctant to accept help from adults Once Penumbra managed to develop their trust we discovered they had great insights into their own experiences which were often not recognised by professionals in contact with them. This was particular evident when we began to work on one of the main presenting difficulties- self harm. What Penumbra Tries to do Acknowledge young people’s suspicion to accept help Recognise their expertise and knowledge about their lives Offer them help “on their terms”- they decide the level of engagement with the projects Encourage young people to develop skills and confidence to - discuss and deal with difficult issues in their lives - take control and responsibility for their own lives - break the pattern of negative experiences and recognise achievements and progress Moving then onto our Work in the Self Harm Field The information gained through this level of engagement with young people allowed us to build huge knowledge and experience in relation to self harm. In 1995 Penumbra organised a conference on suicide and self harm and asked young people to contribute their thoughts and experiences on the issue. Through this we began to realise that the experts on self harm were the people who did it. They had lived with this problem for years and the people who needed to become informed and educated were the people who came into contact with them. To people who have no experience of self harming this behaviour can be a very difficult thing to understand. The first thing we learned is that the vast majority of self harm is done in private. Hospital admissions for self harm appear very high- 16-17000 people every year in Scotland. The information we received from young people indicated that for every self harming episode that required hospital treatment, they had self harmed numerous other times without needing medical attention. They had either learned to self harm to the extent of being able to treat their own injuries or, because of the way they had been treated when they went for medical attention in the past, were very reluctant to return for treatment again. This is also supported in three large scale community based surveys of self harm in adolescents in England and quoted in the recent National Self Harm Inquiry into Self Harm among Young People. Green et al, 2005; Hawton et al, 2002; and Meltzer et al 2001 reinforce the point that the prevalence of self harm is much higher than is indicated by hospital admissions. Why do People do it? Most people have mixed and complex feelings about their self harm. On the one hand they feel frightened and ashamed. They hate the secrecy and isolation involved. The thought that they may be harming themselves for years appals them. On the other hand self harm may have become a valuable tool for survival. Communication Many young people do not have or have lost the skills to communicate and through self harm are attempting to let people know the inner pain they are experiencing. Feeling Real Many young people describe feelings of numbness due to the pain they are dealing with and describe self harming as a way making themselves feel alive again. Self Punishment Many people blame themselves for past experiences and feel they may have been responsible for the death of a parent, for their parents breaking up or particularly for contributing to their sexual abuse. This can cause feelings of self hatred and loathing. They may believe they “deserve to be punished” and self harm may help a person feel they have atoned for their past behaviour which they feel have contributed to these events. Control Often when the rest of their lives are out of control self harm may be the only way they feel they have control i.e. what happens to their own body. Managing Moods and Feelings Self harming can be a way of releasing anger and internal pain. While some people can externalise pain through perhaps targeting their anger at other people by getting into fights etc, people who self harm have learned that self harm can help them manage these types of feelings. Dissociation Many young people describe how they use physical pain to distract themselves from emotional pain effectively making their pain physical rather than emotional. Coping The primary reason described by young people for self harming was as a way of coping. There are many complex reason why someone might self harm but it is generally described as being in response to painful and difficult events in their lives. The feelings and pain around these can build up and become unbearable. Self harming can have a cathartic affect and significantly reduce the pressure that has built up inside them. This is why self harm for many people can become a coping strategy and sometime reduce their feelings of suicide. It is therefore important to look behind the circumstances that lead people to self harm and not necessarily focus on the self harming behaviour itself. Suicide and Self Harm Having worked with this issue for many years we are clear that self harm and suicide are two distinctly different things. Solomon and Farrand (1996) say that although the self injurious and suicidal acts may blur, their meaning does not…one (self injury) is an alternative to the other (suicide). Figures quoted in the Scottish Executive report on tackling suicide “Choose Life” indicate that only 1% of people admitted to a hospital for a self harming injury will die by suicide or undetermined death within a year. Only 3-5% of those people will die in similar circumstances in the next 10 years. Bearing in mind Penumbra’s information that most self harm does not result in a hospital admission then the risk of suicide is relatively low in relation to all self harming episodes. However there is a link which is important and which warrants further engagement and investigation with people who self harm. Of actual completed suicides 40-60% come from people who have been admitted to hospital for a self harming injury (Keith Hawton Oxford University). There is a piece of research funded by the Scottish Executive going on at present with young people in contact with Penumbra who have experience of both self harm and suicide. Within the group of people who self harm there appears to be groups of people who have a higher risk of drifting into a “suicidal space”. We feel that engaging with this group of people will shed more light on why, when most self harm can primarily be a way of coping some people who self harm can end up feeling suicidal. Gender Issues Ongoing research indicates that self harm is more prominent among females that males. The recent National Inquiry into Self Harm Among Young People quoted a number of studies which indicated the prevalence of self harm is significantly higher among young women than men. Many reasons have been suggested for this. It can sometime be related to the role and expectations of women in society. Often women are the main carers either for their children or parents putting other people first and denying their own feelings. Unfortunately their own needs do not go away and can contribute to great internal pain and subsequent self harm in response to this pain. Pressures around body image can lead to young women in particular loathing their bodies. Often women who have been sexually abused feel they have contributed to the abuse and use self harm as I mentioned earlier to punish themselves. They may also use self harm as a way of distracting any further male attention. Penumbra sees a higher number of young gay, bisexual and transgender young women than expected in its self harm projects and many of these young people have been on the receiving end of bullying for many years due to being seen as “different”. It is well documented that young women from black and minority ethnic communities are more likely to self harm than their white counterparts. Bhardwaj (2001:55—56) says that cultural beliefs can both legitimise gender violence (such as domestic abuse) and oppression whilst also silencing women from discussing or seeking help because by doing so would bring shame and dishonour to themselves their families and community. This may be contributing to young women resorting to coping in private and may explain the higher prevalence of self harm among this group. Education, Training and Support While having dedicated self harm projects has helped Penumbra to continue to reach out to young people who self harm and learn from their experiences we believe that there should not need to be projects that specifically work with this issue. Penumbra believes that the most important people who can help and support people who self harm are people who have day to day contact with them. Therefore we feel that anyone who is working in an environment which may bring them into contact with this issue should have access to good quality information, training and support. Agencies should be looking to develop policies and guidelines for working with people who self harm which state clearly how they expect staff to support and respond to people who self harm and Penumbra also feel that it is important to involve people who self harm in developing these policies and guidelines. Patrick Little, Scottish Development Manager (Young People), Penumbra, Norton Park, 57 Albion Road Edinburgh, EH7 5QY, E-mail: patrick.little@penumbra.org.uk MAINTAINING INTEGRATY WHEN LANGUAGE FAILS HELEN MACWHITE Communication Officer, Bodywhys Abstract In this presentation I will explore self harm as a means of expressing something that it does not feel safe to express in words – either because the language has never been learned or because those at whom the message is aimed are unable to hear it. I will draw on my experience of providing support to people with eating disorders, many of whom self harm, some of whom will complete suicide. I will also draw on my experience of providing support for family members and friends struggling to find constructive ways of supporting a person towards recovery. I will briefly put forward some ideas that can be helpful in supporting a person towards more helpful coping strategies and that might also play a role in prevention strategies for both self harm and suicide. Both suicide and self harm are realities that anyone working in the area of eating disorders needs to be prepared for. Living with an eating disorder and struggling towards recovery from an eating disorder can be overwhelming experiences, not just for the person with the eating disorder, but also for partners, parents, siblings, other family members and friends on whom the eating disorder will inevitably have a significant impact. In fact, in many ways, eating disorders are about overwhelm. Eating disorders have the highest mortality rate of all psychiatric disorders. The most common causes of death related to eating disorders are due to complications of the disorder such as cardiac arrest or electrolyte imbalance, and to suicide. Where death has resulted from completed suicide the contributing factors are most likely to include a combination of depression intolerable levels of anxiety the cumulative effect of intolerable feelings of hopelessness , of ineffectiveness, of inadequacy, of isolation feelings of total battle weariness, of being unable to ‘keep up the fight’ no longer feeling able to carry the double burden of one’s own pain and anguish and the pain and anguish inflicted on others coexistence of other psychiatric problems Within the context of the services provided by Bodywhys the interface with suicide occurs in a number of different ways. Typical examples might include disclosure of suicidal intent disclosure of suicidal thoughts (present or historical) disclosure of and reaction to the completion of suicide by a significant other disclosure of and reaction to a significant other’s suicidal intent or thoughts These events can occur during a call to the helpline service, in an email communication to the email support service, during the course of an online meeting or a face to face support group. Interface with self harm occurs in much the same way but is much more common as a significant percentage of people with eating disorders engage in self harm. Indeed, the relationship between self harm and eating disorders can be viewed as intimate. If we adopt as a definition of self harm “the act of doing anything knowingly damaging to yourself for a reason” this would include harming oneself by means of self-injury (e.g. deliberate cutting, bruising, burning, tearing out of hair) and it would also include binge drinking, smoking and drug taking, as well as many of the behaviours associated with eating disorders (self-starvation, self-induced vomiting, misuse of laxatives, excessive bingeing, excessive exercising). Some sources estimate that approximately 25% of people with eating disorders engage in self harm by means of self injury (Eating Disorders Review 2002; 10:205). At this point it may be helpful to clarify that although many people believe that there is a direct link between suicide and self harm, this is in fact inaccurate. While many people who have completed suicide may have self harmed at some point, the majority of people who self harm are not attempting to end their lives or even to communicate that they are entertaining thoughts of wanting to end their lives. In order to be able to respond effectively to self harm, it is essential to understand that self harm is an attempt to preserve life rather than to destroy or end it. It is used as a survival strategy and as such it should not be regarded as an attempt at suicide. There are many parallels between eating disorders and self harm that can provide us with clues in our quest to find better ways of responding to and, ultimately, of developing prevention strategies for self harm (and many of these could also be applicable in the context of suicide): As with an eating disorder self harm develops as a coping mechanism. It is a means of coping with distress/ of surviving one’s emotional states/ of avoiding the direct experience of one’s emotional states modulation of affect is achieved through the body the behaviour patterns are habit forming the person comes to rely on the behaviour in order to cope with feelings (there is a significant element of dependency) there is a huge amount of guilt and shame associated with the behaviour (and the emotional states induced by the behaviour) which breeds secrecy fear and anxiety around how the person will cope if they cannot self harm makes it very difficult to tell someone about what they are experiencing Other similarities that might offer insight relate to the psychological make up of the person such as - low self esteem and experiences of feeling inadequate - difficulties coping with stress/ frequent or continuous sense of overwhelm - difficulties around assertiveness (the person feels disempowered and anticipates disempowerment) difficulties dealing with conflict problems with separating from the family and normal individuation difficulties discerning, establishing and maintaining boundaries difficulties identifying and expressing needs marked tendency to be other referrant (locus of evaluation placed outside of the self) significant experience of pressure to perform A close look at the above lists highlights two very important factors. Firstly, many of the characteristics listed above are related to a fragile sense of self and secondly, they are related to difficulties or disturbances at the level of communication. These two factors can themselves be seen as very intricately linked and can be used to inform our response to the person who self harms. For many of the people who reach out to our services it has taken a huge amount of courage to make that call or write that email, or decide to attend that support group. It may be the first time that they have spoken about their eating disorder or any related issues and they will be very apprehensive about the reaction they will encounter. For some, the very act of making contact might prove too overwhelming for oral communication to be possible. They might remain on a helpline call in silence or attend a group without actively participating. How this first contact is met is crucial. Given the nature of our services, this may be the only contact we have with them. For this reason it is our job first and foremost to ensure that the contact has been one that will enhance rather than hinder the person’s willingness and capacity to reach out again, whether that be to our services, or to someone else. Part of my work over the last number of years has been to help develop information resources and training for the volunteers who provide our services – those who take the calls on the helpline, or who respond to emails on our email support service, and those who facilitate either online meetings or face to face support groups. I will look here at some responses that can lead to the building of resilience and that will in turn enhance the person’s capacity for the communication of distress and for more effective communication generally. In Bodywhys training for volunteers, a huge emphasis is put on active listening skills that are underpinned by an attitudinal stance based on the core conditions of person centred work, i.e. Acceptance (unconditional positive regard), genuineness (realness or authenticity), and empathy. The presence of these qualities alone will help to create the potential for healing to occur. Active listening involves being able to hear on several levels simultaneously, picking up not just on the content but also on the way it is being conveyed, tuning into how the other is feeling, to how they are experiencing and viewing what is happening to them. The quality