CH 16 – Poisoning
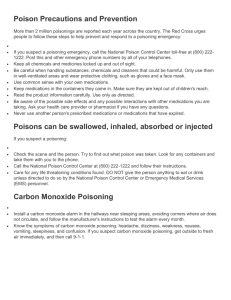
advertisement

1 CH 16 – Poisoning General Information: -poisoning results when external substances enter the body -90% of all poisonings occur in home -Most unintentional poisoning occur in children under the age of 5. But fewer than 5% of those children die -Deaths in children has dropped in last 30 years while adults has gone up. Why? How poisons enter the body: Ingestion Injection Inhalation Absorption Clues of poisoning: Odors Flames or smoke Containers that are open or out of place Plants partially eaten or disturbed Common signs and symptoms of poisoning: Nausea Vomiting Diarrhea Chest or abdominal pain Breathing difficulty Sweating Loss of consciousness Seizures Burn injuries around the lips or tongue or on the skin Headache Dizziness Weakness Irregular pupil size Burning or tearing eyes Abnormal skin color Poisoning Severity The type and amount of poison How and when it entered the body Victim’s size, weight, and age General Principles for Poisoning Emergencies: Conduct scene size-up 2 Remove victim from source of poison Conduct initial assessment Conduct physical exam and SAMPLE history Summon more advanced medial personnel Contact poison control center (PCC) as per local protocols o If unconscious, call 911 Do not give anything to eat or drink ONLY induce vomiting when told to do so by medical personnel. You would never induce if: Victim is unconscious Victim is having a seizure Victim is pregnant Victim has ingested corrosive substance or petroleum product Victim is known to have heart disease. Food poisoning: Approximately 33 million Americans affected by food poisoning each year. Symptoms begin 1 to 48 hours after eating: o Nausea o Vomiting o abdominal pain o diarrhea o fever o dehydration Most food poisoning can be prevented by proper cooking, refrigeration, and sanitation Absorbed poisons: Cause: poison ivy, poison oak, poison sumac, wet or dry chemicals If chemicals contact the skin: brush off dry residue with gloved hand & flush with water Injected poisons: Signs & Symptoms affected by: -type & location of bite or sting -amount of poison injected -time elapsed -victim's size, wt., & age Symptoms include: At entry site: -bite or sting mark -stinger, tentacle, or venom sac -redness -swelling -pain or tenderness 3 Severe allergic reactions to bites & stings may bring on anaphylaxis, & result in a breathing emergency CARE FOR SPECIFIC BITES & STINGS Insects: -between 1 & 2 million Americans are severely allergic to venom or bees, wasps, hornets, and yellow jackets -if highly allergic, one sting = anaphylaxis -If highly allergic--call EMS immediately -for most people, stings hurt, but are rarely life-threatening: -scrape away the stinger -wash & cover the site -apply ice or cold pack -watch for signs of allergic reactions Note: Less than 100 deaths per year from insect bites Ticks ROCKY MT. SPOTTED FEVER - wood or dog tick. Main sign: spotted rash that appears first on wrists or ankles, then spreads rapidly -early treatment is crucial--may die from kidney failure or shock LYME DISEASE: -deer ticks can be very small -may not know you were bitten -disease seen in 40 states symptoms: -a rash at the site of the bite -rash spreads up to 5-7" -rash may have a bull's eye appearance, or in dark skin people, may look black & blue like a bruise. (Note: you may have Lyme disease without a rash.) -fever & chills -headache -weakness or fatigue -joint & muscle pain similar to the flu Remove ticks: slowly with tweezers, wash with soap & water Spiders: Black widow-black w/ reddish hourglass-shaped marking on its underbody Brown recluse - light brown w/ a darker brown violin-shaped marking on the top of its body 4 Scorpions - Southwestern US Symptoms of black widow bite: -sharp pain initially (BW); no pain initially for BR -muscular rigidity in shoulders, back, & abdomen -restlessness -anxiety -profuse sweating -weakness -drooping of eyelids First aid: -call EMS Misc. symptoms of spider bites: -mark indicating a possible bite -severe pain -blister, lesion, or swelling -nausea & vomiting -difficulty breathing or swallowing -sweating or salivating profusely -irregular heart rhythm -muscular cramping or abdominal pain Snakebite: Guidelines for initial care of snakebite: Take victim to medical care immediately Wash wound if possible Immobilize affected part Minimize victim’s movement Keep affected part lower than heart Summon more advanced medical personnel Consider using a commercial suction kit if advanced medical care is more than 30 minutes away Marine Life: CALL EMS IF: -history of allergic reactions -stung on face or neck -develops breathing problems FIRST AID: For jellyfish, sea anemone, or man-of-war stings: soak in vinegar. DO NOT: rub, use fresh water or ammonia. For sting ray, sea urchin, or spiny fish: flush with water; immobilize; soak in HOT water (or hot sand) for 30 min or until pain eases; clean & bandage 5 Domestic and Wild Animals: Rabies is transmitted through saliva -most common carriers: skunks, raccoons, cats, dogs, cows, bats, & foxes. -rabies is fatal unless treated Tetanus is potentially fatal; caused by transmission of toxin when bitten by animal or human symptoms: -irritability -headache -fever -painful muscular spasms (particularly stiffness of the jaw) Takes 3 days to 5 wks for symptoms Prevention: -professionals clean wound -immunization injections All animal bites: -get person away from animal -contact animal control--do NOT try to capture animal First aid: Minor: wash w/ soap & water; then control bleeding & apply antibiotic ointment & a dressing. Visit the Dr. Watch for infection. Major: control bleeding; call EMS Human bites: May be highly contaminated with bacteria Require professional medical care immediately Need to be washed with soap and water Can bleed if severe; control severe bleeding Anaphylaxis: Cause: insect bites, stings, medications, foods, and chemicals. Symptoms: swelling & redness hives itching rash weakness nausea or vomiting 6 Care: dizziness rapid or difficult breathing burning skin and eyes restlessness slurred speech dilated pupils chest discomfort or pain weak or rapid pulse coughing or wheezing assess airway and breathing summon more advanced medical care if they have any trouble breathing or say they feel their throat closing help the victim in the most comfortable position administer oxygen is available and you arte trained to do so monitor ABCs and keep victim calm Have victim use anaphylaxis kit if one is available. Substance Misuse and Abuse: Six major types of substances that are abused and misused are: 1. stimulants 2. hallucinogens 3. depressants 4. narcotics 5. inhalants 6. cannabis products Depressants: Relieve anxiety Alter consciousness Promote sleep Relieve pain Relax muscles Impair coordination and judgment Other substances: Designer drugs – are variations of other substances, such as narcotics and amphetamines – ex -ecstasy Anabolic steroids Over the counter substances Care for substance miscue and abuse: Your initial care does not require you know the substance Care as you would for poisoning 7 The following factors may contribute to substance abuse: A lack of parental supervision The breakdown of traditional family structure A wish to escape unpleasant surroundings and stressful situations The widespread availability of substances Peer pressure and the basic need to belong Low self-esteem, feelings of guilt or shame Media glamorization A history of substance abuse in the home or community environment Preventing substance misuse: 1. To prevent unintentional misuse or overdose: Read product information and take as directed Ask your doctor about side effects and drug interactions Never use anyone else’s prescription medication Always keep medication in marked containers Destroy out of date medications Always keep medications out of children’s reach