Canine Malassezia dermatitis
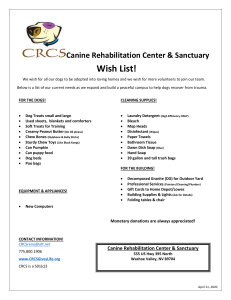
advertisement

Malassezia dermatitis: an opportunist attacks and a host responds Daniel O. Morris, DVM, Diplomate, ACVD Asst. Professor and Chief of Dermatology & Allergy University of Pennsylvania, Philadelphia, PA USA Background: Yeast of the genus Malassezia (formerly Pityrosporum) are lipophilic, non-mycelial, unipolar fungi that occur as commensal organisms on the skin of vertebrates. The two originally described species, M. pachydermatis and M. furfur, have been studied extensively as animal and human opportunistic pathogens, respectively. The now well-established association between M. pachydermatis and canine and feline dermatoses requires a working knowledge of the host/pathogen relationship by all veterinarians, but especially by veterinary dermatologists.1-4 Microbiology/Ecology: The genus Malassezia is now described to consist of seven lipid-dependent (M. furfur, M. sympodialis, M. globosa, M. obtusa, M. restricta, M. sloofiae, M equi) and one non-lipid-dependent species (M. pachydermatis).5,6 The latter, while not exhibiting an absolute requirement for lipid, is still enhanced by the addition of lipid substrates to the culture media. Lipophilic organisms exhibit the unique capability of utilizing lipid as a source of carbon. Malassezia yeasts are characterized by a thick, multilayered cell wall and the production of blastoconidia by repetitive monopolar (or sympodial) budding. This gives them the appearance of unshelled peanuts. M. pachydermatis is easily cultured from the non-inflamed skin of normal dogs but is quite difficult to demonstrate by cytological techniques (direct impression smear, cotton-tip swab, dry skin scrapings) of these same normal dogs.7 The yeast has also been localized to the distal hair shaft, where it may occur as a commensal, but its presence in the hair follicle infundibulum is rare.8 The yeast is best cultured at 37oC on lipid-enhanced Saubaraud’s dextrose/glucose media at 5% CO2, although microaerophilic conditions are not mandatory.9 Optimum growth is typically achieved by 72 hours, when individual colonies can be counted (prior to confluence). Techniques to obtain culture samples will vary according to purpose. For quantitative cultures, the tape-strip method, detergent scrub method, or contact plate method can be applied.7,10,11 These allow estimation of the number of colony-forming organism per unit of skin surface area. A sterile swab of the skin surface or ear canal exudates is also quite successful in isolating the organism. Since the yeast is a commensal on normal skin, a positive culture result cannot necessarily be equated with “infection”. The genus Malassezia can be speciated by either phenotypic and biochemical characteristics12, or by molecular mechanisms.13 Such laboratory tests are germane to the epidemiological study of yeast species and strains, especially in zoonotic outbreaks. In regards to zoonosis, M. pachydermatis is known to cause life-threatening fungemia in immunocompromised human infants and adults, and the point source of some infections have been traced to pet-owning health care workers.14,15 A large epidemiological study of normal dogs, atopic dogs with Malassezia dermatitis (MD) and their respective owners is currently being conducted by the author. Paired isolates from dogs and their human companions will be characterized by pulsed-field gel electrophoresis (“genetic fingerprinting”) to search for concordance of genetic identity. Even at the sub-species level, various strains are becoming recognized that could potentially behave in clinically distinct manners.16,17a Clinical manifestations of Malassezia overgrowth: While isolated from species as diverse as the rhinoceros and ferret,17b clinical disease manifestations have been studied in relatively few species. In dogs, cats, and human beings, Malassezia yeast contribute to the pathogenesis of several disease states, including seborrheic dermatitis, atopic dermatitis (AD), endocrine/metabolic diseases, and disorders of