VISITING NURSE ASSOCIATION - For Medical Professionals
advertisement

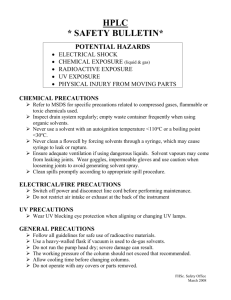
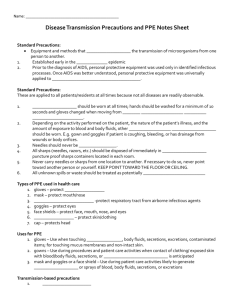
AURORA VISITING NURSE ASSOCIATION OF WISCONSIN FIELD SERVICE POLICIES Policy No.: Effective: Revisions: 406 11/91 11/91, 12/94, 12/97, 9/01, 11/04, 9/06, 9/07, 10/07, 8/09, 12/10 Last Review: 9/05 Intended Users: All field staff INFECTION CONTROL RESPONSIBILITIES OF FIELD STAFF I. Policy The Aurora Visiting Nurse Association of Wisconsin (VNA) field staff have the responsibility to prevent infections in the care/service of patients. Staff should follow the infection control procedures outlined here and in nursing/clinical procedure manuals to significantly reduce the potential for the transmission and development of preventable infections in the home. II. Purpose To prevent the development of organization acquired infection in patients. III. Procedure A. Good hand hygiene is the single most important practice for preventing infection. Hands are to be cleansed prior to providing care, between procedures, and after the completion of care. Hands must always be washed with soap and water when visibly soiled. Keep nails medium/short and well groomed. Jewelry and rings should be conservative and kept to a minimum. HR Policy #12 (Appearance Policy) prohibits artificial nails or extenders for direct care staff. Natural nail tips must be kept less than ¼ inch long. Nail polish must be a conservative color, intact and not chipped. (See HR #12 for more detail.) B. The home environment should be assessed for potential sources of infection. Always consider the floor to be contaminated; clean, disinfect, sterilize, or discard any items that fall onto the floor. Work surfaces and patient care areas should be kept clean and clear of clutter. Avoid raising dust, which carries organisms; use vacuum cleaners, and dampened/treated cloths to dust. Keep linens and used supplies and equipment away from your uniform/clothing. Do not shake linens. Patients who have problems with rodents and/or insects should be advised of resources to help resolve the problem. Social Service referral may be appropriate in instances of noncompliance or significant infestation. C. Patient food preparation should be such that it is not a contributing factor to infections. Always cleanse hands before handling food. D. Patients with poor personal hygiene should be taught the importance of personal hygiene as it relates to the development of infections. Education and any noncompliance should be documented. FS 406: Infection Control Responsibilities of Field Staff Page 1 of 4 E. Clinical field staff should adhere to bag technique per VNA procedure. It is expected that all field staff will bring a bag into the home for all visits unless there is infestation, or it is medically contraindicated, e.g. a drug resistant organism. Isolation precautions should be discontinued per CDC guidelines for the respective organism/infectious disease. F. Those field staff who use a laptop computer should make sure it is kept on a clean surface during the visit and: After touching the patient, perform hand hygiene before using the laptop, OR Wipe down the “high touch” surfaces, i.e., the keyboard, at the end of the visit using a manufacturer-approved cleaner G. Patient health care solutions may only be used according to these guidelines: 1. Do not use any solution past its expiration date, even if unopened. 2. Original solutions of alcohol, hydrogen peroxide, and betadine may be used up to one month after opening. Date bottle when opened; if not dated, must be discarded. 3. Sterile irrigating solutions, e.g. sterile water or sterile saline, may be used up to one week after opening. Date bottle when opened; if not dated, must be discarded. 4. Pharmacy mixed solutions, e.g. Dakins or Domeboro’s, may be used up until the expiration date printed on the label. 5. Employee mixed solutions, e.g. 1:10 bleach water or ½ NS: ½H2O2, may be used up to 24 hours. Label and date container when mixed. H. All staff will adhere to Standard Precautions at all times. Treat all bodily fluids as if potentially infectious. (See clinical procedure manual.) In addition, double gloving may be followed when handling sharps and working with known HIV positive patients. I. J. To alert delivery staff of the need to observe precautions (contact, respiratory, etc.) in the home, agency defined codes will be entered onto the delivery ticket (Dezine and CHIP systems). These codes are as follows: DRO: Drug Resistant Organism - contact precautions CD: C. Diff positive – special hand washing precautions and equipment cleaning precautions in addition to contact precautions. RD: “Red Dot” - blood and body fluid precautions RI: Respiratory Isolation - respiratory precautions TP: Transplant Precautions - reverse precautions. The following precautions will be taken whenever there is knowledge that the patient has a drug resistant organism (DRO), or is either suspected of, or diagnosed with Creutzfeldt-Jakob Disease, or Gertsmann-Straussler-Scheinter Syndrome. 