chapter 23-the digestive system - Shelton State Community College
advertisement

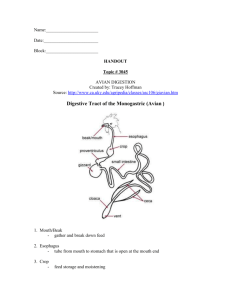
CHAPTER 23-THE DIGESTIVE SYSTEM I. THE DIGESTIVE SYSTEM-takes in food, breaks it down into nutrients, absorbs the nutrient molecules into the bloodstream, and then rids the body of the indigestible remains. A. The organs of the Digestive System are classified into two groups: 1. Those of the Alimentary Canal-which is also known as the GI Tract. a. The alimentary canal is a continuous, muscular tube that winds through the body. This canal specifically functions by breaking food down into small fragments and absorbing the fragments through its lining into the blood. Due to this, many people refer to the digestive system as a “disassembly line.” b. The major organs of the alimentary canal are: the mouth, pharynx, esophagus, stomach, small intestine, and large intestine. The large intestine leads to the terminal opening known as the anus. 2. The Accessory Digestive Organs-which includes the teeth, tongue, gallbladder, salivary glands, liver and pancreas. II. SIX MAJOR DIGESTIVE PROCESSES A. Ingestion-taking food into the digestive tract. B. Propulsion-movement of food through the alimentary canal. This includes swallowing and peristalsis. Peristalsis involves alternate waves of contraction and relaxation of muscles in the walls of organs. It squeezes food along through the digestive system. C. Mechanical Digestion-physically prepares food for chemical digestion. This includes chewing, mixing of food with enzymes, churning food in the stomach and segmentation (rhythmic, local constrictions of the intestines). Segmentation mixes food with digestive juices and it increase the rate of absorption. D. Chemical Digestion-occurs as enzymes break down food materials into their primary components. Much of this occurs in the lumen of the alimentary canal. E. Absorption-the passage of digested end products with vitamins, mineral and water, from the lumen of the GI Tract into the blood or lymph. F. Defecation-the process through which indigestible wastes are removed from the body in the form of feces. III. GENERAL STRUCTURE OF THE ORGANS IN THE DIGESTIVE SYSTEM A. Most of the digestive organs reside in the abdominopelvic cavity. The peritoneum is a serous membrane that covers the abdominopelvic cavity. The visceral peritoneum covers the external surfaces of the digestive organs and the parietal peritoneum lines the body wall. 1. The space between the two peritoneums is referred to as the peritoneal cavity which usually contains lubricating fluid. B. Mesentery-double layer peritoneum that extends to the digestive organs from the body wall. 1. These are made of two sheets of serous membranes fused back to back. 2. Mesentery functions by: providing routes for blood vessels, lymphatics and nerves to reach the digestive viscera, holding organs in place and storing fat. 3. Intraperitoneal organs are covered by and held on place by mesentery; whereas Retroperitoneal organs lose their mesentery and lie posterior to the peritoneum. 4. What is peritonitis? IV. THE SPLANCHNIC CIRCULATION-includes those arteries that branch off of the abdominal aorta to serve the digestive organs and the hepatic portal circulation. A. The major arteries in this circulation include: 1. The Hepatic Artery-supplies blood to the _____________. 2. The Splenic Artery-supplies blood to the _____________. 3. Left Gastric branches of the Celiac Trunk-supply blood to the ____________. 4. Superior and Inferior Mesenteric Arteries-supply blood to the _________________. B. The Hepatic Portal Circulation collects nutrient-rich venous blood from the digestive viscera and delivers it to the liver where absorbed nutrients are processed or stored before they are released back to the bloodstream for cellular use. V. HISTOLOGY OF THE ALIMENTARY CANAL A. The walls of the alimentary canal (from the esophagus to the anus) contain the same four basic layers or tunics. Each of these layers is involved in a specific function in food breakdown. B. The Four Basic Layers of the Alimentary Canal: 1. The Mucosa (Mucous Membrane)-the innermost layer, is composed of moist epithelial tissue. This layer lines the lumen from the mouth to the anus. a. Its Major Functions are: 1) Secretion of mucus, digestive enzymes and hormones. 2) Absorption of the end products of digestion into the blood. 3) Protection against infectious disease b. Three Sublayers That Makeup Digestive Mucosa 1) A lining epithelium-usually simple columnar epithelium with goblet cells. 2) A lamina propria-loose areolar connective tissue, highly vascular. 3) A muscularis mucosa-smooth muscle cells that produce movement of the mucosa. 2. The Submucosa-external to the mucosa. Composed of connective tissue that contains blood vessels, nerve fibers and lymphatic vessels. 3. The Muscularis Externa-is involved in segmentation and peristalsis. This layer is composed of two layers of smooth muscle (an inner circular layer and an outer longitudinal layer). a. In some areas, the circular layer of smooth muscle thickens to form sphincters to prevent backflow and control the passage of food from one organ to the next. 4. The Serosa-also known as the Visceral Peritoneum, this is the outermost, protective layer around a digestive organ. a. It is formed by areolar connective tissue covered by mesothelium-a single layer of squamous epithelial tissue. VI. THE ENTERIC NERVOUS SYSTEM OF THE ALIMENTARY CANAL A. The alimentary canal has its own nerve supply that is produced by enteric neurons. 