cornification. Occurrence of several Malassezia spp. from normal horses and domestic ruminants (cattle, sheep, and goats) has been reported, and lipid-dependent species were isolated more frequently (42%) than M. pachydermatis (3%).18 Occurrence in the external ear canals of normal swine is also known, and a single strain was shown to have colonized a herd of pigs on one isolated farm.19 In dogs, the role of M. pachydermatis in the atopic dermatitis phenotype has been well described clinically and to some degree, immunologically (see below). The inflamed skin and ear canals of dogs with AD often harbor increased numbers of yeast (compared to the skin of normal dogs), and specific antifungal therapy will ameliorate a large portion of the pruritus experienced by many of these dogs. Malassezia overgrowth is also associated with primary (idiopathic) seborrhea of dogs (especially in Basset hounds, Cocker spaniels, Dachshunds, and West Highland White terriers).2,3,20 A correlation with recent antibiotic treatment has also be documented.2 M. pachydermatis is commonly associated with otitis externa. Protein profiling of M. pachydermatis isolates from dogs has shown that there is generally no difference between strains of epidermal versus otic origin.21 There appears to be an increased incidence of Malassezia overgrowth in dogs with allergic and seborrheic otitis, endocrinopathies, and iatrogenic immunosuppression. However, it is also commonly seen in general practice occurring in otherwise normal dogs, but after swimming or bathing (ie, water trapping or “swimmer’s ear”). While rare, it has also been reported that M. pachydermatis can promote oral pathology (stomatitis, pharyngitis, tonsillitis).22 Occurrence in the oral cavity is considered to be normal,23 but oral cavity populations actually decreased in a group of seborrheic Basset hounds that were being treated with topical antifungal shampoos for Malassezia dermatitis.24 This suggests either that oral populations reflect direct transfer of cutaneous inhabitants to the oral cavity during licking, or that transfer of the antifungal from the hair coat to the oral cavity was therapeutic. While a definitive relationship between Malassezia yeast and atopic dermatitis has not been described in cats, it has been reported to be associated with feline chin acne, otitis externa, and pruritic/inflammatory dermatoses.25,26a Certainly, it is a known commensal of feline skin.26b In a recent review of 550 feline skin biopsies, Malassezia spp. were most commonly associated with feline paraneoplastic alopecia and thymomaassociated dermatosis/erythema multiforme.27 All cats with histology consistent with these underlying systemic diseases had died within 8 weeks of skin biopsy sampling. In contrast to a prior report,28 there were no biopsy samples in this series in which the yeast were associated with an inflammatory reaction pattern typical of feline allergic skin disease. As this report was a retrospective study of archived biopsy specimens, it did not evaluate the cytological status of the same cats. Still, it is recommended that cats with Malassezia dermatitis be evaluated for internal/systemic diseases, especially when the clinical picture is not suggestive of allergic dermatitis. While anecdotal reports have suggested a role for Malassezia on avian skin (especially in association with feather picking in Psittacine birds), a pilot study which evaluated feather follicles and feather pulp cytologically, histologically, and by culture failed to reveal any yeast.29 A larger scale study in which normal and picking Psittacines are sampled by tape-strip cytology and tape-strip quantitative culture techniques is currently under way within the author’s clinical group at the University of Pennsylvania. Pathogen-dependent immunological factors: In dogs, as in human beings, Malassezia yeast are known to produce allergens which, upon percutaneous absorption, contribute to the inflammatory reaction in the skin via a Type-1 hypersensitivity response (see host immunological responses below). The