Volume 8 (Number 2) - The Ethiopian Journal of Health Development
advertisement
yx!T×ùÃ -@Â L¥T m{ÿT
THE
ETHIOPIAN
JOURNAL
OF
HEALTH
DEVELOPMENT
OFFICIAL ORGAN of THE ETHIOPIAN PUBLIC HEALTH ASSOCIATION
Volume 8
Number 2
August 1994
The Ethiopian Journal of Health Development
EDITORIAL BOARD
Editor-in-Chief: Asfaw Desta
Associate Editor-in-Chief: Derege Kebede
Gebre-Emanuel Teka
Hailu Yeneneh
Tesfaye Bulto
David Zakus
Hailegnaw Eshete
Mehari Woldeab
Tigest Ketsela
Zewdie Wolde-Gebriel
Publication officer: Simon Tekle-Haimanot
Secretary: Meskerm Buzuayehu
________________________________________________
Jointly Sponsored
by
The Ethiopian Public Health Association & The Addis Ababa University
The Editorial Office of the Ethiopian Journal of Health Development
is the Department of Community Health, Faculty of Medicine, Addis Ababa University.
The Ethiopian Journal of Health Development P.O.Box 32812, Addis Ababa, Ethiopia.
Telephone: 157701 or 518999 ext.7, FAX: (251-1) 517701
Addis Ababa University
Faculty of Medicine
Department of Community Health
ANNOUNCEMENT
The Department of Community Health in the Faculty of Medicine of Addis Ababa University wants
interested individuals to be aware of the Master of Public Health Degree Program which will welcome a new
class of students in September 1992.
The program includes basic postgraduate courses in Management, Epidemiology, Biostatistics, Maternal
and Child Health, Health Education, Environmental Health and Nutrition. Another vital part of the curriculum is
the Community Health Residency in an Awraja Health Department or its equivalent.
The candidate's individual interests and career plans can be pursued in an area of concentration and thesis
research. The applied research project is carried out during the second year, usually in the location of the
Community Health Residency.
The program continues for 22 months from September 1992 until July 1994. Application forms are
available at the Registrar's Office in the Sidist Kilo Campus of the University. All documents must be submitted
to the Registrar's Office between March and May 1992. Equally important is obtaining letters of support from
institutions which plan to utilize the new knowledge and skills acquired by the trainee. Most candidates are
sponsored by the Ministry of Health. The Department encourages other institutions to do likewise.
Prospective students must have at least a baccalaureate degree, previous training in a health or related
professions, and at least two years' experience in health or related services. Other academic requirements are as
specified in the application form of the School of Graduate Studies of the University.
If you have inquiries please forward them to Dr.Derege Kebede, Head, Dept. of Community Health,
Faculty of Medicine, P.O.Box 1176, Addis Ababa.
Fax: 251-1-51-77-01
-----------------------
INFORMATION FOR CONTRIBUTORS
1. The Ethiopian Journal of Health Development is a multi-disciplinary publication concerned with the broad field of health development. The Journal
publishes analytical, descriptive and methodological papers, as well as original research, on public health problems, management of health services, health
care needs and socio-economic and political factors related to health and development. Book reviews, letters to the editor, news items and short
communication are also acceptable. Articles which support the goals of "Health for All by the Year 2000" through the primary health care approach are
particularly welcome. Contributions from and/or about developing countries in general and African countries in particular will be given priority. The
following is a representative, but not exhaustive, list of subjects of interest to the Journal: health policy and health politics, health planning, monitoring and
evaluation, health administration, organization of health services, hospital administration, health manpower, including training, health statistics/health
information systems, maternal and child health and family planning, environmental health and water, food and nutrition, communicable diseases, health
education, epidemiology, community involvement, intersectoral activities, health economics/financing of health department, health technology, drug supply
and distribution, international health organizations/technical cooperation among developing countries.
2. All manuscripts should be submitted to the Editor of the Journal. Manuscripts will be considered for publication on the understanding that they have not
been previously published and are not simultaneously submitted or published elsewhere. This does not refer to papers presented orally at symposia or other
proceedings. Each manuscript will be assessed by at least two reviewers knowledgeable in the relevant subject. Manuscripts that are accepted for publication
become the property of the Journal; rejected manuscripts will be returned to the author.
3. Manuscripts should be submitted in triplicate, typewritten on one side of quarto or A4 paper with double spacing and liberal margins. There should be a
single separate title page containing the title, each author's full name, with the senior author listed first, organization or institution where the work was done,
each author's present address if different and the name and full postal address of the author to whom correspondence should be addressed.
Acknowledgements of those making substantive contributions to the paper, and any relevant informations such as if the paper was presented at a meeting or
is part of a large study should be noted at the end of the manuscript. A short summary or abstract should be included on a separate page.
4. The language of the Journal is English. Articles of national importance written in Amharic might be accepted for special issues.
5. References should be cited in the text as consecutive, bracketed numbers. Those appearing for the first time in tables or figures must be numbered in
sequence with those cited in the text. References in numerical sequence should be listed on a separate sheet, double-spaced, at the end of the manuscript. It is
the author's responsibility to verify that all references are accurate and complete. Titles of journals should be cited in full. References should give the full
facts of publication. For a book, these are; full name of the author(s) or editor(s); year of publication; full title of the series, if any, and volume number;
publisher's name and city of publication; page number(s) of the citation. For an article in a journal: author's full name; title of the document; information
identifying the source and location, date; Ph.D. dissertation (include department and institution), paper presented at a workshop (include name, location,
month and year of workshop), mimeo or photocopy (include department and institution). References to personal communications should be placed in
brackets in the text, giving the full name and date. Ethiopian names should be referred to in accordance with national usage, e.g. Taye Daniel as Taye Daniel
but will be cross-referenced in indexes as, e.g. Daniel, Taye. 6. Tables should supplement not duplicate the text, unnecessary and lengthy tables are
discouraged. Each table should be typed (double-spaced) in triplicate, on a separate sheet, numbered and given a suitable title. The approximate place in the
text should be indicated. Place explanatory material in footnotes. Figures and illustrations should be submitted in triplicate. They should be unmounted,
black and white glossy prints of line drawings or photographs; do not send original art work or negatives. Each figure or illustration should be given a
number, the author's name lightly marked in pencil on the back and a brief caption, double-spaced, should be typed on a separate sheet. If it is not possible to
provide glossy prints of figure, they should be accurately drawn in black ink on good quality white paper and the numbers and wording should be typed on an
overly of tracing paper, not on the figure itself. Coloured illustrations will be reproduced at the author's expense.
7. Miscellaneous. The generic names of drugs should be used; if necessary, the proprietary name may be placed in parenthesis after the generic name. When
percentages are used in case studies, the actual numbers should be indicated as well. e.g. 39/75, (52%). The first time an abbreviation or acronym is used it
should be preceded by the full name for which it stands.
8. Twenty reprints will be supplied free to the senior author. Additional reprints may be ordered and paid for in advance.
9. The Editorial Board reserves the right of final acceptance, rejection and editorial correction of papers submitted. Authors are responsible for all statements
made in their work including changes made by the copy editor. Priority and time of publication are governed by the Editorial Board's decision.
ANNUAL SUBSCRIPTION RATES
Ethiopian Journal of Health Development, P.O.Box 32812, Addis Ababa, Ethiopia. The Journal will publish at least two issues a year.
Ethiopia (in Birr) institutional 18 (annual) & 10 (single), individual 12 (annual) & 7 (single), student 8 (annual) & 5 (single). Africa (in U.S$) institutional 18
(annual) & 10 (single), individual 12 (annula) & 7 (single), student 8 (annual) & 5 (single). Overseas (in U.S$) institutional 25 (annual) & 15 (single),
individual 18 (annual) & 10 (single), student 12 (annual) & 7 (single). All prices include postage (airmail outside if Ethiopia). Checks should be made out to:
Chairman, Dept. of Community Health, Addis Ababa University.
The Ethiopian Journal of Health Development
Volume 8 Number 2 August 1994
DEDICATED TO THE SOCIAL GOAL OF
HEALTH FOR ALL
THROUGH THE PRIMARY HEALTH CARE APPROACH
CONTENT
ORIGINAL ARTICLES
HEALTH IN ETHIOPIA: A SUMMARY OF 52 DISTRICT HEALTH PROFILES
Charles P. Larson, Tadele Desie …………………………………………………87
SOME CHEMICAL CONSTITUENTS OF SELECTED WATER SOURCES
IN AND AROUND ADDIS ABABA AND AMBO
YesehakWorku, SinkneshEjigu………………………………………………… 97
CARE GIVERS' KNOWLEDGE, BELIEFS, ATTITUDES AND PRACTICES
ON CASE MANAGEMENT OF ACUTE RESPIRATORY ILLNESSES
IN A RURAL DISTRICT IN ETHIOPIA
Saba Woldemichael, DennisG. Carlson, Derege Kebede ………………………103
THE IN VITRO ANTIBACTERIAL ACTIVITY OF "T AZMA MAR "
HONEY PRODUCED BY THE STINGLESS BEE
Mogessie Ashenafi ……………………………………………………….……109
BRIEF COMMUNICATION
RETROSPECTIVE STUDY OF CERVICAL CARCINOMA: 1988-1992
Feleke Bojia, Amare Dejene, Yared Mekonnen …………………….………119
UPDATE
AIDS CASE SURVEILLANCE IN ETHIOPIA: APRIL 30, 1994
National AIDS Control Program, Ministry of Health
EXCERPTS FROM TRANSITIONAL GOVERNMENT'S PROCLAMATION
NO41/1993ANDHEALTHPOLICY .………………………………………139
HEALTH IN ETHIOPIA:
A SUMMARY OF 52 DISTRICT HEALTH PROFILES
Charles P. Larson, MD, MSc, FRCP(C) 1, Tadele Desie, MD MPH2
ABSTRACT: This paper integrates the data contained in 52 district health profiles completed during the
years 1988 to 1991. These profiles encompass approximately 40% of the Ethiopian population and thus
provide a summary assessment of health services and health status. Thirty percent of children were found to
be attending school, 33% of children under five years of age were malnourished, and 35% of the population
had access to safe water. The analysis was stratified by districts, urban versus rural populations, and hospital
versus non hospital health institutions. Large disparities between districts were found in measures of health
and human development. On a per capita basis, urban districts benefit from three times the number of
physicians, four times more nurses, and double the number of health assistants. Nearly 70% of physicians
and nurses were hospital based. Of the 1.88 birr per capita yearly health expenditure, hospital budgets
accounted for 60%. This summary review of health profiles provides baseline data on the health of
Ethiopians early in the establishment of district health services from which future trends can be monitored.
[Ethiop. I. Health Dev. 1994;8(2):87-96].
INTRODUCTION
The planning and management of health services in lesser developed countries often proceeds within an
environment of inadequate information about the health status of the populations served and the occurrence
of important determinants of health. This is particularly the case at the district level where health services
have traditionally been underdeveloped and information systems lacking (1,2). Recognizing these
weaknesses, assignment as a district health manager and the completion of a district health profile (HP) have
been cornerstones of Ethiopia's two recently established health management training programs. The first of
these is a two year Masters of Public Health (MPH) course taught in the Department of Community Health,
Addis Ababa University (DCH-AAU) and the second was the Accelerated District Health Managers
(ADHM) course given at the Training and Demonstration Centre, Ministry of Health (TDC-MOH) (3,4).
Trainees are provided with in-depth classroom instruction in the preparation of a health profile, given a
detailed reporting outline, and then supervised in the field by faculty during the profile preparation. These
profiles bring together existing information on the health status and occurrence of important health
determinants in a district. Additional information is then gathered through interviews, surveys, and
epidemiologic research. The purpose of this report is to summarize the information contained in the health
profiles submitted by trainees in the two training programs. By combining the information contained in the
district health profiles, a profile representative of the country as a whole is expected to emerge Collectively
the analyses presented {J,.)vidt: a Cvst efficient, alternative source of national health information useful in
assessing Ethiopia's progress towards national health goals .
METHODS
All health profiles completed by a trainee in either the MPH or ADHM course between 1988 and 1991 were
eligible for inclusion in this review. Health profiles on file at the MOH- TDC or in the DCH-AAU were
identified and checked for completeness. Next, each was reviewed according to
a prearranged format and data related to health status and determinants were recorded. From Figure 1 it can
be seen that 56 profiles were found. In two instances a district had had two profiles completed; in which case
the most recent was used. Due to the geographic redefinition of districts in 1989, there is some additional
population overlap between profiles. Profiles were judged to be urban if more than 50% of the population
with access to health institutions was urban. This included districts making up Addis Ababa and several
regional capitals.
_____________________________
1Department
2Health
of Epidemiology & Biostatistics McGill University, 1020 Pine Avenue West Montreal, Quebec, Canada H3A 1A2
Services Branch Ministry of Defense of Ethiopia, Addis Ababa
In several instances specific data contained in a HP were rejected. Morbidity and mortality rates had to be
derived from data generated by the district health service. Data were excluded in those instances where it
were evident it had been extracted from national or regional statistics, such as the 1984 census, rather than
from the district. Also excluded were data which seemed highly improbable and could not be verified from
the information provided in the HP. On several occasions rates were calculated or corrected based upon the
frequency counts and denominators provided.
One HP, following review by three individuals, was judged to be unreliable and was therefore excluded.
Finally, a fourth was a profile of a military population and it was also excluded. All data were entered and
analyzed using EPI-INFO version 5.0, Overall and mean figures for urban and rural districts were determined
on the basis of the newnber of occurrences per total population at risk. Ringes stem from a similar
calculation, but were calculated separately for each district.
DISTRICT HEALTH PROFILES REVIEW
56 HEALTH PROFILES
52 HEALTH PROFILES
URBAN
ADHM
N=3
RURAL
MPH
N=13
ADHM
N= 13
MPH
N=24
Figure 1. Results of search and inclusion of health profiles (ADHM: Accelerated District Health Managers' course MPH: Masters of Public
Health Course)
RESULTS
DEMOGRAPHC: The 52 HPs covered a total population of approximately 22,970,000 people (about 40%
of Ethiopia's total population), Wherever possible, the results will be presented separately for urban and rural
districts, but it is to be pointed out that in most instances districts are made up of sizeable numbers of both.