1. Enteric neurons communicate with each other to regulate the activities within the digestive system. B. There are two major Nerve Plexuses found in the walls of the alimentary canal: 1. The Submucosal Nerve Plexus-located in the submucosa, this nerve plexus generally regulates the activity of glands and smooth muscle in the mucosa. 2. The Myenteric Nerve Plexus-lies in the smooth muscle of the muscularis externa. a. Enteric neurons here regulate GI tract motility. C. The Autonomic Nervous System often regulates many of the activities of the enteric neurons in the digestive system. VII. We will now begin our examination of the major organs and structures involved in digestion. We will discuss the special features of each structure and examine what activities they perform in digestion. VIII. THE MOUTH-the only part of the digestive system that is involved in ingestion. A. The mouth plays a key role in beginning the digestive process. B. The opening of the mouth is referred to as the Oral Orifice. C. The walls of the mouth (oral cavity) are covered by mucosa and stratified squamous epithelium which can withstand friction and stress. D. The Major Structures Associated With the Mouth Include: 1. The Lips and Cheeks-composed of a skeletal muscle core that is covered by skin. a. These two structures keep food between the teeth. b. The Labial Frenulum-a fold of tissue that joins the internal aspect of each lip to the gum. 2. The Palate-forms the roof of the mouth. a. Two Parts to the Palate: 1) The Hard Palate-anterior portion, is supported by the palatine bones and the palatine processes of the maxillae. This structure forms a thick structure against which the tongue forces food against during chewing. The mucosa on either side of the midline of the hard palate is corrugated which helps to create friction. 2) The Soft Palate-composed of mostly skeletal muscle. a) The Uvula-projects downward from the free edge of the soft palate. b) The soft palate rises reflexively to close off the nasopharynx when we swallow. c) The soft palate is held in place by the palatoglossal arches and the palatopharyngeal arches. These structures form the boundaries of fauces-the region of the oropharynx that contains the palatine tonsils. 3. The Tongue-occupies the floor of the mouth. a. It is composed of bundles of skeletal muscle fibers. b. During chewing, the tongue holds and positions the food so that saliva can be mixed with the food. This process produces a mass called a bolus, which the tongue can push into the pharynx. c. The Lingual Frenulum-a fold of mucosa that attaches the tongue to the floor of the mouth and limits posterior movements of the tongue. 1) What is Ankyloglossia? d. Recall that the tongue is covered by papillae which store taste buds. 4. The Salivary Glands-produce and secrete saliva into the oral cavity. a. Two Categories of Salivary Glands: 1) Extrinsic Salivary Glands-lie outside of the oral cavity and empty their secretions into it. 2) Intrinsic Salivary Glands-are scattered throughout the oral cavity mucosa. b. The Major Extrinsic Salivary Glands include: 1) The Parotid Gland-large, is anterior to the ear between the skin and masseter muscle. Saliva is carried from this gland to the mouth via the Parotid Duct which opens in the mouth near the second molar. a) What are the Mumps? 2) The Submandibular Gland-lies near the mandibular body. Its duct opens near the lingual frenulum. 3) The Sublingual Gland-anterior to the submandibular gland, under the tongue. a) Connects to the floor of the oral cavity via 10-12 ducts. c. Saliva is slightly acidic (6.75-7.00) and it is composed mostly of water (97-99.5%). 1) Saliva also contains: a) Electrolytes (Such as K+, Na+) b) Salivary amylase-a key digestive enzyme c) Mucin-forms a lubricating mucus when dissolved in water. d) Lysozome-enzyme that inhibits bacterial growth on the teeth. e) Defensins-a natural antibiotic. 2) Specific Functions of Saliva a) Cleanses the mouth b) Dissolves food chemicals for taste c) Moistens food for digestion d) Contains various digestive enzymes d. Humans secrete about 1000-1500 ml of saliva per day. e. Salivation is primarily controlled by the Autonomic Nervous System through the Glossopharyngeal nerve. 1) What is Xerostomia? 2) What is Halitosis? 5. The Teeth-located in sockets (alveoli) of the mandible and maxillae. a. The teeth allow us to grind and tear food as we chew. b. Humans have two sets of teeth: 1) Primary Teeth (Baby or Milk Teeth)-20 of these total. These loosen and fall out between the ages of 6 and 12. 2) Permanent Teeth-there are typically 32 teeth in the permanent set. a) What are the major types of teeth, where are they located and what is their major function? c. Tooth Structure 1) Crown-exposed portion of a tooth above the gingiva (gums). 2) Enamel-hardest compound in the body, forms the outer covering over a tooth. It is primarily composed of mineral salts and mineral crystals. The cells that produce enamel erupt when the tooth is damaged. 