ENTAll
advertisement
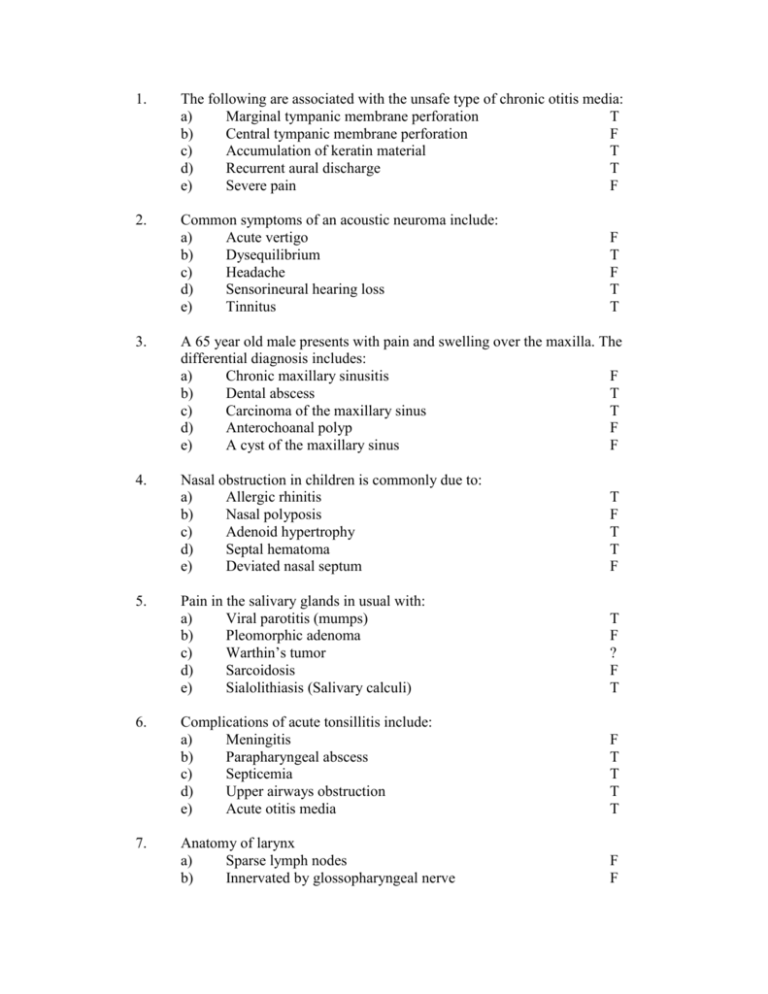
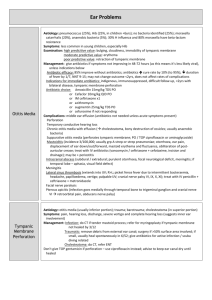
1. The following are associated with the unsafe type of chronic otitis media: a) Marginal tympanic membrane perforation T b) Central tympanic membrane perforation F c) Accumulation of keratin material T d) Recurrent aural discharge T e) Severe pain F 2. Common symptoms of an acoustic neuroma include: a) Acute vertigo b) Dysequilibrium c) Headache d) Sensorineural hearing loss e) Tinnitus F T F T T 3. A 65 year old male presents with pain and swelling over the maxilla. The differential diagnosis includes: a) Chronic maxillary sinusitis F b) Dental abscess T c) Carcinoma of the maxillary sinus T d) Anterochoanal polyp F e) A cyst of the maxillary sinus F 4. Nasal obstruction in children is commonly due to: a) Allergic rhinitis b) Nasal polyposis c) Adenoid hypertrophy d) Septal hematoma e) Deviated nasal septum T F T T F Pain in the salivary glands in usual with: a) Viral parotitis (mumps) b) Pleomorphic adenoma c) Warthin’s tumor d) Sarcoidosis e) Sialolithiasis (Salivary calculi) T F ? F T Complications of acute tonsillitis include: a) Meningitis b) Parapharyngeal abscess c) Septicemia d) Upper airways obstruction e) Acute otitis media F T T T T Anatomy of larynx a) Sparse lymph nodes b) Innervated by glossopharyngeal nerve F F 5. 6. 7. 8. Esophageal foreign bodies a) Are always visible on soft tissue xrays b) Are always associated with esophageal strictures c) Most often lodge in the lower esophagus d) Require rigid esophagoscopy for removal e) Commonly occur in edentulous patients F F F T T 9. Indicated whether the following statements on laryngeal anatomy are true or false a) The cricoid is the only complete cartilaginous ring T in the upper respiratory tract b) The hyoid is a laryngeal cartilage F c) The vocal cord has sparse lymphatic drainage T d) The thyroid notch indicates the level of the vocal cords T e) The arytenoid cartilage forms a boundary of the pyriform fossa T 10. Complications of tracheotomy include a) Surgical emphysema b) Pneumothorax c) Vocal cord paralysis d) Esophageal perforation e) Dislodgement of the tracheotomy tube T T F F T Gram negative organisms are commonly responsible for: a) Acute sinusitis b) Auricular perichondritis c) Peritonsillitis d) Chronic otitis media e) Neck space infection T T F T T The following cranial nerves may be involved in referred otalgia a) Vagus b) Abducens c) Glossopharyngeal d) Hypoglossal e) Trigeminal T F T F T Complications of cocaine anesthesia include a) Vasoconstriction b) Vasovagal reaction c) Cardiac arrhythmia d) Rebound vasodilation e) Respiratory failure T F T F F 11. 12. 13. 14. 15. 16. 17. 18. 19. Tracheostomy may be performed to a) Bypass laryngeal obstruction b) Facilitate positive pressure ventilation c) Remove tracheal foreign body d) Facilitate pulmonary toilet e) Manage pneumothorax Stridor in children a) Is commonly due to laryngomalacia b) May be caused by vocal cord polyp c) Demands that the patient have a laryngoscopy d) Mandates a tracheostomy e) Is not due to a lesion in the vocal cord if the child has a normal cry T T F T F T F F F T The following are features of peritonsillar abscess a) Trismus b) Dysphagia c) Meningitis d) Sleep apnea e) Cervical lymphadenopathy T T F F T The following are usually associated with chronic otitis media with effusion a) Purulent middle ear fluid b) Retracted tympanic membrane c) Otalgia d) Fluctuating hearing loss e) Perforated tympanic membrane T T F T F Menieres disease is characterized by a) Conductive hearing loss b) Tinnitus c) Episodic vertigo d) Recurrent otalgia e) Aural discharge F T T F F Unilateral purulent discharge may be due to a) Congenital choanal atresia b) Septal hematoma c) Nasal foreign body d) Allergic rhinitis e) Rhinitis medicamentosa T F T F F 20. 21. 22. 23. 24. 25. 26. Stridor can be caused by a) Bronchial asthma b) Vocal cord paralysis c) Consolidation F T F Calculi in the salivary glands a) Are more common in the submandibular than parotid b) Are always radioopaque c) Reflect an underlying sialectasis d) Are a feature of Sjogrens disease e) Always require surgical removal T F F F T Facial nerve paralysis may be associated with the following a) Head injury b) External auditory canal osteoma c) Acute otitis media d) Pleomorphic adenoma e) Acoustic schwannoma T F T T T Direct relations of maxillary sinus a) Hard palate b) Lamina paprycea c) Middle turbinate d) Optic nerve e) Orbit T F F F T Direct relations of the parotid gland a) Ramus of mandible b) Mastoid process c) Vagus nerve d) Internal jugular vein T F F F Contents of the posterior triangle a) Carotid sheath b) Accessory nerve c) Vagus nerve d) Lymph nodes e) Submandibular gland F T F T F Branches of the facial nerve include a) Parasympathetic to lacrimal gland b) Parasympathetic to parotid gland c) Sensory to stapedius d) Sensory to posterior 1/3 of tongue T F F F 27. 28. 29. 30. 31. 32. 33. Adenoid cystic carcinoma a) Occurs most commonly in salivary glands b) Presents as a painful swelling in the parotid gland c) Is prone to perineural extension d) Often occurs bilaterally T T T F Vestibuloneuritis a) Can occur in epidemic b) Causes momentary episodes of vertigo c) Often has association with tinnitus d) Can be preceded by viral illness e) Never associated with deafness T F F T T Globus pharyngeus a) Occurs commonly in females b) May be associated with anemia c) Indicates pathology in the oropharynx d) Can be associated with GORD e) Dysphagia T F F T F The cochlea a) Is situated in the part of the temporal bone b) Is sensorial damaged in longitudinal fractures of the temporal bone c) Contains perilymph d) Gives information regarding posture control Squamous cell carcinoma commonly occurs in a) Vocal cords b) Middle ears c) Nasopharynx Facial paralysis a) All type of malignant tumors in the parotid gland may cause facial paralysis b) Causes the affected side to be pulled down Acute retropharyngeal abscess a) Usually occurs in children b) The swelling is central c) The swelling is to one side of the midline d) The patient extends the head and opens the mouth to maintain an airway e) Does not obstruct respiration T F T F T F T T T T F T T F 34. 35. 36. 37. 38. 39. 40. Which of the following are presenting features of nasopharyngeal carcinoma a) Epistaxis b) Dysphagia c) Paraplegia d) Enlarged cervical lymph nodes e) Otalgia T F F T T The earliest signs of carcinoma of hypopharynx include a) Enlarged lymph node behind angle of the jaw b) Facial nerve paralysis c) Dysphagia d) Dyspnea e) Hoarseness F F T F F The tonsil appears enlarged on inspection. This may be due to a) Tonsillitis b) Tonsil carcinoma c) Lymphoma of tonsil d) Parotid tumor e) Amyloidosis T T T T F Polyps histopathology appearance a) Malignant neoplasia b) Benign neoplasia c) Granulation tissue d) Edematous pouches e) Fatty degeneration F F T T F Ethmoid sinuses have direct anatomical relation with a) Optic nerve b) Inferior turbinate c) Nasal process of maxillary bone d) Lamina capricus F F F F Bells palsy is associated with a) Herpes zoster virus b) Part of polyneuropathy c) Recurrence F F T Unilateral hearing loss may be caused by a) Presbycusis b) Otological drugs c) Mumps d) Acoustic neuromas F F T T 41. 42. 43. 44. 45. 46. 