Not Just Grapes & Flowers
advertisement

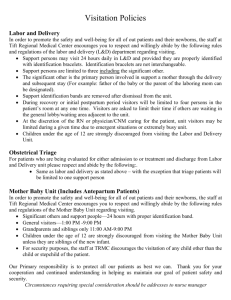
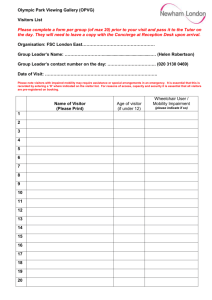
“Not Just Grapes & Flowers” Older People’s Perspectives on the Role and Importance of Hospital Visiting A Service User Controlled Research Project by members of OPRSI [Older People Researching Social Issues]: Barbara Hawkes, Gwyneth Raymond, John Peardon, David Fox, Bert Green, with Dr Michelle Cornes Transcripts by: Mrs Sheila Cornes Funded by a North Lancashire Teaching PCT bursary Introduction: The idea for this research arose from one of our member’s personal experience of hospital visiting. The topic is little covered in the literature let alone from the point of view of older visitors or older patients. Some studies suggest that having visitors increases the wellbeing of the patient and helps their recovery; some health authorities publish guidance and advice for visitors; some hospitals or ward managers restrict visiting times to suit the ward routines or for reasons of hygiene or infection control or they may allow open visiting; some hospital staff welcome visitors, some do not. Our research provides commentary by older people as visitors, or as patients receiving visitors, on that experience and its value to them, given their individual circumstances and those prevailing at the hospital. Methods: Nine focus groups were recorded at locations throughout the region: North Lancashire and South Cumbria, which is served mainly by Royal Lancaster Infirmary, Blackpool Victoria, Westmorland General Hospital at Kendal, Furness General Hospital at Barrow and the Royal Preston; but some participants also spoke about their experience of more remote Hospitals. We tried to interest established groups such as Old Peoples’ Forums and Age UK in participant recruitment and setting up venues, and we were also greatly assisted by local librarians who allowed us to recruit and hold most of our focus groups in some of the Lancashire and South Cumbria libraries. Focus Group Locations: 1 Location of Focus group Garstang Fleetwood Grange-0verSands KirkbyLonsdale Morecambe PoultonLe-Fylde Kendal 1 and 2 Preston GHS Number of participants 6 6 6 4 7 8 9 8 Participant details: Age 50-59 60-69 70-79 80-89 90+ Nil Response Total 2 [4%] Male 10 [18%] Female 12 [22%] 21 [39%] 1 [2%] 8 [15%] 54 Sex 21 [39%] Yes 31 [57%] No 2 [ 4%] 54 Carer 15 [28%] WhiteEnglish 42 [78%] 26 [48%] White-Irish 13[24%] 54 Ethnicity North Indian RLI 1 [2%] B’pool 8 [15%] Barrow WG 3 [5%] Out of Area 54 Hospitals attended 29 15 6 13 Other 7 6 Older people are defined by the NHS as over 50 years so we recruited on that basis. Of the 43 older participants in the focus groups, 65% were over 70 years when the effects of age are likely to be more pronounced. We tried, not always successfully, to direct our discussions towards our participants’ experiences during the previous 6 or 12 months, as any practical suggestions to improve the visiting experience for older people would be more applicable. Full transcripts of digital recordings from the nine focus groups were typed, and these were analysed to identify particular concerns or vivid experiences that we could classify into common themes. We noted apposite quotes to illustrate the themes, and in some instances to provide a narrative of the visiting experience. Key findings: 1. Getting there and back: Older visitors encounter many difficulties travelling to and from the hospitals, parking at the hospitals, and locating the patient’s ward. If they are visiting daily the travel can be exhausting and at times being out in the dark it may be frightening. But they persist because there seems to be no alternative and some older people, who perhaps have never before been separated from the hospitalised family member, feel compelled to visit every day. Quotes: • Distance and time: “as [medical] specialities are [centralised] then distances I suppose get greater”. “...you know, nothing is round the corner”. 