3) The Root-the portion of the tooth that is embedded in the jawbone. a) How many roots do teeth typically have? 4) The Neck-connects the crown and root of the tooth together. 5) Cementum-this calcified material covers the outer surface of the root and connects the tooth to the Periodontal Ligament which anchors the tooth into the jawbone; thus forming a joint known as a Gomphosis. 6) Dentin-bonelike material, underlies the enamel of the tooth and forms the bulk of the tooth. It surrounds a pulp cavity that stores blood vessels, nerves and connective tissue (which is collectively referred to as Pulp). a) Where the pulp extends into the root, it becomes the Root Canal. b) At the end of each root, there is an Apical Foramen that allows blood vessels and nerves to enter the tooth c) Odontoblasts are responsible for secreting dentin. d) Enamel, cementum and dentin are all calcified like bone; however they are avascular-unlike bone tissue. d. What are the following? 1) Dental Caries 2) Dental Plaque 3) Calculus 4) Periodontitis IX. THE PHARYNX-connects the oral cavity to the esophagus. A. Food passes from the mouth into the oropharynx and then the larngopharynx (both are common passageways for flood, fluid and air). B. The histology of the pharynx is essentially the same as the oral cavity. X. THE ESOPHAGUS-a muscular tube that carries food materials from the larngopharynx to the stomach. A. The esophagus runs essentially straight through the mediastinum of the thorax and pierces the diaphragm at the esophageal hiatus. This tube enters the stomach at the cardiac orifice which is surrounded by the esophageal or cardiac sphincter. 1. The esophageal sphincter acts as a valve that opens when food passes into the stomach and closes when food is not present. Smooth muscle and contractions of the diaphragm act to control this sphincter. 2. The esophagus is approximately 25 cm long. 3. The esophagus is collapsed when food is not passing through. B. The wall of the esophagus has all four of the basic alimentary canal layers. Some specific features of the layers in the esophagus are as follows: 1. Simple columnar epithelium appears in the mucosa at the esophagus/stomach junction. This tissue is specialized for secretion. 2. The submucosa contains esophageal glands which secrete mucus as a bolus passes by. The mucus acts to “grease” the esophagus to aid in food passage. 3. The muscularis layer is skeletal muscle at the upper portion of the esophagus, a mixture of skeletal and smooth muscle in the midportion of the esophagus and smooth muscle as the esophagus approaches the stomach. C. Homeostatic Imbalances: 1. Heartburn 2. Hiatal hernia XI. DIGESTIVE PROCESSES IN THE MOUTH, PHARYNX AND ESOPHAGUS A. In the Digestive Process, the Mouth functions by: 1. Ingesting food 2. Starting mechanical digestion by chewing 3. Initiating propulsion via swallowing 4. Releasing Salivary Amylase and Lingual Lipase via saliva secretion. a. Salivary Amylase is an enzyme that initiates the breakdown of starch. b. Lingual Lipase functions in the acidic environment of the stomach. B. Essentially no absorption occurs in the mouth. C. The Pharynx and Esophagus simply serve as passageways for food to pass as it moves from the mouth to the stomach. D. Mastication (Chewing)-this occurs as the teeth tear and grind food and as food is softened as it mixed with saliva. E. Deglutition (Swallowing)-Involves 22 muscles and occurs through two phases: 1. Buccal Phase-voluntary, occurs in the mouth. In this phase, the tongue contracts to push the bolus into the oropharynx. Deglutition becomes involuntary at this point. 2. Pharyngeal-Esophageal Phase-controlled by the swallowing center in the medulla and pons. When food enters the pharynx, breathing is temporarily stopped as: the tongue blocks the mouth, the epiglottis covers the respiratory passages and the soft palate closes off the nasopharynx. a. It takes about 8 seconds for solid food to reach the stomach from the mouth. XII. THE STOMACH-organ where chemical breakdown of proteins begins and food is converted into a material known as chyme. A. Anatomy of the Stomach 1. The stomach ranges from 15-25 cm in length and it can hold up to 4L (1 gallon) of food when full. When the stomach is empty, it collapses throwing its mucosa into folds known as Rugae. B. Major Regions of the Stomach: 1. Cardiac Region (Cardia)-“near the heart.” This area surrounds the cardiac orifice through which food passes as it enters the stomach from the esophagus. 2. The Fundus-dome-shaped portion of the stomach, beneath the diaphragm. 3. The Body-midportion 4. The Pyloric Region a. Pyloric Antrum-wide portion of the pyloric region, narrows to form the pyloric canal which terminates at the pylorus. b. The pylorus is continuous with the duodendum (of the small intestine). c. The Pyloric Sphincter separates the pylorus and the duodendum. This muscle regulates and controls stomach emptying. C. Greater vs. Lesser Curvature of the Stomach 1. Omenta extend from these curvatures to attach the stomach to other structures in the abdominal cavity. 2. The Lesser Omentum-extends from the liver to the lesser curvature of the stomach and becomes continuous with the visceral peritoneum that covers the stomach. 