The average population of a rural district was 478,000 (range 49,000 to 1,905,000) and urban 360,000 (range
41,000 to 1,399,000).
As seen in Table 1, 75% of the population resided in predominantly rural and 25% in predominantly urban
districts. This urban over- representation is explained by two factors: first, urban centers tend to have better
developed health institutions; and second, district health managers are more likely to be assigned to districts
with the best physical facilities and therefore to the larger urban centers as opposed to remote, entirely rural
districts. The age distribution is essentially the same in rural and urban districts. The median age was found
to be between l8 and 19 years and the overall dependency ratio is high, at 0.83. Women of childbearing age
(15 to 49 years) make up 20% of the population.
Table 1. Age Distribution of the Population Covered by health Profiles (to nearest 1000) (1988-91)
Age
Rural
Urban
Total
N (%)
N (%)
N (%)
0-4
5-14
15-64
>64
Total
2,581,000 (15)
4,817,000 (28)
9,291,100 (54)
516,000 (3)
17,205,000
807,000 (14)
1,499,000(26)
3;287,000(57)
173,000(3)
5,766,000(25)
3,388,000(15)
6,316,000(27)
12,578,000(55)
689,000(3)
22,971,000(100)
Crude (unadjusted) birth, death, and growth rates are summarized in Table 2. The large difference in growth
rates between rural and urban districts is almost entirely explained by the higher rural birth rate. The overall
crude growth rate of 25.4 per 1000 population is high, but is. probably a conservative estimate given the bias
in district assignment previously mentioned. In contrast to the high birth rates, contraception use is
exceedingly low and in many districts approaches zero.
Table 2. Summary of Crude Demographic Rates. (1988-91)
Rate
Crude Birth Rate*
Crude Death Rate*
Crude Growth Rate*
Contraception
Prevalence Rate**
*Per 1000 Population
*per 100 females 15-49 years of age
RURAL
Mean (range)
43.8 (25.6-58.0)
17.0(8.5-40.7)
29.5(6.6-45.4)
URBAN
Mean (range)
33.9(12.2-46.0)
17.3(12.2-22.0)
23.9(17.2-29.6)
OVERALL
mean
42.5
17.1
25.4
2.29(0.3-8.0)
4.2(0.5-14.0)
2.9
The wide ranges found among these demographic rates are to be noted. The upper crude birth rate estimate of
58.0 births/1000 population is based upon a well conducted survey carried out in an eastern Ethiopian
district. The lower estimate of 12.2 is based upon a community household survey carried out in an Addis
Ababa district. Given the wide inter-district disparities, the precision of national estimates will be greatly
influenced by the number and spectrum of communities surveyed.
HEALTH and DEVELOPMENT: In the absence of routine reporting of vital statistics reliable district
mortality figures are difficult to obtain. The most frequently occurring and best documented is the infant
mortality rate (IMR). The overall IMR was 114 infant deaths per 1000 live births. As expected, the IMR was
lower in urban than rural districts; urban,107 (range 38.0-155) and rural,116 (range 54.6-195). Nearly all
health profiles contained a listing of the 10 most frequently diagnosed conditions seen by health centers and
health stations. These tables are to be interpreted with considerable caution. First, diagnostic accuracy,
capacity, and range will vary between institutions and is generally symptom or complaint focused. For
example, trachoma and tuberculosis are rarely found among the top 10 diseases, yet they are known to be
highly endemic throughout Ethiopia. Second, lists conform to prearranged diagnostic categories which
involve an overlapping array of symptoms. Third, certain diseases will vary considerably in occurrence
between districts and regions due to environmental factors such as altitude and sources of water. Finally, in
many instances the actual number of cases diagnosed is not recorded or the numbers reported are not
internally compatible. Table 3 includes the 10 most frequently listed d:agnostic categories.
Table 3. Ten Most Frequently Cited Outpatient Diagnostic Categories in Health Institutions (Hospitals,
Health Centers, Health Stations) (1988-91)
1. Helminthiasis
2. Respiratory Infection
3. Diarrheal Illness
4. Gastritis Diseases
5. Malaria
6. Lacerations/Injury
7. Malnutrition
8. Sexually Transmitted
9. Skin Diseases
10. Rheumatism
Table 4 summarizes three additional measures of health and development. The proportion of children in
school was calculated by taking the total elementary and secondary school enrolment figures and dividing
this by the total population of 5-14 year-olds. If a significant proportion of students are over 14 years old, this
calculation will result in a 'generally more favourable estimation of school enrolment. The figures are fairly
similar in rural and urban districts, with the overall proportion of children enroled being about 30% .In one
rural district only 2% of eligibles were enroled, yet a few districts exceeded 50% .
Rates of malnutrition fluctuated widely by district and were considerably higher in the rural districts, where
over one-third of children under five years of age suffer from protein-energy malnutrition. Access to safe
water, defined as piped water or a protected source, was present among 27% of the population. In several
urban, Addis Ababa districts access approaches 100% . These figures address access and not actual practices.
Many urban poor continue to obtain water from unsafe sources.
Table 4. Indices of health and Development (1988-91)
Index
5 to 14 year olds in school
Under five Malnourished
Access to safe water
RURAL
% (range)
33 (2-48)
37 (3-65)
27 (3-68)
URBAN
% (range)
26 (9-55)
21 (15-28)
47 (14-99)
ALL
%
30
33
35
HEALTH SERVICES: Table 5 lists the health institutions found in the districts and per capita or catchment
population estimates for these facilities. From these figures it is evident that rural based hospitals are far
fewer in number and serve much larger catchment populations. The distribution of health centers and health
stations is somewhat comparable in rural and urban districts. Catchment populations, on average, for health
centers and health stations in rural districts are 302,000 and 26,000, and. in urban areas are 251,000 and 29,
700, respectively. Health posts, which are constructed by communities at their own cost, were found in only
one out of every 20 rural peasant associations (1:45,000 population). Access to health services can be defined
either in terms of distance (within 10 kIn) or time (within lor in some cases 2 hours travel time). Using
distance as the criteria, only 23 of the 52 HPs provided data on access. Of the seven urban districts providing
access data, 6 reported 100% access. Among the 16 rural districts, 51% of the population had access, with the
range between districts being 32 to 85% .
Table 5. Health Institutions Found in the Districts (1988-91)
Institution
Rural
Urban
N (N (per capita)
N (per capita)
Hospitals
Health Centres
Health Stations
18 (1:956,000)
57 (1:302,000)
672 (1:26,000)
34 (1:170,000)
23 (1:251,000)
194 (1:30,000)
Using the total population as the denominator (not just those with access), Table 6 summarizes the utilization
findings for maternal and child health services. In several instances it was not possible to distinguish between
total antenatal care visits and total number of women enroled, therefore the antenatal care percentages found
in - Table 6 may be artificially high. From this table, it can be seen that obstetrical services are far better
utilized in the urban districts, while well child care is better utilized among rural populations. This latter
figure may be partially explained by the presence of private clinics in the urban districts. All three utilization
rates are low, with attended deliveries the least, at less than 10% overall.
The number of OPD visits were recorded in nearly all the BPs. Taking the total number of OPD visits, the
per capita annual number of visits is 0.23 overall, with the mean for urban nearly double that of rural
districts; urban 0.32 (range ,08-.94) vs rural 0.17 (range .03-.46).
Table 6. Utilization of Health Services (1988-91)
index
RURAL
URBAN
% (range)
% (range)
Antenatal care
23 (3-68)
33 (5-56)
Attended delivery
7 (1-32)
11 (4-15)
Well child care
27 (2-71)
14 (5-29)
ALL
%
25
8
25
Immunization coverage rates are found in Table 7. These rates can vary considerably, depending upon how
the denominator is defined. The rates reported in Table 7 are based upon the total number of vaccines given
over the preceding one year divided by the number of expected births. They have not been adjusted for infant
mortality over the first year of life, thus inflating the denominator for DPTJ and measles by about 10% .As
can be seen, coverage rates vary a great deal between districts, in particular the rural. Overall, approximately
one-quarter of all children were found to be fully immunized by one year of age.
Table 7. Immunization Coverage (1988-91)
Vaccine
BCG
DPT3
Measles
Coverage
Rural % (range)
49 (1-90)
25 (1-73)
26 (1-69)
Urban % (range)
65 (39-88)
42 (28-71)
38 (19-62)
Overall %
51
27
28
HEALTH PERSONNEL: Per capita health manpower figures are summarized in Table 8. This table
provides overall and rural vs urban per capita manpower ratios, as well as between district ranges. The ranges
do not include districts where there are zero workers of a particular category .Secondary calculations were
carried out for non-hospital need manpower ratios. These include all physicians, nurses, and health assistants
employed outside a hospital; in nearly all cases a health centre or health station. Finally, for community
health agents (CHA) and trained traditional birth attendants (TTBA) a secondary calculation is found which
includes only fuose who are known to be functional. A community health worker is defined as functional on
the basis of continued, quarterly reporting to their supervising health station. This definition is less restrictive
than that of the MOH, which expects at least 6 reports per year. Therefore we may be overestimating
community health worker availability.
The overall physician-to-population ratio was found to be one per 52,000 population. The ratio is nearly three
times higher for rural vs urban districts and this difference is largely explained by the relatively large number
of urban, hospital-based physicians. These figures do not include private clinics, which are few in number
outside Addis Ababa. In total, 58% of the physicians are located in the urban districts and 83% are hospitalbased. In five districts, four rural and one urban, there were no physicians at the time the HP was completed.
The nurse-to-population ratio was found to be one per 17,000 population. Again, there are large rural vs
urban disparities, with the ratio nearly four times greater in the rural districts. If one includes only those
nurses working outside a hospital setting, the per capita ratio is increased to I :47 ,000 population. From the
total, 52% of the nurses are located in the urban districts and 63% are hospital employed. In six urban
districts, there were no nurses working outside a hospital. A total of 108 sanitarians and 123 pharmacists or
pharmacy technicians were identified in 49 of 52 HPs. These represent per capita ratios of 1:203,000 and
1:178,000, respectively. In Ethiopia health assistants (HA) are considered to be the first point of contact with
health institutions. They are found at all institutional levels and have been trained to carry out preventive,
diagnostic, and curative activities. The overall ratio of HA to population was found to be 1:5,200. When
comparing urban to rural districts, the ratio is more than doubled in the latter. This discrepancy is also largely
explained by the increased number of hospital employed HAs in urban settings. From the total, 61% of HAs
are located in rural districts , however the majority, 52% , are hospital based.
Community health agents (CHAs) and trained traditional birth attendants (TTBAs) are community based
health workers supported by their communities. They have been nominally trained, but are not employed by
the Ministry of Health. They are supervised from the nearest health station or health center by a health
assistant to whom they are expected to report on a quarterly basis. The per capita ratios in urban and rural
districts are similar, whether examined in terms of the total trained or those actively reporting to a health
station, the latter being one per 12,000 population. Assuming the average village population to be 2,500,
approximately one in three can be expected to have either a functioning CHA or TTBA.
Table 8. per Capita Distribution of health manpower (per 1000 population) (1988-91)
Profession
Physicians
All Non-hospital Nurses
All
Non-hospital Health Assistants
All
Non-hospital Community Health
Agents
All
Functional Traditional Birth Attend.
All
Functional
Rural Ratio
(range)
1: 89 (11-571)
1: 302 (25 - 1905)
1:29 (4.1 -106)
1:50 (8.2 -212)
1:7.4 (1.3 - 19)
1:11 (2.4 -35)
Urban ratio (range)
Overall ratio
1:29 (3.8 - 82)
1:251 (33 - 1399)
1:8.0 (2.4 -36)
1:3.39 (5.1 - 155)
1:3.3 (0.9 - 13 )
1:15 (2.2 -57)
1: 52
1:287
1:17
1:47
1:5.8
1:12
1:4.5 (1.1 - 16)
1:12 (2.0 -105)
1:5.0 (1.5 - 37)
1:13 (4.4 -244)
1:5.1 (1.1 - 22)
1:14 (5.0 - 60)
1:6.2 (1.3 -15)
1:11(2.7 -29)
1:5.2
1:12
1:5.2
1:13
HEALTH SERVICES FINANCING: Health services are financed through fixed, global budgets. At the
time these health profiles were completed the districts did not have budgets of their own. They were
supported through a redistribution of resources from the existing health institutions in the district. The
proportional breakdown by cost category is nearly identical across districts, with the current allocation found
to be 69% for salaries (range 48% to 90%), 16% for drugs (range 6% to 41 %), and 12% for operational costs
(range 2% to 33% ). Not includes ;n these figures are costs related to the Ministry of Health central and
regional headquarters, its divisions (e.g. rnatemal and child health, epidemiology, planning, etc.), and vertical
programs (e.g. diarrhoeal disease, malaria and tuberculosis control programs). Also not included are funds
received through multilateral (UNICEF, WHO) or bilateral contributions (including non- governmental
organizations). With these exclusions in mind, the overall per capita expenditures on health in the districts is
1.88 birr (about 0.95 $US)/person/year.
Approximately 60% of total expenditures are allocated to hospitals. If one considers only those districts with
a hospital, on average, 70% of government health expenditures are consumed by the hospitals. The range in
per capita expenditures between districts is extremely wide. As can be seen over 20 birr/person was expended
in one urban district, while in one rural district only 0.10 birr/person was allocated to health services.