yeast are also capable of fixing complement through the alternate pathway, which may result in inflammation via the production of anapylatoxins (C3a, C4a, C5a).30 This mechanism is a non-specific reaction and should be capable of occurring in any animal with yeast over-growth and compromised stratum corneum barrier function. Perhaps this is the case in non-atopic animals with dermatitis secondary to Malassezia overgrowth. Dermatologists commonly observe highly inflammatory Malassezia infections occurring in cases of zinc-responsive dermatosis, generic dog food dermatosis, cutaneous T-cell lymphoma, and canine Cushing’s disease in which allergic diseases are absent.a Studies of human keratinocytes, incubated with different Malassezia species, indicate that cytokine production is provoked by the yeast, and that different species induce heterogenous responses. Interestingly, the species Malassezia furfur, a normal commensal of human skin, did not induce inflammatory cytokines, while M. pachydermatis and other “non human” species did.31 Pathogen virulence factors: Several virulence factors also contribute to the ability of the yeast to survive and proliferate on the skin. Adherence to corneocytes is thought to play an important role in the colonization and infection of the skin by the yeast. It is known that M. pachydermatis is capable of adhering to canine corneocytes via trypsinsensitive proteins or glycoproteins and mannosyl-bearing carbohydrate ligands on yeast cell walls.32,33 Knowing the specific adherence factors might allow intervention by use of ligand inhibitors. However, marked variability between yeast strains may limit identification of a universal inhibitor.33 In otic infections, adherence to corneocytes appears to be mediated through lipid ligands rather than carbohydrate moieties.34 In human skin, adherence of M. furfur is increased by elevated skin temperature (as would be the case with inflammatory dermatoses), and is not hindered by concurrent Staphylococcal colonization.35 Malassezia yeast are also capable of hydrolyzing lipids to free fatty acids in the sebum film. FFA’s are inhibitory to other microorganisms and therefore may help protect the yeast from competition.36 Production of proteinase, chondroiton-sulphatase, phospholipase, and hyaluronidase by M. pachydermatis isolates from dogs37 may serve as a ACVD/AAVD roundtable on Malassezia dermatitis; 1998, San Antonio, TX mediators of keratin invasion or (as in the case of proteinase) mediate the sensation of pruritus which is provoked at free nerve endings in the skin. Although an initial report38 suggested that M. pachydermatis may promote epidermal hyperplasia (a well known histological feature of Malassezia dermatitis39), a recent study argues against this theory, as yeast culture supernatants and yeast cell extracts failed to stimulate cultured canine corneocytes.40 Host factors -- skin surface microclimate: In dogs, cats, and human beings, Malassezia yeast colonize the skin during the immediate perinatal period.41-43a In a canine study, yeast was present as early as 3 days after birth, colonizing the lips, nailbeds, and external ear canals of 22 Rottweiler puppies (39.4% of tape-strip samples). In a Devon Rex cattery in Western Australia, waxy paronychial exudates loaded with yeast were identified within several hours of birth in kittens. b In dogs and cats, it is apparent that alterations in the skin’s surface microclimate contribute to susceptibility to overgrowth of Malassezia yeast. The yeast colonizes moist areas of the skin and mucosa of normal dogs in higher numbers than in more densely haired areas.7 In human beings, increased M. furfur numbers are directly correlated with increased sebum film at the skin surface (i.e., head and neck).43b Increased M. pachydermatis numbers on seborrheic canine and feline skin is the veterinary homologue. The ear canals, which express a higher temperature and humidity than the skin, are a very favorable environment for yeast growth, and the lipid-rich cerumen is also supportive.44 In fact, the