3. The Greater Omentum-extends from the greater curvature of the stomach and covers the folds of the small intestine. This structure also covers the spleen and large intestine before it becomes part of the mesocolon. The greater omentum is covered with fat deposits and lymph nodes; therefore, this structure plays a role in defense and immunity. D. The stomach is regulated by the ANS and the bulk of the blood flowing to the stomach comes from branches of the celiac trunk. E. Microscopic Anatomy of the Stomach 1. The stomach contains the four typical layers of the alimentary canal, but its muscularis and mucosa are specialized for the specific functions that occur in the stomach. 2. The Muscularis of the Stomach-contains smooth muscle arranged in the normal circular and longitudinal fashion. However, there is an extra layer of fibers arranged in an oblique fashion in the muscularis of the stomach. 3. The Mucosa of the Stomach is composed primarily of simple columnar epithelium that contains nothing but goblet cells. How do goblet cells function? a. The mucosa of the stomach at first appears smooth, however, it contains millions of deep pits known as Gastric Pits which lead to Gastric Glands that are responsible for secreting Gastric Juice. b. Secretory Cells Found in the Gastric Pits of the Stomach Mucosa 1) Mucous Neck Cells-found in the upper or neck of gastric glands. These secrete an acidic mucus during digestion. 2) Parietal Cells-secrete hydrochloric acid and intrinsic factor. These cells contain folds known as microvilli which increase their surface area for acid production. Why is hydrochloric acid important in digestion? 3) Chief Cells-produce pepsinogen (the inactive form of the protein-digesting enzyme pepsin). 4) Enteroendocrine Cells-releases chemical messengers (Histamine), and hormones (such as Gastrin) into the stomach during digestion. c. The stomach mucosa is exposed to an extremely acid environment. To protect itself, the mucosa produces a Mucosal Barrier that is created by: 1) Bicarbonate mucus layer that covers the stomach wall. 2) Tight connections between the cells of the mucosa to prevent acid leakage. 3) Rapid replacement of the cells in the mucosal layer of the stomach. F. What are Gastric Ulcers and what are they caused by? G. Digestive Processes That Occur in the Stomach 1. In general, the stomach is involved in breaking down food into chyme and then moving the chyme into the small intestine. 2. The stomach releases hydrochloric acid, digestive enzymes and intrinsic factor (involved in absorption in the intestines) into the food/chyme as digestion is occurring. a. Secretion of these compounds in the stomach is regulated by the ANS (Vagus Nerve) and Hormones. Various stimuli in the stomach and small intestine can provoke or inhibit secretion by the glands in the stomach. b. Three Phases of Gastric Secretion: 1) Cephalic (Reflex) Phase-occurs before food enters the stomach. Triggered by the smell, taste or thought of food. This prepares the stomach for digestion. This area is often suppressed during depression. 2) Gastric Phase-occurs when food reaches the stomach, may last up to 4 hours. Stimuli (low acidity, partially digested protein etc…) can force the release of G cells in the stomach which initiate the production of acid and enzymes by glands in the stomach. 3) Intestinal Phase-may be excitatory or inhibitory. a) The Excitatory Portion–occurs when food moves into the duodenum stimulates gastric glands to continue secreting their digestive materials. b) The Inhibitory Portion-triggered by the Enterogastric Reflex which inhibits digestive reflexes and prevents chyme from moving into the small intestine. H. Gastric Motility and Emptying 1. Stomach contractions act to mix food materials with gastric juice and they move food towards the small intestine. 2. Plasticity-the ability of visceral smooth muscle to stretch without greatly increasing its tension and contracting expulsively. 3. Peristalsis-muscular contractions occur in the stomach to move food/chyme forward. These movements push about 3ml of chyme into the small intestine. Many food materials pass through the stomach within 4-6 hours. I. What is vomiting (emesis)? XIII. THE SMALL INTESTINE AND ASSOCIATED STRUCTURES A. The small intestine is the body’s major digestive organ. This is the site where digestion is completed and most absorption occurs. B. Gross Anatomy of the Small Intestine 1. It extends from the pyloric sphincter to the ileocecal valve at the large intestine. 2. It is the longest organ in the alimentary canal (about 20 feet long). 3. 3 Subdivisions of the Small Intestine: a. Duodenum-immovable, retroperitoneal region of the small intestine. 1) Curves around the pancreas. 2) Hepatopancreatic Ampulla-in the duodenum. This is the site where the bile duct and pancreatic duct meet to empty their secretions into the small intestine. The ampulla actually opens into the duodendum via the major duodenal papilla. The Hepatopancreatic Sphincter is a muscular valve that controls the flow of bile (from the liver) and pancreatic juice into the duodenum. b. Jejunum-extends from the duodenum to the ileum, about 8 feet long. c. Ileum-about 12 feet long, attaches to the large intestine at the ileocecal valve. The jejunum and ileum occurs as rounded coils that are held in place by mesentery. The distal portions of the small intestine are held in place by the large intestine. 