Job Description - NHS Scotland Recruitment
advertisement

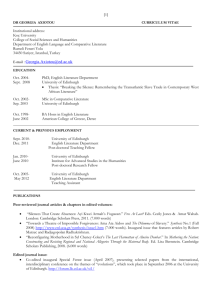
NHS Lothian Royal Edinburgh and Associated Services Royal Edinburgh Hospital Consultant Adult Psychiatrist - Full time (10 PA) Eating Disorders Service Outline of the post This is a full-time (10 PA), fixed term post to be recruited to immediately. The successful candidate will join a long established eating disorders service with two experienced multi-disciplinary teams. The Cullen Centre team provides outpatient treatment to people across the range of eating disorder diagnoses. The Anorexia Nervosa Intensive Treatment Team (ANITT) provides intensive community treatment to patients with severe Anorexia Nervosa. The two teams work closely together with a clinical management team spanning the whole service. In-patient facilities serve the SE region of Scotland and are provided at the Regional Eating Disorders Unit (REDU) at St. John’s Hospital, Livingston. The Consultant will provide a central role within both teams, delivering psychiatric management for a caseload of complex patients, providing the psychiatric liaison role with the inpatient service for admissions and taking the lead role in providing psychiatric & medical risk management and consultation for the service as a whole. Assessment of complex new referrals along with liaison & consultation with other services over co-morbid presentations will be a further component of the post. The Consultant will join the clinical management team, contributing to the further evolution of the already wide-ranging and high quality service. Existing evaluation and research projects will offer opportunities to pursue interests in research. These roles have previously been fulfilled by the Consultant Psychiatrists in each team. The two established Consultant Psychiatrists will continue to provide the medical psychotherapist roles within the service and so will be readily available to support the appointee in fulfilling their role. The post would appeal to anyone who enjoys psycho-somatic medicine, is interested in the relationship between mental and physical health and has an appreciation of psychological models of treatment. The post will attract 1 core SPA although additional SPA time will be available and negotiable according to the interests of the successful candidate and the requirements of the service. Page 1 of 12 NHS Lothian NHS Lothian is an integrated NHS Board in Scotland providing primary, community, mental health and hospital services. Mr Tim Davidson is Chief Executive and Dr David Farquharson is Medical Director. The NHS Board determines strategy, allocates resources and provides governance across the health system. Secondary care services are delivered by Lothian University Hospitals Division. The majority of Edinburgh based mental health services are delivered by Royal Edinburgh Hospital and Associated Services (REAS) a division of City of Edinburgh Community Health (and Social Care) Partnership. Other CH(C)Ps include West Lothian, East Lothian and Midlothian, and a Public Health Directorate. NHS Lothian serves a population of 850,000. Royal Edinburgh Hospital and Associated Services The Royal Edinburgh and Associated Services provides a range of Mental Health services to the population of Lothian and other Boards within Scotland. The Royal Edinburgh Hospital is located on the south side of the City of Edinburgh. It comprises some 20 wards, 420 beds, day hospitals and outpatient facilities. The hospital provides the following range of specialities: Acute Mental Health Rehabilitation Psychiatric Emergency Team 24/7 Outpatients Assessment Phychiatry of Old Age Forensic Medium Security Unit Child and Adolescent Mental Health Services Psychotherapy Service Psychology Services Services for Eating Disorders Day Hospitals – Psychiatry of Old Age The hospital is currently housed in a mix of accommodation ranging from 19th century to present. The Royal Edinburgh Hospital is undergoing an exciting period of development with a major reprovision of all accommodations in modern fit for purpose premises over coming years. Phase one, to include all acute general adult and psychiatry of the elderly beds, is due to be completed in Autumn 2016. REAS also provides a comprehensive range of community mental health services, including the emergency Mental Health Assessment Service (MHAS) and Intensive Home Treatment Team. University Hospitals Division The University Hospitals Division provides a full range of secondary and tertiary clinical services to the populations of Edinburgh, Midlothian, East Lothian and West Lothian. The Division is one of the major research and teaching centres in the United Kingdom. Hospitals included in the Division are: The Royal Infirmary of Edinburgh The Western General Hospital The Royal Hospital for Sick Children, Edinburgh St Johns Hospital Royal Victoria Hospital Page 2 of 12 Liberton Hospital The Princess Alexandra Eye Pavilion. The Royal Infirmary (RIE) is