Table 9. per Capita ministry of health Expenditures in Ethiopian Birr (Birr = .49 $US) (1988-91)
Expenditure
Hospital
Non-hospital
Total
RURAL
Mean (range)
0.56 (00-4.53)
0.74(.03-2.90)
1.30 (10-7.79)
URBAN
Mean (range)
2.83 (.00-20.27)
0.84(.00-4.14)
3.67(.54-20.27)
ALL
1.13
0.75
1.88
DISCUSSION
By combining the information contained in 52 district health profiles completed over the four year interval
1988 to 1991, it has been possible to establish a representative summary health profile of Ethiopia. District
health services have been rapidly developed over the past five years i in Ethiopia and therefore much of the
data presented in this paper can be viewed as baseline. As mentioned, district health managers have been
preferentially placed in districts where a minimum standard of institutional facilities are in place. In relation
to the country's total population, the population covered by the district health profiles is therefore relatively
more urban, has greater access to health and other government services and resides in communities less
directly affected by the civil war in progress at the time. For these reasons, the figures presented in this paper
likely represent an optimal assessment of the health status of Ethiopians at this time. The distribution of
health indices and health system determinants were assessed by 1) district, 2) urban vs rural populations and
3) hospital vs non-hospital institutions. One of the more important findings of this health profile review is the
wide disparity between district on measures of health and human development and in the distribution of
human and physical resources. As an example, the prevalence of malnutrition in children ranges from 3 % to
65 % among the districts". Under such circumstances the global prevalence of 33% tends to obscure the
actual situation whereby in some districts food security and nutritional status have attained high standards,
while in others they remain extremely low. A good example of disparity in resource distribution is the per
capita spread of health assistants which range from one per 900 to one per 57 ,000 inhabitants.
By stratifying the analyses into rural and urban districts, it has been possible to identify a consistent urban
bias in the distribution of health manpower and expenditures. After adjustment for population size, it is found
that urban districts benefit from three times the number of physicians, nearly four times more nurses and
more than double the proportion of health assistants. Given that nearly 70% of health expenditures are salary
related, it is evident that similar urban-rural disparities in the financing of health services will also be found.
A nearly three-fold increase in per capita expenditures favouring the urban districts was found. By separating
the analyses into hospital and non-hospital sectors one is able to appreciate the impact hospitals have on the
distribution of human and financial resources within a developing country's health care system. Access to
hospitals is largely limited to urban residents, which in Ethiopia reporting approximately 10 to 15% of the
population. In this study. 69% of the nurses and doctors were hospital based. It is to be noted that all
hospitals in Ethiopia provide primary health care services to a varying extent. It is also the case that health
centers distant from a hospital typically offer in-patient services, thus blurring the distinctive roles of these
institutions.
Approximately one-half of the sanitarians identified were hospital employed, yet spend nearly all their time
on preventive, environmental health activities. In general , measures of health status contained in the profiles,
whether it be mortality , morbidity , or human development parameters, were found to be absent or
inadequate in the profiles. This reflects the absence of vital statistics recording and poorly functioning district
health information systems. In nearly all instances morbidity data were passively obtained and based upon
OPD diagnoses or patient complaints.
The health profiles reviewed in this paper represent an important baseline of data upon which future district
health information systems can evolve. Prior to 1988 and the submission of the first of these profiles,
comprehensive assessments of the state of health of Ethiopians at the district level were largely unobtainable.
All of the profiles reviewed in this paper were completed as a requirement for graduation from either of
Ethiopia's two health management training programs: the MPH program - Department bf Community Health,
Addis Ababa University and the Accelerated District Health Managers' training program -Training and
Demonstration Center, Ministry of Health. These training programs have played a leading role in the
development of health profile protocols and their conduct in Ethiopia. What is required at this point is the
continued generation of health profiles, but outside the context of a training program and their integration
into dynamic, up-to-date health information systems.
ACKNOWLEDGEMENTS
The author wishes to acknowledge the work done by each of the district health managers in completing their
district health profiles and upon which this paper is based. Appreciation is extended to the staff of the former
Ministry of Health Training and Demonstration Centre for their kind assistance in obtaining copies of the
district health profiles.
REFERENCES
1. Schaefer M. New needs in health management. World Health Forum, 1989;10:438-447.
2. World Health Organization. Evaluation of the strategy of Health for An by the Year 2000: Seventh Report
on the World Situation. WHO, Geneva, 1986.
3. Gebreselassie 0. Ethiopia: success story .World Health, 1989.
4. District Health Development Study Core Group. Review of district health system development in Ethiopia.
Ministry of Health of Ethiopia, Addis Ababa, 1991.
SOME CHEMICAL CONSTUENTS OF SELECTED
W A TER SOURCES IN AND AROUND
ADDIS ABABA AND AMBO
Yesehak Worku., PhD1, Sinknesh Ejigu, MSc2
ABSTRACT: Water samples were collected from the following Sources: 1. rawand treated water from
Gefersa and Legadadi upstream dams as well as tap water from Addis Ababa, 2. Ambo mineral water,3. two
rivers that flow through Addis Ababa and 4. Lake Aba Samuel. The sample collection was carried out at the
end of the rainy season (September 1993) except for Ambo mineral water which was obtained in mid-June
1994.
Analytic data of seven anions(HCO3-,P- ,Ct, Br, 1,NO3- ,SO42) and nine cations (Na+,K+,Mi+,Ca2+,
Fe2+i3+,Zn2+,pb2+Cd2+,Cr6+) were compiled. Samples from all sources revealed the following: 1.the
concentration of all ions is far below the toxic level, 2. all ions exist at concentrations of less than 8% of
Man's daily requirement except for the sodium concentration (2OOmg/L) of Ambo mineral water .Ambo
water and tap water from Addis Ababa are found to be chemically safe. The same can be said about water
from Aba Samuel and city rivers although more work is necessary to determine the microbial exposure of
animals and irrigations that depend on these sources. [Ethiop. i. Health Dev. 1994;8(2):97-102]
INTRODUCTION
Since water has a very high solvent capacity for polar molecules, it dissolves many compounds from soils
and rocks .The resulting mineral content of drinking water can contribute to the maintenance or deterioration
of health. In this context minerals in drinking water and food provide the following essential functions to
organisms: sustain the electrochemical activity of cells (H+, Na+, K+ etc.), form catalytic parts of enzymes
(Mg2+,Zn2+,etc.) and serve as structural units of molecules (Ca2+ ,HPO4 = ,t) (I). Their subnormal
concentration would lead to various deficiency diseases while high concentration cause numerous toxicity
diseases (2,3).
Drinking water is an important source of minerals. Consequently, data on its chemical composition can
enable health workers to estimate the mineral consumption of individuals or communities from a daily
average water intake of two liters per person per day with an additional intake of 0.75 liter from food (4,5).
Furthermore, such information is important to monitor community water sources for their toxic concentration
of ions (1,3,6).While assessment of minerals to maintain health or cause toxicity require information on
concentration of several ions(1,2,14) shortage of analytic resources restricted this report to focus only on
Na+,K+, Mg2+ Ca2+ Fe2+/3+ Zn2+ Pb2+ Cd2+Cr6+ HC03-,P- , Ct, Br, t, N03- & S042-. Forinstance,
although Hg2+ could be a major pollutant of industrial waste,no analysis was made for it due to lack of
vapour generator . Chemical analysis was conducted on water from the following four different sources: first,
raw and treated water of two upstream dams as well as tap water from Addis Ababa; second, Ambo mineral
water; third, two rivers that pass through Addis Ababa and, finally Aba Samuel, an artificial lake at a lower
altitude to the city . The two rivers carry Addis Ababa's domestic as well as industrial waste to lake Aba
Samuel. The first two sources of water supply are for human consumption while the other two are used for
animals and irrigation systems.
METHODS
Sample sites were Gefersa and Lagadadi dams that supply tap water to Addis Ababa; Ambo mineral water
bottling factory; Akaki and Bulbula rivers that flow through Addis Ababa and lake Aba Samuel(fig. la&b).
Moreover tap waters of Addis Ababa were collected from six weredas selected by lottery , while the precise
location was decided by convenience (fig. la). The dates for sample collection are shown in tables 1 and 2.
________________________
1Department of Biochemistry., Faculty of Medicine, AAU
2Central Geological Laboratory, Ministry of Mines, AA
These water samples were collected in polyethylene bottles thoroughly cleaned and fmally rinsed with
deionized water . The samples were then filtered and stored at 4°C until analysis was carried out.
Temperature was taken during sample collection. Information on the odour, taste and colour of each sample
was obtained from five assessors. The pH was read on calibrated Beckman's 050 pH meter.
Conductivity(con.) was read on microprocessor LF 2000/C conductivity meter of GmbH W .Germany, which
was caliberated using 10,25,50, 75 and l00mM standard KCI solutions. Both Beckman's 050 pH meter and
LF 2000/C possess inbuilt programme that calculate and display readout at 25°C. The total dissolved solids
(TDS) of a sample that was evaporated by a steam bath and dried at 105°C was measured using an analytical
balance.
The cations,( Sodium, Potassium, Magnesium, Calcium, Iron, Cadmium, Chromium, Lead and Zinc) were
determined by atomic absorption spectrometer (Varian's SP-20) using their respective hollow cathode
lampes(7) . Carbondioxide and Bicarbonate were measured by titration using phenolphthalein and methyl
orange indicators, respectively (8). However, estimation of CO2 in carbonated beverage (bottled Ambo
water) which is not based on manometery is probably a lower estimate. Chloride was titrated by 10mM
AgNOJ to K2CrO4 endpoint(9). Halogens(P- ,Br,t) were assayed by their specific ion selective electrodes
(10). Sulphate was determined as BaSO4 particles in a turbid solution (11). Nitrate was estimated using
Beckman's DU-64 spectrophotometer set at two different wave lengths. The absorption at 22Onm is for
nitrate and organic nitrogen whereas the absorption at 275nm is only for the latter. Optical density due to
nitrate was then obtained by subtracting double the reading at 275nm from the reading at 22Onm (12).
RESULTS
All filtered water samples were colourless. However, unfiltered water samples of Gefersa and Legadadi were
brownish yellow. None of the samples, including that of Aba Samuel, had any detectable odour although the
lake gave offensive smell ( which could be attributed to volume difference between the lake and the sample
and/or to organic decay at the bottom of the lake). The taste of Akaki, Bulbula and AbaSamuel waters was
not determined. The rest were tasteless except Ambo water. The concentration of ions in samples from lake
Gefersa, lake Legadadi, Ambo water and tap waters of Addis Ababa are far below toxicity levels. However,
ion concentration in Ambo mineral water is generally higher than tap waters of Addis Ababa, though these
values are within WHO's guidelines. Likewise, the concentration of Ca2+ ,Mg2+ , SO4= and NO3- in City
rivers are significantly higher than what was observed in tap waters of Addis Ababa (tables 1 & 2). Finally,
effort to detect lead, Cadmium and Chromium titer of Akaki, Bulbula and Aba Samuel samples revealed
these ions exist at concentrations that are below detection limit ( <O.O5mg/I).
DISCUSSION
Information on man's daily requirement of various ions is available in many standard text- Books of nutrition
(15,16). Assuming a daily water intake of two litres (4) 1ap water from Addis Ababa provides 1.2% of
Mg2+'s and 8% of Zn's daily requirement. The contribution of tap water to daily requirement of other
essential ions is only 2-8%( table 2). This observation suggests that the concentration of certain essential ions
in tap water of Addis Ababa is far below the daily requirement of man so that the difference ought to be
obtained from food. Ambo mineral water has a high concentration of dissolved solutes (1.32 grn/l). Most of
this is due to Na+,K;+,Mg2' ,Ca2+ and HCO-3.This mineral water contains sufficient Na+ (approx.230mg/lt)
to meet man's daily requirement of 200mg/day (13). It is also within wHO's broad guideline values for Na+
concentration in drinking water (15). On the
Note: The numbers within Addis Ababa are code numbers of Weradas (Councils). The black dots
are sampling sites.
3-Blaklion: From an MU Laboratory, 7-Merkato: Near Yekatit 23 School by Provincial bus terminal, 8Gullele: A Pharmacy infront of National Institute of Health, 17-Megenagna: A tyre repair shop by kebele
17/24's office, 19a-Nifas-Silk: Near Addis Amba School, 19b-Bulbula: About O.3km down stream from St.
Yoseph's Cemetary, 19c-Akaki: at Saris Mill Bridge and 23-Mekanisa: At Institute of Geological Survey.
Table 1. Some Physical and Chemical measurements obtained on selected water sources in and
around Addis Ababa and Ambo. (September 1993*)
Sample source
Lak
Treated
Cityriver
ABC Samuel
Ambo
parameter
e
GF
LE
GF
LE
AK
BU
SP
BO
Date (Sep.93)*
29
17
29
17
18
18
30
17
17
Temperature
(0 C)
16
19
16
19
18
17
20
31
22
PH
7.1
6.7
7.2
6.8
7.2
7.3
7.0
6.7
6.1
Con.
62.6 45.4
65.0
44.3
447
454
195
1500
1496
TDS
71
53
60
48
280
280
140
1320
1312
Na+
1.8
1.7
1.8
1.6
20
30.5
10.3
231
238
K+
2.2
0.9
1.1
0.8
15.3
8.7
2.4
35
35
Mg2+
2.75 1.6
1.98
1.49
9.72
11.8
4.5
44
46
Ca 2+
8.0
3.93
6.9
3.5
45.1
35.9
16.5
74
73
Fe2+/3+
3.8
1.5
0.07
0.06
0.11
0.09
0.5
0.09
0.09
Zn 2+
0.5
0.5
0.5
0.5
0.43
0.42
0.7
0.4
0.45
CO 2
11.4 10.6
8.8
10.6
40.5
31.7
18
805
2653
HCO3
35.1 23.0
25.4
24.0
173
150
100
1116
1092
F0.22 0.12
0.22
0.08
0.39
0.55
0.58
0.76
0.76
CI2.1
2.0
5.2
5.5
23
34
10
32
33
Br0.12 0.11
0.12
0.10
0.40
0.51
0.23
0.33
0.34
I
2.8
2.4
2.7
1.6
3.8
4.2
4.0
1.0
1.0
NO 3
2.6
1.95
1.0
1.4
6.5
38.4
5.1
3.0
3.0
SO4
1.0
0.6
0.5
0.5
14.0
16.0
3.0
0.9
0.9
GF= Gefersa, LE = Legadadi, AK = Akaki, BU = Bulbula, SP= Spring, BO = Bottled. Cond. In - mho/Cm. TDS and concentration in mg/l
except iodide which is in (g/L). The values given are mean of three measurements and their standard error of the mean is
5% of the mean.
*Except Ambo wate which was resampled in june, 1994.
<
Table 2. Physical and Chemical measurements of tap-water from six sites in Addis Ababa
Sample Source
B
G
M
MK
Me
N
Normal or Aesthetic
parameer
Date
17
29
17
17
29
17
Temp (o C)
20
18
20
20
19
20
Unknown
pH
7.1
7.1
7.0
7.0
7.1
7.0
6.5-8.5
Con.