4. The Vagus Nerve and the Splanchnic Nerves are the major nerve connections to the small intestine. C. Microscopic Anatomy of the Small Intestine 1. It is highly adapted for nutrient absorption. The length of the small intestine offers a great surface area for this to occur in. Three structural modifications in the small intestine greatly increase the surface area of the organ for greater absorption to occur. 2. Structural Modifications That Are Involved In Absorption In The Small Intestine a. Plicae Circulares (Circular Folds)-deep folds of the mucosa and submucosa. These folds force chyme to spiral through the lumen, slowing its movement and allowing time for full nutrient absorption to occur. b. Villi-fingerlike projections of the mucosa. 1) The epithelial cells that make up the villi are primarily absorptive columnar cells. 2) The core of each villus contains: a) A Capillary bed b) A Lacteal-a wide lymph capillary. 3) Digested food materials are absorbed through the epithelial cells into both the capillary bed and lacteal. 4) There is also a band of smooth muscle in each villus core that allows it to alternately shorten and lengthen. These pulsations act to: a) Increase the contact between the villus and the contents of the lumen (opening) of the small intestine. This increases absorption. b) “Milk” lymph along the lacteals. c. Microvilli-tiny projections of the cell membrane of the absorptive cells of the mucosa. These structures give the mucosa a fuzzy appearance known as the brush border. This membrane produces enzymes that complete the digestion of carbohydrates and proteins. 3. Histology of the Wall of the Small Intestine a. The small intestine contains the typical 4 layers of the GI Tract; however, the mucosa and submucosa are modified for the digestive and absorptive functions of the small intestine. b. The Mucosa is composed of columnar epithelial cells that are highly adapted for absorption of nutrients. Goblet cells, enteroendocrine cells and T cells are also abundant in the mucosa of the small intestine. 1) Between the villi, the mucosa contains pits that lead into tubular intestinal glands called Intestinal Crypts or Crypts of Lierberkuhn. The cells that line these pits secrete intestinal juice. This fluid/mucus material serves as a carrier molecule for absorbing nutrients from chyme. 2) Paneth Cells-found in the crypts, these release defensins and lysozyme to protect the small intestine from microbial invasion. c. The Submucosa is composed of areolar connective tissue and it contains lymphoid follicles. The aggregated lymphoid follicles are referred to as Peyer’s Patches. 1) What are Peyer’s Patches involved in? 2) What are Duodenal (Brunner’s) Glands involved in? D. Intestinal Juice 1. The intestinal glands normally secrete 1-2L of intestinal juice daily. This secretion is stimulated by the presence of acidic chyme in the intestine itself which irritates the mucosa of the small intestine wall. 2. Intestinal juice is slightly alkaline (pH of 7.4-7.8). 3. Intestinal juice is largely water but it also contains some mucus. Few enzymes are present in intestinal juice. XIV. THE LIVER AND GALLBLADDER-these are considered to be accessory organs associated with the small intestine. A. The Liver-serves many roles but from a digestive point of view, the liver is responsible for producing the fat emulsifier Bile. 1. The liver is the largest gland in the body (weighs 1.4Kg or 3 Lbs.). It is located under the diaphragm and the largest portion of the liver is to the right of the midline. It is somewhat protected by the ribcage. 2. 4 Major Lobes of the Liver: a. The Right Lobe-largest lobe of the liver. b. The Left Lobe-separated from the right lobe by a deep fissure. c. The Caudate Lobe-most posterior of the lobes. d. The Quadrate Lobe-inferior to the left lobe. 3. The Falciform Ligament-mesentary, separates the right and left lobes of the liver and suspends the liver from the diaphragm and abdominal wall. 4. The Round Ligament (Ligamentum teres)-located along the inferior edge of the falciform ligament, is a remnant of the fetal umbilical vein. 5. The entire liver is covered by a visceral peritoneum and the lesser omentum anchors the liver to the lesser curvature of the stomach. 6. The major blood vessels to the liver include: the hepatic artery and the hepatic portal vein. a. These blood vessels enter the liver at the porta hepatis (gateway to the liver). 