propensity for yeast to be the etiological agent (as opposed to bacteria) in otitis externa appears to depend more upon the fatty acid composition of the canal than the pinnal shape. Even though the incidence of otitis externa in general is significantly higher in dogs with pendulous pinnae than in those with erect pinnae, there is no statistical difference between these morphological types in the occurrence rate of yeast otitis specifically.45 It has been shown experimentally that the addition of sterile saline to the canine ear canal can result in Malassezia otitis without predisposing inflammation.46 Similarly, the author has noted a higher incidence of primary Malassezia otitis and pododermatitis (in otherwise normal dogs) living in a humid coastal climate than in dogs living in more arid and temperate climates. Host factors -- immunological responses: In human beings with atopic dermatitis, hypersensitivity to Malassezia furfur (formerly Pityrosporum ovale and P. orbiculare) has been confirmed by several independent groups, utilizing intradermal allergy testing47 as well as skin prick testing,48-51 the atopy patch test,49,52 and in-vitro demonstration of anti-Malassezia furfur IgE by ELISA and RAST techniques.48,53-58 Furthermore, the cellmediated immune response to M. furfur has also been investigated, where both the peripheral blood mononuclear cell (PBMC) response and the in-situ (dermal) lymphocyte response to yeast extracts have been characterized in-vitro in patients with AD.48,59-62 In addition, the cytokine profiles of the responding lymphocytes have been reported in some of these studies. Both the PBMC and in situ populations, when isolated from AD patients, show increased blastogenic responses. However, human beings with seborrheic dermatitis do not show an altered PBMC response to Malassezia furfur when compared to normal subjects.63 b Personal communication: Dr. Mandy Burrows, Murdoch University, Perth, W.A. The canine immune response has been characterized in a similar fashion, albeit in more limited studies. Type-1 hypersensitivity responses (wheal and flare) to M. pachydermatis have been demonstrated after intradermal injection.4,64,65 However, delayed reactions were absent in most atopic dogs.4,64 In seborrheic Basset hounds, which often show marked Malassezia overgrowth without an atopic constitution, immediate reactivity to M. pachydermatis extracts is not significant compared to normal Bassets. This lack of immediate hypersensitivity, along with the blunted cell-mediated response noted in seborrheic Bassets (see below) may indicate an overtly different pathomechanism for MD associated with seborrheic dermatitis.66 Atopy patch testing utilizing yeast extracts has not yet been reported in dogs. Recently, anti-Malassezia IgE and IgG has been described in a population of atopic dogs.67 Passive transfer of cutaneous anaphylaxis by the serum of atopic dogs with MD (performed in the author’s laboratory) confirms that canine anti-Malassezia IgE is pathogenic in-vivo.68 Another group has characterized several major allergens of M. pachydermatis recognized by canine serum (via Western Blot analysis).69 A major allergen is an allergenic epitope recognized by at least 50% of an allergic population. Currently, 9 allergens of M furfur recognized by IgE from the sera of atopic humans have been characterized.70-73 The PBMC responses of normal dogs, atopic dogs with MD, atopic dogs with Malassezia otitis, and atopic dogs free of yeast infections have been compared. Atopic dogs with MD had an increased lymphocyte blastogenic response to crude M. pachydermatis extract as compared with clinically normal dogs and dogs with Malassezia otitis. However, atopic control dogs did not differ significantly in their responses when compared with the responses of dogs with MD or Malassezia otitis.74 These atopic dogs with MD also had a significantly increased CD4:CD8 ratio versus normal dogs, while atopic dogs without MD were not different from normal dogs.74 The PBMC response of atopics with MD contrasts to seborrheic