1. Do not take your visit bag or any reusable equipment or supplies into the home. 2. The admitting professional is responsible for securing a Drug Resistant Organism Admission Kit and any disposable medical supplies to be taken to the home. Contents of the kit remain in the home. 3. Cleanse hands with antibacterial hand gel or soap and water. Practice hand hygiene upon entering the home, after gloves are removed, between procedures, and prior to exiting the home. Dry hands with paper towel to avoid cross-contamination. 4. Gloves and gowns are worn whenever treating a patient with a DRO who is incontinent of stool or urine; or whose wound exudate cannot be contained; or when contact with blood or body fluids is anticipated. Both are always worn when caring for a bed-bound patient. Gloves may be worn alone when doing environmental cleaning in the patient’s home. FS 406: Infection Control Responsibilities of Field Staff Page 2 of 4 5. The patient should be advised to clean and disinfect the toilet and/or sink that they personally use daily, IF they share this toilet/sink with others AND depending upon where their DRO has been cultured as positive. 6. Masks should be worn when in close proximity to the patient when there is a possibility that any body fluids will become aerosolized (i.e. coughing through a trach tube), or when a patient is known to be colonized with a DRO in the throat or lungs or infected with a DRO in the nares, throat, or lungs. 7. Linens soiled with blood or body fluids should be laundered separately; see Disinfection of Linen in the Home. 8. In the event of transfer from the VNA to another health care facility, notify the receiving staff of the patient’s actual or suspected DRO/diagnosis. K. Isolation Precaution - CONTACT 1. Contact Precautions are used when germs can be spread from touching the patient or things in their environment. 2. Examples: a. Patients with DRO such as MRSA or VRE b. Uncontained drainage from wounds c. Diarrhea – NOTE: for patients with clostridium difficile (c-diff) special hand washing guidelines apply: first wash hands with liquid soap and water, then when hands are dry, use approved, alcohol-based hand gel. In addition, all surface cleaning (i.e., equipment) must be done with a 1:10 bleach solution. d. Disposable gloves and gowns are worn for Contact Precautions e. Put on Personal Protective Equipment (PPE) in this order: i. Disposable gown (tie at neck and waist) ii. Gloves (should cover the cuffs of the gown) f. Remove PPE in this order: i. Before leaving the room/patient care area/home ii. Remove gloves and discard iii. Remove gown – untie back of gown and remove, do not touch outside front of gown – double bag. iv. Use alcohol hand gel to clean hands or wash with soap and water. L. Isolation Precaution – DROPLET 1. Droplet Precautions are used when the germs are spread by large droplets from the respiratory tract that travel only about three feet. This infection can be spread by droplets that occur with sneezing or coughing 2. Examples: a. Meningitis b. Some Pneumonias c. Influenza 3. Masks are worn or Droplet Precautions a. Put on PPE (mask) b. Remove PPE in this order: i. Before leaving the room ii. Remove mask in room and discard iii. Use alcohol hand gel to clean hands or wash with soap and water c. Then exit the patient environment M. Isolation Precautions – AIRBORNE 1. Airborne precautions are used when the germs are spread long distances on tiny particles in the air 2. Examples: FS 406: Infection Control Responsibilities of Field Staff Page 3 of 4 a. b. c. d. e. Measles Chicken Pox Active or Suspended Tuberculosis (TB) Disseminated Shingles (herpes zoster) SARS 3. An N95 Respirator Mask or a PAPR (Powered Air Purifying Respirator) is worn for Airborne Precautions. a. Put on PPE (N95 respirator mask or PAPR) Note: N95 mask must be fit tested for each employee b. Remove PPE in this order: i. Before leaving the patient room ii. Use alcohol hand gel to clean hands or wash with liquid soap and water c. When leaving the room: i. Exit the room and close the door ii. Remove and discard N95 respirator mask or PAPR iii. Use alcohol hand gel to clean hands or wash with liquid soap and water. NOTE: For suspected or confirmed Novel H1N1 Influenza: a. Contact Precautions PLUS N95 mask b. Airborne Precautions (negative pressure not required; sign is for N95 mask) c. Eye protection (goggles or faceshield) at all times (Note: fogging can occur while wearing goggles), must be cleaned with bleach wipes if reused. Faceshield is worn over the N95 mask d. Door signage (At AZFH) that can be printed from the H1N1 Resource Center. Door closed at all times Suspect Case: Isolation precautions until a negative result is finalized Confirmed Case: Consult with Infection Control prior to discontinuing isolation FS 406: Infection Control Responsibilities of Field Staff Page 4 of 4