80
79
80
81
80
81
TDS
60
60
60
60
61
61
1000
Na+
2.3
2.2
2.4
2.3
2.3
2.3
200
K+
1.2
1.2
1.1
1.2
1.1
1.1
Unknown
Mg2+
2.0
2.1
2.1
2.0
2.0
2.1
300
Ca 2+
7.0
7.0
6.9
6.9
7.1
7.1
800
Fe2+ /3+
0.1
0.1
0.09
0.09
0.1
0.1
18
Zn 2+
0.60
0.6
0.61
0.61
0.60
0.61
15
CO2
6.0
5.9
6.0
6.1
5.9
5.9
HCO3
23
23
22
22
23
23
F0.15
0.14
0.14
0.15
0.15
0.15
1.5
CI 4.3
4.3
4.2
4.3
4.3
4.4
250
Br 0.13
0.12
0.13
0.11
0.13
0.12
0.1
I2.0
1.9
1.9
2.0
2.0
1.9
150
NO31.6
1.5
1.6
1.5
1.6
1.7
10
SO4=
1.0
1.0
1.0
1.1
1.0
1.1
400
B= Balacklion Hospital, G=Gullele, M=Megenagna, MK=Mekanisa, Me=Merkato, N=Nifas Silk.
See table-1 for units. The values given are means of three measurements.
other hand, essential minerals such as Ca2+, Mg2+ , Fe2+ and texist in tap water in insignificant amount
compared to man's daily requirement (13).
Mineral waters that contain very high concentrations of certain chemicals are said to possess curative value.
For instance, water containing iron at > 10mg/litre improves oxygen transport and oxidative processes (16).
Looking at the constituents of Ambo mineral water from a medical perspective, it is impossible to speculate
any curative value; hence the need for more work to identify the significance of Ambo mineral water other
than for its role as beverage.
The concentration of chemicals in the two rivers passing through Addis Ababa and in lake Aba Samuel( table
1) is below the toxicity cut off level (1). Further more, the concentrations of Lead, Cadmium and Chromium
in Akaki, Bulbula and Aba Samuel samples taken at the end of rainy season is below detection limit ( <
0.05rng/l), which may be compared with the normal daily adult level of 0.05 mg/L of Pb;0.005mg/L of Cd
and 0.05mg/L of Cr or toxic levels of 3mg/L for Cd and 2OOmg/L for Cr(l, 15). Although this work has not
dealt with only organic or inorganic chemicals(particularly Hi+) exhaustively, the data indicates that the level
of chemical pollution of lake Aba Samuel and the city rivers immediately after the rainy season, is not
serious. Nevertheless there is a big difference in the concentrations of some ions such as Mg2+ , Ca2+, S04and No3, between water in lakes at higher altitude and water from City rivers (tables 1,2). It is, therefore,
necessary to initiate preventive measures that minimize chemical pollution by discouraging all concerned
from damping waste in urban rivers. By the same logic, it is even more pressing to prevent urban expansion
towards lakes Gefersa and Legadadi.
ACKNOLWDGEMENTS
This project was partialy supported by a research fund from Addis Ababa University . We are very greatful to
Ethiopian Water and Sewerage Authority as well as Ambo Mineral Water Bottling Factory for permission
that facilitated sample collection. We are also very greatful to W to Mersha Mengestie for typing this
manuscript.
REFRENCES
1. Brown, H.I.M. Trace elements in biochemistry, London, Academic Press, 1966;FF 102-34.
2. Mc Neely, M.D.D. Nutrition, Vitamins and Trace elements. In: Applied biochemistry of clinical disorders,
d. ( Gornall, A.G., Ed.), Philadelphia, Lippincott, 1986;FF487-99.
3. Trevethick, R.A. Environmental and Industrial Hazard, London, William Heinemann,1973;FF 2-206.
4. Gabre-Emanuel Teka. Water supply -Ethiopia: An introduction to enviromental Health practice, Addis
Ababa, Addis Ababa University, 1917:F16.
5. Wilson, E.D., Fisher, K.I. and Garcia, F.A. Principles of Nutrition, 4.. Ed., New-York, John Wiley,
1979:FF 326-7.
6. Tekle-Hairnanot, R., Fekadu, A. and Bushra, B. Tropical and Geographical Medicine 1987; 39: 209-217
7. American Public Health, American water works Assoc., Water pollution and Control Federation. Metals
by Atomic Absorption Spectrophotometry. In standard method: For examination of water and waste water,
14.. Ed., Washington, American public Health Assoc., 1975;FF 144- 162.
8. Titremetric method for carbondioxide. Ibid, FF 298- 301.
9. Cotlove,E. Determination of Chloride in Biological materials. Methods of Biochemical Analysis 1964; 12:
277- 391
10. Oesch, U. Anunann, D. and Simon, W. Ion selective Membrane electrode for clinical use. Clin. Chem.
1986; 32(8): 1448-59.
11. Jackson, S.G. and Mc Candless, E.L. simple, Rapid, Turbidometric Determination of Inorganic sulphate
and or protein. Analy Biochem 1978; 90: 802-8.
12. Miles, D.L. and Espejo, C. Comparison between an Ultraviolet spectrophotometric and the 2,4-xylenol
method for the determination of Nitrate in Ground waters of low salinity. Analyst 1977; 102: 104-9.
13. Anderson, L., Dibble, M.V., Turkki, F.R., Mitchell, H.S. and Rynbergen, H.J .Nutrition in Health and
Disease, FF 69-102. Philadelphia,] .B. Lippincott comp.,1982.
14. Goodhart, R.S. and Shils, M.E. Modem Nutrition in Health and Disease, 6.. Ed. , Philadelphia, Lea and
Febiger , 1986;FF294-441.
15. WHO. Guidelines for drinking water Quality, Recommendations, WHO, Geneva, 1984;1:pp 6-8.
16. Storicescu, C. and Munteanu, L. Natural curative factors of the Main balneoclimateric Resorts in
Romania, Bucharest, Editura sport- Turisin, 1977;Fll.
CARE GIVERS' KNOWLEDGE, BELIEFS, ATTITUDES AND
PRACTICES ON CASE MANAGEMENT OF ACUTE
RESPIRATORY ILLNESSES IN A RURAL DISTRICT
IN ETIHIOPIA
Saba Woldemichael MD, MPH', Dennis G. Carlson MD, MPHl, Derege Kebede MD, MScl
ABSTRACT: A survey was conducted in three randomly selected farmers' associations in Sululta District,
around Chancho town out of which, 540 households were selected randomly. Mothers and other care givers
of children under-five were interviewed regarding their knowledge, beliefs, attitudes and practices in case
management of acute respiratory illnesses. The study showed that 406(75% ) of the care givers have
favorable practice, whereas 483(89.4%),497(92.0%) and 334(61.9%) of the care givers have unfavorable
attitudes, knowledge and beliefs, respectively. Care givers' age is significantly associated with practice,
attitudes and beliefs. Care givers' economic status is also significantly associated with their practice, attitudes
and knowledge whereas care givers' education and presence of grand parents in the neighborhood affected
significantly their attitude, knowledge and belief. [Ethiop. i. Health Dev. 1994;8(2): 103-108]
INTRODUCTION
Diarrhoea, acute respiratory infections (ARI) and protein-energy malnutrition are considered to be the three
leading killing diseases of early childhood (1).
Although there are no accurate figures of incidence and prevalence globally, the existing data show that acute
respiratory infections (ARI) are one of the major causes of deaths among children under five years of age.
Out of the total 15 million deaths among under-five children per year , one third of these deaths are caused by
ARI; and of these, approximately 90% are caused by pneumonia alone. This means that there are about four
million deaths due to ARI in the world each year. The morta1ity rate of ARI in developing countries is more
than 30 times higher when compared to the USA and Canada (2).
The occurrence of ARI in under five children is usually about four to eight episodes per child per year ,
suggesting there are about two billion episodes of ARI infections in developing countries each year .On
average a child in an urban area has from 5-8 episodes of respiratory illnesses annually during the first five
years of life (3-7). In rural areas, the annual incidence per child is reported to be lower, ranging from one to
three episodes per year (8-13).
Because of the high mortality and morbidity due to ARI, WHO has developed standard guidelines for the
control of ARI. The suggested control programs are standardized case management, immunization and health
education. To implement an effective control program in Ethiopia, it is essential to know maternal
knowledge, attitudes and practices regarding the important signs and symptoms and case management of
ARI. Therefore, this study was designed to serve as a baseline in the implementation of ARI-specific health
education intervention study.
METHODS
This study on care givers' knowledge, beliefs, attitudes and practices regarding case management of ARI
was conducted in Sululta District from April 1990 to August 1990.
Of the five farmers' associations found within a five kilometre radius around Chancho Health Centre, three
farmers' associations were randomly selected. The study included 540 randomly selected care givers of
children under five years of age living within the selected farmers' association. To ensure an adequate
________________________
Community Health Department, MU,
P.O.Box 1176, Addis Ababa
response rate and to obtain the informed consent of the study subjects, the study was discussed in general
terms with the farmers' association leaders, the District Health Committee and by the women's associations.
Mothers or other care givers were informed about the study through the farmers' associations and the
women's associations.
Before the interviews were conducted, a questionnaire was prepared to assess knowledge, beliefs, attitudes
and practices regarding the case management of ARI. The questionnaire was back-translated to assess
reliability. Then the questionnaire was pretested in a community similar in social, economic and educational
background to the study areas. The interviews were conducted by ten trained female interviewers.
Analysis was made using SPSS/PC statistical package. Variables were combined to determine the
economic status, practice, attitudes, beliefs and knowledge. Measurements for economic status were created
by calculating a composite score of numbers of cows and oxen and the type of roof. The highest and lowest
scores for economic status were 8 and 1 respectively. A score of < 4.5 was considered as low and a score of >
4.5 was considered as high.
Knowledge, attitudes, beliefs and practice were dichotomized into favorable and unfavorable. The
dichotomization of knowledge scores was made on the ability of the care givers to identify danger signs and
symptoms and cause of pneumonia. Care givers' practice was assessed on their previous health-seeking
practices and on their knowledge of where to seek treatment. Accordingly, care givers attitudes and beliefs
were measured by the ability of the care givers to perceive of the, danger signs of pneumonia and on the
preference or choice of health care providers. Responses referring to un-scientific concepts of disease
causation and spiritual ways of treating ARI, such as considering evil spirits as cause and holy water as
treatment of ARI were attributed to the belief of the individual.
RESULTS
As shown in table 1, 285(52.8%) of the care givers were young (15-34 years), 486(90%) were illiterate,
532(98.5% ) were housewives and 492(91.1%) were married. Three hundred and thirty nine(62.8%) of the
care givers were classified as haying low economic status. Of the 540 care givers, 487(90.2%) were mothers
and 345(63. 9% ) had their grandparents around their house.
Four hundred and six(75.2%) of the care givers reported that they would treat their children with home
treatment initially and take them to a health institution if the illness worsens.
Four hundred and eighty three(89.4%) of the care givers perceive pneumonia as not dangerous and
330(16.1%) prefer to take their children to the local healer .
Four hundred and ninety seven(92.0%) of the care givers do not have adequate knowledge as to what
causes ARI and 312(57.8%) of the mothers do not know the signs and symptoms of pneumonia (table 4).
Three hundred and thirty four(61.9%) of the care givers believe that pneumonia is caused by evil spirits and
312(57.8%) said that it can be cured by holy water (table 5).
When practice is dichotomized in terms of favourable and unfavourable practices and these are compared
by demographic factors, old and middle aged care givers are found to have less favorable practices (RR =
0.18 ; 95% confidence interval (CI)=0;ll, 0.30 and RR= 0.07;95% CI=O.04, 0.11 respectively) as compared
to young care givers. Care givers with high economic status also had better practice in case management as
compared to those with low economic status (RR= 1.99;95% CI= 1.49-2.67) (table 2).
Old and middle-aged care givers were more likely to have negative attitudes as compared to young care
givers (RR=0.36,95% CI=0.23- 0.56 and RR=0.17,95% CI=0.13-0.24 respectively). As compared to illiterate
care givers, mothers who have attended literacy campaigns and completed grades 1-3 have unfavorable
attitudes (RR=0.24,95% CI=0.19- 0.31 and RR=0.73, ' 95% CI=0.20-0.46 respectively). Care givers with
high economic status have less favorable attitudes as compared to those with low economic status
(RR=0.2,95% CI=0.12-0.33). Care givers whose parents are living in the neighborhood also have more
unfavorable attitudes (RR=0.23,95% CI= 0.16- 0.33).
Care givers who have attended literacy campaign and who have completed grades 1-3 have better knowledge
(RR=1.20,95% CI=1.03-1.38 and RR=1.79,95% CI=0.19- 2.67 respectively) as compared to those who are
illiterate. Care givers' knowledge has a statistically significant negative association with economic status
(RR=0.96,95% CI=~.93=0.99) and a positive association with the presence of grandparents in the
neighborhood (RR=1.04,95% CI=1.00-1.07).
No statically significant association was found between care givers' beliefs and care givers , age, education
and economic status. However, there was a statistically significant positive association with age and
education. Presence of grandparents has proved to have an association with unfavorable beliefs (RR=0.80,
95% CI=0.69-0.94).
Table 1. Selected Demographic Characteristics of Care Givers, Sululta District, 1990
Characteristics
Age in years
15-34
35-49
50& above
Total
Education
Illiterate
Lit. Camp.
Grade 1-3
Total
Economic Status
High
Low
Total
Marital Status
Married
Divorced
Others
Total
Relation to the Children
Mother
Others
Total
Grandparents Around
Yes
No
Total
No.(%)
285(52.8)
196(36.3)
59(10.9)
540(100.0)
486(90.0)
36(6.7)
18(3.3)
540(100.0)
201(37.2)
339(62.8)
540(100.0)
492(91.1)
35(6.5)
13(2.4)
540(100.0)
487(90.2)
53(9.8)
540(100.0)
345(63.9)
195(36.1)
540(100.0)
DISCUSSION
More than 50% of the care givers were young (15-34), which is typical of developing countries where
women have children in their early ages. About 90% of the care givers were illiterate, thus affecting their
general outlook of disease causality and case management. About two- thirds of the care givers had low
economic status, which in turn affects their access to health care.