of presence brought to an encounter will be felt keenly and will determine to what extent a person will feel able to say what they need to say, and to say it as fully as possible. It will also determine how well they are able to hear their own words in a way that will empower them to acknowledge ‘where they are at’ so that movement forward becomes more possible. Accepting the person as they are without putting any expectation on them to change their mind state or behaviours is essential. Change can only occur if it has been preceded by acceptance of what is. This is not easy when we are in the presence of someone who is in deep distress and who is engaging in behaviours that carry a risk. Acceptance involves a caring response that is uncontaminated by judgement or evaluation of the thoughts, feelings or behaviours of the other person. It is about valuing, respecting, accepting a person unreservedly no matter what they have done or are doing, no matter what their opinions are, what decisions they may decide to make. It serves to create a climate within which the person can feel safe and free to express themselves without judgement. Acceptance does not always have to be voiced. It can be communicated through shared silence, through taking care not to interrupt, through withholding criticism or comment. Developing acceptance involves developing an awareness of our own assumptions and prejudices which can impose conditions of worth on the person with whom we are interacting. An awareness of how our own needs might come in the way of a supporting/ helping relationship is also essential. Are we allowing the person to really be as they are or is our need to fix things, to make things better, to know that we have made a difference getting in the way of our capacity to remain focused on the needs of the person who is in distress and to offer full acceptance? Genuineness is simply about being real, about just being yourself and not assuming a role or façade of any kind. When I am genuine or congruent, I am who I am. I am being real. I am in touch with my own flow of experiencing. I am able to own the thoughts, the feelings and attitudes flowing through me. It is not necessary for me to express these – an awareness of them is enough to increase my capacity for both acceptance and empathy. It is said that genuineness is ‘contagious’. Being genuine encourages the person with whom you are communicating to be genuine too. Your being just yourself has the effect of giving them permission to be themselves and not to be over-concerned with notions of how they should be. Through your genuineness you are providing them with an example, a model. They will be less likely to pretend, to deny, to hide, to conceal thoughts and feelings, to be defensive. Genuineness allows for the development of trust and facilitates disclosure. Empathy refers to our ability to experience the other person’s world as if it were our world, but without losing the ‘as if’ quality. Empathy is different from sympathy which has its roots in our own thoughts and feelings about what is happening. It involves entering into the private world of the other person in order to understand it, irrespective of whether we feel sympathy. It is different also from identification (‘I know how you feel because something similar has happened to me’). With empathy, the uniqueness of the other’s experience is fully respected and the frame of reference remains that of the other person. A prerequisite to being able to bring these qualities to our response to an individual in distress is self awareness. Active listening involves listening to the other while simultaneously listening to yourself. This practise of inner listening (listening to yourself, being aware of your own thoughts and feelings in the process) can be vital to the quality of your outer listening (listening to the other and tuning into their experience of the process). The benefits of good active listening skills when interacting with a person who is in distress are that they help to establish rapport (a sense of a relationship in which the speaker feels the listener is available and willing to focus on his/her needs) establish and build trust (a belief in the honesty, integrity and reliability of the other which will also increase openness to further contact) create feelings of acceptance, safety, and understanding (helps to dispel any fear of rejection or ridicule or of being pressured to make changes beyond what is perceived as tolerable) facilitate disclosure increases self esteem (a sense of both self worth and self competence) This last point is of immense significance as every experience of the self being affirmed is helping in the task of building resilience and slowly opening the person to a healthier way of relating to themselves, to others, and to the world around them. Research into the etiology of both eating disorders and of self harming behaviours often focuses on very early development and its impact on the separation and individuation processes. Coming into the world is an overwhelming and potentially traumatic experience by any standards and the subsequent task of learning to be in the world is a highly challenging and complex business. We are not in control of it. Our survival is continually dependent on a feedback loop between our internal world and the external world. Whether or not a person experiences the world as a hospitable, accepting, safe place in which they can be themselves freely and fully is dependent on a myriad of factors related to the functioning of that feedback loop. There are many things that can cause the feedback loop to contain a surcharge of anxiety. Surges of anxiety are a natural aspect of the feedback loop. It is the way in which these surges of anxiety are mediated within the feedback loop that sets up a pattern for dealing with overwhelming emotions. If a surcharge of anxiety is continuously sustained this can ultimately lead to an incapacity to express emotions appropriately and to integrate experience and the individual will develop behaviour patterns that will display a dominance of anxiety relieving strategies that do not involve a mediating factor that elicits a response from the world around them. Self harming behaviours can be seen as fulfilling this anxiety alleviating function in this way. What cannot be communicated in words or actions is mediated through the body and directed at oneself. This type of behaviour also ensures that distress remains hidden from others and the integrity of the self is further protected from anticipated disintegration. Of course, the relief is short lived because the underlying factors that have led the person to respond in this way have not been modified. When a person is coping with life in this way, the journey through life becomes a constant struggle to survive and this can lead to a sense that life is not being lived but is being bypassed. There is no sense of effectiveness, no sense of one’s capacity to shape one’s world. Discernment of objective reality is problematic. The self harming behaviours provide a means of coping with the intolerable sense of alienation that ensues. Unfortunately, the energy that is put into coping in this way also serves to perpetuate a vicious cycle of withdrawal and isolation from the objective world thus compounding the isolation and increasing the distress. Self harming allows the person to maintain a ‘window of tolerance’ that insures survival. Respectfulness of this window of tolerance is essential and can be achieved through the attitudinal skills outlined above. A significant key to improving our response to mental distress and to building resilience in those who resort to self harming behaviours in order to survive is rooted in self awareness and effective communication skills. Each one of us can contribute to both the alleviation and prevention of mental distress by developing these skills for ourselves and thus improving our capacity to meet those in distress in a way that makes them feel valued and safe. Each time that they experience such an encounter, it creates the potential for them to move from a fear based response to life to a more trust based response. Ms. Helen MacWhite, Communications Officer, Bodywhys Central Office, PO Box 105, Blackrock, Co Dublin, E-mail: communications@bodywhys.ie Chairperson: Seán McCarthy - Comments It was a privilege and a pleasure to chair session 4 at the Irish Association of Suicidologys’ 11th Annual Conference. The session provided an opportunity to the presenters to share both their experiences and research findings. These presentations were extremely relevant and insightful and contributed in a meaningful way to the dialogue around the issues around self-harm and the whole area of communication with people in distress. Mr. Pat Little who is Development Manager with the Penumbra services in Scotland presented us with an overview of their services. They currently run 6 projects across Scotland and are funded by Choose Life (Scotland Executive National Strategy for Suicide Prevention) to tackle self-harm issues. Findings of research conducted by Penumbra called “No Harm In Listening” were presented. I was particularly taken with this as it acknowledged the insights of young people when designing programmes/interventions for young people. Many of the young people who contributed to this research had experienced self-harm and attempted suicide. Helen McWhite is Communications Officer for Bodywhys. This is a voluntary support organisation for people with eating disorders their family and friends. Their services include a network of support groups throughout the country, a helpline and an education and awareness programme. During this presentation, the self-harm event as a mean of expressing something that it does not feel safe to express in words was presented. The reasons behind the difficulty with the communication, be it either an inability of the individual to express their distress with appropriate language or the inability of the person at whom the message is aimed at to hear it were discussed. Ideas that can be helpful in supporting a person towards more helpful coping strategies and that might also play a role in prevention strategies for both self-harm and suicide were discussed. POSTERS THE EXPERIENCE OF PATIENT SUICIDE AMONG GENERAL PRACTITIONERS MS MARY MOORE-CORRY¹²³, MS ELAINE MCMAHON²³, DR MARGARET KELLEHER²³, PROF COLIN BRADLEY³4, DR ELLA ARENSMAN²³. 1 Doctorate in Clinical Psychology, University of Limerick, 2 National Suicide Research Foundation of Ireland, 3 Cork and Kerry Alliance for Depression and Suicidal Behaviour (CKADS), 4 Department of General Practice, University College Cork The General Practitioner (GP) is the first, and sometimes the only, health professional that individuals, who die by suicide contact within the health and social services. There is a clear lack of research in the area of the personal and professional impacts of such a client group on the GP. This study set out to elicit and explore GP views of the impact of patient suicide among General Practitioners. A qualitative study using in-depth interviews were conducted with a GP sample varying in gender, age, years in practice, urban/rural location, public/private patients, and specific psychiatric training was carried out. Eight GPs who had shown an interest in being involved with the Cork and Kerry Alliance for Awareness of Depression and Suicidal Behaviour (CKADS) run by the National Suicide Research Foundation (NSRF) were interviewed. Interviews were transcribed and analyzed using thematic analysis. Professionally, suicides for the GP can mean a great deal of self analysis of their work. The analysis revealed that GPs generally felt that although the effects of a suicide was devastating, there was a certain amount of acceptance in that as being all part of their profession. Personally, GPs found that suicide, as with any patient sudden death, was difficult to cope with in terms of dealing with one’s own emotions while trying to deal with the relatives and family. There was a huge sense of loss when the GP knew the patient well. A number of GPs reported the feeling of shock at the news of a suicide being related to the lack of any suicide ideations or serious intent during their consultations with them. Concern was noted with respect to the levels of support available for GPs to get through the death of a patient by suicide. Training and educational issues were also identified and implications for the provision of personal therapy, reflective practice group model and supervision were discussed. SUPPORTING THE SUICIDE BEREAVED OWEN O’MAHONY P.R.O. Clare Living Links Abstract The feelings and reactions to suicide bereavement have aspects in common with other bereavement. There is shock, disbelief, denial, sadness, loss, anger, blame and the need to come to terms with the event. Friction within the family unit is often a major problem and some families become totally dysfunctional. Grief is a different levels within the family unit and this leads to accusations of “you have forgotten very quickly” to “you were always the selfish one”. Circumstances such as this prevent conversation and prohibit the exploration of feelings. In general, after a death, neighbours and friends offer support and help. This support tends to die our after a short period and individuals and families have to deal with the event on their own. There is also mutual avoidance. Neighbours and friends feel incapable and are unsure what to say or do. For various reasons, the bereaved avoid speaking about what happened. At this stage many people do not know where to look for help and support. Prior to the bereavement little attention was paid to the existence of the available support and now in the aftermath of suicide, with the resultant emotional confusion, many people feel isolated, not knowing that help is available or where to look for this help. Being aware of these factors those involved in Living Links are conscious of the need to use any available means to inform people that help and support is available. What is Living Links? Living Links is a groups of trained volunteers providing a listening/support service which is free of charge and available to any person in the community including emergency personnel, gardai, clergy etc. and anyone who has been in any way effected by suicide. The group is supported and guided by an executive committee and the Organisation is under the auspices of the HSE. In each area a group of people are interviewed as regards suitability and then asked to undertake a training programme specifically designed towards suicide bereavement support. The training programme is comprised of formal lectures and workshops relating to the immediate needs of the bereaved, exploration of grief and how to deal with it, the role of the gardai and the coroner’s court. Trained volunteers are now available in a number of areas to offer confidential practical support and advice to families who have experienced a death by suicide. At the request of the family or individual, the Suicide Outreach Support Person can call to the home or meet at an agreed location. The outreach worker can provide information and practical support concerning the following areas: The funeral The inquest Entitlements What to say to children How to deal with the neighbours Help the person to clarify their personal grief Connect the person to other support services in the area Provide information on suicide and attempted suicide Be there as a friend for the person Living Links Objectives are: To provide support and outreach to those bereaved by suicide. To increase awareness and understanding of suicide and its effects on individuals, families and communities. To liaise and exchange information with similar support groups nationally and internationally. To support and encourage relevant research. To produce leaflets and associated literature for the survivors. To liaise with and provide families with information on health services available in the region, and the referral pathways to such services should professional counselling or other help be required. To provide and facilitate a group healing programme, on a needs basis for the suicide bereaved. To encourage the suicide bereaved to establish and foster an ongoing support group among themselves. In addition to one to one support for individuals and families Living Links volunteers provide and facilitate a group Healing Programme on a needs basis for the suicide bereaved. The programme consists of eight two hour sessions which include three to five people in each group with one facilitator. Families are separated in the small groups where possible. Each group has a lighted candle as a symbol of confidentiality. The Aims of the Healing Programme are: To help adults, who have experienced a death by suicide, to find healing and support in a safe and caring environment. To provide an opportunity of meeting others who have experienced loss through a death by suicide. To provide healing through talking and listening in small groups. Mutual help is received and given through sharing. Living Links Nationally East Cork 087 1370792 Galway City & County 091 565066 Limerick City & County 087 7998427 North Tipperary 087 9693021 Co Clare 086 0565373 Co Kerry 087 9006300 Co Meath 046 9021407 Co Wicklow 01 2868413 Mr. Owen O’Mahony, P.R.O. Clare Living Links, E-mail: abomahony.ennis@eircom.net SAMARITANS GERRY DOBBIN Abstract Samaritans was founded in 1953 and provides confidential emotional support, 24 hours a day for people who are experiencing feelings of distress or despair, including those which may lead to