Basset hounds with high M. pachydermatis counts on the skin: these dogs had significantly lower PBMC reactivity to M. pachydermatis extract than did clinically normal Basset hounds, suggesting an impaired cell-mediated immune response to the yeast in seborrheic dermatitis.75 These findings, considered in parallel, support a role for T-cell hyper-responsiveness to M. pachydermatis as part of the atopic paradigm in dogs. One odd caveat, mentioned in the study of PBMC response by atopic dogs, occurred in the Malassezia otitis group. The decreased PBMC activity to M. pachydermatis extracts in the otitis group (vs. atopic controls and atopics with MD) may suggest that the waxy microenvironment of the external ear canal provides a protective effect against T-cell/antigen interaction.74 A role for superantigens in canine MD has also been hypothesized. Superantigens are microbial products capable of binding a large repertoire of T-cell receptors that share common V regions without regard for other binding determinants. This allows activation of as much as 5-30% of the entire T-cell population.76 A role for Malassezia superantigens has now been ruled out in human atopic dermatitis.77 Similar studies are planned for canine T-cells in the author’s laboratory. Future therapies: For the time being, the clinical manifestations of Malassezia dermatitis must be dealt with using topical and systemic antifungal agents.26,78 It is the author’s hope that immunotherapy may palliate the hyper-responsiveness of atopics to Malassezia allergens. Such studies, if done properly, will require double-masked, placebo-controlled clinical trials that last a minimum of 12 to 18 months. It is already known that M. furfur and M. pachydermatis express some of the same major allergens (for human beings) in common.79 If it is found that allergic dogs and humans recognize the same common allergens of Malassezia sp. yeast, recombinant allergens would be the purest products for utilization in IDT and immunotherapy protocols. For the immediate future, Greer Laboratories has recently introduced an M. pachydermatis allergen for IDT and immunotherapy. It will be necessary to characterize the host immune response to the extract itself, as well as to the major M. pachydermatis allergens, whether or not this commercial extract is clinically useful as an immunotherapeutic. REFERENCES 1. Mason KV, Evans AG. Dermatitis associated with Malassezia pachydermatis in 11 dogs. J Am Animal Hosp Assoc 1991;27:13-27. 2. Plant JD, Rosencrantz W, Griffin CE. Factors associated with and prevalence of high Malassezia pachydermatis numbers on dog skin. J AmVetMedAssoc 1992;201:879-82. 3. Bond R, Ferguson EA, Curtis CF, et al. Factors associated with elevated cutaneous Malassezia pachydermatis populations in dogs with pruritic skin disease. J Sm An Pract 1996;37:103-7. 4. Morris DO, Olivier NB, Rosser EJ. Type-1 hypersensitivity reactions to Malassezia pachydermatis extracts in atopic dogs. Am J Vet Res 1998;59:836-841. 5. Gueho E, Midgley G, Guillot J. The genus Malassezia with description of four new species. Antonie Van Leeuwenhoek 1996;69:337-55. 6. Nell A, James SA, Bond CJ, et al. Identification and distribution of a novel Malassezia species yeast on normal equine skin. Vet Record 2002;150:395-8. 7. Kennis RA, Rosser EJ Jr, Olivier NB, et al. Quantity and distribution of Malassezia organisms on the skin of clinically normal dogs. J Am Vet Med Assoc 1996;208:104851. 8. Bond R, Lamport AI, Lloyd DH. Colonisation status of Malassezia pachydermatis on the hair and in the hair follicles of healthy beagle dogs. Res Vet Sci 2000;68:291-3. 9. Blanco JL, Guedeja-Marron J, Blanco I, Garcia ME. Optimum incubation conditions for the isolation of yeasts from canine otitis externa. J Vet Med B 2000;47:599-605. 10. Bond R, Lloyd DH. Evaluation of a detergent scrub technique for the quantitative culture of Malassezia pachydermatis from canine skin. Res Vet Science 1995;58:133-137. 11. Bond R, Collin WS, Lloyd DH. Use of contact plates for the quantitative culture of Malassezia pachydermatis from canine skin. J Sm An Pract 1994;35:68-72. 