a major teaching hospital on a green field site in the South East of the city of Edinburgh built in 2003. It comprises 25 wards, 869 beds, and 24 operating theatres, and is equipped with modern theatre and critical care equipment and monitoring. Within the main building is a dedicated, multidisciplinary, 5 theatre day surgery complex. The hospital provides for most specialities and is the centre for: General surgery with a focus on the upper GI tract Vascular surgery Hepato-biliary and Transplant medicine and surgery Cardiac and Thoracic surgery Elective and trauma Orthopaedics surgery Neonatology Obstetrics & Gynaecology Cardiology Renal Medicine Sleep Medicine Regional major Accident and Emergency centre. There is a Combined Assessment Unit which takes unselected GP or direct emergency referrals, and from A&E. CAU includes the Dept of Liaison Psychiatry and the Scottish Poisons Bureau and Treatment Centre. There are full supporting Laboratory and Diagnostic Radiology Services (including CT, MR, Ultrasound and NM and PET scanning will be available in 2008). There is a full range of lecture theatres, a library and AV facilities. The Western General Hospital (WGH) has 600 beds and 5 operating theatres and is equipped with modern theatre and critical care equipment and monitoring. The Anne Ferguson building was completed in 2001. The hospital provides for most specialties and is the centre for: • Neurology, Neurosurgery and neuropathology UK CJD unit Colorectal Surgery Urology and Scottish Lithotriptor Centre Breast Surgery and Breast screening Gastro-Intestinal disease Rheumatology Infectious Diseases Haematology Oncology Medical Oncology Radiation Oncology (including 6 LINACs) Dermatology (Inpatient) Medicine of the Elderly/Stroke Medicine There is an Acute Receiving Unit, which accepts GP referrals and 999 ambulance medical cases on a zoned basis within the city, and a nurse led Minor Injuries Unit. There is no trauma unit at this hospital. There are full supporting Laboratory and Diagnostic Radiology Services (including CT, MR, Ultrasound and NM).There is a full range of lecture theatres, a library and AV facilities. St John’s Hospital opened in 1989 and is located in the centre of Livingston, a new town about 30 minutes drive west from Edinburgh. The hospital provides for most common specialties but does not have emergency general surgery or orthopaedic trauma operating. The hospital has a paediatric ward and is the centre for: Page 3 of 12 General Medicine with specialists in Cardiology, Diabetes & Endocrinology, Gastroenterology, Respiratory Medicine and Care of the Elderly Obstetrics & Gynaecology Child Health including Paediatrics and community child health The supraregional Burns and Plastic Surgery unit. Oral and Maxillofacial Surgery ENT Critical Care (ITU, HDU and CCU) Accident and Emergency General Surgery Orthopaedics Anaesthetics Mental Health including ICCU and ICPU Since 2005 general surgery and orthopaedics have been reconfigured in NHS Lothian with SJH being developed as a major elective centre for the region. Lothian’s ENT service was relocated to SJH to create an integrated head and neck unit with OMFS and Plastic Surgery. Recent developments at SJH include a new endoscopy suite, an Intensive Psychiatric Care Unit, a digital mammography unit, an oncology (cancer care) day centre, a satellite renal dialysis unit and a £2.75m reprovision of A&E. There are full supporting Laboratory and Diagnostic Radiology Services (including CT, Ultrasound and NM). The hospital has been accredited full teaching hospital status by the University of Edinburgh. There is a full range of lecture theatres, a library and AV facilities. Royal Hospital for Sick Children (RHSC) is a 141 bedded hospital providing general and specialist services for children. The hospital is situated in a residential area close to the centre of Edinburgh and is approximately 3 miles from the site of the New Royal Infirmary and the co-located University of Edinburgh Medical School and 3 miles from the Western General Hospital. The RHSC is a 151-bedded Hospital, and is the main paediatric teaching hospital for the South-East of Scotland providing general and specialised services on a local, regional and national basis. It acts as the local paediatric referral centre for the children of Edinburgh and surrounding areas, and as a tertiary referral centre for intensive care patients; gastroenterology, hepatology & nutrition; respiratory medicine; cardiology; nephrology; neurology; oncology; haematology; neonatal surgery; plastic surgery; orthopaedic surgery; urological surgery and aspects of general surgery. Hospital accommodation encompasses five theatres, a critical care unit comprising a 6/8 bedded Paediatric Intensive Care Unit, 4/6 bedded High Dependency Unit and a 3 bedded Neonatal Intensive Care Unit. There is an excellent library facility and a modern lecture theatre with a full range of audiovisual equipment. All services are supported by comprehensive