7. Bile leaves the liver via several ducts that fuse to form the Common Hepatic Duct. This duct fuses with the Cystic Duct, which drains the gallbladder of bile, to form the Bile Duct. 8. Microscopic Structure of the Liver a. The liver is composed of functional units known as Liver Lobules. Each lobule consist of liver cells (Hepatocytes) that are stacked like bricks. These hepatocytes extend outward away from a central vein that runs through the lobule. Each lobule has a 6-sided shape (Hexagonal shape). b. Remember that the primary function of the liver is to filter and process blood that contains a substantial supply of nutrients. c. Portal Triad-at the tip of each of the corners of the lobule. Three structures are always present at a Portal Triad: 1) A branch of the Hepatic Artery-what does this structure do? 2) A branch of the Hepatic Portal Vein-what does this structure do? 3) A Bile Duct. d. Liver Sinusoids-located between plates of hepatocytes, blood passes from the hepatic portal vein, through these sinusoids into the central vein. Eventually, blood from the central vein empties into the inferior vena cava. 1) Hepatic Macrophages (Kupffer Cells)-line the walls of the liver sinusoids. These cells function by removing bacteria and worn out blood cells as blood flows by. 9. Specific Functions of Hepatocytes a. Produce Bile-which is secreted into bile canaliculi that run to bile ducts. b. Process nutrients-they can store glucose as glycogen for example. c. Store fat-soluble vitamins d. Detoxify the blood of chemicals such as ammonia. e. Secrete Vascular Endothelial Growth Factor during liver injury. This hormone forces hepatocytes to multiply and replace dead or damaged cells in the liver. Due to this, the liver has a tremendous ability for regeneration. 10. Homeostatic Imbalances of the Liver a. Hepatitis b. Cirrhosis 11. Bile-a yellow-green solution that contains salts, pigments, cholesterol, fats, phospholipids and electrolytes. Bile salts and phospholipids are involved in the digestive process; however, the remaining compounds are waste products. a. Bile Salts-primarily cholesterol derivatives, these function by emulsifying fats which spreads the fats throughout the liquid in the intestine. Due to this, large fats that enter the intestine are broken down into millions of small fat droplets that can be easily acted upon by digestive enzymes. 1) Bile salts also increase fat and cholesterol absorption in the small intestine. 2) Bile salts are recycled in the small intestine. Essentially, the salts are reabsorbed in the ileum, returned to the liver via the hepatic portal blood and then resecreted in newly formed bile. b. Bilirubin-primary pigment in bile. This is a waste product of the heme portion of hemoglobin. Bilirubin is actually a breakdown product of erythrocytes. 1) Bilirubin is removed from old erythrocytes, absorbed in the liver and excreted as bile. One of the breakdown products of bilirubin is a compound known as urobilinogen which gives feces its characteristic color. 2) Humans secrete 500-1000ml of bile daily. B. The Gallbladder-a green, thin-walled organ located in a shallow fossa on the ventral surface of the liver. It is roughly about the size of a kiwi fruit. 1. The gallbladder functions by storing bile that is not immediately needed for digestion or absorption. It also concentrates bile by absorbing water and ions. Bile leaving the gallbladder is 10X more concentrated than the bile entering the gallbladder. 2. The inner wall of the gallbladder is lined with folds that allow the organ to expand as it fills with bile. 3. Bile is forced out of the gallbladder via the cystic duct and it then it flows into the bile duct. This movement is produced by contractions of smooth muscle in the walls of the gallbladder. 4. Like the liver, the gallbladder is covered by a visceral peritoneum. 5. The Hepatopancreatic Sphincter-regulates the flow of bile and pancreatic juice into the duodenum. When this structure is closed, bile backs up in the cystic duct and into the gallbladder where it is stored until needed. Bile does not enter the small intestine until the gallbladder contracts. a. Cholecystokinin (CCK)-an intestinal hormone that enters the blood when fatty and acidic chyme moves into the duodenum. This hormone functions by: 1) Fat emulsification 2) Stimulating the secretion of pancreatic juice 3) Relaxing the hepatopancreatic sphincter so that bile and pancreatic juice can enter the duodenum. 6. What are gallstones (biliary calculi)? XV. THE PANCREAS-gland extending from the stomach to the small intestine, where it is encircled by the duodenum. Most of the pancreas lies deep to the greater curvature of the stomach. A. The pancreas is an accessory digestive organ produces enzymes that breakdown all of the major organic molecules found in food. These enzymes are delivered to the duodenum. B. Pancreatic Juice-produced by the pancreas, contains the above digestive enzymes. It is delivered to the duodenum via the Main Pancreatic Duct. C. Acini-clusters of secretory cells that surround ducts within the pancreas. The cells of the acini contain structures known as Zymogen granules that manufacture digestive enzymes. D. Islets of Langerhans (Pancreatic Islets)-scattered amid the acini. These small endocrine glands release insulin, glucagon and carbohydrate-digesting hormones. E. Pancreatic Juice-humans produce 1200-1500ml of pancreatic juice daily. 1. This juice consists primarily of water, enzymes, electrolytes and bicarbonate buffer. Cells in the acini produce pancreatic juice. 2. Pancreatic juice has a reasonably high pH. This helps to neutralize acidic chyme that is entering the small intestine. 3. Many enzymatic precursors are secreted by the pancreas in pancreatic juice. These compounds become active digestive enzymes when they enter the duodenum. This prevents the enzymes from digesting the pancreas itself. 