2 • • • • • • • • Parking: “...the point about parking [for older people] is that it is stressful”. “...taking older relatives [visiting] ...we had to drop them at the door and then go and find somewhere to park and [we] had to take someone to be with the older person whilst we were parking.” Buses/trains: “...it is difficult to get to [and from] hospital within the visiting times”. “Not all buses take wheel chairs”. Finding the ward: “...corridors are enormously long...there is a need for help with pushing wheelchairs...a location map and an explanation of facilities for visitors...” “It’s very easy to get lost in Victoria unless you can find someone with a badge to take you to the ward.” Signage: “...I lost direction and finished up in the emergency area.” Waiting for wards to open: “...if you are early it’s just standing and I can’t stand a long time” Travel on a winter’s night: “...coming home it was dark ... at the bus stop... teenagers were congregating...it frightened me” Repeated daily journeys: “it made me ill in the end going twice a day” Compulsion: “...I couldn’t do anything if I didn’t see him, I was as good as lost...” 2. On the ward: There are often contradictory views about visiting times and visitor numbers. Older people want behaviour to be controlled on the wards but they also want flexibility in visiting times. Information about the patient is very important to older visitors, for their own peace of mind and to tell to other people in their social world, but this information is not always easy to find from staff on the ward. On wards where a visitor is not considered by the staff or is treated in a perfunctory way, an older person may have their physical and emotional frailty strained by a hospital visit. Staff attitudes can make a big difference to whether the older visitor has a satisfactory visit. Hygiene is a worry both for the patient and the visitor. The older visitor recognises the need to follow the hand washing rules when entering wards. Some older visitors think they are in danger from MRSA infection even though they are quite healthy. Hospitals, it appears, expect that personal laundry will be taken away to be done by visitors, friends or family. What happens when this does not happen was a concern. Participants were concerned that older patients would not be properly fed if they did not have visitors to assist them at meal times, thus they questioned the need for so called ‘protected meal times’ when visiting was not allowed. Quotes: • Visiting times: “Just an hour and a half in the afternoon and an hour in the evening... I would just get home, swallow a sandwich and a cup of tea and off back again”. “... they are flexible so long as you’ve got a good reason...” 3 • • • • • • Numbers of visitors: “I believe patients need a rest and this open visiting where you can come and they bring half a dozen children with them ...climbing on the beds or whatever...I think they should see into that” Getting information about the patient: “I feel I am making a nuisance of myself... overstepping the mark in asking for information”. “Nurses sometimes are very reluctant to express their opinions as to a patients well-being...” “...the doctors might give you 10 seconds in passing”. “I have always had an adequate response [when I phone up the hospital rather than visit]”. “People don’t use the quiet rooms and that is where a lot of information is”. Staff attitudes: “The hospital is a strange place, and they are often strange to you...and you don’t know where to go, who to see, what to do”. “...there is almost no consideration given to the state of mind of the [older visitor], how upset they are, how worried they are.” “They never make eye contact with you as a patient or a visitor”. “ Don’t you think sometimes nurses are glad to see the visitors...they need to see you as well as being a visitor to the patient?” Hygiene: “I always wondered about hygiene when visitors came in...some of the clothes looked like they came straight from work”. “[staff] ask visitors to wash their hands, and so few visitors do it.” “ for years I was apprehensive about visiting hospital ...because of the infections you could pick up...and the hospital became more dangerous than staying at home.” “They talk about cross-infection ...yet bring in children in school uniforms and you might just as well bring in a bag of germs”. Laundry: “my visitors took my clothes away every night”. “The problem is the relationship between the residential home and the hospital is quite weak...you get this void...the follow up [getting clothes laundered] is left to friends”. Meals: “The hospital didn’t have the resources to come round and actually help patients to eat...” “You could be most help at meal times...” “ [the nurse] said oh no not until after 2pm...protected meal times they call it. I’m not sure what they are protecting you from”. 