radiology, neurophysiology, laboratory and therapy services. The local radiology department provides on site Magnetic Resonance Imaging, CT Scanning, nuclear scanning and ultrasound. On site laboratories provide biochemistry, haematology, pathology and neuropathology services Community Healthcare Partnerships The four established Lothian Community Health (and Social Care)Partnerships serve the population of Edinburgh, Midlothian, East Lothian and West Lothian. Hospitals in the CH(C)Ps include: The Astley Ainslie Hospital in Edinburgh Page 4 of 12 Rosslynlee Hospital in Midlothian Herdmanflat Hospital RoodlandsHospital in East Lothian. The four CHPs are coterminous with Edinburgh, Midlothian, East Lothian and West Lothian Councils bringing together those responsible for planning, managing and providing community-based health services for the population of Edinburgh and the Lothians. There are 7,500 members of staff. In addition, there are approximately 1,000 independent contractors in General Medical and Dental Practice, as well as pharmacists and opticians. A population of 850,000 people is served across health board area. The range of services care of the elderly, medical rehabilitation, community mental health, substance misuse and learning disability, district nursing and health visiting, family planning, well woman, , comprehensive dental care and those provided by Professions Allied to Medicine, such as physiotherapy, pharmacies and optometrists. Specialist services provided include brain injury rehabilitation, bio-engineering and prosthetics, drugs and alcohol misuse and harm reduction, AIDS/HIV and Children and Family Psychiatric Services. Department of Public Health Medicine The aim is to improve the health of the people of Lothian in collaboration with many other partners. Using our range of knowledge, experience and networking capability, our distinctive contributions are: the promotion of specific measures to monitor and improve health; the collation and interpretation of health related information. The following objectives have been agreed as the basis for the Department’s work plans: 1. To monitor the health status and health needs of people in Lothian; 2. To promote improvements in the health of Lothian people directly, and by providing information and advice to the public on health matters; 3. To assist Lothian NHS Board to fulfil its statutory obligations To contribute to strategic changes within the NHS in Lothian by providing information on clinical effectiveness To facilitate improvements in health and health care services directly, and through ‘managed clinical networks’ and wider alliances. 4. To contribute on a 24 hour basis to the control and prevention of communicable diseases and environmental hazards 5. To maintain commitments to teaching, training, professional development, audit and research. 6. To enable efficient management of the Department: there are at present four groups in the Directorate. These are; Healthy Communities, Healthcare; Health Protection and Health Information. University of Edinburgh The University of Edinburgh was established in 1582 and is one of the largest in the United Kingdom located on a number of prominent sites in Scotland’s capital city. It is Scotland’s premier research university, graded within the top six multi-faculty British Universities in the last national research assessment exercise (90 percent of its academic staff were in units rated 4, 5 or 5*). It has 3,000 academic staff, over 16,000 undergraduate and over 4,000 postgraduate students and an annual expenditure of over £261M for teaching and research. The University is organised into 3 Colleges: Humanities and Social Science, Medicine and Veterinary Medicine, Science and Engineering. There are strong academic and clinical links between the University and NHS mental health services. Page 5 of 12 Eating Disorders Service Information The successful candidate will join a long established eating disorders service with two experienced multidisciplinary teams. The service delivers a comprehensive tiered matched-care service model to provide the appropriate level and intensity of treatment for each patient, using our resources as cost-effectively as possible. The Cullen Centre team provides outpatient treatment to people across the full range of eating disorder diagnoses. A wide range of individual and group psychological treatments are offered as the core treatment, alongside specialist dietetic, nursing and psychiatric interventions & management. The therapies provided currently are Cognitive Behavioural Therapy (CBT), Cognitive Analytic Psychotherapy (CAT), Interpersonal Therapy (IPT), Dialectical Behavioural Therapy (DBT), Mindfulness-based therapy, Art Therapy and Specialist Structured Clinical Management (SSCM). The multi-disciplinary team includes psychiatric, clinical psychology, nursing, dietetic and specialist psychotherapy skills. The Anorexia Nervosa Intensive Treatment Team (ANITT) provides intensive