suicide. Samaritan support is provided by phone(08457 90 90 90 in the UK and Northern Ireland and 1850 60 90 90 in the Republic of Ireland);through visits to individual branches; by letter and email (jo@samaritans.org.) There is also a Samaritan presence at major festivals. People who contact Samaritans are listened to in confidence and treated in a non-judgemental way. Suicidal feelings are explored at every opportunity. Samaritans are there for those who are experiencing feelings of distress or despair, people who may feel lonely and isolated and those who have come to a point when life is getting too much to bear. Samaritans are prepared to listen regardless of how trivial or disturbing a problem appears to be. Our message to our callers is: no matter what you are going through, you're not alone. We're here to listen to peoples concerns, worries and anxieties any time, day or night. We don't judge people, nor do we tell people what to do. What we will do is give people time to think things through, listening with an open mind and in complete confidence. People who contact Samaritans can share their innermost feelings without fear, criticism or judgement and be safe in the knowledge that it is confidential and also anonymous. Samaritans believe that simply talking about feelings and being really heard can make a difference- sometimes the difference between life and death. It is part of our vision for society that if people are free to explore their feelings in a safe and non-judgemental way and if people are able to acknowledge and respect the feelings of others then fewer people will die by suicide. Samaritans volunteers befriend people who feel they have no where else to go: people who may feel betrayed by life and are desperate, lonely or suicidal. Volunteers are the Samaritans greatest resource. There are approx. two thousand such volunteers manning twenty branches in Ireland, 24 hours a day, seven days a week. Samaritans volunteers are ordinary people who are open minded and who have natural listening skills; People who respect confidentiality and who have care and compassion for other human beings. Samaritans volunteers do not invoke religion, philosophy or personal view points when engaged with callers, nor do we give advice or direction. Recruitment and training take place annually. The initial training is intense and comprehensive. Volunteers also have to attend ongoing training on an annual basis while they are with the organisation. Samaritans are continually developing our service to meet the needs of our callers. As well as our twenty four hour phone service, people may visit our branches during specified daylight hours. In recent years an e-mail contact service has been provided jo@samaritan.org -and this year a new text service has been launched -text phone at 1850-60-90-90. Samaritans also provide our service in various prisons. In addition, volunteers attend major festivals around Ireland during the year befriending people at such events. Samaritans work in partnership with local and national government, businesses, local organisations and the media in order to raise awareness of suicide and the importance of listening to others. Samaritans school talks programme is particularly relevant given the high number of young people who self harm and who take their own lives. We talk to young adults about the issues that concern them and offer them a forum to discuss these issues in a real and open way and also raise awareness and understanding of the service that Samaritans provide. Samaritans......when needed we are there; when it would help to talk to someone who cares, someone who will stay with you, contact Samaritans. What ever you are going through, we'll go through it with you. Mr. Gerry Dobbin, Samaritans. E-mail: dobcat@eircom.net PAPER PRESENTATIONS REACH OUT, THE NATIONAL STRATEGY FOR ACTION ON SUICIDE PREVENTION DEREK CHAMBERS, GEOFF DAY, ANNE CALLANAN AND KAREN MURPHY National Office for Suicide Prevention Abstract Reach Out, the national suicide prevention strategy, was launched in September 2005 following nationwide consultation. Implementation (in three phases) of this broad-based ten year strategy is being coordinated by the National Office for Suicide Prevention (NOSP). Actions are being implemented across four levels of suicide prevention as follows: General population actions Targeted (risk group) actions Responding following suicide Information and research Implementation Plan Monitoring of implementation will be facilitated by the identification of broad time frames, lead agencies and ‘deliverables’ for each action in the strategy. In the first year of implementation, the NOSP appointed an advisory group and established a national forum of stakeholders. In addition, a 12-point service plan was agreed for 2006, based around Phase 1 actions, addressing the following issues and actions: Making it Happen 1. To establish a national forum of key stakeholders (Reach Out p.17, 18 (Making it Happen) Level A – General Population 2. To deliver agreed training programmes (e.g. Action 7.3) 3. To work with the media (Reach Out Action Area 9) 4. To launch a national mental well being campaign (Reach Out Action Area 10) 5. To pilot a ‘gateway’ service post to inter-face between Primary Care and Secondary Services in responding to suicidal crises (Reach Out Action 11.5) Level B – Targeted Actions 6. To develop services to respond to presentations to hospital following deliberate selfharm (Reach Out Action 12.3) 7. To develop a travellers suicide prevention project (Reach Out Action Area 15) 8. To complete research into the link between institutional abuse and suicide (Reach Out Action Area 19) Level C – Responding following Suicide 9. To review and develop bereavement support services (Reach Out Action Area 23) Level D – Information and Research 10. To review and improve suicide mortality data collection (Reach Out Action 25.2) 11. To develop methods of reaching people (especially young people) through Information and Communications Technology (ICT) (Reach Out Action 25.4) 12. To agree a national programme of research on suicide prevention in Ireland (Reach Out Action 26.1) This paper presents an overview of progress in relation to the 12-point plan outlined above. Process in Implementation Making it Happen 1. Establish a National Office for Suicide Prevention and Convening a National Forum of Stakeholders (Making it Happen) The National Office for Suicide Prevention (NOSP) was established by the Minister for Health and Children at the launch of Reach Out in September 2005. The NOSP held its first National Forum Meeting in March 2006. The Forum was attended by over 100 representatives from a wide range of suicide prevention and mental health promotion agencies. Plans are underway for the next Forum in 2007. Level A – General Population 2. Training & Awareness Programmes (e.g. Reach Out Action 7.3) Reach Out sets a challenging agenda for the development and delivery of training and awareness programmes for communities, organisations and professionals. Such training will need to be delivered at both local and national levels. Some training in suicide prevention is already undertaken at local HSE level and through voluntary organisations. Mental health promotion training also takes place through HSE health promotion services. The NOSP secured approval for one National Training and Development Officer and three Regional Training Officers. The HSE is currently recruiting for these posts on behalf of the NOSP. The NOSP will continue to coordinate delivery of the ASIST (Applied Suicide Intervention Skills Training) programme which has already trained over 70 trainers and delivered nearly 100 workshops to ‘gatekeepers’ around the country. 3. Media (Reach Out Action Area 9) Revised Irish Association of Suicidology (IAS) /Samaritans media guidelines were launched in June 2006 simultaneously in Dublin and Belfast. The IAS are also planning an awards event in 2006 to acknowledge journalists who have demonstrated sensitivity and understanding in reporting on suicide prevention issues. These awards will be partfunded by the NOSP. A print media monitoring study was finalised in 2006 and published by the NOSP. This monitoring study will be used in the development of training modules for students of journalism. Headline is a new media monitoring campaign being developed by an alliance of voluntary support organisations and the NOSP under the management of Schizophrenia Ireland. Staff have been recruited to lead the campaign which, it is intended, will facilitate improved working relations with the media in covering issues around suicide prevention and mental health. 4. National Mental Health Promotion Campaign (Reach Out Action Area 10) The NOSP has prepared a detailed project plan for the development of a major national mental health awareness campaign which will be developed in partnership with the National Office for Social Marketing of the HSE. The aim of this campaign is to launch, in conjunction with voluntary organisations, a national multi media campaign to impact on the stigma of mental health and to encourage help seeking. The campaign will be developed through a professional advertising/media agency (engaged by HSE) with a view to launch in late 2006. The campaign will be whole population based initially but as it develops over time more targeted/local campaigns will be initiated. A public attitudes survey will be conducted prior to launch in order to generate baseline information that will facilitate evaluation of the campaign at a later stage. 5. Pilot ‘gateway’ worker between Primary and Secondary Care (Reach Out Action 11.5) A pilot service to inter-face between primary care and secondary services in the management of suicidal crises is being developed as a partnership between the Cluain Mhuire Service in Dublin and the NOSP. The service will be lead by an experienced mental health professional and will be evaluated with a view to informing such service development throughout the HSE. This mental health professional has been recruited and the evaluation methodology is currently being agreed. Level B – Targeted (Risk Group) Action 6. A&E response to deliberate self harm (Reach Out Action 12.3) Additional resources were made available in 2005 to put in place experienced psychiatric nursing staff in A & E departments to respond to deliberate self harm presentations. Further investment will be made in 2006 to ensure that all A & E departments have a service to respond to such presentations by the end of the year. 7. Travellers Suicide Prevention Project (Reach Out Action Area 15) The NOSP has worked with an alliance of travellers support groups to develop a project worker post to support suicide prevention activities among the traveller population in Ireland. The project is due to commence in the coming weeks. 8. Institutional Abuse and Suicide Risk (Reach Out Action Area 19) There is some anecdotal evidence that those who have suffered institutional abuse have a high rate of suicide. The National Suicide Research Foundation have been commissioned to examine the risk associated with suicide for victims of institutional abuse and to advise on service needs. Interviews with survivor support groups and staff of the National Counselling Service have taken place. Seminars with victims of abuse have been attended throughout the country and a Phase One report on the project has been finalised. The findings of Phase One were accepted for presentation at the 2006 IAS Conference on Suicide Prevention (September, 2006). Level C – Responding following Suicide 9. Support the Development of Bereavement Support Services (Reach Out Action Area 23) A major national review of bereavement support services has been commenced on behalf of the NOSP, involving statutory and voluntary service providers in the area of general and suicide-specific bereavement support services. As part of the review a detailed directory of support services will be completed and made available online. The results of the review will be used to inform a national bereavement support care plan. In the meantime, the NOSP has provided existing services in the area of suicide bereavement support with funding of over €200,000 to ensure ongoing and expanded service provision while the national review work is being completed. Level D – Information and Research 10. Data collection on Suicide Mortality (Reach Out Action 25.2) Recording practices in relation to mortality from ‘external causes’ is currently being reviewed and a report will be made available in late 2006 highlighting current practice and making recommendations for future developments in recording practive to ensure accuracy of mortality data. A specific target in relation to the reduction of suicide rates in Ireland will be set if the accuracy of suicide mortality data can be determined. It is intended that a system of data collection will be developed that will allow more in-depth information on trends in suicide mortality so that more effective prevention strategies can be developed. 11. Reaching Young People (Reach Out Action 25.4) The NOSP is exploring ways of reaching young people through email and text messaging in order to develop a sustainable programme of action which can be funded in late 2006/2007 onwards. We will be consulting young people, voluntary organisations and those using technology in innovative ways to provide services for young people. To date, some support has been provided to one such service based in the north west but targeting young people nationally, i.e. www.spunout.ie. 12. National Research Programme (Reach Out Action 26.1) There is much research on suicide/self harm being undertaken at local/national and international level. It is important to ensure a coordinated approach to funded research and in particular to use such research to influence future suicide prevention activity. A national research meeting was held in June 2006, bringing together all of those involved in research in order to seek agreement on a national research plan. It is planned that a national research network will be developed comprising participants at this inaugural national research meeting. Future Developments Progress is being made in implementing Reach Out, and this progress can be clearly monitored in the context of the Action Plan that was incorporated into the strategy. By assigning something ‘deliverable’ next to each of the 94 actions in the strategy process evaluation has been facilitated. Therefore, the NOSP can answer the question “did we do it?”. However, the question “did it matter?” is more complex and will require an independent outcome evaluation of the implementation so that we can answer the question “did it matter?”. In 2007, the NOSP will be commissioning this independent evaluation of Phase 1 Reach Out implementation. Mr. Derek Chambers, Mr. Geoff Day, Ms.Anne Callanan and Ms. Karen Murphy National Office for Suicide Prevention, Room G29, Population Health, Dr. Steevens Hospital Kilmainhan, Dublin 8. Tel: 01 6352179 MATERNAL SUICIDE: A TWENTY YEAR REVIEW OF SUICIDES IN THE UNITED KINGDOM BY NEW MOTHERS AND PREGNANT WOMEN IAIN W. MCGOWAN, MARLENE SINCLAIR School of Nursing, University of Ulster Abstract In the United Kingdom suicide has recently been noted as the main cause of maternal death. This paper will outline preliminary results of on-going research into the prevalence and characteristics of maternal suicide in the United Kingdom since 1985. The prevalence of maternal suicide in the UK will be presented followed by the characteristics of the completed suicides, to include age of the mother at death, the outcome of the pregnancy, marital status of the deceased, method of suicide and the length of time from birth. Finally, the implications for paediatricians, midwives, general practitioners and health visitors will be discussed. AN INVESTIGATION INTO THE RISK AND PROTECTIVE FACTORS FOR SUICIDAL BEHAVIOUR AMONGST PERSONS WHO HAVE EXPERIENCED INSTITUTIONAL CHILD SEXUAL ABUSE MARTINA O’ RIORDAN, ELLA ARNESMAN National Suicide Research Foundation Abstract Studies examining the relationship between childhood trauma and adult suicidal behaviour have reported evidence that the two are frequently linked. Preliminary results from this qualitative study indicate factors associated with suicidal behaviour most frequently cited by specialist support professionals were alcohol/substance abuse (13 out of 15 counsellor/therapists) and social isolation (6/15). Other factors included a lack of experience of forming attachments or developing coping skills by those who had entered the institutions as babies (4/15), a feeling of anti-climax following their settlement from the Redress Board or ill-advised spending of their award (3/15) and impulsive behaviour (3/15). The most frequently cited protective factors were the ability to form lasting relationships or marriage (12/15) and having children (7/15). Other protective factors included education (4/15), being in employment (3/15) and having the support of a survivor group (3/15). This information provides a valuable basis for a study comparing persons who experienced institutional child sexual abuse and who died by suicide versus those with a similar experience but who did not engage in suicidal behaviour. Introduction Following the Industrial Schools Act of 1868, the Irish state developed a system of institutional care for children which continued for over one hundred years. These industrial schools were run by religious orders and funded by the public, their remit being to care for ‘neglected, orphaned or abandoned children’ (Rafferty & O’Sullivan, 1999). Children were placed in institutional