Table 2. Care Givers’ practice by Selected Demographic Characteristics, Sululta District, 1990
Practice Age in years
15-034
35-49
50-&above
Care Giver’s Education
Illiterate
Lit.Camp.
Grade 1-3
Care Giver’s Occupation
Housewife
Others
Economic Status
High
Low
Grandparents
Yes
No
Total
Unfavourable
17
65
51
Favourable
268(94.0)
131(66.8)
8(13.6)
Total
285
196
59
RR (95% CI)
1.00*
0.18(0.11,0.30)
0.07(0.04,0.11)
125
7
1
361(74.3)
29(80.5)
17(94.4)
486
36
18
1.00*
1.32(0.67,2.62)
4.63(1.69,31.29)
131
2
401(75.4)
6(75.0)
532
8
1.00*
0.98(0.29,3.30)
72
61
129(64.2)
278(82.0)
201
339
1.00*
1.99(1.49,2.67)
88
45
133
257(74.5)
150(76.9)
407(75.4)
345
195
540
1.00*
1.11(0.81,1.51)
*Reference Group
Table 3. Care Givers’ Attitudes by Selected Demographic Characteristics, Sululta Dirstrics, 1990.
Attitude age in years
15-34
35-49
50&above
Care Giver’s Education
Illiterate
Lit.Camp.
Grade 1-3
Care Giver’s Occupation
Housewife
Others
Economic Status
High
Low
Grandparents
Yes
No
Total
* Reference group
Positive
49
57
43
Negative
236(82.8)
139(70.9)
16(27.1)
Total
285
196
59
RR ((95% CI)
1.00*
0.36(0.23,0.56)
0.17(0.13,0.24)
110
28
11
376(77.4)
8(22.2)
7(38.9)
486
36
18
1.00*
0.24(0.19,0.31)
0.31(0.20,0.46)
146
3
386(72.8)
5(62.5)
532
8
1.00*
0.73(0.30,1.81)
16
133
185(84.3)
206(60.8)
201
339
1.00*
0.20(0.04,0.33)
32
117
149(27.6)
313(63.7)
178(36.3)
391(72.4)
345
195
540
1.00*
0.23(0.16,0.33)
Table 4. Cavers’ knowledge by Selected Demographic Characteristics, Sululta District, 1990
Knowledge Age in years
Unfavourable Adequate
Total
RR (95% CI)
15-34
278
7(2.5)
285
1.00*
35-49
190
6(3.1)
196
1.01(0.98,1.04)
50 & above
56
3(5.1)
59
1.03(0.97,1.09)
Care Giver's Education
Illiterate
484
2(0.4)
486
1.00*
Lit. Camp
30
6(16.7)
36
1.20(1.03,1.38)
Grade 1-3
10
8(44.4)
8
1.79(1.19,2.71)
Care Giver's Occupation
Housewife
519
13(2.4)
532
1.00*
Others
5
3(37.5)
8
1.56(0.91,2.67)
Economic status
High
190
11(5.5)
201
1.00*
Low
334
5(1.5)
339
0.96(0.93,0.99)
Grandparents
Yes
339
6(1.7)
345
1.00*
No
185
10(5.1)
195
1.04(1.00,1.07)
Total
524(97.0)
16(3.0)
540
*Reference group
Table 4. Cavers’ knowledge by Selected Demographic Characteristics, Sululta District, 1990
Belief Age inYears
Unfavourable Adequate
Total
RR (95% CI)
15-34
133
152(53.3)
285
1.00*
35-49
106
90(45.9)
196
0.86(0.73,1.03)
50 & above
47
12(20.3)
59
0.59(0.49,0.70)
Care Giver's Education
Illiterate
268
218(85.8)
486
1.00*
Lit. Camp
12
24(9.5)
36
1.65(1.04,2.64)
Grade 1-3
6
12(4.7)
18
1.65(0.86,3.20)
Care Giver's Occupation
Housewife
282
250(47.0)
532
1.00*
Others
4
4(50.0)
8
1.06(0.53,2.13)
Economic status
High
96
105(52.2)
201
1.00*
Low
190
149(44.0)
339
0.85(0.72,1.01)
Grandparents
Yes
168
177(51.3)
345
1.00*
No
118
77(39.5)
195
0.80(0.69,0.94)
Total
286(53.0)
254(47.0)
540
* Reference group
In general, the prevalence of unfavourable practices was quite low. This may be due to the geographical
proximity' of Sululta to the capital city which might have enabled the members of these study communities to
make frequent visits and gather new ideas and better ways of practice. It is also possible that the majority of
the study population gave the correct answer telling the interviewers what they thought was desired. To find
out the true practices, other methods of data collection should be used.
The prevalence of negative attitudes was lower than expected during the baseline survey. This may be due
to some of the same reasons as for the low prevalence of unfavourable practice. One of the factors which can
lead to change in people's behaviour is thought to be the level at which they consider a disease risky .
This study shows that care givers think that pneumonia and some of the danger signs of ARI are not life
threatening. Therefore health workers should educate mothers on the signs and symptoms of ARI. There was
a high prevalence of unfavourable knowledge regarding causes and case management of ARI. This was
probably due to the low literacy rate.
The prevalence of negative beliefs was also relatively high. This may be due to traditional concepts of
disease causation which have been held for generations. To address this, the study differentiated beliefs from
knowledge, classifying spiritual concepts of causation of ARI as beliefs.
Care givers' knowledge, attitudes, beliefs and practices are strongly associated with age, education and
economic status. Stronger health education interventions or more effort should be put in on educating the
care givers with relatively high risk groups.
We can conclude from this study that care givers' practice were relatively good and care givers' attitudes,
knowledge and beliefs were unfavorable. The study also showed that care givers' knowledge, attitudes,
beliefs and practices were affected by age, education and economic status.
ACKNOWLEDGEMENTS
The study was financially supported by IDRC. It was done as a thesis work for the MPH 4egree (Dr. Saba
Woldemichael) in the Department of Community Health. We gratefully acknowledge all those who have
helped us in the conduct of the study, including the mothers and other care-takers of the study children.
REFERENCES
1. S. Berrnan. K. Mesndlosh. Acute Respiratory Infections Review of Infections Disease. 1985;7:674-91.
2. WHO. Area of Research on Acute Respiratory Infections WHO/RSD/87. 1987 ;35 :P3 .
3. WHO. Memorandum for a WHO bull. 1984;62(1):47-59. 4. James. J.W. Clinical Nutrition. Am. Med. I.
1972; 25:690.
5. Freij. L., Wall. S. Exploring child healdl and its ecology. Acta Pediatr. Scand. Suppl. 1977;267
6. Kanatgm I .R. et al. American Journal of Epidemiology 1979;89:375.
7. Fox. J.p. et al American Journal of Epidemiology 1975; 101:122.
8. Black. R.E. American Medical Journal of Epidemiology 1982;115:305.
9. Li-MCI. Gao. Primary Report of Acute Respiratory Infections Surveillance in Dong Guan Brigade.
Document 1982; WHO/WPR/82.13.
10. Dodge. R.E., Demeke T. Edl. Med. Jour. 1979;8:53. 11. Gordon. J.E. et al. Arch Environmental
Healdl1968; 16:426.
12. Karyadi. A./A. Acute Viral Respiratory Infections: Their Public Healdl Importance in Indonesia,
Document WHONIR/SGn9, Agenda Item 7.5. Geneva 2-6.
13. Smidl. D. et al. Patterns of ARI morbidity. Mortality and Healdl Service Utili7.ation in dIe Asaro Valley.
Papua New Guinea 1982;1989 ~Q81.
14. Woldemichael S. Heal III Plan and Action Plan of Sululta Awraja. 1990.
THE IN VITRO ANTIBACTERIAL ACTIVITY OF "TAZMA MAR"
HONEY PRODUCED BY THE STINGLESS BEE
(Apis mellipodae)
Mogessie Ashenafi, B.Sc., M.Sc., Ph.D.1
ABSTRACT: In 1993 the antibacterial effect of "tazma mar" was evaluated on Salmonella typhimurium,
Salmonella enteritidis, Escherichia coli, Bacillus cereus and Staphylococcus aureus at concentrations of 10%,
15% and 20% in Brain Heart Infusion
Broth. In the absence of "tazma mar", the Gram negative test strains
reached counts > 108 cfu/m1 within 12 hours and maintained the count until 48 hours. At 10%
concentration, typhimurium, S. enteritidis and E. coli were not inhibited until 12 hours, but thereafter their
number declined faster and complete inhibition was observed at 48 hours. Retarded growth and inhibition
was noted at 15% and 20% concentrations. A more marked growth retardation and inhibition at all
concentrations was noted on B.
cereus and Staph. aureus. "Tazma mar" may be effective to treat foodborne infections at low concentrations. [Ethiop. J. Health Dev. 1994;8(2):109-117]
INTRODUCTION
Although honey has been used for dressing wound since ancient times (1), its antibacterial property was
recognized only very recently (2). The antibacterial activity was originally believed to be only due to high
osmolarity , with its water content rarely exceeding 20% (3). Another antibacterial factor in honey was
reported to be its relatively low pH value which is normally around 4 (4). A third factor was believed to be
"inhibine" (5), an antibacterial substance, later found to be hydrogen peroxide generated by the action of
glucose oxidase in honey (6). White and Subers (7) later observed that some honey samples had antibacterial
activity in excess of that which could be accounted for by the action of hydrogen peroxide alone. This
antibacterial activity persisted after the removal of hydrogen peroxide by the addition of catalase (8).
Recently, the use of honey as a topical antibacterial agent has been accepted to treat surface infections such
as ulcers and bed sores (9, 10), and those resulting from burns, injuries and surgical wounds (11-13).
Many investigators have reported the antibacterial activity of honey against Staphylococcus aureus,
Pseudomonas aeruginosa, Citrobacter freundii, Escherichia coli, Proteus mirabilis, Streptococcus faecalis,
and Listeria monocytogenes ( 14-15) .
Most of these studies were made on honey produced by the honey bee. In Ethiopia, honey produced by the
stingless bee (commonly known as "tazma mar") is considered to be important in traditional treatment of
respiratory ailments, surface infections and various other diseases. Considering the fact that there is a
significant association of the potency of honey with the floral type (16), it would be Worthwhile to examine
the potency of honey produced by a different species, the stingless bee. The purpose of this work was to
evaluate the antibacterial activity of "tazma mar" against some food-borne pathogens, thereby determining
the possible role of "tazma mar" in the treatment of food infections.
_____________________
Awassa College of Agriculture,
Department of Basic Sciences,
Addis Ababa University. P.O.Box 5, Awassa, Ethiopia.
METHODS
Preparation of "tazrna mar" "Tazma mar" was purchased from a local market and diluted in Brain Heart
Infusion (BHI) Broth (MERCK) in 100 mi amounts in sterile screw capped bottles to give a final
concentration of 10%, 15% and 20%. BHlbroth with no "tazma mar" served as a control.
Cultures
The following bacterial cultures were used in this study. Salmonella typhimurium (A 13), Salmonella
enteritidis (A 2), Escherichia coli (WS 1323), Staphylococcus aureus (WS 1759) and Bacillus cereus (WS
1537). The cultures were obtained from the culture collection of Bakteriologisches Institute, SVFA,
Weihenstephan, former Federal Republic of Germany.
Inoculation with test organisms
The test organisms were separately inoculated in the three dilutions of "tazrna mar" and in the control bottle
to get a final inoculum level of around 103 cfu/ml. The mixture was shaken thoroughly and incubated at
32°C for 48 hours. The initial inoculum level was determined by surface plating with appropriate dilutions
from the freshly inoculated control bottles on Brain Heart Infusion Agar (MERCK) in duplicates.
Analysis of samples
Cultures were sampled at 6-hour intervals for 48 hours. Appropriate dilutions of all cultures were separately
surface plated on BHI agar and incubated for one hour at 32°C to allow metabolic recovery of injured cells.
An overlay of the following agar media was then separately added on to the inoculated plates: XLD for S.
typhimurium and S. enteritidis, VRB for E. coli, Mannitol Salt agar for Staph. aureus, and Bacillus cereus
agar for B. cereus. Colony counting was done after incubation at 32°C for 24-48 hours.
The pH of the "tazma mar" solutions was measured using a digital pH meter .
RESULTS
S. typhimurium, S. enteritidis and E. coli showed a similar pattern of growth in the control broth and of
inhibition at the various concentrations of "tazma mar" (Figures 1-3). They reached a level higher than lOS
cfu/rn1 within 12 hours in the control broth and maintained nearly the same level upto 48 hours. At 10%
"tazma mar" concentration, growth was not affected until 24 hours, where all reached a count of > 108
cfu/rn1. After 24 hours, however, there was a sharp decline in count resulting in complete inhibition at 36
hours in the case of S. enteritidis and E. coli and 48 hours in the case of S. typhimurium. At 15%
concentration, the lag phase for the test organisms was longer, the growth rate was low and the maximum
count reached was less than 1& cfu/rn1.
"Tazma mar" concentrations of 20% had a bacteriostatic effect until 24 hours, followed by a sharp decline
and then complete inhibition at 36 hours. The Gram positive test organisms (B. cereus and Staph. aureus)
showed a different growth pattern from that of the Gram negative ones at the various "tazma mar"
concentrations. Growth in the control broth was luxurious, although the count of B. cereus did not reach 108
cfu/rn1 at all times (Figure 4).
At 10% "tazma mar" concentration, the count of B. cereus did not decrease markedly until 5 hours, but a
slight decline was observed until 12 hours. Decline in count was sharper after 24 hours but no complete
inhibition was observed even at 48 hours (about 10 cfu/rn1). A similar pattern was also observed at 15%
"tazma mar" concentration.
A concentration of 20% was effective to reduce the count gradually from 0 hour until complete inhibition at
48 hours. Although Staph. aureus grew to counts > 108 cfu/rn1 in the control broth, its count was maintained
under 1Q4 cfu/rn1 at all times at all concentrations of "tazma mar" .A sharp decline in counts started at 30
hours followed by a complete inhibition at 36 hours (Figure 5).