12. Guillot J, Gueho E, Lesourd M, et al. Identification of Malassezia species: a practical approach. J Mycol Med 1996;6:103-110. 13. Senczek D, Siesnop U, Bohm KH. Characterization of Malassezia species by means of phenotypic characteristics and dectection of electrophorectic karyotypes by pulsed-field gel electrophoresis (PFGE). Mycoses 1999;42:409-414. 14. Chang HJ, Miller HL, Watkins N. An epidemic of Malassezia pachydermatis in an intensive care nursery associated with colonization of health care workers’ pet dogs. N Engl J Med 1998;338:706-711. 15. Chryssanthou E, Broberger U, Petrini B. Malassezia pachydermatis fungaemia in a neonatal intensive care unit. Acta Paediatr 2001;90:323-7. 16. Aizawa T, Kano R, Nakamura Y, et al. Molecular heterogeneity in clinical isolates of Malassezia pachydermatis from dogs. Vet Micro 1999;70:67-75. 17a. Midreuil F, Guillot J, Gueho E, et al. Genetic diversity in the yeast species Malassezia pachydermatis analysed by mutilocus enzyme electrophoresis. Int J Syst Bacteriol 1999;49:1287-94. 17b. Guillot J, Chermette R, Gueho E. Prevalence of the genus Malassezia in the mammalia. J Mycol Med 1994;4:72-79. 18. Crespo MJ, Abarca ML, Cabanes FJ. Occurrence of Malassezia spp. in horses and domestic ruminants. Mycoses 2002;45:333-7. 19. Pinter L, Anthony RM, Glumac N, Hajsig D, et al. Apparent cross-infection with a single strain of Malassezia pachydermatis on a pig farm. Acta Veterinaria Hungarica 2002;50:151-6. 20. Bond R, Lloyd DH. Skin and mucosal populations of Malassezia pachydermatis in healthy and seborrheic Basset Hounds. Vet Dermatol 1997;8:101-6. 21. Coutinho SD, de Souza T, Paula CR. Protein profiles of Malassezia pachydermatis isolated from dogs. Mycopathologia 1997;139:129-35. 22. Printer L, Noble NC. Stomatitis, pharyngitis, and tonsillitis caused by Malassezia pachydermatis in a dog. Vet Dermatol 1999;9:257-60. 23. Bond R, Saijonmaa-Koulumies LEM, Lloyd DH. Population sizes and frequency of Malassezia pachydermatis at skin and mucosal sites on healthy dogs. J Sm Anim Pract 1995;36:147-50. 24. Bond R, Lloyd DH. Effect of topical therapy of Malassezia pachydermatisassociated seborrheic dermatitis on oral carriage of M. pachydermatis. Vet Record 1998;142:725-6. 25. Mason KV. Malassezia pachydermatis-associated dermatitis. In August JR (ed): Consultations in Feline Internal Medicine 3. Philadelphia, WB Saunders, 1997;221-3. 26a. Morris DO. Malassezia dermatitis and otitis. In: Campbell KA (ed): Veterinary Clinics of North America: Small Animal Practice. Philadelphia: W.B. Saunders Co., 1999;1303-10. 26b. Bensignor E, Weill FX, Couprie B. Population sizes and frequency of isolation of Malassezia yeasts from health pet cats. J Mycol Med 1999;9:158-61. 27. Mauldin EA, Morris DO, Goldschmidt MK. A retrospective study: the presence of Malassezia in feline skin biopsies. Vet Dermatol 2002; in press. 28. Scott, D.W. Bacteria and yeast on the surface and within non-inflamed hair follicles of skin biopsies from cats with non-neoplastic dermatoses. The Cornell Veterinarian 1992; 82: 371-377. 29. Morris DO, Peikes H, Mauldin EA, et al. A cytological, histological, and cultural study of the feather pulp and follicles of feather-picking psittacines: a preliminary report. In: Proceedings of the 16th meeting of the ACVD/AAVD, Norfolk, VA, USA; 2001. 30. Belew PW, Rosenberg EW, Jennings BR. Activation of the alternative pathway of complement by Malassezia ovalis (Pityrosporon ovale). Mycopathologica 1980;70:187-91. 31. Watanabe S, Kano R, Sato H, et al. The effects of Malassezia yeasts on cytokine production by human keratinocytes. J Invest Dermatol 2001;116:769-73. 32. Bond R, Lloyd DH. Factors affecting the adherence of Malassezia pachydermatis to canine corneocytes in vitro. Vet Dermatol 1996;7:49-56. 33. Bond R, Lloyd DH. Studies on the role of carbohydrates in the adherence of Malassezia pachydermatis to canine corneocytes in vitro. Vet Dermatol1998;9:105-9. 