care either by referral from the Health Board, by private arrangement or by order of the courts. The number of children in industrial schools peaked in 1900 with 8,000 children in 71 schools. By 1969 there were under 2,000 children in 29 schools as the suitability of the institutional care system came into question. In response to growing criticism, the Government commissioned District Justice Eileen Kennedy to enquire into the industrial school system. The Kennedy Report was published in 1970 and recommended that institutional care was not appropriate for children. Schools began to close during the 1970s and eventually in 1984 the Government decided that foster families were a more suitable place for children in the care of the state. However, it was not until media attention in the late 1990s with documentaries such as Dear Daughter and States of Fear that the horrifying picture of widespread abuse, deprivation and neglect in the former institutions became evident. On the 11th May 1999, An Taoiseach Bertie Ahern apologised on behalf of the Irish government to its citizens who had been abused in institutions as children. Following this apology the National Counselling Service (NCS) was established in September 2000 to cater for survivors of child abuse, with priority given to those with a history of institutional child abuse (NCS, First Report, 2002). The Commission to Inquire into Child Abuse was also established in 2000. Studies examining the relationship between childhood trauma and adult suicidal behaviour have reported evidence that the two are frequently linked (Brodsky et al, 2001; Peters & Range, 1995). Consequently, the Reach Out National Strategy for Action on Suicide Prevention, 2005-2014 has identified survivors of abuse, particularly those from state institutions, as a group that should be prioritised for suicide prevention and mental health promotion initiatives. This paper reflects the first phase of a larger research project. It consists of a detailed literature review into institutional child sexual abuse and suicidal behaviour, along with the primary results of a qualitative study with specialist support service personnel. The qualitative study seeks to highlight the factors associated with increased risk of suicidal behaviour amongst persons with a history of institutional child sexual abuse along with protective factors. Part I: Literature Review Studies included: The literature search yielded three primary studies and forty-five secondary studies, thirty-six of which met the inclusion criteria for review. Four government reports were also included. Studies were matched against four quality criteria, thus the possible range of quality scores was between 0 and 4. The actual range of scores was from 0.5 to 3.66. The inclusion criteria were one or both of the following: 1) The study investigated the nature or long-term effects of institutional abuse or child sexual abuse 2) The study examined the relationship between institutional abuse/child sexual abuse and suicide, deliberate self-harm and/or suicide ideation. The quality criteria were as follows: 1) Operationalization/definition of institutional abuse or child sexual abuse or suicide ideation, suicide attempt or deliberate self harm 2) Selection of the sample 3) Measures of institutional abuse or child sexual abuse used 4) Appropriate statistical analyses The studies were rated independently by the two authors and then cross-checked to ensure reliability. Main outcomes: There is a lack of studies addressing the relationship between institutional child sexual abuse and suicidal behaviour and related mental health difficulties. Studies focusing on the consequences of child sexual abuse in general reveal consistent evidence for an association with adult suicidal behaviour, in particular nonfatal, as well as suicide ideation (Ystgaard, 2004; Brodsky et al, 2001; Vajda & Steinbeck, 1999; Silverman et al, 1996). Research indicates that the consequences of child sexual abuse by peers are similar compared to abuse by adults in terms of suicidal behaviour and mental health difficulties (Shaw et al, 2000; Sperry & Gilbert, 2005). There is consistent evidence that child sexual abuse is associated with Post Traumatic Disorder (PTSD) in adulthood, with the severity of the abuse linked to the severity of the PTSD symptoms (Hetzel & McCanne, 2005; Peleikis et al, 2004; Schaff & McCanne, 1998; Briggs & Joyce, 1997). Research indicates that people with a history of child sexual abuse are at risk of developing mental health problems (incl. depression, sexual difficulties and decreased self-esteem) in adulthood (Modestin et al, 2005; Tanskanen et al, 2004; Zlotnick et al, 2001; Cheasty et al, 2000). Recommendations: Further research into risk and protective factors for suicidal behaviour among persons with a history of institutional child sexual abuse. Research into consequences of institutional child sexual abuse should focus on abuse by both adult perpetrators and by peers. Further research into consequences of institutional child sexual abuse among men. Part II: Qualitative Study A total of fifteen professionals offering specialist support services to survivors of institutional abuse participated in the study. A manager and a member of frontline counsellor/therapist staff from seven of the ten branches of the National Counselling Service took part. When saturation was reached amongst the NCS staff, no further interviews took place, although there was a 100% response rate from the ten branches. The MASC (Male Abuse Survivors Centre) in Galway also participated. A semistructured interview schedule was prepared by the NSRF, the recorded interviews were later transcribed and a thematic analysis was undertaken. Main outcomes: Factors associated with suicidal behaviour most frequently cited by specialist support professionals were alcohol/substance abuse (13 out of 15 counsellor/therapists) and social isolation (6/15). Other risk factors included a lack of experience of forming attachments or developing coping skills by those who had entered the institutions as babies (4/15), a feeling of anti-climax following their settlement from the Redress Board or ill-advised spending of their award (3/15) and impulsive behaviour (3/15). The most frequently cited protective factors were the ability to form lasting relationships or marriage (12 out of 15 counsellor/therapists) and having children (7/15). Other protective factors included education (4/15), being in employment (3/15) and having the support of a survivor group (3/15). Recommendations: The risk and protective factors identified in this study provide a valuable basis for further research directly involving survivors of institutional child sexual abuse. This study is supported by the National Office for Suicide Prevention Ms. Martina O’ Riordan, Dr. Ella Arnesman, National Suicide Research Foundation, 1, Perrott Avenue, College Road, Cork. Tel: 021 4277499 BASELINE CHARACTERISTICS OF DELIBERATE SELF-HARM PATIENTS RECRUITED IN A RANDOMISED CONTROLLED TRIAL OF GROUP PROBLEM-SOLVING SKILLS TRAINING COMPARED WITH STANDARD CARE CARMEL MCAULIFFE1, BREDA C. MCLEAVEY2, PAUL CORCORAN1, BERNIE CARROLL3, BRIAN O’ KEEFFE3, MARY O’ REGAN1, EVA FITZGERALD1, LOUISE RYAN3, PORTIA HICKEY1, ELLA ARENSMAN1, ANTHONY P. FITZGERALD1. 1 National Suicide Research Foundation, 2 HSE Southern Area, 3 HSE Mid-Western Area Abstract This study describes baseline characteristics and treatment satisfaction of DSH patients recruited in an RCT to determine the efficacy of a group interpersonal problem-solving skills training programme (IPSST) versus standard care. Consenting DSH patients meeting inclusion criteria were interviewed within three days of their index episode. Of the 2,654 DSH patients screened, 1,151 (43%) were eligible, of whom, 441 (38%) were randomised to IPSST or standard care. From analysis of baseline interviews 64% had previously self-harmed, while the following mean scores were obtained: (Suicide Intent Scale mean 13; Beck Depression Inventory mean 36.3; Hopelessness Scale mean 10.8). Only 32% felt they could solve their main problem. IPSST clients attended 67% of sessions and were more were satisfied with treatment (91% v 60%, p<0.001) compared with standard care clients. Higher attendance and greater satisfaction with IPSST indicate that this treatment approach is suitable for a high risk sub-group of DSH patients. Deliberate self-harm (DSH) is the most important risk factor for suicide (Hawton & Sinclair, 2003) such that those who engage in DSH are 20 to 40 times more likely to eventually kill themselves (Gunnell & Frankel, 1994; Harris & Barraclough, 1997). Deliberate self-harm among young men and women poses a significant challenge to the health system in Ireland (Corcoran et al., 2003). A total of 10,347 hospital presentations due to deliberate self-harm were made by 8,055 individuals in the Republic of Ireland in 2004 (National Suicide Research Foundation, 2005). More than one-fifth of these presentations were due to repeat acts and the proportion of presentations in Ireland due to repeat acts - as in other countries - is thought to be increasing (Hawton et al., 2003; Henriques et al., 2004; National Suicide Research Foundation, 2005). Over one-in-five of all hospital treated presentations with deliberate self-harm in the Republic of Ireland in 2004 were due to repeat acts and approximately 14.9% of deliberate self-harm patients made a further repeat attempt during the calendar year in which they presented to hospital. There is also evidence that many more individuals engage in repeat episodes, without presenting for medical treatment (Guthrie et al., 2001; Tyrer et al., 2003). There has been a longstanding lack of research evidence of effective treatment interventions in reducing repetition of DSH (Hawton et al., 1998; Arensman et al., 2001). Poorer problem-solving ability has been found among people engaging in DSH in general (Linehan et al., 1987; McLeavey et al., 1987; Rotheram-Borus et al., 1990; Pollock & Williams, 1998; Pollock & Williams, 2004), and particularly among those who self-harm repeatedly (Kehrer & Linehan, 1996; Rudd et al., 1996; Dieserud et al., 2003; McAuliffe et al., 2006) and promising results have been found for problem-solving therapy in reducing repetition of DSH (Hawton et al., 1998; Arensman et al., 2001). A recent trial of cognitive therapy that included a problem-solving component reported a significantly lower re-attempt rate (Brown et al., 2005). The failure of a recent trial - using a manual assisted cognitive therapeutic approach - to demonstrate a reduction in repeat episodes (Tyrer et al., 2003) in which over one-third of the active treatment sample received a treatment manual alone without any treatment sessions, suggests that reliance purely on a self-help approach among repeaters of deliberate self-harm is ineffective in reducing repetition (Arensman et al., 2004). Aside from repetition, a number of other important treatment outcomes should be considered using standardised measures (Arensman et al., 2001) for two reasons: Firstly, in trials of problem-solving and other psychosocial therapies, including those where a significant reduction in repetition has not been achieved, other important outcomes have been found, such as the alleviation of depression and hopelessness (Guthrie et al., 2001; Raj et al., 2001; Townsend et al., 2001; Brown et al., 2005;), improvements in problems or problem-solving ability (Raj et al., 2001;Townsend et al., 2001), and a significant reduction in suicidal ideation (Guthrie et al., 2001; Raj et al., 2001). Secondly, trials that achieve a consistently positive effect across several outcomes (e.g. depression, hopelessness) in addition to repetition, provide stronger evidence that the significance of the results is not just due to a small shift in the number of repeat attempts during a follow-up period (Brown et al., 2005). There is an urgent need for the development of effective treatments for this group of people. This presentation describes the baseline characteristics and treatment satisfaction of deliberate self-harm patients recruited in a randomised controlled trial (RCT) to determine the efficacy of a structured group interpersonal problem-solving skills training programme (IPSST) compared with standard care. Consenting DSH patients meeting inclusion criteria were interviewed within three days of their index episode. A total of 441 DSH patients in Cork and Limerick were randomised to IPSST or standard care. The IPSST programme consisted of weekly two-hour sessions of group problem-solving skills training over six weeks at a community based venue, using clients’ own problems for training sessions and practice at home. Outcomes including coping skills, symptoms of mood disorder, and repeated self-harm were measured following treatment and again six months later. Information on repeat episodes of DSH was collected up to one year following entry to the study. This is one of the first such large-scale studies undertaken in any country, and findings will have far-reaching implications for the treatment of DSH, which is known to have poor follow-up attendance rates at mental health services and to lack effectiveness in terms of repetition rates. The interpersonal problem-solving training is expected to significantly improve psychological and social functioning, and to reduce repetition rates. Results are currently being analysed, and preliminary outcomes are encouraging with regard to attendance at problem-solving group training and satisfaction with treatment. From analysis of baseline interviews of those randomised 64% had previously selfharmed, while the following mean scores were obtained: (Suicide Intent Scale mean 13; Beck Depression Inventory mean 36.3; Hopelessness Scale mean 10.8). Only 32% felt they could solve their main problem. IPSST clients attended 67% of sessions and were more were satisfied with treatment (91% v 60%, p<0.001) compared with standard care clients. Higher attendance and greater satisfaction with IPSST indicate that this treatment approach is suitable for a high risk sub-group of DSH patients. Carmel Mcauliffe1, Breda C. Mcleavey2, Paul Corcoran1, Bernie Carroll3, Brian O’ Keeffe3, Mary O’ Regan1, Eva Fitzgerald1, Louise Ryan3, Portia Hickey1, Ella Arensman1, Anthony P. Fitzgerald1 1 National Suicide Research Foundation, 1, Perrott Ave, College Rd, Cork, 2 HSE Southern Area, 3 HSE Mid-Western Area Chairperson: Sheila Dalton - Comments This part of the conference had a poor attendance unfortunately. It provided some very valuable research and information on what is happening on all fronts in the area of suicide prevention. Derek Chambers opened the session outlining the 12 point plan of Reach Out, the National Strategy for Action on Suicide Prevention. Much work has been done in the past year. It is heartening to hear of the liaising and development of professional, statutory and voluntary bodies across all sections of society. The networking of all involved in research to agree on a national research plan was good to hear. Derek said that their aim is achievable and deliverable and an independent evaluation of Phase 1 will be carried out in 2007. Iain McGowan had prepared a paper, which, in his absence was read by Mark Owens from Derry. This was a 20 year review of suicide among new mothers and pregnant women in the UK. It was a statistical study and complemented an earlier paper presented by Dr. Veronica O’Keane. It raises questions and issues. A multidisciplinary health professional approach is vital in this area. Martina O’Riordan presented her findings on the factors that influence suicidal behaviour among those who have experienced institutional C.S.A. This was interesting in the light of current media coverage. While the Redress Board makes financial settlements, further counselling and survivor groups are needed. The final paper was from Carmel McAuliffe. She compared the treatment satisfaction in those who participated in combined group solving skills along with standard treatment. There was a lesser degree of recurrent self-harm with those who participated in both. An interesting aspect of this study which was carried out in Limerick and Cork was that Limerick had a much higher degree of self-harm and repeated self-harm. It poses questions! It is not easy to remain focussed on research papers, but they are so important as they are the basis for the future intervention and services. I would actively encourage people to attend this session. Bereavement Seminar In Conjunction with CONSOLE MY STORY NUALA WHELAN Bereaved by Suicide Abstract Nuala lost her husband to suicide in July 1999, she was left with eight children ranging in age 6 – 18. Her mission now is to tell the story of how she coped and to give anybody themselves going through this horrific ordeal hope for the future. I actually found recounting my story quite a harrowing experience. However, if telling my story helps another through a similar tragedy, then surely, it will have been worthwhile. My name is Nuala Whelan. When I was 38 years old my husband John committed suicide. Today, I am a widow with eight lovely children, and as proud as punch of every one of them. They are Emma 25, Derek, 24, Anne Marie 23, Siobhan 21, Brendan 20, Eoin 17, Edwin 15 and Conor 13. It was the 19th of July 1999, the day before my eldest daughter Emma’s 18th birthday. My eldest son Derek was 17 just the day before. My husband John decided that he was going to take the day off work in order to talk to a family member. John kissed me goodbye and told me he loved me and the kids, like he always did. He left home with Emma, as he was