The pH values for "tazma mar" concentrations of 10%, 15% and 20% were 4.0, 3.94 and 3.91 respectively.
DISCUSSION
There is no information available in the scientific literature on "tazrna mar" to make comparisons. But similar
studies on honey produced by the honey bee have shown that honey could inhibit S. aureus, Pseudomonas
aeruginosa, Citrobacter freundii. E. coli, Proteus mirabilis, and Streptococcus faecalis (15). Other workers
have reported that honey has an antibacterial effect on Salmonella spp . and E. coli, but the inhibitory effect
was much more pronounced at 75-80% of honey concentration (14). The complete inhibition of organisms
causing surgical infection or wound contamination was also effected by honey concentration of 100% and
partial inhibition at 50% (17). In contrast to these reports, "taima mar" , in this study, could inhibit most of
the test organisms at very low concentrations (10-20%). The antibacterial property of "tazma mar" could be
due to various factors. Its low pH (around 4) could be inhibitory to B. cereus, which does not normally
multiply in acidic conditions. The other organisms are reported to tolerate a lower pH (18,19). In addition,
since there was no marked difference in pH values of the various "tazma mar" concentrations, the high
growth rate of the Salmonella spp. and E. coli at 10% concentration indicated that pH alone is not an
important inhibitory property; it is worth noting that highly osmotolerant strains like S. aureus were markedly
retarded at a concentration as low as 10% .The inhibitory property of hydrogen peroxide in honey may not
be so significant since all the test organisms were catalase producers which can break down hydrogen
peroxide. "Tazma mar" may, in addition, have other antibacterial substances which are effective at lower
concentrations. Bogdanov (20) characterized a flavonoid compound as the antibacterial substance in honey
produced by the honey bee and very recently Russel et. al. (21) identified trimethoxybenzoic acid, methyl
syringate and syringic acid as the antibacterial constituent of honey. Further studies are, therefore, required to
identify the important antibacterial constituents of "tazma mar".
The effectiveness of "tazma mar" in retarding or inhibiting growth of the test strains in this study may
indicate that it may be used to treat food-borne infections at relatively lower concentrations. Its use in
traditional medicine may thus be properly evaluated and it may also serve the food preserving industry .
ACKNOWLEDGEMENTS
The technical assistance of Haile Alemayehu and Tsigereda Bekele is acknowledged. This paper was
presented at the DAAD- NAPRECA follow-up Conference, held at the Addis Ababa University , Addis
Ababa, Ethiopia, Nov. 5-9, 1993.
REFERENCES
1. Majno, G. The Healing Hand -Man and Wound in the Ancient World. Harvard University Press,
Cambridge, Massachusetts, USA 1975.
2. Sackett, WG. Honey as a carrier of intestinal diseases. Bull. Colorado Statt: Univ. Agric. Exp. SIn. 1919;
252:18.
3. White, IW. Honey. II. The Hive and Honey Bee. Hamilton. 1975.
4. Sancho, MT ., S Muniategui, IF Huidobro and I Simal. Honeys of the Basque district of Spain. I. pH and
acidity . Anal. Bromotolog. 1991; 43:77-86. .
5. Dold, H., DH Du and ST Dziao. Nachweis antibakterieller, hitze und lightempfindlicher Hemmungsstoffe
(Inhibine) im NaturhonigBluetenhonig. S. Hyg. Infekionskr. 1937;120:155-167.
6. White, IW., MH Subers and A Shepartz. The identification of inhibine. Am. Bee I. 1962;102:430-431.
7. White IW. and MH Subers. Studies on honey inhibine. 2. A chemical assay. I. Apic. Res. 1963;2:93-100.
8. Adcock, D. The effect of catalase on the inhibine and peroxide values of various honeys. I. Apic. Res.
1962;1:38-40.
9. Bloomfield, R. Old remedies. I. R. ColI. Gen. Pract. 1976; 26:576.
10. Keast-butler, I. Honey for necrotic malignant breast ulcers. Lancet 1980; ii:809.
11. Efem, SEE. Clinical observation of the wound healing properties of honey. Br. I. Surg. 1988; 75:679-681.
12. Green, AB. Wound healing properties of honey. Br. I. Surg.1988;75:1278.
13. Mclnemey, RJF. Honey -a remedy rediscovered. I. R. Soc. Med. 1990; 83:127.
14. Radwan, SS., AA EI-Essawy and MM Sarhan. Experimental evidence tor the occurrence in honey of
specific substances active against microorganisms. Zbl. Mikrobiol. 1984;139:249-255.
15. Hodgson, MI. Investigation of the antibacterial action spectrum of some honeys. M.Sc. Thesis University
of Waikato,-Hamilton, New Zealand. 1989.
16. Allen, KL., PC Molan and M Reid. A survey of the antibacterial activity of some New Zealand honeys.
Parm. Pharmacol. 1991; 43:817-822.
7. Efem, SEE, KT Udoh and CI Iware. The antimicrobial pectrum of honey and its clinical significance.
infection.1992;20:224-229.
18. Mogessie Ashenafi and M Busse. Inhibitory effect of LaCtobaciUus plantarum on Salmonella infantis,
Enterobacter aerogenes and Escherichia coli during tempeh fermentation. I. Food Protect. 1989; 52:167-172.
19. Mogessie Ashenafi. Growth potential and inhibition of Bacillus cereus and Staphylococcus aureus during
the souring of ergo, a traditional Ethiopian fermented milk. Ethiop. I. Health Dev. 1992; 6:23-29.
20. Bogdanov, S. Characterization of antibacterial substances in honey. Lebensm. Wiss. U. Technol. 1994;
17:74-76.
21. Russel, KM., PC Molan, AL Wilkins and PT Holland. Identification of some antibacterial constituents of
New Zealand manuka honey. I. Agric. Food Chem. 1990; 38:10-13.
BRIEF COMMUNICATION
RETROSPECTIVE STUDY OF CERVICAL CARCINOMA:1988-1992
Feleke Bojia, B&., MD, Dip. Pad1l, Amare Dejene, BSc., MSc. l, Yared Mekonnen, BSc. l
INTRODUCTION
Carcinoma of the cervix is one of the most frequently seen malignant neoplasms in the female genital tract
(1).
The disease is unknown in virgins, of very low incidence in Jews, intermediate in frequency in Muslims and
high among Caucasians and African races. The average age is 48 years, the range being 20-80 years (1).
The Pathology Section of NRIH receives biopsy specimens from five hospitals in Addis Ababa and from one
or more hospitals of seven administrative regions, namely from three hospitals, in Wollega, one hospital in
Arsi, two hospitals in Tigray and one hospital in Eritrea.
There is no previously documented study to show the pattern of this disease in our country . We, therefore,
believe that the assessment of age distribution and frequency of occurrence is of great importance in setting
up the general background of the pattern of occurrence of the disease in order to be able to suggest possible
preventive measuring.
METHODS
A.systematic sampling technique was used to select the samples which are included in the study.
Accordingly, every 5d1 record was selected out of a total of 10,000 documented cases so that 2126 cases
were included in the study. Of these, 178(8.4%) (Table 1) were specimens from the cervix, out of which
54(30%) (Table 2) were found to have carcinoma of the cervix.
New sections of all 54 cases of carcinoma of the cervix were prepared. The slides were stained by
hematoxylin and eosin method and cases of adenocarcinoma of the cervix were stained by special technique
of alcian blue for differentiation from endometrial carcinoma (2). All sides were reviewed independently by
two pathologists. The histologic types were identified and compared according to their mode of occurrence
(3).
Data were entered in a microcomputer using Dbase III + and analysis were conducted using SPSS PC+ and
EPI-INFO.
RESULT
Carcinoma of the cervix was found to affect both reproductive age groups and the elderly in about the same
proportion in our study (Table 3).
The age range is 25- 70 years with a mean age of occurrence of 44.5 years. The disease shows an increasing
pattern with age, ranging from 11.4% for those women of age 20-29 to 41.7% for those women of age 40-49.
In comparison with the 178 specimens of the cervix, carcinoma of the cervix is by far the most frequently
occurring lesion of the cervix (30.4%) in our study (Table 1).
According to our result, the most frequently occurring histologic type is a well differentiated keratinizing
type and moderately differentiated non-keratinizing type of squamous cell carcinoma of the cervix, 73.2%
(Table 2).
_______________________
National Research Institute of Health (NRIH)
P.O.Box 1242, Addis Ababa. Ethiopia
DISCUSSION
Carcinoma of the cervix may occur at any age from the second decade of life to seility (4). The peak
incidence of invasive lesion occurs around 45 years of age and invasive lesions at 30 years (4). However, the
peak incidence of carcinoma of the cervix in our study is 49 years and above, suggesting a positive trend of
occurrence.
Table 1: Comparative Analysis of Cervical Lesions From the Cervix
Cervical Lesions
Cervical carcinoma
Cervical cervicitis
Cervical polyp
Cervical biopsy
Cervical dysplasia
Cervical nabothian cyst
Others
Total
Frequency
54
42
24
22
3
3
30
178
Percent
30.4
23.6
13.5
12.4
1.7
1.7
16.7
100
Table 2: Histologic Types of Carcinoma of the Cervix (1988-1992)
Histologic Types
CIN(Cervical intra epithelial neoplasia)
Keratinizing & non-keratinizing squ. carcinoma
Adenocarcinoma
Adeno Sq. Carcinoma
Total
Table 3: Age Distribution of Cervical Carcinoma
Age
Cervical Carcinoma
(%)
< 19
0
(0.0)
20-29
4
(11.4)
30-39
15
(26.3)
40-49
20
(41.7*)
50+
15
(46.9)
Total
54
(30.5)
p < 0.01 (X2 = 15.5)
No. (percent)
7(12.9)
41(75.9)
1( 1.9)
5( 9.3)
54(100)
Total (%)
5
(2.8)
35
(19.8)
57
(32.2)
48
(27.1)
32
(18.1)
177
(100.0)
But, the fact that a considerable percentage occurs between 30-39 years still poses the gravity of the disease
in our country .The fact that the frequency of occurrence of well differentaited keratinizing type and
moderately differentiated squamous cell carcinoma is significantly high as compared to other histologic types
indicates a better prognosis for Ethiopian Patients. Since the principal factor which will improve the
prognosis of cancer of the cervix at present, apart from improvements in techniques for treatment and
organizing gynecological oncology centers, is mass cervical cytologic screening (6).
We, therefore, believe mass cervical cytologic screening, early diagnosis and due treatment of cervical
carcinoma will significantly reduce the incidence of the disease in our society.
ACKNOWLEDGEMENTS
We are grateful to The National Research Institute of Health for the due financial and moral support. We
extend our thanks to Dr. Yohanis Legesse for reviewing the slides and Ato Tesfamariam Mahari, Ato Asfaw
Beyene and Wlro Debretsgie Admasu for assisting us in slide preparation and data collection. We also thank
Wit Zebib Tilahun and Wit Wagaye Teshome for typing the manuscript.
REFERENCE
1. A.D. Thomson, R.E. Cotton. Lecblre Notes on Padlology 3. Edition; 1983; 420-421.
2. Yugo Japaze, lUng Vanpinii and Donald Woodnlff. Venucous Carcinoma of the Vulva obstetrics and
Gynecology, 1982; 60, 4 462-468.
3. Disia AS. Surgical Aspect of Cervical Carcinoma Cancer, 1981; 48:548.
4. Robbins, Cotran and Cumar 4" Edition. Padlologic Bases of Diseases, 1984; 1124.
5. Henery Clay Prick, Nikolas, A. Janovski, Saul B. Gusberg, Howard C. Tacor JR. The Cure Rate of
Carcinoma of dIe Cervix is 97.0%, Rang 95-97% American Journal of Obsterics & Gyneclogy, 1963; 85,
No.7.926-935.
6. Clinics in Obtetrics and Gynecology, 1976; 3, No.2:365-357.
7. Rotman, M., et al. Prognostic Factors in Cervical Carcinoma. Implication in Staging and Management.
Cancer, 1981; 48:560.
UPDATE
AIDS CASE SURVEILLANCE IN ETHIOPIA: JUNE 30, 1994
Epidemiology & AIDS Control Department
Ministry of Health
INTRODUCTION
This report is published by the Epidemiology and AIDS Control Department of MOH on a monthly basis.
And distributed free of charge for over 400 government and non-government institutions. The major
objectives of the Publication are to:
* Notify the current status of AIDS epidemc in the country , and provide. information for decision making
and future planning .
** Provide feedback to health institutions and colaborating agencies in the country. From January 1986 to
June 30, 1994, a total of 13, 644 AIDS cases have been reported by hospitals in the country .Surveillance and
research activities carried out in Ethiopia among different population groups have also indicated the extent of
the HIV / AIDS epidemic and its progression.
___________________________
Note (1) you are kindly requested to share information with your staff. (2) Comments and suggestions are
appreciated for improving our reporting system
Table 1: summary of AIDS Cases Reported in Ethiopia, as of 30
June 1994.
Variable
Cumulative value
Number of AIDS cases reported
13644
Number of reporting hospitals
51
Average age of patients
30.5
Sexually active age group (15-49 yrs)
93.3%
Proportion of paediatric cases (age <15 yrs)
1.6%
Heterosexual transmission
87.1%
Proportion of married people
35.3%
Female to male ratio of total cases
1:1.6
Reported cases by A. A hospitals
53.5%
Patients residing in Addis Ababa
42.4%
Major clinical symptoms
Weight Loss of >10% body weight
88.1%
Prolonged Fever for > month
84.4%
Persistent Cough for >1 month
67.8%
Chronic Diarrhea for >1 month
60.7%
Criteria used to diagnose AIDS patients in Ethiopia.
The World Health Organization (WHO) provisional case definition with positive serology test for HIV
antibodies is the criteria used to diagnose AIDS. According to the case definition, a patient has to manifest at
least two major and one minor signs and show an HIV positive serology.
(See page 9 of the report for the list of major and minor clinical symptornslsigns).
Summary of the report for the month of June 1994
In June 1994 alone, a total of 686 AIDS cases were reported by 16 hospitals; 366 cases were from 6 Addis
Ababa hospitals and the remaining 320 cases were from 10 regional hospitals. The following table identifies
the number of cases reported during this month, by reporting hospital and region/zone.