47. Submandibular gland a) Can be below hyoid bone b) Can go beyond angle of mandible c) Opens opposite lower canine d) Common place for neoplasm T F F F Trismus can be caused by a) TMJ b) Tonsillar carcinoma c) Peritonsillitis (quinsy) d) Nasopharyngeal carcinoma T T T T Nasopharyngeal carcinoma can cause a) Proptosis b) Ulcers of the palate c) Epistaxis d) Enlarged neck mass F F T T A 50 year old man with enlarged lymph nodes between digastric and jugulo-hyoid may be caused by: a) Old TB b) Chronic tonsillitis c) Nasopharyngeal carcinoma d) GI tumors T T T F Glandular fever features a) Cervical lymphadenopathy b) Hypersplenism c) Polyneuritis d) Pain T T F T Facial nerve paralysis may be caused by a) Cystadenolymphoma b) Acoustic schwannoma c) Pleomorphic adenoma d) Head trauma T T T T Sjogrens syndrome a) Painful swelling b) Predispose to lymphoma c) Dry eyes d) Presents with osteoarthritis e) Diagnosed with sublabial biopsy F T T F T 48. 49. 50. 51. 52. 53. 54. Longitudinal fractures of the temporal bone a) Hard to see on Xray b) Commonly cause facial nerve paralysis c) Cause inner ear damage d) Cause bloody ear discharge e) Cause conductive hearing loss T T F F T Positional vertigo a) Can have CNS causes b) Usually associated with inner ear problems c) Prolonged vomiting d) Head trauma T T T T Clinical features of maxillary sinus Carcinoma include a) Anosmia b) Diplopia c) Facial swelling d) Supraclavicular neck lymphadenopathy e) Epistaxis T T T F T SCC is common in a) Thyroid gland b) Middle ear c) Oropharynx d) Mouth e) Submandibular gland F F T T F Laryngotracheobronchitis a) Commonly occurs in >6 years old b) Always requires hospitalization c) Affects epiglottis F F F Cliical features indicative of complications of acute Otitis media a) Vertigo b) Tinnitus c) Severe otalgia d) Progressive hearing loss T T F T Temporal bone a) Cochlea is in petrous part b) Cochlea contains scala media c) Cochlea is commonly damaged in longitudinal fractures of temporal bone d) Cochlea involved in balance T T F F 55. 56. Carcinoma of the lip a) More often affects lower lip then upper b) Metastasizes early to internal jugular lymph nodes c) Affects men more often than women d) Has a poor prognosis if it occurs at the angle of the mouth e) Is best treated by surgical excision T F T T T Malignant disease of a) The tonsil most commonly arises in the lymphoid tissue b) The tongue can cause pain radiating to the ear c) The nasopharynx may present with deafness d) The floor of the mouth is most commonly an ulcerating SCC e) The buccal mucosa can arise in a patch of leukoplakia F F T T T 57. In acute mastoiditis a) Inspection from behind may reveal the pinna is pushed forward T b) Conductive deafness is present T c) Perceptive deafness is present F d) Moving pinna up and back is painful T e) Patient is a child T 58. Which of the following are true of the varieties of nasal sinusitis a) Frontal sinusitis is a disease of the aged b) Frontal sinusitis is a disease of the young c) Ethmoiditis is largely confined to infants and young children d) Maxillary sinusitis is found only before the 12th year 59. 60. 61. 62. In otosclerosis a) Deafness is commonly bilateral b) Tinnitus is common c) Tympanic membranes are normal d) Audiometry shows normal bone conduction but impaired air conduction Acute otitis media: a) commonly caused by hemophilus influenzae b) commonly associated with tinnitus c) commonly associated with vertigo Organisms commonly causing chronic otitis media include a) Gram positive b) Staph c) Haemophilus influenza Indications for myringotomy/tympanocentesis include: a) Neonates b) Failure of antibiotic treatment c) Intracranial complications F T T F T T T T T T F T T T F T T ENT answers explained: 1. Chronic otitis media arises because of late or ineffective treatment of acute otitis media, lowered resistance (malnutrition, anemia, etc) or upper airways sepsis. There are two types of chronic otitis media, being mucosal and bony (aka attico-antral disease). Both give rise to discharging ear, but the two can be differentiated on the basis of discharge type, complications, perforation location and location of disease. COM type Mucosal Bony Discharge mucoid scanty, foul-smelling but persistent Complications deafness granulations Aural polyps Cholesteotoma Perforation central (pars tensa) postero-superior (pase flaccida) Location . tubo-tympanic attico-antral Granulations and aural polyps are both made out of granulation tissue. Treatment of BONY disease involves regular aural toilet or suction toilet (removes small cholesteotoma). If cholesteotoma is present, mastoidectomy is needed Treatment of MUCOSAL disease requires frequent aural toilet. If the performation requires repair, a myringoplasty can be done. Earache and deafness can be present in both forms of the disease, although neither are as pronounced as in acute otitis media. 2. Acoustic neuromas (aka vestibular Schwannomas) are benign tumors of the superior vestibular nerve. They are usually unilateral except in neurofibromatosis-2 (Chromosome22) in which case bilateral vestibular Schwannomas may be present. Symptoms include: - EARLY signs are: - hearing loss (sensorineural) - imbalance - LATE signs are due to impingement on other structures and include: - loss of corneal sensation (impingement on CN V) - facial nerve palsy (CN VII) - Increased intracranial pressure ( headache, nausea, papilloedema) Since late signs would be rare, headache would be a rare symptom in acoustic neuroma. Since any form of deafness can cause tinnitus, acoustic neuromas cause tinnitus. 3. Chronic maxillary sinusitis usually has very few symptoms, but MAY include nasal obstruction, anosmia, nasal/postnasal mucopus discharge or cacosmia. There is not a visible mass although there may be a fluid level or opacity on radioimaging. While swelling of the cheek is rare in maxillary sinusitis, when it IS present, it is often dental of origin. Usually cheek swelling over the maxilla is due to carcinoma of the maxillary antrum. Antro-choanal polyps extend from maxillary antrum BACK through ostium, presenting as a smooth swelling in the nasopharynx. Treatment involves avulsion within nose. A cyst in the maxillary sinus would not be painful and would not expand onto the cheek. 4. Nasal obstruction in children can occur from: adenoid hypertrophy (adenoids begin atrophy at 7, gone by 16/17) unilateral choanal atresia (presents about age 5 with thick mucus) bilateral choanal atresia (presents at birth since newborns aren’t able to mouthbreath) foreign body in nose acute or chronic maxillary sinusitis allergic or non-allergic rhinitis - RARE causes include: septal hematoma (hemorage between 2 sheets perichondrium,after trauma) septal deviation (maybe due to injurytreat with SMR or reduction) nasal polyposis (RARE unless child has CF) 5. Pain in the salivary glands can arise from acute inflammation or stones. Malignancies are not characteristically painful. Parotitis can be caused by mumps or bacterial infection (Staph aureus, Strep pyogenes, Strep pneumoniae). It presents with a painful lump, usually of the parotid gland (rarely, the submandibular gland can be affected). Pleomorphic adenoma is a benign tumor that accounts for 90% of adult benign parotid tumors. They are painless slowly expanding lesions. Warthin’s tumor is also known as a cystic lymphoepithelial lesion. It is exclusive to the parotid gland and causes a cystic smooth swelling to the tail of the gland. Sarcoidosis rarely involves a salivary gland, causing a slowly expanding swelling. It is painless. Sialolithiasis (salivary calculi) are acutely painful, and characteristically more painful after eating. They can be expelled through the mouth, or superficially removed from the gland. All salivary calculi should be removed. 