dropping her off at work on his way. I did my usual mundane things about the house, went to work and came home at 3pm. Naturally, I began to wonder where John was, as It wasn’t like him to be out of touch with me for so long. I carried on getting dinner ready for the kids, but worrying in the back of my mind as to where on earth he could be. We had two Chernobyl boys staying with us at the time. So, when night-time came and all the children had gone to bed, I waited up for John. I was angry at first, as he must have known that I would worry. It was about 3am that morning when I started to cry and wonder - Had he been involved in an accident? Was he in the hospital? All manner of strange and weird scenarios went through my head. As morning broke, I had to pull myself together as today was Emma’s 18th birthday. I went through the day in two minds – Part of me was sick with worry on the inside and on the outside, mammy was joining in with Emma’s birthday celebrations. The children didn’t question where John was, as they were used to him working shifts. That evening, Emma took my three small children, plus both the Russian boy to her boyfriend’s house. Once they had left, I rang John’s sister to see if she had seen John and explained that he had been missing now for 36 hours. We decided to check out John’s old home, which had been lying idle for two years since being sold. John would check the house regularly. Helen and her husband Michael picked me up from home. When we arrived at the house I saw John’s car. I went from relief to annoyed in a matter of seconds. Strange to say it now, but I was going to kill him for the worry he had caused me. I passed the shed and saw an old bucket wedged in the door. Anxious and curious, I went with Helen to push open the door. A man shouted at us and in shock, I grabbed Helen thinking we had been caught trespassing or something. Sadly, that wasn’t it at all. John had been found by his brother in law Bobby, just minutes earlier and before he ran to get help, he had sent a neighbor to look out for me. It was the neighbor that shouted at me. That was the moment my world just fell apart! John had hung himself inside the shed! I stood outside and cried openly. Then it dawned on me - The Children!!!! I started to panic……. “Get me home to the children”. My head was spinning and my thoughts went into overdrive. How on earth do I tell them? What do I say? How the hell, do I break something like this to them? I rang my sister Susan, telling her what had happened and asked her to tell the five older children. We agreed that I would tell the three younger ones when I got home. That I did. I told them that Daddy had chosen to go to heaven. After consoling the children and finally getting them off to bed, my whole family; i.e. mother, father, sisters, brothers, partners, nieces and nephews arrived. The house was bursting at the seams with people. In the middle of all of this, I looked at the dresser and saw Emma and Derek’s birthday cards and could not believe that John had done this on such a happy time in his children’s lives. I felt as though I was living in some awful nightmare. A nightmare from which I could not wake! My sister Susan, my brother Ciaran and five of Susan’s children stayed to support the children and myself. At around 4am I broke down, questioning everything about John….. my life, our lives, the lives that we had built around the children - I questioned everything. I just could not understand why? I still can’t. It was shortly afterwards that I decided within myself that I had to be strong, whether I liked it or not. I kept reminding myself, that these good children had lost their daddy, (whom they idolised). I was damned sure that they were not going to lose their mother to insanity as well! This was not such an easy step to take so soon after something so harsh has been forced upon you. I had to face some more facts though….. Now that John was gone, I was no longer a wife. I was no longer my partners best friend, or part of a unit in what I thought was a marriage with sound foundations. Moreover, I had to quickly accept that I was now a widow and the only person the children could realistically look to for reassurance at this time. I never touched a drink or took a tablet during this time, as I was afraid I would become dependant on them or they would cloud my judgement. I had to be fully aware of everything around me if we were to pull through this tragedy. And I was determined that we would do just that! No matter how difficult the subject matter, we always held family meetings with the children. We still do now, but not as often. However, the meeting we held the day after John was found, had to be the hardest family meeting we had ever held. It was here that I handed the funeral arrangements over to the children and asked them to “just do it with dignity and respect”. I can proudly say, that that is exactly what they did. They all had their parts to play in the funeral. The children were fantastic. To this day though, I can’t help but wonder why John couldn’t also see, how great our children were. It is something that will always baffle me! The amount of neighbors, family and friends that called to offer condolences was huge. Day and night, night and day they came. Finally though, on Thursday night, Susan persuaded me to go to bed, as I hadn’t slept since the Sunday. I had put off going to bed, as I knew that when I woke up, I really would have to face the fact that John was dead. I was too exhausted to object now though. Ironically, the funeral was held in the same church that we were so happily married in some nineteen years earlier. All our babies were christened in the same church. Joyous occasions all of them. The church held over a thousand people and was packed inside and out, far into the car park. I looked at all those people and wondered if John really knew just how much he was loved. Normally, one can take stock of their life once the funeral is over. When the death has been one of suicide though, it is completely different. An inquest has to be held and of course, your life is on hold until that happens. One can only wait. Three months later, I decided to seek emotional help for the children. This is when I found out about Sr. Sheila and her suicide support in Bray. The three girls and myself went to the first meeting. I told them I didn’t know what to expect but we had to give it a try. Emma and Siobhain never went back but Anne-Marie found comfort there. Derek joined us later. The three younger children went to Rainbows, which was great for them. I had told them at the time, that Daddy had killed himself. I hadn’t told them that he had hung himself. Edwin asked how his daddy had died but I hadn’t the strength to tell him then. I told him that the inquest hadn’t been held but once that was over, I would be in a position to tell him. It also gave me time to put that uncomfortable matter on hold until he was at least a little older. The first Christmas came without John, but we still celebrated and for the sake of the three little ones and as they still believed in Santa. We still had our Christmas dinner. January arrived, and a brand new millennium followed, it was to be the start of a whole new way of life for me. It was also the advent of the inquest into John’s death. The inquest was hugely important to me, as the bank was looking for several mortgage payments, and the insurance company wouldn’t pay out until I had an official death certificate. The inquest was held on the 23rd January - the day before my wedding anniversary. It was a horrible experience, but it had to be done in order for me to at least start to get my life back on track. With the inquest finally out of the way, I embarked upon a mission of teaching my children how to laugh again. I started with a family meeting and I asked them all to give me a bucket of laughter for every tear they had shed. Eventually, we planned John’s 1st anniversary. Most people thought I was mad as I took the kids to Butlin’s for the day and then visited John’s grave the same evening. All in all, the day was one of good heart. It was a good day, on a bad date. As a family unit, we had to cope without John at the head of our huge and happy family. We had to cope with the fact that he had killed himself and left us to fend for ourselves. Bringing up eight children on my own really was an uphill struggle, and at times I was fraught with despair, but we all soldiered on and battled through those hard times. Seven years on and I can honestly say that my children have done both themselves and me proud. Sure, we had our bad times, but they were over-shadowed by the good times that we carved out for ourselves. Emma has a diploma in interior design and has a lovely home with her fiancée Dale. She is planning on getting married on her daddy‘s birthday. Derek has a first-class honors degree in computers science, is working in the financial centre in Canary Wharf and has just bought his first home in London. Anne-Marie achieved a first class honors degree in Law and is now a barrister. Siobhain is a qualified nurse and works in St Vincent’s hospital in Dublin. Brendan has recently qualified as an architect and works for the National Building Agency. Eoin has just passed his leaving certificate and is doing a course in interior design. Edwin is got his stupid junior certificate results as that’s what we listened to from him doing the exams and Conor is doing his junior cert even though he is 13 , as he is a sponge for knowledge. And me? Well, what mother wouldn’t be happy to see her whole family pull through hell on earth, with such flying colours? As you can see it has been a long road for us but we struggled through. That’s why I want people in the same circumstances to understand that you can live again after suicide. It is the learning that is the hard bit. Talking is important, as it helps to get out all the whys and learn to leave that big “why did he or she do it” with the person who died. Thank you for listening and I would wish that if even one person could find hope in my story then that’s my job done Ms. Nuala Whelan, 1, Farrenboley Cottages, Windy Arbour, Dublin 14 GOOD PRACTICE IN THE CORONERS COURT JOHN O’DWYER Coroner for South Mayo Abstract In this talk the role of the coroner in Ireland will be discussed. It will outline the importance and indeed the necessity of investigating deaths due to external causes such as accidents, suicides and homicides. The public interest is best served by public and open inquiry to establish the facts, to establish the truth and thereby to allay rumour and misrepresentation which can be so hurtful particularly to those bereaved through suicide. Aware that practices differ from coroner to coroner the personal approach to inquests is outlined. The importance of explaining to the relatives of the bereaved what the proceedings are and what to expect on the day is expressed. The importance of care not to add to the grief and pain of the family and the need for proper support services are available to the bereaved is also stressed. 1. The Coroner is the Legal Officer charged with responsibility for investigating sudden, unexplained or unnatural deaths. 2. A Coroner may be a Solicitor, Barrister or General Practitioner. At the present time there are 40 Coroners in the Republic of Ireland and the numbers are almost equal between Lawyers and Medical Practitioners. 3. A Coroner is subject to the general supervision of the Minister for Justice. He/She enjoys operational independence similar to that of a High Court Judge. The Coroner is solely responsible under law for the discharge of his/her duties in any decisions made by him/her in the course of his/her duties. 4. The accurate certification of the Cause of Death is the most important function of the Coroner. I suggest it reflects the recognition of civilised communities of the need for an independent and open investigation of unexplained and unnatural deaths, free from political interference or control from any outside body. 5. The Supreme Court has previously decided the number of public interest duties of a Coroner in holding Inquests and they are as follows:a) b) c) d) e) 6. To determine the medical cause of death To allay rumours or suspicions To draw attention to the existence of circumstances of which if unremedied might lead to further deaths To advance medical knowledge To preserve the legal interests of a deceased family, heirs, or other interested parties. The Coroner system puts its emphasis on investigating the relatively wide range of unexplained deaths and reflects the essential value placed on life itself. No death should be left uninvestigated unless there is a clear and certifyable reason for that death. The Coroner honours the dignity of human life by the proper investigation of the cause of the ending of life. The Coroner Service is independent of the medical profession, the Garda Siochana and all other State Agencies or any parties who may have an interest in the outcome of the death investigation. The Coroners’ Service assures society that there is an independent process of a public hearing which can establish that nothing unlawful has taken place. At the present time the Coroners’ Service operates under the Coroners’ Act, 1962. This is subject to review and Coroners are awaiting new legislation which has been promised for many years. There have been some interim changes made dealing primarily with the question of compellability of witnesses to attend an Inquest. Witnesses who are in a position to give evidence which might assist the Coroner in establishing the facts surrounding a death can now be compelled to attend an Inquest. There is also a proposal by the Department of Justice to abolish Coroners in each County and replace them with fewer regional ones. This is the position in Northern Ireland where there are 3 Coroners covering the entire North of Ireland. This is unlikely to happen in the near future unless the Department of Finance decide to buy out the Contracts of Coroners who are entitled to remain in their appointments until the age of 70. At the present time no new Coroners are being appointed and of the total number of Coroners operating at the present time, about half of these are in an acting capacity having been a Deputy Coroner to a Coroner who either retired on age grounds or who died. 7. The purpose of an Inquest is to establish the identity of a deceased person and how, when and where the death occurred. 8. All sudden, unexplained, violent or unnatural deaths must, by law, be reported to a Coroner. Examples of these include:Where a Medical Practitioner cannot sign a Medical Certificate as to the cause of death; Where the deceased had not been attended by a Registered Medical Practitioner for a documented illness, sudden infant death, road traffic accidents; accidents in the home, workplace or elsewhere; any physical injuries; falls and fractures, fractures in the elderly; drug overdose or drug abuse; neglect including self-neglect; burns or carbon monoxide poisoning; poisoning from any cause either occupational or therapeutic or accidental; drowning; hanging; firearms injuries; deaths resulting from industrial disease or accident; deaths which are directly or indirectly the result of any surgical and/or medical treatment or procedure; where there is an allegation of medical negligence; misconduct or malpractice on the part of a registered Medical Practitioner or Nurse; septicaemia which may have been caused by injury; death occurring during a surgical operation or anaesthesia; acute alcohol poisoning; deaths connected with crime or suspected crime; deaths due to homicide or occurring under suspicious circumstances; deaths of prisoners or those in legal custody in a Garda Station; death of a patient in a Mental Hospital; death of a child in care; death due to CJD; where a person is found dead or where human remains are found; death occurring in an Accident or Emergency Department of a Hospital; deaths occurring within 24 hours of admission to hospital; deaths associated with childbirth; where a patient dies in hospital having been recently discharged from hospital or discharged from a Nursing Home or other Residential Institution including a Mental Hospital or a Prison or in any other case where there is any doubt as to the cause of death. You will see that there is a wide range of deaths which are reportable to a Coroner. No Doctor may certify a cause of death which is due directly or indirectly to any unnatural cause. The Coroner’s enquiry is concerned with establishing whether or not the death was due to natural or unnatural causes. 9. A death involving self-destruction or suicide is automatically reportable to the Coroner. A Medical Practitioner cannot certify the cause of death in such a case. The legal requirements make it quite clear that where a Medical Certificate as to the Cause of Death is not available, the Coroner must cause inquiry to be made to establish the cause of death by directing a Post-Mortem examination to establish the definitive cause of death. A Pathologist’s Report following the Autopsy on a deceased person will disclose the cause of death which will clearly establish whether or not the death was due to violence or occurred in a natural manner and if it is the finding of the Pathologist that death was due to unnatural or violent means, then the Coroner is legally obliged to hold an Inquest in to such death. 10. The Coroner then directs that the Garda Siochana who act as Coroners’ Officers to take appropriate statements from all the relevant witnesses and furnish a file to the Coroner who then decides within the limitations of the Coroner’s Act, what witnesses are required and fix a date for the holding of a formal Inquest in to the death of a deceased person. 