Table 2: distribution of Reported AIDS Cases by Hospital, for the month of June 1994.
Hospital
Period of diagnosis
Cases
Central Prison
Mar. 94 - May 94
10
Kolfie TBC
May 94 - June 94
22
Menelik II
Apr. 94 - June 94
143
St. Paulos
Apr. 94 - May 94
50
Ras Desta
Mar. 94 - May 94
107
Yekatit 12
Apr. 94 - May 94
34
Sub Total
366
Attat
May 94
14
Bushulo
Mar. 94 - June 94
13
Dire Dawa
Mar. 94
88
Gimbi
Apr. 94 - June 94
24
Gondar College
April 94 - June 94
78
Heroes Center
May 94
1
Hossan
Mar. 94 - June 94
14
Metehara
Nov. 93 - Apr. 94
21
Nazareth
Feb. 94 - May 94
63
Wonji
May 94 - June 94
4
Sub Total
320
Total
686
Table 3: AIDS Cases by Quarter of Report.
Year-quarter
Males
Females
Total
Percent
86-1
1
0
1
0.01%
86-2
0
1
1
0.01%
87-1
4
0
4
0.03%
87-2
0
2
2
0.01%
87-3
2
2
4
0.03%
87-4
6
1
7
0.05%
88-1
4
3
7
0.05%
88-2
21
5
26
0.19%
88-3
19
4
23
0.17%
88-4
23
6
29
0.21%
89-1
11
4
15
0.11%
89-2
44
17
61
0.45%
89-3
21
16
37
0.27%
89-4
52
25
77
0.56%
90-1
49
27
76
0.56%
90-2
67
14
81
0.59%
90-3
92
49
141
1.03%
90-4
84
66
150
1.10%
91-1
218
82
300
2.20%
91-2
101
77
178
1.30%
91-3
161
80
241
1.77%
91-4
105
61
166
1.22%
92-1
145
108
253
1.85%
92-2
327
218
545
3.99%
92-3
603
397
1000
7.33%
92-4
909
549
1458
10.69%
93-1
618
403
1021
7.48%
93-2
528
94
822
6.02%
93-3
1030
620
1650
12.09%
93-4
1011
620
1631
11.95%
94-1
1158
762
1920
14.07%
94-2
1023
694
1717
12.58%
Total
8437
5207
13644
100.00%
Tab;e 4: Distribution of AIDS Cases by Year of Report.
Sex
Sex
Ratio
(M:F)
Year
Male
Female
Percent
of Tolal
Total
86
1
1
2
1:1
0.01%
87
12
5
17
2.4:1
0.12%
88
67
18
85
3.7:1
0.62%
89
128
62
190
2.1:1
1.39%
90
292
156
448
1.9:1
3.2%
91
585
300
885
1.9:1
6.49%
92
1984
1272
3256
1.6:1
23.86%
93
3187
1937
5124
1.6:1
37.55%
94
2181
1456
3637
1.5:1
26.66%
Total
8437
5207
13644
1.6:1
100.00%
The proportion of female patients being reported has increased since 1992.
Table 5: Age and Sex distribution of Reported AIDS Cases
Age group
Sex
Males
Females
0-4
100
96
5-14
13
14
15-19
174
589
20-29
3136
2774
30-39
3085
1194
40-49
1390
388
50-59
432
131
60+
107
21
Total
8437
5207
(percent)
(61.84%)
(38.16)
Total
196
27
763
5910
4279
1778
563
128
13644
Percent
1.44%
0.20%
5.59%
43.32%
31.36%
13.03%
4.13%
0.94%
100.00%
Average age for females = 27.1 years, and for
males = 32.6 years, and for both sex = 30.5 years.
Table 6: Distribution of Reported AIDS Cases by Marital Status.
Marital status
Male
Female
Single
3973
2017
Married
3306
1516
Divorced
439
1012
Widowed
69
341
Paediatric Cases (Age < 15 years)
107
104
Unspecified
543
217
Total
8437
5207
Total
5990
4822
1451
410
211
760
13644
Percent
43.90%
35.34%
10.63%
3.00%
1.55%
5.66%
100.00%
Table 7. Reported AIDS Cases by Occupation.
Occupation type
Males
ARMED FORCES
1569
BAR WORKER*
85
DAILY LABOURER
413
DRIVER
958
FARMER
222
GOVT EMPLOYEE
1506
Females
35
106
130
5
10
386
Both
1604
191
543
963
232
1892
Percent
11.76%
1.40%
3.98%
7.06%
1.70%
13.87%
HOUSE WIFE
MECHANIC
MRCHANT
OTHERS
PRISONER
SERVANT/HOUSE MAID
0
253
888
668
51
14
996
4
207
413
0
336
996
257
1095
1081
51
350
7.30%
1.88%
8.03%
7.92%
0.37%
2.57%
SEX WORKER
STUDENTS
TELLA/TEJ SELLER
UNEMPLOYED (ADULT)
UNEMPLOYED (CHILDREN)
UNSPECIFIED
Total
0
234
11
296
107
1162
8437
847
343
187
376
103
723
5207
847
577
198
672
210
1885
13644
6.21%
4.23%
1.45%
4.93%
1.54%
13.82%
100.00%
* Bar worker include bar owners and those who are not at high risk as sex workers.
Table 8. Average Number of AIDS Cases Per Month and Number of Reporting Hospitals by Year.
Year
Average no. of cases per Reporting hospitals
month
Addis Ababa
Region
Total
Before 1988
0 to 1
7
0
7
1988
7
13
2
15
1989
16
15
4
19
1990
37
17
14
31
1991
74
17
22
39
1992
269
17
29
46
1993
427
18
30
48
1994
18
30
48
Total
18
30
48
Table 9: Distribution of AIDS Cases by Reporting Hospitals and by Years of Report for Addis Ababa Hospital.
Reporting Hospitals
Year or Report
86
87
88
89
90
91
92
93
ALERT
0
1
32
37
61
0
339
224
AMANUEL
0
0
0
0
0
1
6
5
ARMED FORCE
0
4
3
22
59
64
36
30
BALCHA*
0
0
3
0
0
0
0
0
Total
Percent
94
63
0
13
0
757
12
231
3
10.37%
0.16%
3.16%
0.04%
CENTRAL COMMAND
CENTRAL PRISON
ETHIO-SWEDISH
GANDHI
KOLFIE TBC
0
0
0
0
0
0
0
0
0
0
2
0
5
0
0
0
0
0
1
0
0
0
0
1
0
0
0
3
0
0
11
0
3
0
0
33
19
0
0
49
28
33
7
14
73
74
52
18
15
127
1.01%
0.71%
0.25%
0.21%
1.74%
MINILIK II
ST. PAULOS
ST. PETROS
POLICE
RAS DESTA
0
0
0
0
0
0
0
1
2
1
0
4
1
1
0
13
0
4
10
30
7
1
84
5
44
0
23
39
36
106
210
18
76
29
196
378
294
235
52
362
292
223
67
38
318
900
563
507
173
1057
12.33%
7.71%
6.94%
2.37%
14.48%
TATEK
TIKUR ANBESSA
YEKATIT 12
ZEWDITU
Total
0
0
2
0
2
0
3
5
0
17
0
25
3
3
82
0
47
13
3
180
6
43
22
21
358
22
148
16
50
508
0
148
251
118
1441
2
634
199
273
2789
3
520
133
100
1925
33
1568
644
568
7302
0.45%
21.47%
8.82%
7.78%
100.00%
Table 10: Distribution of AIDS Cases by Reporting Hospitals and by Years of Report for Regional Hospital.
Reporting Hospitals
Year or Report
86
87
88
89
90
91
92
93
AIR FORCES
0
0
0
0
0
0
0
18
ALAMATA
0
0
0
0
0
0
0
0
AMBO
0
0
0
0
0
3
14
42
ARBAMINCH
0
0
0
0
7
24
41
86
ASEBE TEFERI
0
0
0
0
0
12
6
30
Total
Percent
94
0
13
16
42
19
18
13
75
200
67
0.28%
0.20%
1.18%
3.15%
1.06%
ASELLA
ASSAB
ASSELA
ATTAT
BORENA
0
0
0
0
0
0
0
0
0
0
0
2
0
0
0
0
0
0
0
0
0
0
1
0
1
0
0
26
14
0
0
0
6
59
0
0
0
0
176
0
23
0
0
79
0
32
2
33
328
1
0.36%
0.03%
0.52%
5.17%
0.02%
BUSHULO
DEBRE BREHAN
DEBRE MARKOS
DEBRE TABOR
DESSIE
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
11
19
20
8
46
70
86
93
12
32
0
94
107
24
0
65
311
220
44
78
146
510
3.47%
0.69%
1.23%
2.30%
8.04%
DIREDAWA
FELEGE HIWOT
GIMBI
GOBA
GONDAR COLLEGE
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
8
0
0
0
13
1
7
0
32
31
18
0
5
82
72
575
0
0
214
335
162
74
45
144
116
0
119
0
307
567
764
200
50
779
8.94%
12.05%
3.15%
0.79%
12.28%
HEROES CENTER
HIWOT FANA
0
0
0
0
0
0
0
0
1
14
3
59
0
93
1
150
1
22
6
338
0.09%
5.33%
Table 10.....cont'd
Reporting Hospitals
Total
Percent
92
34
0
0
93
0
121
0
94
14
0
9
48
135
9
0.76%
2.13%
0.14%
0
1
14
0
0
1
5
180
0
59
0
0
132
81
60
21
8
151
0
0
22
14
478
81
119
0.35%
0.22%
7.54%
1.28%
1.88%
1
0
0
3
10
0
9
0
13
11
0
17
31
42
136
0
10
112
70
255
6
0
81
42
116
6
36
224
170
538
0.09%
0.57%
3.53%
2.68%
8.48%
90
377
1815
2335
1712
6342
100.00%
Table 11. Distribution of AIDS cases by Region/country of Residence and by Year of Report
Region/country of residence
Year or Report
86
87
88
89
90
91
92
AA
2
12
59
113
271
355
1204
ARSSI
0
0
2
5
1
30
30
ASSOSA
0
0
0
0
0
0
1
BALE
0
0
0
2
2
10
18
BORENA
0
0
0
0
3
1
9
DIREDAWA
0
0
1
2
24
39
89
Total
Percent
93
2214
27
0
75
24
383
94
1551
35
6
22
19
110
5781
130
7
129
56
648
42.37%
0.95%
0.05%
0.95%
0.41%
4.75%
E. GOJJAM
E. HARARGE
E.SHOA
GAMBELLA
ILLUBABOR
0
0
0
0
0
1
1
1
0
0
0
0
2
0
1
2
4
10
1
2
3
10
16
4
0
10
48
49
0
17
68
84
251
3
10
91
132
309
8
144
42
49
286
5
9
217
328
924
21
183
1.59%
2.40%
6.77%
0.15%
1.34%
KAFFA
METEKEL
N GONDAR
N OMO
N SHOA
N WOLLO
OGADEN
0
0
0
0
0
0
0
0
0
0
0
1
0
0
0
0
1
0
1
1
0
1
2
1
0
2
0
0
0
2
28
5
2
2
2
2
3
74
16
6
15
1
9
72
207
38
26
41
3
8
64
149
86
58
162
7
16
1
126
39
64
99
3
36
144
586
184
160
320
16
0.26%
1.06%
4.29%
1.35%
1.17%
2.35%
0.12%
S GOJJAM
S GONDAR
S OMO
S SHOA
S WOLLO
0
0
0
0
0
0
0
0
0
1
0
0
0
0
0
0
1
0
0
8
0
4
0
7
9
0
17
4
16
31
0
91
0
89
97
0
13
3
85
98
1
221
4
62
316
1
347
11
259
560
0.01%
2.54%
0.08%
1.90%
4.10%
HOSSANA*
JIMMA
MAICHEW
86
0
0
0
87
0
0
0
88
0
1
0
89
0
1
0
90
0
0
0
METEHARA
MIZAN
NAZARETH
NEKEMET
PAWIE
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
1
1
0
0
0
0
0
1
QUIHA
SHASHEMENE
WOLDIA
WONJI
YIRGALEM
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
Total
0
0
3
10
Year or Report
91
0
12
0
Table 11.Cont'd
Region/country of residence
SIDAMO
TIGRAY
W GOJJAM
W HARARGE
W SHOA
WOLLEGA
86
0
0
0
0
0
0
87
0
0
0
0
0
0
88
1
1
1
0
4
0
89
0
4
11
0
6
2
90
9
2
6
3
2
5
DIJIBOUTI
ERITREA
INDIA
S AFRICA
SOMALIA
UGANDA
UNKNOWN
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
10
0
0
0
0
0
0
9
0
0
0
0
2
0
25
0
0
0
0
1
Total
2
17
85
190
448
Table 12. AIDS Cases by Risk Factors
Risk Factors:
History of Multi-Partner Sexual
Contact (MPSC)
History of Blood Transfusion
Maternal HIV of Breast Feeding
History of Illegal Injection
IV drug abuse
Unspecified
Total
Percent
92
127
8
556
19
63
9
93
281
22
166
49
228
184
94
187
42
8
31
126
117
621
87
772
120
451
325
4.55%
0.64%
5.66%
0.88%
3.31%
2.38%
1
37
0
0
0
0
7
1
24
0
1
3
2
3
3
26
1
0
1
0
23
4
24
0
0
0
0
0
9
155
1
1
4
2
48
0.07%
1.14%
0.01%
0.01%
0.03%
0.01%
0.35%
885
3256
5124
2395
12402
100.00%
Male
7430
Female
4455
Total
11885
Percent
87.11%
69
97
64
4
773
48
93
59
2
550
117
190
123
6
1323
0.86%
1.39%
0.90%
0.04%
9.70%
Table 13. Clinical Signs and Symptoms of Reported AIDS Cases.