6. Complications of acute tonsillitis include: (remember acute tonsillitis looks like “CORN”) - Chest infection (pneumonia, etc) - Otitis media (acute) - Rheumatism (acute) - Nephropathy (IgA mediated) quinsy (PERItonsillar abscess); abscesses in the deep neck spaces and around the pharynx (parapharyngeal) may also occur. Obviously, as a focus of infection, vascular access may cause septicaemia, so septicaemia is a potential complication of acute tonsillitis. Moreover, one of the symptoms of a grossly enlarged tonsil is upper airway obstruction. Complications of acute otitis media include: - Abscess (cerebral, subdural, epidural) - Meningitis - Acute mastoiditis - Labyrinthitis - Thrombosis (of lateral sinus) - Facial nerve paralysis - Petrositis (don’t forget DeGagliano’s syndrome CN VI palsy 7. The muscles of the larynx are innervated by the vagus nerve’s recurrent laryngeal branch, except for the cricothyroids which are supplied by the vagus nerve’s superior laryngeal nerve. The larynx is well supplied with lymphatics though generally, tumors of the larynx tend to spread locally and only to lymphatics late. 8. The esophagus is composed of three narrowings which tend to be the most common sites for obstruction. The first site is at the junction between the top 1/3 and the middle 1/3 of the esophagus, where the skeletal muscle becomes smooth muscle. Here about 70% of obstructions are likely to take place. The next narrowing is where the aortic arch and carina cross the esophagus, where 15% of obstructions occur. The final narrowing is at the gastroesophageal junction, where another 15% of obstructions occur. Obstructions are rarely caused by esophageal strictures, although a stricture clearly increases the likelihood of an obstruction from occurring. Depending on what is causing the obstruction, the object may be radioopaque or radiolucent (fish or chicken bones, wood, plastic, most glass, and thin metal objects) and thus a negative Xray is considered inconclusive and thus, if symptoms of obstruction (dysphagia, vomiting, respiratory distress, hematemesis, perforation, etc) persist, an esophagoscopy is required. Given the edentulous commonly have dentures, and elderly commonly swallow their dentures, being edentulous can cause obstruction! The tonsillar area is a popular area for fish bones!! The vocal folds are at the level of the middle of the laryngeal prominence (“Adam’s apple”) which is made of the thyroid cartilage. 9. The laryngeal part of the pharynx extends from the superior part of the epiglottis to the inferior cricoid cartilage, where it is continuous with the esophagus. A small piriform fossa on each side of the laryngeal inlet is bounded medially by the aryepiglottic fold (includes aryepiglottic cartilage) and laterally by the thyroid cartilage and thyrohyoid membrane. There are several cartilaginous rings in the neck- the cricoid cartilaginous ring is complete while all others are incomplete (C-rings of trachea are all inferiorly incomplete). The laryngeal lymphatic drainage is delineated into superior and inferior drainage at the level of the vocal cords, but there are extensive anastomoses here. Superior drain into the superior deep cervical lymph nodes while inferior to the vocal cords drain into the inferior deep cervical lymph nodes. Curiously, however, the vocal cords themselves are devoid of lymphatic drainage. 10. Complications of tracheostomy include: Tracheostomy is to be performed by: 1. Transverse incision, halfway between cricoid cartilage and sternal notch 2. Identify and retract strap muscles 3. Incise thyroid isthmus 4. Incise 3rd of 4th C-ring of trachea If inserted too low pneumothorax or mediastinal emphysema If inserted too high perichondritis or subglottic stenosis (esp. if cricoid cartilage injured) After tube inserted complete or partial dislodgement Obstruction of tube (can be fatal) 11. Organisms that commonly cause: Condition Organisms Acute sinusitis Viral (RSV, influenza, coronavirus, parainfluenza) Gram(+)= S. pneumoniae, S.aureus Gram(-)= Moraxella catarrhalis, H. influezae Peritonsillitis Viruses and group A Strep (pyogenes) Chronic otitis media SUPPURATIVE: Gram(+)=Staph aureus, Gram(-)=Pseudomonas, Proteus Bacteroides, Chronic otitis media SEROUS (microbes same as AOM) Gram(+)=S.pneumoniae, S. aureus Gram (-)=Moraxella catarrhalis, H. influenzae Neck space infusion Gram(+)=S.pneumoniae Gram (-)=H. influenzae, P. aeruginosa Auricular perichondritis Gram (+)=Staph aureus Gram (-)=P. aeruginosa 12. Nerves involved in referred otalgia include cranial nerves 5,7,9,10 and cervical nerves 2 and 3. 13. Cocaine anesthesia can cause effects related to its inhibition of catecholamine uptake by noradrenaline and dopamine transporters. It causes psychomotor stimulation and euphoria. It’s effects on peripheral sympathomimetic actions cause tachycardia, vasoconstriction and increased blood pressure. Toxic effects include cardiac dysrhymias and coronary/cerebral thrombosis. Prolonged use can cause myocardial damage leading to cardiac failure. On overdose, respiratory and vasomotor depression can occur. 14. Indications for tracheostomy include: 1. Conditions causing upper airways obstruction 2. Conditions necessitating protection of the tracheobronchial tree 3. Conditions causing respiratory failure Conditions necessitating protection of the tracheobronchial tree include: “Tracheostomy Can Protect Fantastically in MS and MG” Tetanus, Coma, Polio, Fractures of face, Multiple Sclerosis, Stroke, Myasthenia Gravis, Guillain-Barre syndrome In cases of respiratory failure, tracheostomy tubes facilitates reduction of dead space (decreases by 70mL), administer positive airways pressure, bypass laryngeal resistance or obstruction, clean/toilet the pulmonary/bronchial secretions and administer humidified O2. 15. Stridor is a high pitched noise produced by narrowing in the larynx or trachea. In laryngeal obstruction, the stridor is inspiratory, in tracheal it is usually inspiratory AND expiratory. It indicates airways obstruction. The signs of airways obstruction include: 1. Stertor (low pitched sound from supra-laryngeal obstruction) 2. Stridor (high pitched sound from laryngeal/tracheal obstruction) 3. Accessory muscles of respiration 4. Tachycardia 5. Cyanosis 6. Pallor, sweating, restless 7. Intercostal recession BEWARE! When asphyxia is of long duration, exhaustion sets in. Causes of stridor include causes of laryngeal or tracheal obstruction, which include: ACUTE causes: 1. Acute epiglottitis 2. Laryngotracheobronchitis 3. Laryngeal diphtheria Chronic causes (singer’s nodules, tumors, TB larynx, Syphilis of larynx, Hyperkeratosis of larynx) tend to cause hoarseness rather than stridor CONGENITAL causes (present at or close to birth) 1. Laryngomalacia: Stridor shortly after birth because of collapse of soft laryngeal tissues on inspiration. It is surgically remedied by incision of aryepiglottic folds. 