11. The Coroners’ Act is limited to establishing the identity of the deceased person and as to how, when and where the death occurred. An Inquest cannot deal with issues of civil or criminal responsibility. In fact there is a specific prohibition in the 1962 Coroner’s Act to prevent this occurring. 12. The arrival of the Gardai at a home can and does cause a lot of anxiety to a family at a time of tragedy especially in the case of suicide. However in almost 30 years as a Coroner I have found that members of the Garda Siochana have shown themselves at their professional best in such circumstances. The gardai use tact and discretion in dealing with such matters and in many cases they have asked me to post pone Inquests in suicide cases where they have brought to my attention that members of the family are not able to cope with an Inquest at a particular time. If the family contact me I will also facilitate them. 13. The social stigma of suicide has diminished but still exists. This is not necessarily an unhealthy thing for Society. Society must retain some of its taboos to survive. Suicide is a taboo subject in western cultures especially within the Christian way of life and this is still quite real. There was a time when the Church would refuse to allow persons whose deaths resulted from suicide to be buried in consecrated grounds. That unilateral policy by Catholic clergy in particular caused untold grief to the bereaved. 14. All of those who deal with Suicide including the Coroner should fully and fearlessly enquire in to the cause of death to establish the truth. If the truth is that it was a death by suicide then this should be reflected in bringing in a suicide verdict. I suggest that the bereaved cannot begin to grieve properly until they face the truth and it is only then that they begin a process of acceptance and healing. 15. Whilst dealing with suicide is emotionally difficult for the family, it is also difficult for the Gardai who have to deal with it as well as the Coroner and others who have to interact with the bereaved. 16. I believe that there is a social value of an Inquest. Some family members go into denial and these cases are sometimes the most difficult for a Coroner to deal with. A person in denial may tend to latch on to every rumour or suspicion that flies around the District pending the completion of an Inquest in to the death. Human nature being what it is, sometimes the family members may be the object of malicious gossip which generally is unfounded. 17. The Inquest which is held in public provides society with a forum to raise questions concerning the death. 18. At an Inquest there is a right of an aggrieved relative to voice a complaint publicly which I believe is valuable. It might be described as a safety valve because some grievances once expressed publicly do not survive examination in an open forum like an Inquest when faced with the facts. 19. It is important to realise that an Inquest is unlike a civil or criminal trial. People will have seen and heard reports of court cases but they have no idea of what happens at an Inquest. It is a policy of mine to outline to people at the commencement of the Inquest why they are there, inform them of what is going to happen and what the Inquest will hope to achieve. It can be a great comfort for people to be present at deaths but in the case of suicides in particular, there is no opportunity to say goodbye and in many instances family members may be totally unaware that a loved one is so troubled as to take their own life. Many relatives come to an Inquest with expectations at finding answers which regretfully they will not because of the limited powers of an Inquest in death investigation. 20. An Inquest is a fact finding exercise and it is not a method of apportioning guilt. The procedure and rules of evidence as applied in Civil or Criminal Courts are unsuitable at an Inquest. In an Inquest it should never be forgotten that there are no parties, there is no indictment, there is no prosecution, no Defence and there is nobody on trial. It is simply an attempt to establish the facts and the truth about a death of a loved one. 21. Suicide inquests are held without a Jury. It is my policy to leave self-inflicted deaths to the end of the List of Inquests and to try and deal with them in a sensitive way. I usually hold such Inquests around a table where everybody sits at the same level as opposed to the more formal Court setting. I have to say that I did not always deal with Inquests in this way but as a Coroner now for almost 30 years I have to acknowledge that I have changed in the way that I deal with Inquests, particularly when I see, in many cases, the agony in front of me. It is impossible not to be affected by the grief that one sees. The following people are present at an Inquest:- the Superintendent of the Garda Siochana who presents the evidence, the Gardai who conducted the Investigation, members of the family or non-family members who have made Statements and the Pathologist. 22. Each person giving evidence is sworn. The Statements are read out to an Inquest by the Superintendent. Each Witness is then asked to confirm the contents of the Statement as being true and accurate and they are invited to sign the Statement. This Statement becomes their Deposition to the Inquest. There will be a Witness, possibly a family member who gives evidence of identification. The final witness is the Pathologist who gives evidence of the cause of death. If there is alcohol involved, he is in a position to confirm what the alcohol level is. I should say to you in general terms that in many cases of suicide there is a high level of alcohol in the blood when analysed post-mortem. Anybody with an alcohol reading of over 80mgs% is over the legal alcohol driving limit in Ireland. It is not unusual to have results of between 300mgs % and 450mgs% in Post Mortems. Many people who take their own lives consume large volumes of alcohol prior to doing so. 23. When all the evidence is completed I then have a discussion with the next-of-kin as to what type of verdicts they believe I should record. I have found it valuable to the next-of-kin to be involved in this process. I outline to them what I see from the facts as contained in the Statements which have just been read to the Inquest which lead me to form a certain view that this may well be a suicide death. I invite them to tell me why I should not hold this view and I give them an opportunity of trying to defend the deceased. This exchange of views takes place for a little while and very often the family themselves will come round to accept that what actually happened to the deceased was in fact suicide. I believe that this exchange with the next-of-kin is helpful to the family to acknowledge in effect the type of death of the deceased. 24. I should say that the degree of proof required to reach a suicide verdict is the criminal degree of proof, that is beyond all reasonable doubt. It is not the civil degree of proof which is on the balance of probabilities. If, for instance, there is a suicide note or previous threats from the deceased or in the case of drowning if the deceased had removed their clothes before entering the water, folding them neatly, this could be regarded as evidence of an intention to commit suicide. Psychiatrists take the view that behaving in this fashion is indicative of an intention to take one’s life. On the other hand if somebody is found drowned and there is no contemporaneous evidence that there was an intention to take a life then in fairness to the deceased, I would record an open verdict because I would not have sufficient evidence to establish a verdict one way or the other. An open verdict is generally recorded where there is not a chain of evidence up to the time that a body has been found. Dr. John Connolly, Consultant Psychiatrist when employed by the Western Health Board undertook a review of all of the Coroners files in County Mayo to see whether or not there were cases which might not on paper be seen to be on the face of it suicide but on further examination would be sufficient to allow the medical people to reach a conclusion that the death was by suicide. For example there have been a number of road traffic accident cases in my area when the question of a suicide clearly has been on my mind but there is insufficient evidence to reach that conclusion. In one case that comes to mind, a man had a row with his wife. He left the house telling her he intended to kill himself. He drove his car and met an oncoming truck and for no apparent reason the car simply swerved in to the path of the truck and as a result he died. When the driver of the truck went to the car immediately after the impact he found that the deceased had pulled his t-shirt over his head before he swerved in to the path of the truck. Some people might conclude that this was an intention to commit suicide but from using the yardstick of beyond all reasonable doubt, I could not and did not reach a verdict of suicide in that particular case. 25. After engaging with a deceased’s family in coming to a conclusion as to what the appropriate Verdict is, bearing in mind that I would err on the side of caution for the sake of the family, I then suggest to the family that I believe that they should not assume a cloak of guilt for what has occurred. Many people say that if they had known that the deceased was unwell or unhappy they might have kept a better eye on them or gone to visit them more often or be more attentive to the deceased during their lifetime. This I believe is unfair to the relatives themselves and I do not believe that they are responsible for the life of another adult. I know many people who are watching a relative all the time. They are on edge knowing that a person has threatened to take their own life or that there is a suspicion or anxiety that such an incident could take place. This can and does cause great stress to a family who are living with a potential nightmare that may become a reality at any time and over which they have no control. 26. If somebody is determined enough to take their life then they will do it at a time when nobody is around. 27. Having spoken to bereaved families they feel that an Inquest brings closure after the death of a loved one. They can get a Death Certificate and deal with the affairs of the deceased and try and move on. 28. The title of this paper is “Good Practice at the Coroner’s Court”. 29. Coroners as a group are effectively independent republics. There are no set guidelines laid down as to how to conduct an Inquest. It may well be suggested that some Coroners are cold or clinical but I would have to say that the more I do this work the more I see the need for a caring role for the sake of the family to help them come through it. I speak to family members on the telephone on a regular basis. Sometimes they are afraid of certain matters about the deceased coming out in public. If there are notes left then these are read by me and handed to the investigating guard. A note of intention to take one’s life generally contains matters of a personal nature for the family or seeking forgiveness for what they are about to do or in some cases giving reasons why they are doing it and blaming somebody. In a recent case I had there was a very detailed letter written by a man clearly in great distress where he blamed his father for having mistreated him all of his life to such an extent that he felt like a leper within the family. He was not allowed to live in the family home. He was made live in a mobile home. I made the deceased’s brothers and sisters aware of this fact in advance of the Inquest and left it to their own discretion whether or not they would inform their father who was in his 80’s. The father was the one who was being blamed and there was a general acceptance by the family members that what was contained in the note was true and accurate. Some families wish to obtain possession of such a note. Generally I request the Gardai to supply me with a copy only. The attitude of the Garda Siochana is that they retain the original note as they believe they should. There have been occasions where people have suggested that a suicide was not in fact a suicide but rather a murder and there is always the possibility that the Gardai might find further evidence at some state to re-open a case, hence the reason for retaining the original note. Certain difficulties have also arisen recently in relation to getting copies of notes particularly where spouses may have been estranged and suddenly the estranged spouse comes back and wants to reclaim the deceased. This can and does cause difficulties. In one situation a man was asked by his wife to leave home. She wanted a separation from him. He left, went out to a tree in the garden and hanged himself. He left a note and his wife who had an exceptional sense of guilt for what occurred wanted the note. The Gardai did not make this available to her. She was however supplied with a copy of the note. 30. Unfortunately modern technology has now delivered a new way of sending a chilling message and that is either by text message or by voicemail. This is becoming a common way of advising family or friends of an intention to take one’s life. 31. The public nature of an Inquest also serves the public well by highlighting the increase in suicides or self-destruction cases in recent years. A substantial minority of deaths reported to Coroners may be ascribed to social breakdown in one form or another. Inquests and the accurate certification of a cause of death are an important social function which show social trends such as an increase in suicides which challenges the State and State bodies to investigate the underlying causes and to establish a social programme designed to reduce its incidence. There was a family where 3 sons have committed suicide. Such families feel very isolated even within their own community. Many people shun them because they seem to be “different”. They approached a local GP for help. To date the HSE have not given any assistance. The question I ask in these situations is can or should society intervene or offer support to these people or are we too busy in our own lives to think of our neighbour ? 32. The question of why people kill themselves is a matter for Society to deal with. I believe that we may have become too affluent, too busy and have less time for human contact resulting in vulnerable people feeling isolated. 33. As to the media and publication of Inquests, I have spoken from time to time to the Reporters who cover my Inquests. I have asked them what their views are. There are some of these who take the view that having them reported is an intrusion in to people’s lives. Listening to the death notices in the local radio station, the word “tragically” is commonly used. Anybody listening to this clearly knows that somebody has taken their life so the cause of death becomes generally known to the listener. One of the arguments used for not reporting suicides is the risk of copy-cat deaths occurring. Having examined the suicides that I have dealt with over past years, no where can it be suggested that there has been any copycat death. There are those who suggest that people who are considering taking their lives take courage when they hear that somebody has successfully done so. The data of suicides I have does not support this argument. 34. The other commonly held belief is that suicide is generally of young people. In the total number of suicide cases I have had over the past 2 years only in 2 cases out of 29 was a person below the age of 30. Of the 29 persons 7 were female and 22 male. The average age of the 29 persons was 47 years with the youngest 25 and the oldest 73 years. Certainly there is a common feature of the single male, generally living alone, sad, with no one to talk to, feeling isolated from friends and relatives and feeling that life has neglected them. Of more recent times I have had a number of suicides of married women in their 50’s. 35. I would ask this question as to whether or not we are grown up enough in society to deal with unpalatable matters in our lives. We have had full disclosure of sex abuse cases, paedophilia and other high profile matters which the public appear to have been able to take in their stride so why not the reporting of suicides in a plain factual non-judgemental manner ? 36. Having read the final Report of the National Task Force in January, 1998 on suicides there was a recommendation that the Media in general and journalists in particular would establish a code of good practice applicable to reporting matters relating to suicide and that the headline writers, editors, sub-editors and newspaper photographers follow the same stringent code as journalists writing particular articles. 37. It suggested that “the reporting of individual suicides be limited to particular cases where it is thought to be in the public interests to do so, so a Coroner may decide to address the press in this regard but the report should not include specific details as to the mode of death and nothing should be written or said that might encourage others to end their lives.” 38. I do not, as a Coroner, comment on any death before me. I am conscious that the family are already grieving enough and it is not for me to judge a person who has died or the circumstances in which they have died, whether it is a suicide or some other violent or unnatural death. I do not believe it is a task of a Coroner to add to the grief of the family by commenting. 