community treatment to patients with severe Anorexia Nervosa. This novel service model has been developed over 10 years, providing continuity of care and reducing admissions for the highest risk patients. Detailed outcome evaluation remains a core part of the service, to ensure the safety and cost-effectiveness of the service (ref. Munro et al., Psychiatric Bulletin, 2014). The team maintains a small caseload of 30-35 for safe intensive treatment delivery. Schema Therapy and a core needs model, are at the centre of the treatment. Care is delivered either in the patient’s home environment or the outpatient setting at the Cullen Centre. The skill mix involves psychiatric, clinical psychology, nursing, dietetic and specialist psychotherapy skills. The two teams work closely together with a clinical management team spanning the whole service. The Lothian Eating Disorders Operational Management group (LEDOM) meets monthly, with senior line management from each of the disciplinary groups involved. Representatives from LEDOM attend other relevant management meetings relating to the service. The ANITT team has a weekly team meeting and the Cullen team meet fortnightly. There are three posts providing administrative and secretarial support across the two teams. A consultant psychiatrists meeting occurs each week. Case presentations occur weekly, involving both services. A monthly evaluation/research/journal club meeting involves clinicians from both teams. In-patient facilities serve the SE region of Scotland and are provided at the Regional Eating Disorders Unit (REDU) at St. John’s Hospital, Livingston. There is close communication with the inpatient service regarding the prioritisation of admissions, treatment planning for Lothian inpatients and active discharge planning. Psychiatric Colleagues The appointee will be one of a team of three Consultants in the community Eating Disorder Services, joining Dr. Katharine Logan (0.7 WTE – 0.4 Cullen Centre, 0.3 Trauma Service) and Dr Calum Munro (0.5 WTE – Anorexia Nervosa Intensive Treatment Team). The Eating Disorder Service also has close links with Dr. Rhiannon Pugh and Dr. Jon Patrick (Consultant Psychotherapists) in the Dynamic Psychotherapy department, also based on the Royal Edinburgh site. There is a joint peer group for Consultants from the Eating Disorder Service and the Psychotherapy Department. The Cullen Centre has a half-time core trainee doctor on a 6 monthly rotation. A 3 year ST4-6 Medical Psychotherapy post is currently vacant and we are in the process of converting this to an integrated joint training post with GAP. There will also be the potential to offer general psychiatric placements within the service for senior GAP trainees, once the appointee is in post. There is also an active Regional Clinical Network which provides an educational, training and support role for all eating disorder clinicians across SE Scotland. Page 6 of 12 Accommodation Both teams are on the REH site, but there is not sufficient space for them both to be based in one building currently. The Cullen Centre team are based in a stand-alone building on the edge of the REH site. This includes office space/consulting rooms, a medical treatment room, administrative offices, two large meeting rooms and a staff room. The Cullen team share this building with the Rivers Centre, a specialist treatment service for traumatic stress. The ANIT team have an office base a few minutes’ walk away in the Kennedy Tower. This also has one meeting room. The ANIT team use the Cullen Centre consulting rooms for those patients not needing home visits. The new Consultant will have suitable office space at both team bases. It will be furnished with the necessary office and IT equipment. Details of the Post The Consultant will provide a central role within both teams, delivering psychiatric management for a caseload of complex patients. The psychiatric management of a personal caseload is varied and includes medication management, management of self-harm and suicide risk, management of physical health & risks, supportive therapy and family-based interventions. The post-holder will take the lead role for the systems of psychiatric & medical risk management for the service as a whole, and in providing risk management consultation for other case-holding members of the multi-disciplinary team. Systems for the specific risk management of eating disorders patients are well established in the service, but of course there will be room for further development and integration across the teams. A full-time specialist nurse works across both teams and will work alongside the consultant delivering much of the physical risk management work, with the consultant providing weekly supervision. On occasions the Consultant takes on the role of Approved Medical Practitioner and Responsible Medical Officer when risks necessitate the use of the MHA. Consultation support to other clinical services managing patients with eating disorder-related