2. Congenital subglottal stenosis: at level of cricoid cartilage 3. Laryngeal webs: anteriorly situated 4. Laryngeal cysts 5. Vascular ring: anomaly of aorta that encirculates esophagus and trachea causing constriction. Surgery… It is not always necessary to do tracheostomy as antibiotics and humidified air are often sufficient for some acute causes, and endotracheal tube intubation with surgery is sufficient for most congenital causes. 16. Peritonsillar abscesses can arise as a complication of acute tonsillitis (as can chest infections, otitis media, acute rheumatic disease and IgA mediated nephropathy). They are collections of pus outside the capsule of the tonsil but close to its upper pole. Symptoms include: 1. Dysphagia 2. Otalgia (referred) 3. pyrexia 4. TRISMUS (motor disturbance of CN V, causing spasm of masticatory muscles with difficulty opening mouth- should be able to insert three fingers-breadth into mouth as general rule). As peritonsillar abscesses are associated with acute tonsillitis, symptoms of tonsillitis (cervical lymphadenopathy, earache, dysphagia, pyrexia, headache and malaise) can also be expected. While meningitis is a complication of otitis media, it is not a common complication of tonsillitis or quinsy. Sleep apnea is caused by obstruction by enlarged tonsils or adenoids. Peritonsillar abscess may be associated with enlarged tonsils but is not itself a cause of sleep apnea. 17. Chronic otitis media with effusion is also known as “glue ear” and is a considerably important condition to recognize as it can cause deafness. It is caused by: 1. nasopharyngeal obstruction Eustachian tube dysfunction 2. Acute otitis media 3. allergic rhinitis 4. parental smoking, winter months 5. Otitic barotraumas Symptoms include deafness, discomfort (NOT otalgia) and tinnitus or unsteadiness (NOT vertigo). On examination of the tympanic membrane, it appears retracted with a fluid level. It may have a yellow/orange tinge. Tuning fork tests show conductive deafness. The tympanic membrane is NOT perforated! 18. Menieres disease is caused by distension of the membranous labyrinth by excessive endolymph. It is usually unilateral (25% bilateral), comes on age 40-60, and presents with: 1. Intermittent vertigo vomiting 2. “Fullness” in ear 3. Deafness (sensorineural) which is progressive and severe 4. Tinnitus (persistent) Otalgia is not a common feature in Menieres It is treated by antiemetics (prochlorperazine), and restriction of salt and fluids. Avoidance of alcohol, cigarettes and coffee may also be effective. If medical treatments are ineffective, surgical options include: 1. Labyrinthectomy (cures vertigo but kills hearing) 2. Drain endolymphatic sac 3. Divide vestibular nerve (very hazardous) 4. Intra-tympanic gentamycin (reduces vestibular but 10% risk of worsening hearing) 19. Purulent discharge of a unilateral basis can be caused by: 1. unilateral choanal atresia (~age5 with mucoid discharge in one nostril) 2. nasal foreign body (often foul smelling purulent discharge) Allergic rhinitis and rhinitis medicamentosa both cause discharge but of a runny (watery) nature rather than purulent. Septal hematoma causes nasal obstruction but not discharge. In fact, the hematoma is wedged between two layers of perichondrium. 20. Vocal cord paralysis causes hoarseness and weak voice but not stridor. Consolidation does not cause stridor as there is no obstruction present. Bronchial asthma causes a wheeze, not a stridor. Vocal cord paralysis can be caused by recurrent laryngeal nerve palsies. Usually the left recurrent laryngeal nerve is affected because it is more vulnerable given it recurs over the arch of the aorta to return to the larynx. Causes of recurrent laryngeal nerve palsy include: 1. Carcinoma of: - bronchus 2. 3. 4. 5. 6. - esophagus - thyroid - hypopharynx Surgery of: - cardiac, esophagus, thyroid or cervical spine Aortic aneurysm (left only) Malignant mediastinal nodes (left only) Trauma Virus (can be transient or recurrent) 21. Calculi of the salivary glands are more common in the submandibular gland than the parotid, because of the submandibular glands mixed mucous and serous secretion, rather than parotid’s mainly serous secretion. The sublingual gland secretes a mainly mucus secretion, but calculi are less common than in the submandibular gland. Calculi of the salivary glands are not always radioopaque. When they ARE radioopaque, they may be visualized using plain X-ray. If they can not be seen on plain x-ray, a ultrasound can be useful (although only radiologists can read them). Finally, a sialogram will outline the duct system and highlight any strictures, radiolucent calculi or sialectasis (die looks like drops). Sialectasis refers to a dilatation of the salivary gland duct. This has nothing to do with salivary gland calculi. 22. Facial nerve paralysis can be associated with “Some Very Big PAROTid Tumor” Sarcoidosis Vascular lesions in cerebrum Bells palsy Poliomyelitis Acoustic neuroma Ramsay Hunt (herpes zoster of geniculate ganglion, causing extreme pain in ear, vertigo, decreased hearing and cranial nerve palsies in 7 most commonly, and 5,6,9,10,12 less commonly) Otitis media (acute and chronic) Trauma (facial) Tumors (acoustic neuroma, parotid tumors, cerebral tumors, middle ear tumors) 23. The relations of the sinuses are as follows: Maxillary sinus Superior = orbit Posterior = pterygo-palatine fossa Inferior = hard palate Medially = medial and inferior turbinate bones/recess/meatus Ethmoid sinus between lamina proprycea (orbit) and upper nose ALL sinuses open into ostiomeatal complex under middle turbinate. However, given the maxillary sinus communicates with a duct which opens in to the middle turbinate, the relation is not “direct.” 24. The parotid gland relates to the styloid muscles and styloid process of the temporal bone, the angle and ramus of the mandible and the ear. The facial nerve goes through it and divides into its branches (temporal, zygomatic, buccal, marginal mandibular, cervical, posterior auricular). The external jugular vein crosses it superficially. The mastoid process is behind the ear and thus not considered related to the parotid gland. 25. The anterior and posterior triangles of the neck are separated by the sternocleidomastoid. Anterior triangle of neck: lies from the median line of the neck Anterior border of SCM CONTAINS: Submandibular gland Thyroid and parathyroid glands Carotid sheath (common carotid+IJV+vagus nerve) ECA CN XII (hypoglossal nerve) CN XI (accessory nerve) CN X (vagus nerve) Larynx and pharynx Submandibular lymph nodes Branches of cervical plexus Posterior triangle of neck: lies from posterior border of SCM to anterior border of trapezius CONTAINS: EJV CN XI (accessory nerve) Trunks of brachial plexus Cervical and supraclavicularlymph nodes Subclavian artery, subclavian vein 26. The facial nerve supplies 1. Taste anterior 2/3 tongue and soft palate 2. Sensory external ear 3. Motor to: muscles of facial expression stapedius posterior digastric and stylohyoid 4. Parasympathetic to: submandibular and sublingual salivary glands lacrimal gland Despite the facial nerve passing through the parotid gland, it is in fact the glossopharyngeal nerve (CN IX) that supplies it with parasympathetic innervation. 