3. The value of visiting: This has many aspects and implications for the older patient and the older visitor. Value for the older patient: a release from boredom; keeping in touch with family and social life; news of the world outside the institution; reassurance you have not been forgotten or abandoned; and showing others you are not alone. Quotes Being visited: “breaks the day up and tells you what is going on outside” “...he couldn’t come and I saw other visitors coming in, that is when you feel your lowest”. “Visitors take clothes home to wash.” “My father preferred me to go as often as I could but not stay long because he got tired.” “The afternoon goes slowly...that’s when the visitor is more welcome.” “...it was hellish in the evening when everybody else was getting visitors...you are thinking to yourself ‘they think I am on my own’...it doesn’t help.” 4 Value for the older visitor: getting information from and about the patient, as consolation possibly for themselves returning home from the visit and to tell to others in their social group; keeping in contact; possibly feeling able to help the patient in some way; and keeping a clear conscience. Quotes Doing the visiting: “the visitor is a sort of patient’s spokesperson, there needs to be someone on the ward available for the visitor.” “ Visiting daily kept my conscience clear.” “Visiting consoled me...I could leave him, go home and feel he was a little better.” “...you are going to be upset if you don’t see what you want to see...but once they start improving I think it does you as much good as the patient.” “ to help at meal times ...because almost certainly [the patient ] will be ignored if they haven’t eaten up.” “When you go and actually see somebody...you make your own assessment...and the patient knows there is someone outside thinking of them.” 4. Other themes: Dementia: visitors to patients with dementia are aware of their special vulnerability and that this aspect of their condition has no cure, thus inevitably on many occasions the older visitor returns home feeling pretty low or even depressed. Quotes Dementia: “he has no relatives...the solicitors have responsibility for his appearance, basically...look at their nails, look at their appearance and hope that follow up is taking place with the administration...” “she wasn’t able to eat for herself...of course the hospital didn’t have the resources to actually help the patient to eat.” “...in the case of mum...very anxious most of the time...distressed...and nothing could be or was done about that, left us going away feeling pretty low.” “you know they are not going to get any better...you come home feeling distressed, don’t you?” End of Life: visitors are bringing news from their social world, which sometimes may be unwelcome to the patient; for example news of a death in the family. How this is conveyed and the consequence for the state of mind of the patient has to be considered by the visitors and the staff. Quotes End of life: “...staff should not always listen to the patient if that patient needs feeding...I mean she was like a skeleton when she died.” “They had come to tell me my wife had died...the Sister said to them ‘Mr A will be upset...we have a private room ...he can go in there for a few days’.” Recommendations: The times and rules for visitors make a considerable difference to the experience of visiting, both for the older patient and their older visitors. These should be reviewed. 5 Given the importance for older visitors of the response they get from staff, the way nurses, doctors and consultants perceive older visitors and the way they behave towards them, should be reviewed. Consider the potential of older visitors to help improve the welfare of the older patient. Consideration should be given to locating older peoples’ wards where they can be accessed more easily by older visitors. ------------------------------------------------ We would like to acknowledge and thank for their encouragement and practical help: Kate Casey, Sara Morris, Ros Way, Linda Robinson, Tracey Pratchett, and local Age UK and library staff in Lancashire and Cumbria, and all those older people who came to our discussion groups and shared their experiences with us. Appendix 1: Hospital visiting literature: Our literature search was made possible with assistance from the library service at Morecambe Bay Health Library and Knowledge Service, as we do not have direct access to the specialist web sites and journals containing the published research papers. This is a problem for the lay or user researcher and a limitation on this stage of the research process. For example: the study by