39. I believe that following an Inquest that adequate support services should be available to those who wish to avail of them, be there but not be intrusive. Many people who have gone to support groups or have listened to other persons who have been through the same experience find comfort and support in dealing with their loss of a loved one. It has been my experience that nothing can prepare a family for the loss of a loved one in such a manner, no matter whether expected or not. John T. O’Dwyer, Coroner, Mayo South, Ballyhaunis, County Mayo . Chairperson: Joan Freeman – Comments This session involved two speakers who witnessed the impact and trauma of suicide form two different perspectives. Firstly we heard from Nuala Whelan a mother of eight children who was devastated by the suicide of her husband, John. What was most obvious listening to Nuala was her innate wisdom and her selfless concern for her children. She handled that awful question “why” by barring it from the house for six months. This gave her children and herself the space to allow the acceptance of the loss to sink in. Nuala also supplied us with a strategy of coping with and managing those first milestones. The first anniversary was spent as a family going to Butlin’s. This was a true celebration of life and by spending a fun day on their father’s anniversary also included him on the family outing. The second perspective of suicide was a talk given by John O’Dwyer. He spoke about how an inquest is a “fact finding exercise” which of course makes it cold clinical and very public. John O’Dwyer recognised the level of upset and distress experienced by people who are bereaved by suicide and how he created a system that involved the family in a more private and compassionate setting. Both of these speakers, through personal wisdom and experience provided us with personal strategies and structures that could be implemented on a professional level without losing any compassion for the people involved ‘WELCOME TO MY WORLD’ CAROLINE MCGUIGAN Founder, Suicide or Survive Abstract Caroline invites the audience into her world. A world which moves in and out of the complexity of being “human”, of being “real” and the struggle and hardship this can have on an individual. So much so, she herself attempted suicide. She shares what brought her to this point and how after her attempted suicide, she worked on rebuilding her life. She shares what her world is like today and how she now lives on a daily basis being “human” and “real”. Caroline also shares with the audience the “Eden Programme”. How the project was identified, its aims and activities and when it will commence. Caroline shares her overall experience of suffering with panic attacks, being a user of the psychiatric services, attempting suicide, training to be a therapist and being the founder of Suicide or Survive. Talk, talk, talk, that’s what I remember. Constant talking, constant chattering. Non stop, day in, day out. Wakening in the morning thinking, thinking, thinking. So tired, so weary. Who will I meet today? What will I say? How will I get the hell away from them? Oh God what excuses can I come up with today. I fell the pain coming on, I fell the lump in my throat, the tears in my eyes and the pit in my stomach. Take a pill, that will help for an hour or two. Take two pills, sure that will give me the morning. Take them all – NO NEVER – or maybe – NO- maybe – NO – June the 13th 1995. Hello, I would like to introduce myself, my name is Caroline McGuigan. I am married and have two great children. On a daily basis I question my abilities as a parent, I worry about how I am bringing my children up and yet, this is the only way I know. In my life today I am comfortable to share the many parts of myself. The kindness, the genuineness, the passion, the experiences, the expertise, the humour but also the hardness, the anger, the dismissive parts of myself. At a time in my life I was ashamed, embarrassed and uncomfortable to be “me”, as I feared what other people may think of me. My greatest fear was “if they really knew me”. So I became Caroline, who truly worked hard at being liked, entertaining others, believing that “these people knew what they were talking about” and I started to become a shell. Why did I feel this way? Why did I believe this? LIFE. My life experiences had allowed “my story” to unfold. I now realise every individual’s life is complex and it will be a combination of life experiences, the impact they may have on the individual and their copying mechanisms which will have a huge part to play in how life effects them. How and what brought me to be here today, sharing my experience of attempted suicide. Determination, passion, anger, frustration, a drive that I wonder where it came from, people I have met along the way and situations I have experience and at times something that is more than all of this – what that is I am not sure, but I know I sense it. I was diagnosed with an anxiety disorder or “panic attacks”. What was actually happening was I felt I was going crazy? I believed something awful was going to happen in front of everyone and I would have not control. I started to avoid people and places and loss my belief in myself, my self-esteem was slowly falling and my anxiety was quickly rising. At the time I did not know what panic attacks were and thought this was something happening outside of me. I was introduced to medication, again I did not know anything about medication, the effect it would have on me and the road of addiction that lay ahead. The supports that were offered to me were psychiatric. I resisted at first because I believed that only “crazy” people went there. By the time I got there “I” believed I was crazy. I was on 16 tablets a day, full of anxiety and terrified. So now I carried the “stigma” of being in a psychiatric ward so my self-esteem was rock bottom. I did not know what was happening to me. I knew if I took tablets I could function, so I did – 16 a day, every day. I met a lot of wonderful, kind and scared people, this describes both the staff and the clients (I use the word client, in the services you are a patient). I still believed that “panic attacks” were something going on outside of me so I was waiting to be fixed. In the hospital we had a community room which we sat in for most of the day. My smoking trebled. There was a number of very helpful people who truly cared but time was not on their side. There was also a number of very controlling, unfriendly people who believed they were the expert and knew what was best for me. I now realise it was not about me, it was their own insecurities they were fighting with. I started to become a part of this world, which kept me safe from outside and gave me my medication. I also became dependent on this world. I fitted in, I did not feel excluded, different or “crazy”. But outside of the hospital, the staff, the clients, I could barely function. Outside of this world I lied, I avoided people and situations. My world was becoming smaller and smaller. Over time I lost my job, friendships, my self-worth. I remember once a person saying to a friend of mine, “do you feel safe letting Caroline mind your baby, after all she has those Panic Attacks”. I cried and cried and cried. I started to realise people genuinely did not understand when someone was mentally unwell and for a lot of people it frightened the living day lights out of them. But this made it worse for me. So my journey continued – panic attacks, medication, psychiatric services, avoidance, not belonging. Over time I started to see the world I was in (psychiatric) and did not want it yet did not know how to get out of it. At the time I was able to get to the hospital and back, go certain places if I had someone with me. If I drank I could stay out longer but a couple of times I mixed the booze with the drugs, which was a disaster. But I started to become dependant on booze. I was crumbling. WHY, because I was starting to loose hope. The services I was attached to had nothing else to offer, I did not know where to turn. I did know I didn’t fit in anymore. I know I felt great sadness, extreme pain and aloneness. Even though I had people supporting me I felt so alone. Through everything I looked the same on the outside but inside my heart was breaking. At no time was I offered counselling or invited to explore the idea of counselling. The thoughts started. At first I was shocked and quickly started to think about something else. But the thoughts came back. I was exhausted, I felt permanently guilty of the “burden” I had become to others. All I wanted was a minute, an hour, a day where my head would switch off, where I got a break, where my day did not start with…… “God here we go again. Get through this day without having a panic attack, within feeling scared all day long, without making excuses, without lying, without depending on others”. The thoughts, the thoughts…… Take a pill, take two, take them all. Quietness, just a little bit of quietness. The night I attempted suicide I had had a great time. I had enjoyed a bbq with friends and had smiled. I had had drink, which made it easier. So why that night? I just did not want to wake up to those thoughts again. I was so so tired, so weary and just did not know what to do – I felt a failure. After that it become a haze – hospital/blackness/bringing me back/not breathing/gone/back I remember when I woke up and I was surrounded by elderly people who were unwell. A nurse came up to my bed, not much older than I was and said “that was a really silly thing to do, look around you at all these people fighting for life and there is you trying to end yours. I lied in the bed curled up like a foetus. I looked at the locker, all my medication had been left there. I cried and cried and cried. People came, people went. The shock on their face the uncomfortableness of what I had done and the avoidance of talking about my attempted suicide. I was thinking, “I couldn’t even get that right” Over the days that followed the impact of what I had done started to hit me. My world was still a mess but I felt different. I had survived a suicide attempt and was alive. I started to think, “well why am alive, do I want to be alive, yes I do but how the hell do I rebuild my life”? So without me knowing the part of me that was a survivor, that strove to live and change, was coming alive. At the time I was given an option of being signed in, which I refused or going back to the hospital I attended as a day patient 5 days a week. Also, lucky for me, a Therapist was made available for me to work with. I spent 3 days a week for the next year to year and a half talking. Talking, talking talking. It was hard, it was painful. I thought this is a load of crap, all this is doing is going around in circles but I kept going. I cried, I laughed, I became angry, I STARTED TO UNDERSTAND. My anxiety was still in full swing. I joined a support group to help me with the day to day practical issues of living with an anxiety disorder. All of this was so so hard and I wanted to on numerous of occasion’s walk away. Why didn’t I – I was started to change. I was started to feel there was hope, small as it was, it was there. I was still pumping the medication into me but decided with the support of the hospital over a long period of time to come off it but only because I now had access to therapy and a support group to help me with my panic attacks. My recovery is a whole story in itself. It had its good times and it had its bad times. The biggest question and the scariest question throughout was WHO AM I. You see in my “madness” I had a sense of security, I knew I was all over the place and I had somewhere to go. Now I had to figure out who I was, what had brought me to the different experiences in my life and the big one I had to take responsibility for my own recovery and my own quality of life. So what and who was I. What I started to notice was how I was treated in the services and how others were treated. I started to listen to myself and to others. I started to hear what people were craving for – warmth, understanding, kindness and empathy, not sympathy. The services provided some of this but in general they did not have the time and also did not believe a person, given the right environment, could explore what their needs were. It was very much “we know what is best for you”. Through my recovery I realised that to share my experience and for people to listen, I would need to become a “professional” myself. So I started the journey of becoming a therapist. This took me six years. Throughout these years I continued to work on my own development and started to see/understand why and how my medication and treatment had been decided. I wasn’t always happy when I realised some of the reasons for my treatment/medication. But the big thing that stuck out for me was that throughout my journey, it wasn’t the theory/treatment it was some of the people whom I met that made a difference. Qualified and insightful people, who could see that I was more than a label from the DSM book and allowed me to participate in my own recovery. What these people had in common was that I experienced warmth, genuineness, honesty and compassion from them and towards me. So SOS started to form in my head. What would it be like to offer an individual a group where they would experience warmth, genuineness, respect and structure. What would it be like if people were educated on depression, anxiety, the psychiatric services, medication etc. What would it be like if people were given the opportunity to work on their life skills, What would it be like if people were allowed to explore and reflect on the impact life was having on them, particularly when their thoughts were moving towards suicide. What would it be like if all of this was offered to an individual in a group setting? Not for 15 minutes a week, not for a couple of weeks but for a period of time that would allow them to pause and reflect and see if they were ready to start to take responsibility in their own recovery. I spoke to a lot of friends and colleagues. Everyone believing this environment was essential for an individuals development, some wanting to be involved. So Suicide or Survive was established. Suicide or Survive will be running its first programme, the “Eden Programme” within the next couple of months. We as an organisation fund raise on an ongoing basis. We learn through our individual experiences and as a group. We are open and transparent. We do not believe our way is the one and only way but we do believe that it is an option for a person. A tremendous amount of work goes on behind the scenes all being carried out by very passionate, strong and determined people. What have I learned. You need to be ballsey, persistent, determined, passionate and have a tough skin. Why? Because our Country is only starting to recognise that the revolving psychiatric door is not always the way for everyone but is still cautious/fearful of the other options available. Fear was what brought me down. Now I realise if I stop, listen, be compassionate to myself and others, I can respond rather than always reacting. I remember once saying to a very wise lady “I met some really special people along the way who truly made a difference”. She replied “I am sure you did but Caroline we are all special”. I have learned I am made up of many parts and my biggest gift to myself is to try somehow to allow compassion into my life so I don’t continuously judge myself. If I can do this for myself I can then do this for others. I would like to read a piece by a very beautiful young woman who is 17 years of age and is called Hannah Tatschl. PIECE I would like to offer a gift to everyone here today. It’s a piece that stays with me every day. PIECE Thank you for listening to my story. E-mail: carolinemcguigan@eircom.net Chairperson: Josephine Quinlan - Comments Caroline McGuigan, a qualified therapist and tutor shared her personal story of struggling with mental ill health and went on to describe her subsequent suicide attempt. Caroline’s story began when she experienced difficulties coping with everyday life, followed by being diagnosed with an anxiety disorder, entering a psychiatric hospital, returning to her original life, attempting suicide, and again picking up the pieces of her life following her attempted suicide and finally the crossroads! If you feel exhausted just reading the previous sentence, imagine what it is like for thousands of Irish people who go through similar experiences on a daily basis. Why? Caroline stated that our country is only starting to recognise that the revolving psychiatric door is not always the best way for everyone, and that Ireland is still fearful and cautious of the other options available. What stood out in Caroline’s story? The loneliness that accompanied her inner struggle and her need to pretend that everything was ‘okay’, no doubt in an effort to avoid the shame and stigma that our society continues to associate with mental ill health. Thankfully, at the crossroads of her life, following her suicide attempt Caroline chose to travel down the road of personal care and self development, eventually becoming a qualified therapist. Caroline’s personal experience and professional training gave her the determination and insight to create options for people that are struggling with an anxiety disorder or those that have attempted suicide and are trying desperately to rebuild their lives. Caroline founded an organisation called Suicide or Survive that will launch its first major project called the ‘Eden Programme’ over the coming