34. Masuda A, Sukegawa T, Hiroyuki T, Miyamoto T, et al. Attachment of Malassezia pachydermatis to the ear dermal cells in canine otitis externa. J Vet Med Sci 2001;63:667-9. 35. Faergemann J, Aly R, Maibach HI. Adherence of Pityrosporum orbiculare to human stratum corneum cells. Arch Dermatol Res 1993;275:246-50. 36. Mason IS, Mason KV, Lloyd DH. A review of the biology of canine skin with respect to the commensals Staphylococcus intermedius, Demodex canis and Malassezia pachydermatis. Vet Dermatol 1996;7:119-132. 37. Coutinho SD, Paula CR. Proteinase, phopholipase, hyaluronidase, and chondroitinsulphatase production by M. pachydermatis. Medical mycology 2000;38:73-6. 38. von Tscharner C, Wyder M, Busato A, et al. Proliferation characteristics of canine keratinocyte cultures infected with Malassezia pachydermatis. In: 15th Proceedings of the AAVD/ACVD; Hawaii, 1999:107-8. 39. Mauldin EA, Scott DW, Miller WH, et al. Malassezia dermatitis in the dog: a restrospective histopathological and immunopathological study of 86 cases (19901995). Vet Dermatol 1997;8:191-202. 40. Chen TA, Halliwell REW, Hill PB. Failure of extracts from Malassezia pachydermatis to stimulate canine keratinocyte proliferation in vitro. Vet Dermatol 2002;13:323-9. 41. Wagner R, Schadler S. Qualitative study of Malassezia species colonisation in young puppies. Vet Record 2000 ;147:192-194. 42. Robersts, S. Pityrosporum orbiculare : incidence and distribution on clinically normal skin. Br J Dermatol 1969;81:264-9. 43a. Bernier V, Weill FX, Hirigoyen V, et al. Skin colonization by Malassezia species in neonates. Arch Dermatol 2002 ;138 :215-18. 43b. Heng MCY, Henderson CL, Barker DC, et al. Correlation of Pityrosporum ovale density with clinical severity of seborrheic dermatitis as assessed by a simplified technique. J Am Acad Dermatol 1990;23:82-6. 44. Gabal MA. Preliminary studies on the mechanism of infection and characterization of Malassezia pachydermatis in association with canine otitis externa. Mycopathologia 1988;104:93-8. 45. Masuda A, Sukegawa T, Mizumoto N, Tani H. Study of lipid in the ear canal in canine otitis externa with Malassezia pachydermatis. J Vet Med Sci 2000;62:117782. 46. Uchida Y, Mizutani M, Kubo T, et al. Otitis externa induced with Malassezia pachydermatis in dogs and the efficacy of pimaricin. J Vet Med Sci1992;54:611-4. 47. Young E, Koers WJ, Berrens L. Intracutaneous tests with Pityrosporon extracts in atopic dermatitis. Acta Derm Venereol (Stockh) 1989;144(suppl):122-124. 48. Nordvall SL, Johansson SIV. IgE antibodies to Pityrosporum orbiculare in children with atopic disease. Acta Paediatr Scand 1990;79:343-348. 49. Rokugo M, Tagami H, Yasuko U. Contact sensitivity to Pityrosporum ovale in patients with atopic dermatitis. Arch Dermatol 1990;126:627-632. 50. Kieffer M, Bergbrant IM, Faergemann J. Immune reactions to Pityrosporum ovale in adult patients with atopic and seborrheic dermatitis. J Am Acad Dermatol 1990;22:739-742. 51. Devos SA, van der Valk PG. The relevance of skin prick tests for Pityrosporum ovale in patients with head and neck dermatitis. Allergy 2000;55:1056-1058. 52. Linder M, Tengvall A, Johannson C, et al. Positive atopy patch test reactions to Pityrosporum orbiculare in atopic dermatitis patients. Clin Exp Allergy 2000;30:122131. 53. Johannson S, Faergemann J. Enzyme-linked immunosorbent assay (ELISA) for detection of antibodies against Pityrosporum orbiculare. J Med Vet Mycol 1990;28:257-260. 54. Wessels MW, Doekes G, van Ieperen-van Dijk. IgE antibodies to Pityrosporum ovale in atopic dermatitis. Br J Dermatol 1991;125:227-232. 55. Doekes G, vanleperen-vanDijk AG. Allergens of Pityrosporum ovale and Candida albicans I. Cross-reactivity of IgE-binding components. Allergy 1993:48:394-400. 56. Kawano S, Nakagawa H. The correlation between the levels of anti-Malassezia furfur IgE antibodies and severities of face and neck dermatitis of patients with atopic dermatitis. Ja J Allergol 1995;44:128-133. 57. Lintu P, Savolainen J, Kalimo K. IgE antibodies to protein and mannan antigens of Pityrosporum ovale in atopic dermatitis patients. Clin Exp Allergy 1997;27:87-95. 