Can dialysis catheter colonisation be significantly reduced if the
advertisement
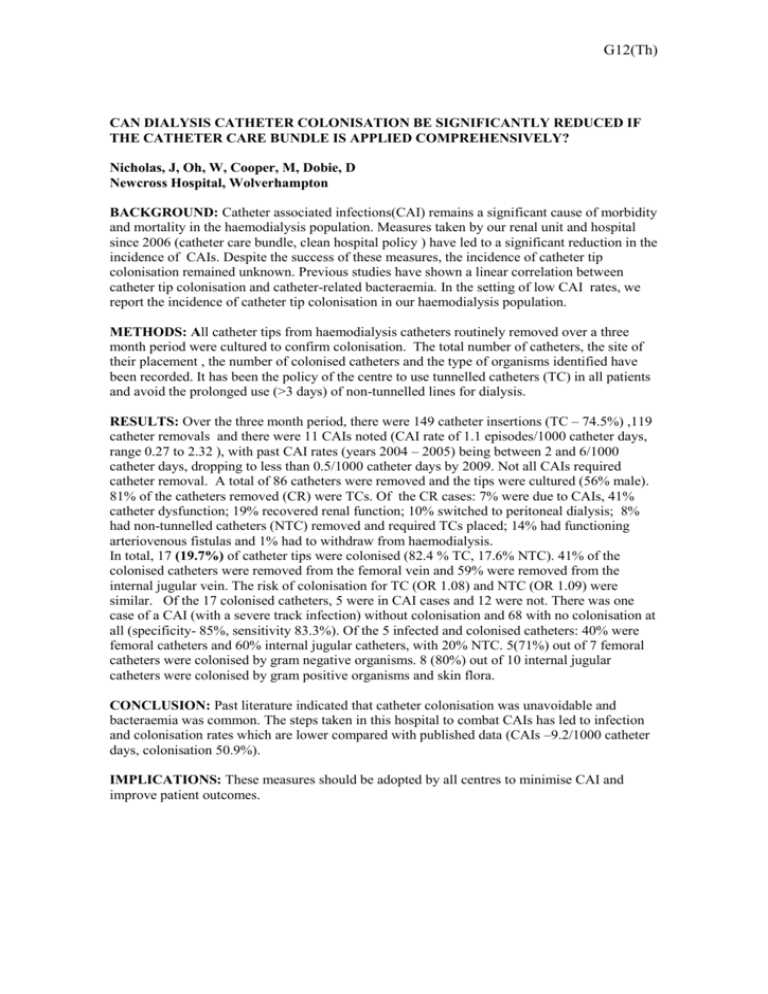
G12(Th) CAN DIALYSIS CATHETER COLONISATION BE SIGNIFICANTLY REDUCED IF THE CATHETER CARE BUNDLE IS APPLIED COMPREHENSIVELY? Nicholas, J, Oh, W, Cooper, M, Dobie, D Newcross Hospital, Wolverhampton BACKGROUND: Catheter associated infections(CAI) remains a significant cause of morbidity and mortality in the haemodialysis population. Measures taken by our renal unit and hospital since 2006 (catheter care bundle, clean hospital policy ) have led to a significant reduction in the incidence of CAIs. Despite the success of these measures, the incidence of catheter tip colonisation remained unknown. Previous studies have shown a linear correlation between catheter tip colonisation and catheter-related bacteraemia. In the setting of low CAI rates, we report the incidence of catheter tip colonisation in our haemodialysis population. METHODS: All catheter tips from haemodialysis catheters routinely removed over a three month period were cultured to confirm colonisation. The total number of catheters, the site of their placement , the number of colonised catheters and the type of organisms identified have been recorded. It has been the policy of the centre to use tunnelled catheters (TC) in all patients and avoid the prolonged use (>3 days) of non-tunnelled lines for dialysis. RESULTS: Over the three month period, there were 149 catheter insertions (TC – 74.5%) ,119 catheter removals and there were 11 CAIs noted (CAI rate of 1.1 episodes/1000 catheter days, range 0.27 to 2.32 ), with past CAI rates (years 2004 – 2005) being between 2 and 6/1000 catheter days, dropping to less than 0.5/1000 catheter days by 2009. Not all CAIs required catheter removal. A total of 86 catheters were removed and the tips were cultured (56% male). 81% of the catheters removed (CR) were TCs. Of the CR cases: 7% were due to CAIs, 41% catheter dysfunction; 19% recovered renal function; 10% switched to peritoneal dialysis; 8% had non-tunnelled catheters (NTC) removed and required TCs placed; 14% had functioning arteriovenous fistulas and 1% had to withdraw from haemodialysis. In total, 17 (19.7%) of catheter tips were colonised (82.4 % TC, 17.6% NTC). 41% of the colonised catheters were removed from the femoral vein and 59% were removed from the internal jugular vein. The risk of colonisation for TC (OR 1.08) and NTC (OR 1.09) were similar. Of the 17 colonised catheters, 5 were in CAI cases and 12 were not. There was one case of a CAI (with a severe track infection) without colonisation and 68 with no colonisation at all (specificity- 85%, sensitivity 83.3%). Of the 5 infected and colonised catheters: 40% were femoral catheters and 60% internal jugular catheters, with 20% NTC. 5(71%) out of 7 femoral catheters were colonised by gram negative organisms. 8 (80%) out of 10 internal jugular catheters were colonised by gram positive organisms and skin flora. CONCLUSION: Past literature indicated that catheter colonisation was unavoidable and bacteraemia was common. The steps taken in this hospital to combat CAIs has led to infection and colonisation rates which are lower compared with published data (CAIs –9.2/1000 catheter days, colonisation 50.9%). IMPLICATIONS: These measures should be adopted by all centres to minimise CAI and improve patient outcomes.