4. The secretion of pancreatic juice is regulated by a variety of hormones, including CCK. XVI. DIGESTIVE PROCESSES OCCURRING IN THE SMALL INTESTINE A. By the time chyme reaches the small intestine, proteins and carbohydrates are partially degraded, but essentially no lipid digestion has occurred. Continued digestion of the above mentioned food materials continues at a rapid pace as chyme proceeds on its three to six hour journey through the small intestine. B. Abosrption of most nutrients and large supplies of water also occurs in the small intestine. Like the stomach, the small intestine plays no role in ingestion or defecation. C. Optimal digestive activity in the small intestine depends on a slow delivery of chyme from the stomach. 1. This ensures that the acidic chyme is effectively buffered before it travels through the small intestine and it also allows for the effective mixing of chyme with intestinal and pancreatic juice and bile. This slow delivery of chyme further prevents water volume problems associated with blood as digestion is occurring. 2. As mentioned earlier, many of the compounds needed for digestion in the small intestine are produced by and secreted into the small intestine by the liver and pancreas. D. Intestinal smooth muscle mixes chyme with pancreatic juice and bile. Segmentation is the common type of smooth muscle movement in the small intestine (as compared to peristalsis in the stomach). This is accomplished as smooth muscle rings in the intestine alternately contract and relax. Peristalsis does occur near the end of the small intestine as many waste materials are moved into the large intestine. XVII. THE LARGE INTESTINE A. The large intestine frames and surrounds the small intestine on three sides and extends from the ileocecal valve to the anus. It is about 7cm in diameter and approximately 1.5m long. B. The Large Intestine is primarily involved in: absorbing the last amounts of water from indigestible food and storing and eventually removing the waste materials generated as food is broken down in the digestive process via feces. C. Three Unique Features of the Large Intestine: 1. Teniae coli-three bands of longitudinal smooth muscle located in the muscularis of the large intestine. 2. Haustra-pocketlike sacs that make up the large intestine. Contractions of the teniae coli form these structures. 3. Epiploic Appendages-fat-filled pouches of visceral peritoneum that hangs from the surface of the large intestine. Their function is unknown. D. The Major Subdivisions of the Large Intestine Include: 1. The Cecum-first part of the large intestine, saclike structure which lies below the ileocecal valve in the right iliac fossa. 2. The Vermiform Appendix-attached to the posteromedial surface of the large intestine. This structure contains masses of lymphoid tissue and it may play a role in immunity. However, its structure can allow bacteria and foreign debris to become trapped, leading to an appendicitis. What is an appendicitis? 3. The Colon-major regions of the colon include: a. The Ascending Colon-travels up the right side of the abdominal cavity to the level of the right kidney where it makes a right-angle turn known as the right colic or hepatic flexure. From here, the colon travels across the abdominal cavity as the Transverse Colon. Anterior to the spleen, the transverse colon bends at the left colic (splenic) flexure and descends downward as the Descending Colon. Inferiorly, the descending colon enters the pelvis, where it becomes the S-shaped Sigmoid Colon. b. All of the above regions of the colon are surrounded by sheets of mesentery known as Mesocolons. 4. In the pelvis, near the level of the third sacral vertebra, the sigmoid colon joins the rectum. a. Internally, the rectum has three lateral bends or curves known as rectal valves. These valves separate feces from flatus so wastes are not passed with gas. 5. Anal Canal-last portion of the large intestine. This canal opens to the exterior of the body via the anus. Two Sphincters in the Anal Canal: a. Internal Anal Sphincter-composed of smooth muscle, is involuntary. b. External Anal Sphincter-composed of skeletal muscle, is voluntary. Both muscles function to open and close the anus. They are ordinarily closed except during defecation. E. Microscopic Anatomy of the Large Intestine 1. The walls of the Large Intestine differ from that of the Small Intestine in several ways: a. The mucosa is composed of simple columnar epithelium. In the large intestine, there are no folds, no villi and very few cells that secrete digestive enzymes. 1) Goblet cells are abundant in the large intestine. The mucus secreted by these cells eases the passage of feces through the large intestine. b. In the rectum, the muscularis is thick and well-developed. 2. There are a number of nerves and blood vessels associated with the large intestine. The hemorrhoidal veins are the major veins associated with the anal canal. What are hemorrhoids? F. Bacterial Flora-refers to the bacteria that inhabit the large intestine. 1. These bacteria ferment many of the indigestible carbohydrates that we eat to produce a mixture of gases known as flatus. About 500ml of flatus is produced each day. 2. The bacterial flora also helps to synthesize B complex vitamins and most of the vitamin K that is used by the liver to synthesize clotting factors. G. Digestive Processes Occurring in the Large Intestine 1. Essentially no food breakdown occurs in the large intestine (except for that associated with the bacterial flora). 