Silva, Lucia et al (2005) aimed to understand the interactive experience of visiting family members and companions of hospitalized adult and elderly people and to develop a theoretical model of this experience; the abstract looked interesting but we did not have the article, which is in Portuguese. From our limited searches it seemed that the literature of hospital visiting hardly refers at all specifically to older people’s experience; a number of articles relate to older people visiting or being visited in care homes, but not in hospital. However we did find some articles and studies addressing issues of more general application. From the start nurse Plowright’s article (2007) influenced our thinking about the project and our analysis of older respondents’ experiences; and her observation from a nursing perspective that visitors’ needs are not always being met was broadly confirmed in our findings with older people. Ismael & Mulley’s article (2007) gives a succinct overview of visiting and suggests ‘a shift in culture is needed to ensure best practice on visiting policies’. Whether the policy guidelines for Northern Ireland introduced in 2008, referred to by McGimpsey, achieve this is yet to be seen. Such policies would be implemented by nurses and effectively depend on the nursing culture. 6 Some studies attempt to examine the influence of visiting in terms of negative effects on the physiology of patients or the need for rest in environments such as ICU wards, but these studies are inconclusive and probably do not provide the justification for limited visiting hours [Whitis G, 1993]. On the contrary visitors at any time can offer patients reassurance, comfort and calming, for example, and can assist the nurse in understanding the patient [Gonzalez C. et al, 2004]. Meyers T. et al studied family presence during emergency care and found there were no ill psychological effects; the family perceived it as a positive experience and were not disruptive during their visits; almost all of the nurses approved as did the great majority of attending physicians; only the residents [junior doctors] were markedly less supportive. Other papers examine the relationship between nursing and caring, and it is suggested that there is a need for unpaid carers, who incidentally made up 28% of our older respondents, to be regarded as a resource by hospital ward staff [Macleod M. et al, 2005]. Hospital policies may restrict visiting times or may favour open visiting, in some hospitals when and for how long visiting is allowed may vary between wards according to established nursing practice and the organisation of the ward. The preference for hospital visiting hours for readers of the publication ‘Nursing Management’ [Oct 2001] were: 37% any time 6am to 10pm/ 32% open and flexible 24 hours a day/ 21% at the discretion of the patient’s nurse; 10% limited to 2-hour periods per day. Bibliography Ismail S & Mulley G. ‘Visiting Times’. BMJ, 22-29 Dec 2007, Vol 335 Plowright C. Visiting practices in hospitals. Nursing in Critical Care 2007 McGimpsey M. Outlines new hospital visiting guidelines. northernireland.gov.uk . June 2008 Silva, Lucia; Bocchi, Silvia Cristina Mangini. Revista Latino-Americana de Enfermagem, March 2005, vol./is. 13/2(180-187),0104-1169;15188345 Whitis G. Visiting hospitalised patients. Journal of Advanced Nursing, 1994,19.85-88 Gonzalez C E et al. Visiting preferences of patients in the ICU and in a CCMU. American journal of critical care, May 2004, vol13, No.3. Gottlieb J A K. Time to care: the evolution and meaning of family visiting policies in the ICU. International journal of human caring. 2003. Vol.7, No.2 Meyers T A et al. Family presence during invasive procedures & resuscitation. American journal of nursing. 2000; 100(2):32-42 Macleod M, et al. To what extent are carers involved in the care and rehabilitation of patients with hip fractures. Disability and Rehabilitation, 2005:27(18-19): 1117-1122 Moola S. (2009) Review summaries: Smith L. et al The impact of hospital visiting hours policies on paediatric and adult patients and their visitors. Journal of advanced nursing, 2009, 65(11), 2293-2298 Parish C. Norovirus kept under control and ward closures limited by reducing visiting hours. Nursing Standard Feb 6: vol22No22:2008 Nursing management. How flexible should visiting hours be? nursingmanagement.com, www.nursingmanagement.com, Oct 2001 thedeafsherlock.blogspot.com. The importance of hospital visitation. 17.12.2008 BG, April 2011 7