Having a Gastroscopy
advertisement

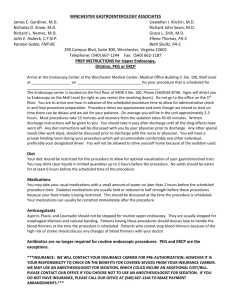
Upper Gastrointestinal (GI) Endoscopy What is an upper GI endoscopy? This procedure allows the endoscopist to look directly at the lining of your oesophagus (gullet), stomach and around the first bend of your small intestine (duodenum). A long, thin, soft & flexible tube (gastroscope), about the thickness of your little finger and with a bright light on the end is passed through your mouth. Why do I need an upper GI endoscopy? This test is usually performed when patients complain of symptoms such as persistent upper abdominal pain, nausea, vomiting, bleeding or difficulty swallowing. An alternative test is a barium meal. However, upper GI endoscopy is more accurate for detecting inflammation, ulcers, tumours and bleeding and allows treatment to be carried out if necessary. What do I need to do to prepare for the test? You should have nothing to eat or drink for at least 6 hours (and preferably overnight) before the procedure, although you may drink a small cup of water if you’re very thirsty. Regular prescription medication can be taken. Please bring a list of these when you attend. Throat Spray or Sedation? We can perform the test using either throat spray (local anaesthetic to numb the back of the throat) or a sedative injection that will make you drowsy. The sedative will not usually make you unconscious as it is not a general anaesthetic. Throat spray is probably safer than the sedative injection. The advantages of throat spray are: A shorter recovery time afterwards You will be able to return to your normal daily routine on the same day. You will be able to discuss the findings of your endoscopy immediately with the endoscopist The main advantage of sedation is that most patients remember little or nothing of the procedure. The main disadvantage of sedation is a longer recovery time afterwards and a possible ‘hangover’ with some drowsiness that may last up to 24hours. Many people prefer throat spray as it is more convenient although a little less comfortable compared to sedation. Modern endoscopes are now very small and easier to swallow. We would generally recommend throat spray unless you are extremely anxious. What will happen? You may be asked to remove some clothing, put on a hospital gown and remove any glasses or dentures. An endoscopist and/or nurse will explain the procedure to you. Please make sure you inform them if you have any heart or lung problems, diabetes or other medical problems. have any allergies have an artificial heart valve or have suffered an infected valve (endocarditis) are taking any medicines to thin your blood e.g. warfarin, aspirin, clopidogrel You will be asked to lie comfortably on your left side. A throat spray or sedative injection will be given before the gastroscope is passed through your mouth into your throat. It will not cause you any pain or interfere with your breathing. A mouthguard will protect your teeth. The endoscope is then passed into the stomach and upper intestine. You may feel bloating or the urge to belch during the procedure because the endoscopist passes air into the stomach to get a better view. This will pass quickly. If saliva builds up in your mouth then the nurse will remove it with a sucker, like at the dentist. The endoscopist may wish to take a sample of tissue (biopsy) for examination in the laboratory. Only a tiny piece of tissue is removed and it is completely painless. Sometimes treatment is possible through the gastroscope such as the stretching of narrowed areas (dilatation), removal of polyps or swallowed objects and the treatment of bleeding from, for example, ulcers. Your endoscopist will talk to you about the likelihood of needing these treatments before the procedure. What happens after an upper GI endoscopy? The procedure will usually take 5-15minutes but you may be in the endoscopy unit for up to 4 hours in total, for preparation and recovery. If you have had throat spray, you should not eat or drink for an hour after the procedure because the spray can temporarily interfere with swallowing. Remember that if you have sedation, and are an outpatient, you must arrange for someone to come and pick you up, as the effects of the sedation may last for up to 24hours. You should not drive, operate machinery, work or make important decisions during this period. Somebody must be able to stay with you 24hours. What are the known risks of upper GI endoscopy? There may be a slight risk to dental crowns or bridgework. Tell the nurses if you have any of these. Complications from upper (GI) endoscopy are very rare (less than 1:1000). These include a perforation or tear of the intestine, which may require surgery, bleeding and a reaction to the sedative injection. The risks are slightly higher when the endoscopy is used to give treatment e.g. dilatation of the gullet. It is important for you to recognise early signs of any complications. Contact your GP if you notice any of the following symptoms or are worried. Fever or chills Trouble swallowing Increasing throat, chest or abdominal pain Passage of black tarry stools When will I know the result? In many cases, the endoscopist will be able to tell you the results of the test immediately. However, it may take several days or weeks to get the results of any biopsies taken. These results will be sent to the doctor who referred you as soon as they are available. Final Points Don’t worry if you do not remember all that you have read, as you will have plenty of opportunity to discuss the test and your condition with the medical and nursing staff. However, it is important that we know that you have understood what you have read so far. Please take some time to re-read this information and when you are happy, please complete the form on the opposite page. If you have any queries at all please feel free to phone us on ☎ 01752 517547 or 01752 245155. Endoscopy Consent Form Please complete the following: Surname……………………………………………… First name …………………………………………… or affix patient label here Date of Birth…………………Hospital No…………. Address………………………………………………. ……………………………………………………….. I have read and understood the information sheet opposite. I therefore give informed consent to have an Upper GI Endoscopy I understand that: A fully trained endoscopist will supervise the procedure although you cannot guarantee a particular person will perform the procedure. Additional procedures may need to be performed if it is necessary to save my life or prevent serious harm to my health. I can decide not to have this procedure There is a small risk of bleeding or perforation of the gut, following which surgery may be necessary. Other rare complications include aspiration pneumonia a reaction to the sedative drugs a slight risk to crowned teeth or dental bridgework If I have sedation, a relative or friend must be available to stay with me for 24 hours I understand that small tissue or fluid samples may be taken for diagnosis and that these may be stored and used for education, training and quality control in the future in the future I give permission/refuse permission (please delete as appropriate) for small amounts of this stored tissue sample to be used for ethically approved research in the future Patients Signature: ……………………………………. Date:………………………….. Endoscopist’s declaration I declare that the patient named above understands the nature, indications, intended benefits alternatives and serious or frequently occurring risks of Upper GI Endoscopy and therefore gives informed consent: Additional comments e.g. therapeutic procedures etc. Endoscopist’s Signature: ……………………… Date:……………………… Print Name: …………………………………… Job Title:……………………..