27. Adenoid cystic carcinoma is a malignant neoplasm of the salivary glands. It comprises about 4% of neoplasms in the salivary glands. It presents as a slowly expanding mass, painless at first, that become painful if it involves nerves. It is especially known to cause perineural invasion by skipping lymphatics and metastasizing to lungs, bones and other tissues. It is most often unilateral. 28. Vestibular neuritis is of viral origin and causes vestibular failure and thus explosive persistent vertigo. Cochlear symptoms are absent (tinnitus and hearing loss). It can occur in epidemics, and resolution occurs over 6-12 weeks with the acute phase lasting 2 weeks. It is thought that the herpes virus may be implicated. It is rarely painful. 29. Globus pharyngeus is a sensation of a lump in the throat. It is sometimes caused by cricopharyngeal spasm. Eating can make the sensation better, but anxiety and introspection can make it worse. Globus pharyngeus is commonly associated with at least mild dysphagia; however, our class notes and the ENT department’s handouts say that globus pharyngeus does NOT cause dysphagia-go with false. If symptoms persist, barium swallow then esophagoscopy is essential. It is commonly associated with older anxious women. 30. The inner ear is buried in the petrous part of the temporal bone and consists of bony labyrinth (perilymph) and membranous labyrinth (endolymph; sacs and ducts suspended in bony labyrinth). Cochlea The outer bony parts have perilymph, the inner membrane (cochlear duct) has endolymph Semicircular canals The CANALS have perilymph while the inner semicircular DUCTS have endolymph The cochlea is the organ for hearing-the semicircular canals, vestibule (saccule and utricle) are for balance. Transverse fractures affect the cochlea 31. Cancers of the larynx are almost all SCC. Adenoid cystic carcinoma and sarcoma occur but rarely. Glottic (60%), subglottic (10%) and supraglottic (30%) Cancers of the nasopharynx are most commonly SCC. Rarely lymphoma or adenoid cystic carcinoma can occur as well. While SCC is the most common middle ear malignant neoplasm, these are extremely rare. 32. Since all malignant neoplasms in the parotid gland can impinge on the facial nerve, all can cause facial nerve palsies, which present by the face being pulled down. 33. Retropharyngeal abscess occurs, as a rule, in infants and young children. Upper respiratory tract infection causes adenitis in the retropharyngeal lymph nodes, which suppurate. The abscess is limited to one side of the midline because of the median raphe of buccopharyngeal fascia. Clinically, the child is ill and pyrexic. Dysphagia and stridor may occur, and the head is often held to one side (abscess on one side, holds head to one side, dancing RETRO!). Alternatively, the kid can extend the head and open the mouth to keep his airway open, according to Bull ENT book. Treatment involves full dose antibiotics, and abscess incision. Incision is done under general anesthesia with great care, since abscess rupture can cause pus aspiration and ultimately…DEATH! Hwa ha ha ha… The high mortality rate of RPA is owing to its association with airway obstruction, mediastinitis, aspiration pneumonia, epidural abscess, jugular venous thrombosis, and erosion into the carotid artery. Aerobic organisms (beta-hemolytic streptococci and Staphylococcus aureus) Anaerobic organisms, such as species of Bacteroides and Veillonella Gram-negative organisms, such as Haemophilus parainfluenzae 34. Nasopharyngeal carcinoma causes a clinical picture reflective of it’s invasion of: Local structures nasal obstruction and blood-stained discharge Otological unilateral serous otitis media from Eustachian tuba obstruction Neurological invasion at skull base causes paralysis of CN III, IV, V, VI, IX, X, XII Cervical deep cervical lymphadenopathy (often between mastoid and angle of jaw) Otalgia can be referred as a result of involvement of involvement of CN 5,7,9,10. Nasal obstruction with epistaxis can occur. 35. Malignant disease of the hypopharynx, as a general rule: Carcinoma of piriform fossa (just above vocal cords)= disease of men Post-cricoid carcinoma=disease of women, perhaps related to PattersonBrown-Kelly aka Plummer-Vinson syndrome Clinically, it cause: - dysphagia and weight loss - cervical lymphadenopathy - hoarseness (LATE sign though) - referred otalgia (worse on swallowing) - mirror exam shows malignant ulcer I think the “lymph node behind angle of the jaw” refers to nasopharyngeal carcinoma, which causes cervical lymphadenopathy between mastoid and angle of jaw, thus I think this is False… 36. Causes of enlarged tonsils include: - acute tonsillitis - neoplasm (often unilateral; includes lymphoma and carcinoma) While amyloid can be found in the tonsil (NCBI does report a case of primary amyloidosis affecting the tonsil), it is so rare I would prefer to think this question is to differentiate the student who realizes that amyloidosis in this area MOST often affects the tongue or salivary glands, and not the tonsil. Enlargement of the parotid gland can push the tonsils outwards, causing them to appear enlarged on examination. 37. Polyps are loose edematous stroma, infiltrated by inflammatory lymphocytes and covered by respiratory epithelium. They are not neoplastic in either a malignant or benign fashion. 38. The ethmoid sinuses are bound: - laterally to the orbit by lamina papyracea - superiorly they communicate with frontal sinus - inferiorly they empty under middle turbinate (indirectly via duct) - medially upper part of nose A google search, and looking into my Dorlands and free medical dictionary found no mention of lamina capricus. I give up. 39. Between 2 and 7% of people who get Bells’ palsy will have a recurrence. Bell’s is a lower motor neuron facial palsy of unknown cause, but possibly viral. It is part of the group of idiopathic cranial mononeuropathies. It may be complete or incomplete, and the worse the severity, the worse the prognosis. It is treated with steroids with or without nerve decompression. It recovers in 85% of cases. A herpes zoster infection that affects the facial nerve is referring to Ramsay-Hunt syndrome, in which case the primary Herpes infection remains dormant in the geniculate ganglion, and the HZV then erupts in CN V, VI, VII, IX, X, XII. The patient is usually elderly and the patient gets a vesicular eruption in the ear, vertigo and impaired hearing. Treatment is with acyclovir. Giving steroids in this condition will make it worse. 40. Causes of UNIlateral hearing loss: - Trauma - Meniere’s disease Causes of Bilateral hearing loss: - Acoustic neuroma - mumps - Presbycusis - Noise trauma - Ototoxicity (esp. aminoglycosides) - Autoimmune Otosclerosis may be unilateral (20%) or bilateral (80%) but usually one ear is affected worse than the other, so unilateral stapedectomy can “save hearing.” It can cause conductive (99%) or sensorineural hearing loss depending on whether the middle ear or the labyrinthine cavity are affected. 