risks, most often primary care teams, is an additional aspect of the post. Assessment of complex new referrals, including those with co-morbid presentations, is a significant part of this post. This will occasionally include the assessment of new eating disordered presentations attending A&E, on medical or surgical units or admitted to other parts of the psychiatric service. All complex new referrals to the service will invariably involve an assessment of psychiatric and physical risk and the generation of a risk management plan. At times it will involve liaison with other services about co-morbid presentations needing the continued input of other community or inpatient teams. A further component of the post is providing the psychiatric liaison role with the inpatient service for admissions and discharges. There are usually around 4-5 Lothian patients in the regional inpatient unit at any one time and occasionally patients with eating disorders are admitted to other wards. Admission planning, attending ward reviews to contribute to ward care plans and discharge planning, will constitute a significant part of the role. This often involves working closely with the therapists from the teams, using both the psychological formulation and psychiatric diagnoses to guide ongoing care. The Consultant will join the clinical management team, and develop their role within this, contributing to the further evolution of the already wide-ranging and high quality service and contributing to the monthly management meetings. This group is currently chaired and led by Louise Randell (Consultant Clinical Psychologist). There will be opportunities to develop a leadership role within the service. Existing evaluation and research projects will offer opportunities to pursue interests in research. The University of Edinburgh Psychiatry department is based on the Royal Edinburgh site. The Scottish Mental Health Research Network (SMHRN) is also based on site. The Eating Disorders service has excellent links with the SMHRN with past and current research projects receiving substantial support. Small project funds can be applied for through the Lothian Health Foundation fund and a local eating disorders specific fund the Butterfly Bursary. On-going projects include: an NIMH outline grant Page 7 of 12 application for a trial of computerised CBT for Bulimic disorders; a proposal for a pilot trial of the use of inhaled oxytocin in AN; a study comparing medical risk outcomes for severe AN in a community & hospital setting; a pilot study of the use of massage therapy in patients with severe AN; and a qualitative study of experiences of patients receiving intensive community treatment. All of the roles above have hitherto been fulfilled by the established Consultant Psychiatrists, KL & CM. They will continue to provide the medical psychotherapist roles within the service and so will be readily available to support the appointee in fulfilling their role and for cross-cover. Education, Training & Research The Royal Edinburgh Hospital offers a comprehensive rotational training scheme in psychiatry along with others in the South East Scottish region. The post-holder will therefore be expected to take part in the supervision and training of doctors in training. Medical students are regularly attached to the mental health service and Consultants are responsible for providing supervision and monitoring clinical experience during this time. In addition, tutorials take place weekly during the academic year for less experienced medical students and Consultants are expected to participate. Opportunities are also available for involvement in postgraduate teaching in the MRC Psych teaching course. The University Department of Psychiatry may award honorary senior lecturer status to the successful applicant at its discretion. The Department of Psychiatry, University of Edinburgh is a recognised centre of excellence. The Department hosts a weekly clinical case conference and a special lecture series, which Consultants are encouraged to support. In summary, the postholder will be expected: To deliver clinical care in the areas of psychiatric treatment for patients with eating disorders and liaison with other services. To share and develop a medical leadership role within the Lothian Eating Disorders community services. To fulfil supervision, teaching and training responsibilities within the service and for medical and psychiatric trainees. To ensure compliance with local and national policy for good care and meet professional requirements for CPD, appraisal and revalidation. Page 8 of 12 9. Provisional Job Plan DAY Monday Tuesday From / To HOSPITAL/ LOCATION REH Cullen Centre REH ANITT 6th floor Kennedy Tower TYPE OF WORK 9-1 CC Outpatient appointments or urgent assessment or liaison work DCC 1-5 Liaison work with REDU and other services 9-12.30 ANITT team meeting 4 Wednesday From / To REH Cullen Centre 3.5 12:30 – 1:30 Consultant meeting 1:30–4 ANITT outpatient appointments or