months. The Eden Programme, is one of a number of new innovative programmes initiated by such creative and courageous thinkers as Caroline McGuigan. Finally, delegates were invited to discuss issues surrounding bereavement before the seminar concluded. Not surprisingly, the discussion swayed through many topics such as mental ill health, the predominance of the psychiatric system in mental health care and the scarcity of suicide bereavement services. The two themes that emerged were firstly that it takes hard work, commitment and determination to launch new projects or services in the present Irish health system. Secondly, everyone both personally and professionally must play a vital role in an effort to reduce the stigma and shame associated with mental ill health. Stigma and shame are barriers that we as a society have created preventing us from seriously tackling the issues surrounding mental ill health. THE SPEAKERS ANNETTE BEAUTRAIS Associate Professor Annette Beautrais is Principal Investigator with the Canterbury Suicide Project at the Christchurch School of Medicine & Health Sciences in New Zealand. She has conducted research and published on various aspects of suicidal behaviour since 1991. She is a current executive member of the International Association for Suicide Prevention and Co-Editor-In-Chief of CRISIS, the journal of the International Association for Suicide Prevention. VERONICA O’KEANE Veronica is Head of Section of Perinatal Psychiatry at the Institute of Psychiatry, London and honorary consultant at the Mother and Baby Unit, Bethlem Royal Hospital: where she is lead clinician in a specialist national-referral centre for perinatal psychiatry. She has also worked as a consultant in General Hospital Psychiatry in Cambridge and Dublin and established the psychiatric service in Beaumont Hospital from 1998-2002. Her research interests are hormonal abnormalities in psychiatric disorders and the effects of stress hormones on behaviour and brain function. Her current research programme examines the mechanisms and the effects of depression during pregnancy on women, pregnancy and their babies. She lives in Howth with her two children. ANNIE DILLON Annie works with the National Women’s Council of Ireland (NWCI) as Policy Outreach Facilitator. She has an MA in Women’s Studies and MSc in Education & Training Management and is a qualified Psychiatric & General Nurse and Midwife Annie has worked in the area of women’s health in Australia, England and Ireland. ANGELA MOHAN Angela is Consultant Psychiatrist in Rehabilitation at St. Vincent’s Hospital Dublin. Former Clinical Director St. Brendan’s Hospital Dublin. Practioner in Cognitive Analytic Therapy and currently in advanced Psychotherapy training. MICHAEL FITZGERALD Michael qualified in medicine in University College Galway in 1979. He did his training in Psychiatry in the Maudsley Hospital and in Kings College Hospital London. He obtained an M.D. from Trinity College Dublin in 1996. He is a consultant psychiatrist for the National Children’s Hospital Dublin, Our Lady’s hospital for Sick children Dublin and the Southern Area Health Board. In 1996 he became Henry Marsh Professor of Child Psychiatry at Trinity College Dublin. Michael is a Fellow of the Royal College of Psychiatrists and plays an active part on the specialist sections of that organisation. He has a special interest in Autism and Asperger’s syndrome and is research consultant for the Irish Association for Autism. He is the first and only Psychoanalyst practicing in the Republic of Ireland recognised by the international Psychoanalytic Association. He is an accomplished teacher in all aspects of his chosen speciality. Michael has set up numerous training courses in psychoanalysis and psychotherapy. He has founded two journals and has published over 300 scientific articles and letters and edited a number of books. He is on the editorial board of several international journals. Michael became chairman of the Irish Association of Suicidology in 2002. PAT LITTLE Pat was appointed Scottish Development Manager for Penumbra’s young people’s services in 1999. He previously developed and managed Penumbra’s young people’s community mental health project in the Scottish Borders. He has over 25 years experience working with young people most of which was specifically with 16-25 year olds. He now has responsibility for networking with young people’s agencies in Scotland to form strategic alliances in order to raise awareness of young people’s mental health issues. He also has responsibility for promoting research and developing training on these issues as well as identifying gaps in current provision of services across the country. This involves contact with the Scottish Executive, Local Authorities, Health Boards and the Voluntary Sector across Scotland. Pat has contributed to several National and International conferences and provides training and consultancy on young people’s mental health issues (particularly on self harm) both in Scotland and abroad. He was responsible for the development of Penumbra’s six dedicated Self Harm projects and currently chairs the Scottish Self Harm Forum. He was a member of the Scottish Executive’s Planning Group on the National Framework for the Prevention of Suicide and Self-Harm (Choose Life) and the planning group which produced Scottish Needs Assessment Programme (SNAP) Report on Child and Adolescent Mental Health in Scotland. CAOIMHE GLEESON Caoimhe is Equality Officer with the Health Service Executive (H.S.E.). The H.S.E. is the biggest public sector employer and service provider in the Republic of Ireland employing over 100,000 employees from diverse backgrounds. Since 2001 she has established an equality and diversity programme within the North West and is currently working through the reform process to ensure this work can be replicated across all regions within the HSE. This work includes policy development, equality information dissemination and training, and the development of new and innovative practices and supports in employment and health service delivery to diverse groups. She formerly worked with NUI, Galway in partnership with a wide variety of agencies and organisations in the North West region of the Republic of Ireland and in Northern Ireland. She has a particular interest in equality, human rights and gender issues and continues to work in a voluntary capacity with a number of organisations. She has also worked on projects relating to gender equality, youth work, intercultural education, development of civil society and citizenship rights in El Salvador, Ghana, United States, Croatia and Bosnia-Herzegovina. HELEN MACWHITE Helen Mac white is the Communications Officer with Bodywhys – The Eating Disorders Association of Ireland. Much of Helen’s work focuses on awareness raising and increasing understanding of the experience of people affected by eating disorders. This includes looking at the language that is used to communicate distress and to respond to distress as well as gaining an understanding of how to promote supportive healing relationships. Before working in the area of mental health, Helen was a lecturer in the School of Applied Language and Intercultural Studies in Dublin City University. She has also undertaken studies in Counselling and Psychotherapy and hopes to complete a BSc in Psychotherapy in the near future. NUALA WHELAN Nuala a mother-of-eight devastated by the suicide of her husband is now a beacon of hope for those bereaved through suicide. Nuala's life was changed forever when her normally happy husband John left the house one morning never to return. Nuala was left to bring up eight children on a small pension and little money from part time work. When her husband died, the family had only £4.50 in the bank. But Nuala did a remarkable job rearing her family. Daughter Ann-Marie is now a qualified Barrister; Brendan has just graduated as an Architect and Siobhan as a Nurse; Derek is working in London's Carary Wharf after getting a first- class Honours Degree in Computer Science from UCD where he was top of his class two years running and Emma has a Diploma in Interior Design. Nuala's is a compelling story that offers hope and inspiration to those bereaved through Suicide. JOHN O’DWYER John O’ Dwyer is Coroner for Mayo South based in Ballyhaunis, County Mayo. John is a Coroner for over 30 years and has a wide experience in dealing with Inquests which may be suicides. Because of the exceptional level of upset experienced by family and friends he has evolved a system of involving family and next-of-kin in the Inquest process particularly in attempting to reach what is a fair Verdict to the deceased. CAROLINE MCGUIGAN Caroline Mc Guigan is a qualified Therapist/Tutor. Her work involves one-to-one therapy and group work. She presently works as a Tutor for Maynooth College delivering the “Foundation in Counselling Skills Course”, a one-year course that covers Theory, Skills and Self-Awareness. Caroline is the Founder and Co-ordinator of Suicide or Survive, a registered Charity. Suicide or Survive aims to support people who have attempted suicide or have suicide ideation, through a group setting over a 6-month period. The group will allow a person to explore their own experiences, develop their skills and source avenues of support and assistance. Caroline is also the Irish Co- ordinator for a Charity called “No Panic”, which has been in existence for 15 years in England and is in Ireland the past 2 years. No Panic aims to aid the relief and rehabilitation of people who suffer with anxiety disorders through a Helpline, Telephone Recovery Groups, Literature and Written Recovery Programmes. Caroline personally believes that a person needs to experience an environment that is genuine, understanding and non-judgemental before they consider trusting and working with another individual. For Caroline to be in a place to provide this environment to another person she used her own personal experiences, went the long road of training and took her “dreams” and made them a “reality”. PAPER PRESENTERS DEREK CHAMBERS Derek is a Research and Resource Officer of the National Office for Suicide Prevention (NOSP) and recently acted as Project Manager for the development of the National Strategy for Action on Suicide Prevention which was published September last under the title ‘Reach Out’. He has an MA in Sociology from UCC and is interested in social change models of suicide and in general population approaches to suicide prevention. IAIN MCGOWAN Iain McGowan is a mental health nurse employed as a lecturer at the University of Ulster. He has authored numerous articles and conference presentations and compiled one book on the philosophical aspects of suicide. He is currently studying for his PhD at the University of Ulster investigating the non-linear dynamics and applying the principles of chaos theory to suicide. Mr McGowan is editor of Mental Health Nursing On-Line. MARTINA O’RIORDAN Martina is a Research Officer with the National Suicide Research Foundation. She has previously undertaken research roles in the Department of Applied Psychology, University College Cork in studies commissioned by the Health Services Executive and the Mental Health Commission. She also worked as a Researcher on the COPINE (Combating Paedophile Information Networks in Europe) Project at UCC. She has a BA in Applied Psychology from University College Cork and a MSc in Forensic Psychology from Glasgow Caledonian University. CARMEL MCAULIFFE Carmel began working as a research psychologist with the National Suicide Research Foundation in 1996, following graduation with a B.A. and Higher Diploma in Applied Psychology at University College Cork. During her appointment she worked on the Repetition-Prediction part of the WHO/EURO Multicentre Study on Suicidal Behaviour. She also completed an MPhil examining suicidal ideation in university students, and an MA in Behavioural and Cognitive Psychotherapy, at University College Cork. She currently works for the HSE Southern Area co-ordinating a randomised controlled trial of group problem-solving skills training for deliberate self-harm patients. She recently submitted her PhD thesis investigating problem-solving characteristics of deliberate selfharm patients. CHAIRPERSONS MICHAEL FITZGERALD Michael qualified in medicine in University College Galway in 1979. He did his training in Psychiatry in the Maudsley Hospital and in Kings College Hospital London. He obtained an M.D. from Trinity College Dublin in 1996. He is a consultant psychiatrist for the National Children’s Hospital Dublin, Our Lady’s hospital for Sick children Dublin and the Southern Area Health Board. In 1996 he became Henry Marsh Professor of Child Psychiatry at Trinity College Dublin. Michael is a Fellow of the Royal College of Psychiatrists and plays an active part on the specialist sections of that organisation. He has a special interest in Autism and Asperger’s syndrome and is research consultant for the Irish Association for Autism. He is the first and only Psychoanalyst practicing in the Republic of Ire land recognised by the international Psychoanalytic Association. He is an accomplished teacher in all aspects of his chosen speciality. Michael has set up numerous training courses in psychoanalysis and psychotherapy. He has founded two journals and has published over 300 scientific articles and letters and edited a number of books. He is on the editorial board of several international journals. Michael became chairman of the Irish Association of Suicidology in 2002. ANNE CLEARY Anne is a sociologist and lecturer in the Department of Sociology, University College Dublin. Her research interests include health and illness – particularly the gender patterning of health and illness, childhood and adolescence. She is the author of several books and reports on these topics most recently ‘From Child to Adult: A longitudinal study of Irish children (2004) and ‘Young Men on the Margins’ (2004). Her current research project (funded by the Irish Research Council for the Humanities and the Social Sciences) involves a qualitative study of suicidal behaviour amongst young Irish men. BRIAN HOWARD Brian is Chief Executive Officer of Mental Health Ireland. Mental Health Ireland is the largest voluntary body representing the interests of people with a mental illness in Ireland and is actively engaged in the promotion of positive mental health. He was elected to the Board of Mental Health Europe in 2001 and to the Board of the World Federation for Mental Health in 2003. Prior to joining Mental Health Ireland, Brian worked with the Department of Health and Children and was assigned to the Mental Health Services Division of that Department. His main responsibilities were preparing, drafting and finalising the content of the Mental Health Act 2001 and the development of psychiatric services in accordance with Government policy. He chaired the National Task Force on Suicide which published its Report in 1998 and is currently a member of the National Advisory Group on Suicide Prevention. SEÁN MCCARTHY Seán is the Regional Suicide Resource Officer for the south eastern region of the Health Services Executive – South. He has worked in the area of suicidology since 1999. He is a member of the Irish Association of Suicidology and of the International Association for Suicide Prevention. Seán is a founder member of “Talk it Over’’, a suicide bereavement support group based in County Waterford and south Kilkenny. He was a member of the steering group for the development of Reach Out, National Strategy for Action on Suicide Prevention 2005-2014 and was also a member of the advisory subgroup on suicide prevention for a Vision for Change, the Report of the Expert Group on Mental Health Policy. Sean’s particular interests lie in the development of bereavement support services and in the development of services to respond and support persons who self-harm. Prior to taking up his current position, Seán worked with the Waterford Mental Health Services as a Clinical Nurse manager. He has also previously worked in Forensic Psychiatry Special Assessment and Supervisory Services in Maidstone, Kent. SHEILA DALTON Kilkenny born Sheila has been a volunteer and support group facilitator with Aware for 16 years. She is also a member of Kilkenny Bereavement Support Group and is involved with their on-going training. She has a special interest in and works with people who have been bereaved by suicide. A qualified Psychiatric Nurse, she worked with CarlowKilkenny Mental Health Services in many capacities for 36 years until her retirement in 2003, she is also a director of Kilkenny Health Association. JOAN FREEMAN Joan had a private counselling practice for 16 years. In January of this year, she opened the first centre for the Prevention of Self-harm or Suicide. Pieta House is based in Lucan where Joan and her team of qualified psychotherapists provide a groundbreaking service to people who have suicidal ideation, people who have attempted suicide and a service for people who self-harm. It is hoped that this service will be nationwide over the next two years. Joan is at present creating a workshop for people who have family members in crisis and workshops for professionals who deal with people who self-harm. JOSEPHINE QUINLAN Josephine is Service Manager of Console in Limerick; an organisation that works with people Bereaved through Suicide. She is a member of Irish Association for Counselling and Psychotherapy (MIACP) and the Irish Association of Alcohol and Addiction Counsellors (MIAAAC). Prior to this, she worked as a Registered Nurse (R.N) in Ireland and Australia.