41. The parotid gland lies on the side of the face in close relationship to ear, angle of mandible and styloid muscles. The facial nerve enters the posterior pole and divides within its substance into branches. It’s duct opens opposite the second molar tooth. Saliva produced is serous and secretomotor supply is from glossopharyngeal nerve. The submandibular gland is in floor of the mouth below and medial to mandible. Deep part of gland goes around mylohyoid and duct opens at sublingual papilla. Secretomotor supply from facial nerve (chorda tympani). Saliva is mixed. 42. Limited jaw mobility can result from trauma, surgery, radiation treatment, or even TMJ problems. The limitation in opening may be a result of muscle damage, joint damage, rapid growth of connective tissue (i.e. scarring) or a combination of these factors. Limitations caused by factors external to the joint include neoplasms, acute infection, myositis, systemic diseases (lupus, scleroderma, and others) pseudoankylosis, burn injuries or other trauma to the musculature surrounding the joint. Limitations caused by factors internal to the joint include bony ankylosis (bony in growth within the joint), fibrous ankylosis, arthritis, infections, trauma and (perhaps) micro-trauma that may include brusixm. Central Nervous System disorders can also cause limitations to mouth opening. Tetanus, lesions that affect the trigeminal nerve and drug toxicity may all be suspects in this condition. Finally, there are iatrogenic causes, such as third molar extraction (in which the muscles of mastication may be torn, or the joint hyperextended) hematomas secondary to dental injection and late effects of intermaxillary fixation after mandibular fracture or other trauma. Quinsy and nasopharyngeal carcinoma commonly cause trismus. In nasopharyngeal carcinoma, trismus usually indicates a younger patient and a more advanced tumor. Cancer of the tonsil accounts for approximately 0.6% of malignancies diagnosed in the United States each year. Presentation of this disease is often delayed because of the lack of early symptoms. Patients usually present with a large mass in the oropharynx, accompanied by a neck mass, as well as pain, trismus, otalgia, and weight loss. Most patients present during the fifth or sixth decade, and men outnumber women 3:1. 43. Nasopharyngeal carcinoma rarely invades the orbit, thus proptosis rarely occurs with nasopharyngeal carcinoma. Nasopharyngeal carcinoma will present with symptoms dependent on invasion of: - local nasal obstruction and bloody discharge - otological Eustachian tube obstruction unilateral serous otitis media - neurological invades skull base palsies of CN V, VI, IX, X, XII - cervical upper deep cervical lymph nodes, often wedged between mastoid process and angle of jaw. 44. The gentleman presents with upper deep cervical lymphadenopathy. GI tumors classically present at Virchow’s node (left supraclavicular if gastric Ca), or the abdominal lymph nodes otherwise, thus a gi aetiology is unlikely in this gentleman. However, nasopharyngeal carcinoma often presents as an expansile mass in the neck, often between the angle of the mandible and the mastoid process. Thus, this is a possibility in this gentleman. The physician should consider the diagnosis of chronic tonsillitis when the patient has a sore throat or pain with swallowing that last longer than 4 weeks. Associated symptoms include tonsilloliths, halitosis, excessive tonsillar debris, peritonsillar erythema, and persistent tender cervical lymphadenopathy. On exam, one may see erythema, dilated surface vessels and a smooth tonsillar surface. 45. Glandular fever is also known as infectious mononucleosis. It is usually caused by EBV although CMV and toxoplasmosis may produce milder clinical forms less commonly. The EBV variant is associated with marked fever, headache (“pain”), sore throat (“pain”), lymphadenopathy (esp. posterior cervical), pyrexia, splenomegaly and malaise. Mild hepatitis, myocarditis, meningitis, encephalitis occur less often. Diagnosis is made by a monospot test. When treating tonsillitis, we should avoid using amoxicillin as this can precipitate infectious mononucleosis. 46. Causes of facial nerve paralysis include: “Some Very Big PAROTid Tumors” Sarcoidosis Vascular lesions in cerebrum Bell’s palsy Poliomyelitis Acoustic neuroma Ramsay-Hunt syndrome Otitis media (acute) Trauma Tumors (acoustic neuroma, pleomorphic adenoma, adenoid cystic carcinoma, Warthin’s tumor) 47. Sjogren's syndrome classically features a combination of dry eyes, dry mouth, and another disease of the connective tissues, most commonly rheumatoid arthritis. Sjogren's syndrome that involves the gland inflammation (resulting in dryness of the eyes and mouth, etc.), but not associated with a connective tissue disease, is referred to as primary Sjogren's syndrome. Secondary Sjogren's syndrome involves not only gland inflammation, but is associated with a connective tissue disease, such as rheumatoid arthritis, systemic lupus erythematosus, or scleroderma. 90% of Sjogren's syndrome patients are female Symptoms of Sjogren's syndrome can involve the glands, as above, but there are also possible affects of the illness involving other organs of the body (extraglandular manifestations). When the tear gland (lacrimal gland) is inflamed from Sjogren's, the resulting eye dryness can progressively lead to eye irritation, decreased tear production, "gritty" sensation, infection, and serious abrasion of the dome of the eye (cornea). Inflammation of the salivary glands can lead to mouth dryness, swallowing difficulties, dental decay, gum disease, mouth sores and swelling, stones and/or infection of parotid gland inside of the cheeks. Other glands that can become inflamed, though less commonly, in Sjogren's syndrome include those of the lining of the breathing passages (leading to lung infections) and vagina (sometimes noted as pain during intercourse). A small percentage of patients with Sjogren's syndrome develop cancer of the lymph glands (lymphoma). This usually develops after many years with the illness. Unusual gland swelling should be reported to the physician. The diagnosis of Sjogren's syndrome involves detecting the features of dryness of the eyes and mouth. The dryness of the eyes can be determined in the doctor's office by testing the eye's ability to wet a small testing paper strip placed under the eyelid (Schirmer's test). More sophisticated eye testing can be done by an eye specialist (ophthalmologist). Salivary glands can become larger and harden or become tender. Salivary gland inflammation can be detected by radiologic salivary scans. Also the diminished ability of the salivary glands to produce saliva can be measured with salivary flow testing. The diagnosis is strongly supported by the abnormal findings of a biopsy of salivary gland tissue. Depending on the source, Sjogrens can cause a painless or mildly painful swelling. I’d go with false here. In Ireland, Sjogrens is diagnosed with sublabial biopsy (as it says in class notes…). 