home visits or urgent assessment or liaison work 1 2.5 4-5 CPD, job planning, appraisal etc. 9-10.30 Cullen Centre Meeting (2 weekly) 10:30–11:30 Case Presentation 1 2.5 11:30-12:30 Eating Disorders Evaluation & Research meeting (monthly) 2–3 Psychiatric Supervision of Cullen Centre CT3 Thursday From / To REH Cullen Centre AM 4 –5 Department of Psychiatry, Special lecture Series (monthly,term time) 9-12 CC outpatient appointments or urgent assessment or liaison work 1 1 1 4 LEDOM management meeting (monthly, 11.30-1) ANITT 6th Floor Kennedy Tower PM 1–4 ANITT outpatient appointments or home visits or urgent assessment or liaison work Regional Clinical Network Meeting (2 monthly, 2-4) Friday From / To REH ANITT 6th floor Kennedy Tower 4-5 Supervision of Specialist Nurse 9-4 ANITT outpatient appointments or home visits or urgent assessment or liaison work 4-5 Administration, Service management & development SPA 4 4 4 4 Notes: 1. non-weekly commitments in italics 2. Balance or work across the two teams approx. 50:50 3. Flexibility to respond to unplanned work in either team is central Page 9 of 12 Contact Details Further inquiries and arrangements to visit the service are welcomed and should be made to: Dr Calum Munro, Consultant Psychiatrist / Psychotherapist, ANITT, Royal Edinburgh Hospital Tel. 07854366831 Dr Katharine Logan, Consultant Psychiatrist / Psychotherapist, Cullen Centre, Royal Edinburgh Hospital Tel. 07816933737 Applicants may also wish to contact the following for a wider view of REH: Dr Peter Le Fevre, Divisional Associate Medical Director, Mackinnon House, Royal Edinburgh Hospital Dr Tim Montgomery, Operations Director, Mackinnon House, Royal Edinburgh Hospital Page 10 of 12 Person Specification REQUIREMENTS Qualifications and Training Experience Skills and Abilities ESSENTIAL MRC Psych (or equivalent) Full GMC Registration Included on the GMC Specialist Register (or eligible for such inclusion). Approval under Section 22, Mental Health (Care and Treatment) (Scotland) Act 2003, or be eligible and willing to gain the approval once in post Wide experience in the provision of adult mental health services in community, out-patient and hospital settings Experience of working with and a multi-disciplinary team Experience of providing leadership Experience of treating patients with eating disorders Experience of managing medical complications in patients with mental health problems Experience of managing and supervising colleagues Experience of preparing and delivering presentations and teaching Ability to provide leadership Ability to constructively engage with and be challenged by colleagues, learn from others and respec a diversity of views. Ability to manage anxiety when treating ‘at risk’ clients Clinical expertise in community psychiatry and knowledge of evidencebased treatment options Understanding of the needs of adults with mental illness, their carers and supporters, and commitment to working in partnership with these groups to develop services Ability to train and supervise junior medical staff and staff from other disciplines, and to support them in managing complex high risk clinical situations DESIRABLE MRCP or general medical experience at postgraduate level to MRCP or MRCGP level Training in supervision skills Experience of working with patients with low weight Anorexia Nervosa Experience of managing a clinical service Experience of family therapy Page 11 of 12 Academic Achievements Teaching and Audit Evidence of skills in the psychological formulation of clients The ability to work with, and integrate, psychological formulations alongside psychiatric diagnoses Ability to make links and form effective relationships with colleagues in related services Ability to communicate with clarity and in an empathic, emotionally attuned manner Good written, verbal and interpersonal communication skills Ability to take full responsibility for the independent management of patients Sound knowledge of research methods and understanding of the importance of evidence based medicine Motivation Personal Attributes Committed to formal and informal teaching and training of junior doctors and medical students. Experience of and commitment to, systematic audit of clinical outcomes Committed to patient focused care, learning and continuous professional development, effective and efficient use of resources Honesty, warmth, enthusiasm and efficiency Comfortable in open communication with patients and colleagues alike Commitment to patient-focused care Ability to work effectively in in a multi-disciplinary team and to be able to motivate colleagues Able to organise time efficiently and effectively Ability to co-ordinate the separate components of the service into a coherent whole in conjunction with others Previous experience in research with publications, especially of relevance to eating disorders. Previous experience of teaching Desire to develop services for patients Previous managerial training and experience Page 12 of 12