58. Scalabrin DM, Bavbek S, Perzanowski MS, et al. Use of specific IgE in assessing the relevance of fungal and dust mite allergens to atopic dermatitis: a comparison with asthmatic and nonasthmatic control subjects. J Allergy Clin Immunol 1999;104:12731279. 59. Gruseck E, Neuber K, Kroeger S, et al. Lymphocyte proliferation, IgE-synthesis, and cytokine secretion (IL-2, IL-2R, IL-4, IL-10) induced by Pityrosporum ovale in patients with atopic eczema. J Allergy Clin Immunol 1994;93:221. 60. Linder MT, Johansson C, Zargari A, et al. Detection of Pityrosporum orbiculare reactive T cells from skin and blood in atopic dermatitis and characterization of their cytokine profiles. Clin Exp Allergy 1996;26:1286-1297. 61. Linder MT, Johansson C, Bengtsson A, et al. Pityrosporum orbiculare-Reactive Tcell lines in atopic dermatitis patients and healthy individuals. Scand J Immunol 1998;47:152-158. 62. Savolainen J, Lintu P, Kosonen J, et al. Pityrosporum and Candida specific and nonspecific humoral, cellular, and cytokine responses in atopic dermatitis patients. Clin Exp Allergy 2001;31:125-134. 63. Parry ME, Sharpe GR. Seborrhoeic dermatitis is not caused by an altered immune response to Malassezia yeast. Br J Derm 1998;139:254-3. 64. Kumar A, Singh K, Sharma A, Kumar S. Immediate hypersensitivity reactions to Malassezia pachydermatis extracts in dogs. J Immunol Immunopathol 2001;3:17-21. 65. Bond R, Curtis CF, Hendricks A, Ferguson EA, Lloyd D. Intradermal test reactivity to Malassezia pachydermatis in atopic dogs. Vet Record 2002;150:448-9. 66. Bond R, Patterson-Kane C, Lloyd DH. Intradermal test reactivity to Malassezia pachydermatis in healthy basset hounds and basset hounds with Malassezia dermatitis. Vet Record 2002;151:105-9. 67. Nuttal TJ, Halliwell REW. Serum antibodies to Malassezia yeasts in canine atopic dermatitis. Vet Dermatol 2001;12:327-32. 68. Morris DO, DeBoer DJ. Evaluation of serum obtained from atopic dogs with dermatitis attributable to Malassezia pachydermatis for passive transfer of immediate hypersensitivity to that organism. Am J Vet Res 2003;64:262-6. 69. Chen TA, Halliwell REW, Hill PB. IgG responses to Malassezia pachydermatis antigens in atopic and normal dogs. Vet Dermatol 2000;11:13(suppl). 70. Schmidt M, Zargari A, Holt P, et al. The complete cDNA sequence and expression of the first major allergenic protein of Malassezia furfur, Mal f 1. Eur J Biochem 1997;246:181-185. 71. Yasueda H, Hashida-Okado T, Saito A, et al. Identification and cloning of two novel allergens from the lipophilic yeast, Malassezia furfur. Biochem Biophys Res Comm 1998;248:240-244. 72. Onishi Y, Kuroda M, Yasueda H, et al. Two-dimensional electrophoresis of Malassezia allergens for atopic dermatitis and isolation of Mal f 4 homologs with mitochondrial malate dehydrogenase. Eur J Biochem 1999;261:148-154. 73. Lindborg M, Magnusson CGM, Zargari A, et al. Selective cloning of allergens from the skin colonizing yeast Malassezia furfur by phage surface display technology. J Invest Dermatol 1999;113;156-161. 74. Morris DO, Clayton DJ, Drobatz DJ, Felsburg PJ. Response to Malassezia pachydermatis by peripheral blood mononuclear cells from clinically normal and atopic dogs. Am J Vet Res 2002;63:358-62. 75. Bond R, Elwood CM, Littler RM, et al. Humoral and cell-mediated responses to Malassezia pachydermatis in healthy dogs and dogs with Malassezia dermatitis. Vet Record 1998;143:381-384. 76. Manders SM. Toxin-mediated streptococcal and staphylococcal disease. J Am Acad Dermatol 1998;39:383-398. 77. Johansson C, Jeddi-Tehrani M, Grunewald J, et al. Peripheral blood T-cell receptor beta-chain V-repertoire in atopic dermatitis patients after in vitro exposure to Pityrosporum orbiculare extract. Scand J Immunol 1999;49:293-301. 78. Muse R. Malassezia dermatitis. In Kirk’s Current Veterinary Therapy XIII, Bonagura JD, ed. Philadelphia, WB Saunders Co. 2000, pp. 574-7. 79. Zargari A, Emilson A, Hallden G., et al. Cell surface expression of two major yeast allergens in the Pityrosporum genus. Clin Exp Allergy 1997;27:584-92.