48. Longitudinal fractures typically result from trauma to the temporal or parietal region, and fractures of the temporal squamosa or parietal bone are common. The line of force runs roughly from lateral to medial. Because a fracture line may extend through the facial nerve canal, injury to this nerve may result. In addition, associated injury, such as transection or intraneural hemorrhage, may cause facial nerve paralysis. The fracture also may disrupt the ossicular chain and result in conductive hearing loss. Transverse fractures typically result from trauma to the occiput or cranial-cervical junction. The line of force runs roughly anterior to posterior. When the fracture passes through the vestibulocochlear apparatus, both sensorineural hearing loss and disorders of equilibrium may occur. Injury to the facial nerve is common in this type of injury as well, since the fracture often courses close to the labyrinthine segment of the facial nerve. Fracture type CN VII damage Longitudinal Yes (CNVII canal) Transverse Yes (labyrinthine) Hearing loss type Conductive Sensorineural Trauma location parietal/temporal occiput/craniocervical Generally, diagnosis of temporal bone fracture (transverse and longitudinal) by plain film is difficult and requires confirmation by CT. A longitudinal fracture roughly parallels the petrous bone long axis. Involvement of the middle ear, carotid canal, bony labyrinth, and external auditory canal should be noted. A transverse fracture is perpendicular to the petrous bone long axis. Involvement of the inner ear structures and facial nerve course should be noted. The longitudinal temporal bone fracture can cause bleeding in the middle ear, leading to hemotypanum. Since there is no perforation of the tympanic membrane, discharge is unlikely. 49. Positional vertigo is an inner ear problem. It causes brief but sometimes severe feelings of spinning. Some people feel that their head or body is spinning. Others feel the room is spinning. People often say they are dizzy, but dizzy is a very general term. Vertigo, on the other hand, is the very specific feeling of uncontrollable spinning. Positional vertigo happens suddenly when you change the position of your head. Another name for this problem is benign paroxysmal positional vertigo. In the inner part of your ear are 3 semicircular canals. Movement of the fluid in these canals helps your brain maintain your balance and know what position you are in (for example, standing up, lying down, or standing on your head). Sometimes small crystals of calcium develop and float in the fluid in the inner ear. This can happen after a head injury (trauma), with a severe cold, or simply as a part of normal aging. The crystals can cause vertigo when you change head position and they strike against nerve endings in the semicircular canals. Usually the calcium crystals dissolve in a few weeks and stop causing vertigo. However, sometimes the crystals do not dissolve and the vertigo returns from time to time. A sudden feeling that you are spinning, or that the room is spinning, is the main symptom. You may feel the vertigo when you first wake up. It may seem that any turn of your head brings on brief but intense spells of vertigo. It may happen when you tilt your head, look up or down, or roll over in bed. You may have nausea and vomiting along with the vertigo. Even if a spell of vertigo is brief, you may have a feeling of queasiness for several minutes or even hours afterward. 50. Maxillary sinus is the most common paranasal sinus affected by carcinoma (80%) with ethmoid (15%) and the facial and sphenoid sinuses (<5%) being less common. Symptoms of maxillary sinus carcinoma include nasal symptoms of unilateral nasal obstruction, epistaxis, anosmia, nasal drainage, and hyponasal speech. Facial symptoms are the next most common and include: loss of definition of the nasolabial fold of the involved side, facial asymmetry, obvious cheek mass, cutaneous fistula, facial edema, and pain. Hypesthesia of the cheek may also occur secondary to invasion of the infraorbital nerve. Oral cavity symptoms include: ill fitting upper dentures, widened alveolus, dental pain, or an obvious palatal mass. 51. Thyroid carcinomas are usually papillary (65%), anaplastic (5%), follicular (20%) or medullary (10%). In the middle ear, the most common benign tumor is cholesteotoma. Malignant tumors in the middle ear and mastoid are very uncommon. Of these very uncommon tumors, the squamous cell cancers are the most prevalent More than 90% of cancers of the oral cavity and oropharynx are squamous cell carcinomas, also called squamous cell cancer. These are seen more commonly than in middle ear…What they mean by “common” though? I say true… Tumors in the salivary glands are more commonly in the parotid gland, where pleomorphic adenoma accounts for the majority. Warthin’s tymor and hemangiomas are also rare benign tumors. Malignant tumors include adenoid cystic carcinoma, muco-epidermoid tumor, acinic cell tumors, lymphoma…The point is that while SCCs DO happen in submandibular and parotid glands, they are very uncommon and have a poor prognosis. 52. Laryngotracheobronchitis (“croup”) (larynx, trachea and bronchi but epiglottis not usually involved) occurs in infants and toddlers. It is a viral (parainfluenzae, influenzae, adenovirus) generalized respiratory infection accompanied by thick tenacious secretions that block the trachea and small airways. There is a harsh, croupy cough. Mild cases settle with humidified air, but severe cases require airway support and possible ventilation. 53. Complications of acute otitis media include: (“FAT PALM” - Facial nerve paralysis - Abscess (extradural, subdural, brain abscess) - Thrombosis of lateral sinus - Petrositis (don’t forget forever important Gradenigo’s syndromeCN VI palsy) - Acute mastoiditis - Labyrinthitis ( vertigo) - Meningitis Acute otitis media can lead to chronic otitis media, especially if poorly treated. Otalgia, tinnitus and progressive hearing loss are features in chronic otitis media. Whether the otalgia is severe or not I can’t establish. Given the long-duration nature of chronic otitis media, I’d be willing to bet this is false. 54. Scala media (or cochlear duct) is a endolymph filled cavity inside the cochlea, located in between the scala tympani and the scala vestibuli, separated by the basilar membrane and Reissner's membrane (the vestibular membrane) respectively. Scala media houses the organ of Corti. Sound waves from the middle ear pass from stapes to the oval window (fenestra vestibuli), which pass to the perilymph filled scala vestibuli, which pass through the Reissner’s membrane, to the endolymph filled cochlear duct (scala media), which stimulate Organ of Corti. The sound dissipates through the scala tympani to the round window. The cochlea is found in the petrous part of the temporal bone, and is dedicated to hearing. It has no role in balance, although other inner ear structures (semicircular canals) do. Longitudinal fractures of the temporal bone commonly occur after trauma to the parietal or temporal regions. Usually the middle ear is affected and conductive deafness may occur. Transverse temporal fractures occur after trauma to the occipital or craniocervical region. They often involve the inner ear and sensorineural deafness may occur. Both transverse and longitudinal temporal bone fractures can cause damage to the facial nerve. 