2. The large intestine does absorb a few vitamins, water and electrolytes. 3. The primary function of the large intestine is to propel fecal material towards the anus and eliminate it from the body via defecation. 4. Musculature of the large intestine is inactive most of the time. Most movements of the large intestine are produced by haustral contractions which are slow movements that occur about every 30 minutes. These contractions move materials from one haustrum to another. a. Mass Movements (Mass Peristalsis)-long, slow, powerful contractions that move over the entire colon. These occur 3 or 4 times a day. These push materials to the rectum. 5. What is diverticulosis? What is diverticulitis? 6. Defecation-feces removal from the body. a. Defecation reflex-parasympathetic reflex that forces the sigmoid colon and rectum to contract and the anal sphincters to relax. b. What is Valsalva’s Maneuver? c. What is diarrhea? constipation? XVIII. PHYSIOLOGY OF CHEMICAL DIGESTION AND ABSORPTION A. Chemical Digestion-catabolic process in which large food molecules are broken down to monomers that are small enough to be absorbed by the GI tract lining. This is accomplished by enzymes that are secreted by cells and glands associated with the lumen of the alimentary canal. This use of enzymes in food breakdown is referred to as hydrolysis. This ends in the small intestine-no chemical digestion occurs in the large intestine. B. Chemical Digestion of Carbohydrates 1. Monosaccharide, Disaccharide, Polysaccharide 2. Most digestable carbohydrates are in the form of starch or simple sugars. 3. Salivary amylase-present in saliva, breaks starch down into glucose molecules. a. This enzyme works best in the slightly acidic environment of the mouth. b. This enzyme continues to digest starch until it is broken down itself by the acid of the stomach. 4. Pancreatic amylase-secreted into the small intestine, completes the digestion of starch that evades digestion in the mouth and stomach. 5. Dextrinase, Glucoamylase-brush border enzymes that digest various simple sugars in the small intestine. 6. What is lactose intolerance? C. Chemical Digestion of Proteins 1. Proteins are usually broken down into amino acids. 2. Protein digestion usually begins in the stomach when pepsinogen is converted into the enzyme pepsin. Pepsin functions extremely well in the acidic conditions of the stomach. Pepsin digests about 15% of the incoming protein. The activity of this enzyme is stopped by the high pH (compared to the stomach) of the duodenum. 3. Rennin-breaks down the protein in milk and dairy products. 4. Trypsin, Chymotrypsin-secreted into the small intestine by the pancreas, both of these play a key role in breaking protein down into amino acids. 5. Aminopeptidase-another protein digesting enzyme, secreted by cells in the brush border. D. Chemical Digestion of Lipids 1. Lipases are responsible for digesting many lipids components in the body. 2. Michelles-collections of fatty elements clustered together with bile salts. These are very small and can easily carry their fat components through the intestinal wall. Once fats are inside of cells, they are resynthesized to produce triglycerides. E. Chemical Digestion of Nucleic Acids 1. These compounds are broken down in the small intestine. The sugars from the various nucleic acids are carried through the small intestine wall by carrier molecules. These sugars are then transported to the blood. F. Absorption-about 80% of the food and drink materials that enter the alimentary canal are absorbed in the small intestine. 1. Most nutrients are absorbed by active transport processes at the mucosa layer of the small intestine. This overall process requires ATP to occur. G. Absorption of Carbohydrates-sugars are generally moved through the small intestine mucosa by active transport. Carbohydrates then diffuse into capillaries for distribution throughout the body. H. Absorption of Proteins-involves the use of carrier molecules that attach to and physically move the amino acids through the wall of the small intestine. I. Absorption of Lipids 1. Micelles are used to carry lipids through the wall of the small intestine. J. Absorption of Vitamins 1. Fat soluble vitamins (A, D, E, K) become incorporated into micelles and are carried across the mucosa layer of the small intestine. 2. Most water soluble vitamins (B and C) diffuse through the small intestine. K. Electrolyte Absorption 1. Many electrolytes are carried through the mucosa of the small intestine via active transport. Electrolyte absorption is often regulated by hormones and vitamins. L. Water Absorption-95% of the water in chyme is absorbed in the small intestine via osmosis. M. Malabsorption-impaired nutrient absorption. This can be caused by a variety of factors. XIX. RELATED CLINICAL TERMS A. Ascites B. Barrett’s Esophagus C. Bruxism D. Bulimia E. Dysphagia F. Endoscopy G. Enteritis H. Hemochromatosis I. Ileus J. Inflammatory bowel disease K. Laparoscopy L. Orthodontics M. Pancreatitis N. Peptic ulcers O. Proctology P. Pyloric stenosis Q. Vagotomy R. Xerostomia