55. Lip cancer patients typically present in their 7th or 8th decade. The male to female ratio approaches 79-to-1 for cancer of the lower lip and 5-to-1 for the upper lip. Several factors have been implicated in the etiology of lip cancer. Sunlight has been implicated as a major contributor to the development of lip cancer. Since the lip lacks a pigmented layer for protection, it is susceptible to actinic changes. Moderate to heavy cigarette and pipe smoking also play a causative role. In earlier studies, an association of carcinoma of the lip and positive serology or clinical evidence of syphilis was implied to be as high as 20%. More recent papers report not more than a 2% association. Poor oral hygiene results in persistent irritation and possibly lip cancer. Chronic alcoholism has been associated with the development of carcinoma of the lip as well as other sites in the oral cavity. The most frequent location of lip cancer is the lower lip where it is reported being found between 91.3% and 97.3%. The upper lip is involved between 1.8% and 7.7% of the time, while the commissure is involved in 1% to 2%. Almost 95% of lip cancers are squamous cell carcinoma. They are most frequently well differentiated. Basal cell carcinoma may extend onto the labial surface. The primary goal of treatment is eradication of the disease. In decreasing order of priority, the goals of therapy are: 1) preservation of oral competence; 2) preservation of an adequate buccal sulcus; 3) minimalization of the deformity; and 4) restoration of a cosmetically acceptable appearance. Primary surgical excision offers the advantage of eradication of disease, pathological survey of margins, and reconstruction of the defect in a single stage. Overall, 5% to 15% of patients with lip cancer will present with regional metastasis. An additional 15% will subsequently develop nodal metastasis. The five-year survival of patients with lip carcinoma and confirmed regional metastasis approaches 50%. The literature suggests that the survival rate for treatment of the initial neck metastasis by elective neck dissection and for salvage for the subsequent development of neck nodes is essentially the same. A review of the literature indicates several prognostic indicators for lip carcinoma. Carcinoma of the upper lip and commissure carry a worse prognosis and the five-year survival is 10% to 20% lower than the overall rate. Cervical metastasis, especially when large, bilateral, or fixed indicate a poor prognosis as does the presence of distant metastasis. Poorly differentiated squamous cell carcinoma, as well as melanoma carry a worse prognosis. Recurrent squamous cell carcinoma at the site of the primary carries a worse prognosis and may be an indication of an aggressive neoplasm. The presence of mandibular involvement drops the five-year survival rate to 30%. At presentation, 15-20% of lip carcinomas have metastasized, most commonly to submandibular and less commonly to submental and internal jugular lymph nodes. In a recent evaluation of sentinel lymph node biopsy at presentation of lip SCC, only 15% of sentinel lymph nodes were found to have disease. 56. The most common malignancy in the tonsil is SCC, while the second most common is a lymphoma. The most common malignancy on the tongue is SCC. Symptoms of tongue cancer may include: - red/white patch on tongue that doesn’t go away - sore throat that lingers - pain swallowing - numb mouth - unexplained bleeding in mouth - otalgia (referred, not radiating) Carcinoma of the nasopharynx results in: Local nasal obstruction and epistaxis Otological Eustachian tube blockage unilateral serous otitis media (Which can deafness) Neurological palsies of CN III, IV, V, VI, IX, X, XII Cervical deep cervical lymph nodes (often between angle of mandible and mastoid process) Leukoplakia (red plaque) and erythroplakia (red plaque) are lesions commonly seen on buccal mucosa and commisures of mouth. They are commonly associated with SCC. The question SHOULD be “leukoplakia can arise in buccal mucosa” but even in the convoluted way it’s written it’s still probably true. 57. Mastoiditis is the result of extension of acute otitis media into the mastoid air cells with suppuration and bone necrosis. Acute mastoiditis symptoms: - pain - otorrhea (creamy and profuse) - increasing deafness (conductive) Signs: - pyrexia and malaise tenderness over maxillary antrum postauricular swelling pinna pushed down and forward (moving ear up and back hurts) - tympanic membrane bulging or perforated - Perceptive deafness refers to sensorineural or inner ear deafness. Acute mastoiditis affects the middle ear and causes conductive deafness. Mastoiditis is most common 15-18 months of age when middle ear infections are most common. Adults rarely get mastoiditis, and it’s usually associated with immunocompromise. 58. The sinuses include as below: Sinus Location Ethmoid Around bridge of nose Maxillary Around cheeks over maxilla Frontal Forehead Sphenoid Behind nose Age of presentation Birth Birth 7 years of age-adolescence adolescence OK, no source for this, but my thoughts: Most cases of sinusitis occur as pediatric cases, and certainly most before 30 (my arbitrary cut-off of “aged”). However, maxillary sinusitis can certainly occur later than 12, since web search revealed multiple cases of patients in 30s getting it (not COMMON, but still happens). 59. Otosclerosis may be unilateral (20%) or bilateral (80%) but usually one ear is affected worse than the other, so unilateral stapedectomy can “save hearing.” It can cause conductive (99%) or sensorineural hearing loss depending on whether the middle ear or the labyrinthine cavity are affected. Since “bone conduction” refers to sensorineural, we can see they are trying to confuse us, given the stapes being prominently affected would lead us to believe “bone” conduction is affected. However, outer and middle ear is referred to as “air” conduction while inner ear is “bone” conduction, so therefore most of the time otosclerosis doesn’t affect bone conduction. Otosclerosis doesn’t affect the tympanic membrane. It is a disease of the middle ear and doesn’t cause tympanic membrane damage or signs. 60. Acute otitis media commonly causes otalgia, deafness and tinnitus. The ear pain is relieved when the tympanic membrane is perforated (and the annoying kid stops screaming). Causative organisms include Streptococcus pneumoniae (35%), Moraxella catarrhalis (15%), Haemophilus influenzae (25%), Group A Strep (Streptococcus pyogenes), and Staphyloccus aureus. 61. Organisms commonly causing chronic otitis media include: Chronic SUPPURATIVE otitis media - Pseudomonas (MOST commonly) - Staphylococcus (gram positive) - Other gram-negative (especially Proteus) Chronic otitis media with effusion (glue ear) (same as acute otitis media) - Strep.pneumoniae, Staph aureus, - Moraxella catarrhalis, Haemophilus influenzae 62. OK, indications for this couldn’t be found anywhere (as in a list). Given symptoms need to be present for at least 4 weeks before surgery is indicated, neonates are out. As for failure of antibiotic treatment? Well if the antibiotics don’t sufficiently eliminate the ear effusion, then yes, the myringotomy would help, so let’s say TRUE. As for intracranial complications? I thought this was more in line with chronic otitis media (attico-antral type abscess) or acute otitis media (can meningitis), but in COM there is already a perforation, and in acute otitis media the tympanic membrane will usually burst…but will doing a myringotomy aid intracranial complications when it HASN’T yet burst? I assume it would but I don’t know…