Clinical Manifestations
Males
Females
MAJOR SYMPTOMS
Weight loss > 10% of body weight
7399
4321
(Failure to thrive)
Prolonged Fever for > 1 month
7069
4451
Chronic Diarrhoea for > 1 month
5117
3165
MINOR SYMPTOMS
Generalized Lymphadenopathy
Persistent Cough for > 1 month
Skin rashes
Tuberculosis (Plumonary and/or
Disseminated)
Recurrent herpez zoster
Generalized pruritic dermatitis
Year or Report
91
16
8
24
18
22
8
Total
Percent
12020
88.10%
11520
8282
84.43%
60.70%
2168
5790
118
1371
1140
3464
63
797
3308
9254
181
2168
24.25%
67.82%
1.33%
15.89%
1234
1403
671
935
1905
2338
13.96%
17.14%
Oropharyngeal candidiasis
Pneumonia (including PCP)
1692
404
1031
227
2723
631
19.96%
4.62%
Chronic herps simplex
CNS derangement
91
130
70
50
161
180
1.18%
1.32%
Night sweats & Generalized Body
Weakness
113
62
175
1.28%
Loss of appetite
Kaposi's Sarcoma
19
31
6
8
25
39
0.18%
0.29%
Table 14. Reporting Status of AIDS Cases for Addis Ababa Hospitals, January -June 1994.
Hospital
J F
M A M J
J
A
S O
N D
1.ALERT
X X X
2. AMANUEL
3. ARMED FORCES
X
X
4. BALCHA
5. CENTRAL COMMAND
6. CENTRAL PRISON
7. ETHIO-SWEDISH
8. GANDHI
9. KOLFEI TBC
X
X
X
X
X
X
X X
10. MINILIK II
11. ST. PAULOS
12. ST. PETROS
X
X X
X
X
X
1
2
5
13. POLICE
14. RAS DESTA
15. TATEK
X
X
X
X
X
X
X
11. DEBREMARKOS
12. DEBRE TABOR
13. DESSIE
14. DIREDAWA
15. FELEGE HIWOT
16. GIMBI
17. GOBA
18. GONDAR
COLLEGE
19. HEROES CENTER
20. HIWOT FANA
X
X X
X
X X
X
X
X X
X X
X
X X
X
X
X
2
3
1
N
D
Total
1
1
2
1
1
6
6
1
X
1
4
2
X X
X
1
3
1
X
16. TIKUR ANBESSA
X
X
17. YEKATIT 12
X
X
X
18. ZEWDITU
X
Table 15. Status of AIDS Cases Report for Regional Hospitals, January -June 1994
Hospital
J
F M A M J
J
A
S
O
1. AIRFORCE
2. ALAMATA
X
3. AMBO
X
4. ARBAMINCH
X
X
5. ASEBE TEFERI
X
6. ASSELA
7. ATTAT
8. BORENA
9. BUSHULO
10. DEBRE BERHAN
2
4
3
X
X
2
1
4
X
X X
Total
3
X X
X
X
5
X
X
X
3
X
1
1
X
Table 15.... Cont'd
Hospital
21. HOSSANA
22. JIMMA
23. MAICHEW
24. METEHARA
25. MIZAN
26. NAZRETH
27. NEKEMET
28. PAWIE
29. QUIHA
30. SHASHEMENE
31. WOLDIA
32. WONJI
33. YIRGALEM
J
F
M
A
M
J
X
X
X X
X X
X
X
X
X
A
S
O
N
D
Total
1
X
1
1
1
X
2
X
X
J
X
1
X
X
1
6
4
X
EXCERPTS FROM THE TRANSITIONAL GOVERNMENT'S
PROCLAMATION NO 41/1993 AND HEALTH POLICY
In this issue we have included two important sources of information of the Transitional Government of
Ethiopia (TGE) on health as an additional service for our readers. One of these is proclamation No 41/1993,
which defines "The powers and duties of the central and Regional Executive Organs of the Transitional
Government of Ethiopia " from which, we have extracted only those parts of the proclamation that relate to
health. We advise all health workers to read the full text of the proclamation in the Negarit Gazeta. The other
source of information we have included here is the Health Policy of the TGE the full text of which is
presented. The Eth. I. of Health Dev. welcomes discussions or comments on either one or both of these
important documents hoping that this contributes to better understanding and implementation.
1. Proclamation No 41/1993
This proclamation is effective as of Ian. 20, 1994.
Short title
This proclamation my be cited as the "Definition of powers and Duties of the Central and Regional Executive
Organs of the Transitional Government of Ethiopia, Proclamation No. 41/1993." Definitions In this
Proclamation:
1. "Regional Self-Government" means a National/Regional Self-Government established pursuant to
proclamation No. 7/1992;
2. "Regional Executive Committee" means a National Regional Executive Committee established in
accordance with Article 15/1/b/ of Proclamation 7/1992
Common Powers and Duties of Ministries Each Ministry shall:
I. in its field of activity:
a. initiate policies, prepare plans and budget and, upon approval, implement same;
b. ensure the enforcement of laws, regulations and directives of the Central Government:
c. undertake studies and research; collect and compile statistical data;
d. give assistance and advice to Regional self-Governments, and follow up the proper implementation of
Laws, regulations and directives by their executive organs;
e. enter into contracts and international agreements in accordance with the law;
2. perform the duties specified in this Proclamation and such others as are assigned to it by other laws;
3. submit periodic activity reports to the Council of Ministers.
The Ministry of Health
The Ministry of Health shall have the powers and duties to:
1. formulate the Country's public health policies and strategy and, upon approval, follow up and supervise
their implementation;
2. prepare and submit draft laws to be issued on public health and supervise their enforcement;
3. establish and 'administer referral hospitals and research centers; provide technical and professional
assistance to hospitals, health centers, clinics and research and training centres;
4. determine and supervise standards to be maintained by health services as well as research and training
establishments operated in the country by anyone; issue licences to non- governmental hospitals, health
services established by foreign organizations and investors in accordance with the policy and law to be issued
by the Government and to research and training establishments;
5. determine the qualifications of professionals required for engaging in public health services at various
levels; register and issue certificates of competence to medical practitioners and pharmacists;
6. ensure that traditional medicines are investigated promoted, encouraged and utilized side by side with
modern medicines and, for this purpose. organize centres for research and experiment;
7. devise and follow up the implementation of ways and means of preventing and eradicating communicable
diseases;
8. undertake the necessary quarantine controls to protect public health;
9. undertake studies with a view to determining the nutritional value of foods;
10. prepare and enforce essential drugs' list; control the quality standards of drugs and medical supplies;
11. promote international cooperation relating to health services. Bureaus -Each regional self-government
may establish a health bureaus.
Powers and Duties Common To All Bureaus Each bureau shall:
1. in its area of activity:
a) Prepare and, upon approval, implement plans' and budget; .
b) ensure the implementation of laws, regulations and directives;
c) undertake studies and research; collect and compile statistical data; and transmit same to the concerned
central executive organ;
d) enter into contracts in accordance with the law;
2. Perform the duties assigned to it under this Proclamation and other laws
3. Submit to the regional executive organ and to the concerned central executive organ periodic activity
reports.
Health Bureau
The Health Bureau shall have the powers and duties to: prepare on the basis of the health policy of
the country, the health care plan and program for the people of the region and to implement same when
approved:
2. ensure the observance in the region of laws, regulations and directives issued pertaining to
public health;
3. organise and administer hospitals, health centers, clinics, and research and training institutions to be
established by the regional self-government:
4. issue licence to health centers. clinics, laboratories and pharmacies to be established by domestic
organizations and investors: supervise to ensure that they maintain standard fixed of the national level:
5. ensure that professionals engaged is public health services in the region satisfy the prescribed standard;
and supervise same;
6. cause the application, together with modern medicine, traditional medicines and treatment methods
whose efficiency is ascertained;
7. cause the provision of vaccinations and take other measures, to prevent and eradicate communicable
diseases;
8. participate in quarantine controls undertaken for the protection of public health;
9. ascertain the nutritional value of foods. Accountability and Responsibility of
Bureau Head
Accountability
Each bureau head shall be regards the execution activities programs and laws pertaining to the bureau to
which he is assigned shall be accountable to the Executive Committee of the region.
Responsibility
Each Bureau Head Shall:
1. implement the powers and duties entrusted to the Bureau to which this is assigned:
2. submit to the executive committee of the region draft laws necessary for the proper carrying out of the
activities of the bureau;
3. effect expenditure on the basis of the approved budget of the bureau. Other Central Govenunent
Organs Without prejudice to the provisions of Article 11 of this Proclamation central government organs
specified in Article 41 sub-article 4, 8, 9, 11, 12, 13, 14 and 15 of Article Proclamation No. 8/1987 shall
continue their functions in accordance with their respective establishment laws.Executive Organs to be
Established in Woreda and Other Administrative Levels The powers and duties of the executive organs to
be established in Worda and other administrative levels in each regional self-government shall be
determined, consistently with this Proclamation, by the regional self-government. Repeal
The following are hereby repealed:
1. Proclamation No. 8(1987;
2. The National Water Resources Commission Establishment Proclamation No. 217/1981;
3. The Building and Transport Construction Design Authority Establishment Proclamation
No.327/1987.
2. Health policy of the Transitional Govenunent of Ethiopia
PREAMBLE
Ethiopia, an ancient country with a rich diversity of peoples and cultures has however remains backward in
socio-economic and political development, and in technological advances. Conventional health parameters
such as infant and maternal mortality, morbidity and mortality from communicable diseases, malnutrition and
average 1ife expectancy place Ethiopia among the least privileged nations in the world. In recent times, the
country has experienced severe manmade and natural calamities and political upheavals which have caused
untold suffering to its peoples. At no time in the past has the country enjoyed the leadership of a
representative government with a defined mandate and accountability. In the field of health there was no
enunciated policy up to the fifties. Subsequently, references to the development of health with provision of
basic health services through a network of health centres and health stations and the need to give due
attention to prevention alongside curative services could be discerned. Towards those of the Imperial period a
comprehensive Health Services Policy was adopted through initiatives from the World Health Organization.
However, the downfall of the regime precluded the possibility of putting this scheme to the test. The Dergue
regime that came into power in the midseventies formulated a more elaborate health policy that gave
emphasis to disease prevention and control, priority to rural areas in health service and promotion of selfreliance and community involvement. But in practice the totalitarian political system lacked the commitment
and leadership quality to address and maintain active popular participation. in translating the formulated
policy into action. In addition, the bulk of the national resources were committed to the pursuit of war
throughout the life of the regime which left little for development activities in any sector .
Therefore, in health as in most other sectors, in both of the previous regimes there was no meeting ground
between declaration of intent and demonstrable performance. Furthermore, the health administration
apparatus contributed its own share to the perpetuation of backwardness in health development because, like
the rest of the tightly centralized bureaucracy, it was unresponsive, self-serving and impervious to change.
The Health policy of the Transitional Government is. the result of a critical examination of the. nature,
magnitude and root causes of the prevailing health problems of the country and awareness of newly emerging
health problems. It is founded on commitment to democracy and the rights and powers of the people that
derive from it and to decentralization as the most appropriate system of government for the full exercise of
these rights and powers in our pluralistic society .It accords appropriate emphasis to the needs of the less
privileged rural population which constitute the overwhelming majority of the population and the major
productive force of the nation. As enunciated in these articles, it proposes realistic goals and the means for
attaining them based on the fundamental principles that health, constituting physical, mental and social wellbeing, is a prerequisite for the enjoyment of life and for optimal productivity. The Government therefore
accords health a prominent place in its order of priorities and is committed to the attainment of these goals
utilizing all accessible internal and external resources. In particular the Government fully appreciates the
decisive role of popular participation and the development of self -reliance in these endeavours and is
therefore determined to create the requisite social and political conditions conducive to their realization.
The Government believes that health policy cannot be considered in isolation from policies addressing
population dynamics, food availability , acceptable living conditions and other requisites essential for health
improvement and shall therefore develop effective intersectorality for a comprehensive betterment of life.
In general, health development shall be seen not only in humanitarian terms but as an essential component of
the package of social and economic development as well as being an instrument of social justice and equity.
Pursuant to the above the health policy of the Transitional Goverment shall incorporate the following basic
components.
GENERAL POLICY
1. Democratization and decentralization of the health service system.
2. Development of the preventive and promotive components of health care.
3. Development of an equitable and acceptable standard of health service system that will reach all segments
of the population within the limits of resources.
4. Promoting and strengthening of intersectoral activities .
5. Promotion of attitudes and practices conductive to the strengthening of national self-reliance In health
development by mobilizing and maximally utilizing internal and external resources.
6. Assurance of accessibility of health care for all segments of the population.
7. Working closely with neighbouring countries, regional and. international organizations to share
information and strengthen collaboration in all activities contributory to health development including the
control of factors detrimental to health.
8. Development of appropriate capacity building based on assessed needs.
9. Provision of health care for the population on a scheme of payment according to ability with special
assistance mechanisms for those who cannot afford to pay.
10. Promotion of the participation of the private sector and nongovernmental organizations in health care.
PRIORITIES OF THE POLICY
I. Information, Education and Communication (I.E.C.) of health shall be given appropriate prominence to
enhance health awareness and to propagate the important concepts and practices of self-responsibility in
health
2. Emphasis shall be given to:2.1 the control of communicable diseases, epidemics and diseases related to malnutrition and poor living
conditions,
2.2 the promotion of occupational health and safety,
2.3 the development of environmental health,
2.4 the rehabilitation of the health infrastructure and
2.5 the development of an appropriate health service management system.
3. Appropriate support shall be given to the curative and rehabilitative components of health including
mental health.
4. Due attention shall be given to the development of the beneficial aspects of Traditional Medicine including
related research and its gradual integration into Modem Medicine.
5. Applied health research addressing the major health problems shall be emphasized.
6. Provision of essential medicines, medical supplies and equipment shall be strengthened.
7. Development of human resources with emphasis on expansion of the number of frontline and middle level
health professionals with community based, task-oriented training shall be undertaken.
8. Special attention shall be given to the health needs of:8.1 the family particularly women and children,
8.2 those in the forefront of productivity,
8.3 those hitherto most neglected regions and segments of the population including the majority of the rural
population, pastoralists, the urban poor and national minorities, 8.4 victims of man-made and natural
disasters.
GENERAL STRATEGIES
1. Democratization within the system shall be implemented by establishing health councils with strong
community representation at all levels and health committees at grass-root levels and to participate in
identifying major health problems, budgeting, planning, implementation, monitoring and evaluating health
activities.
2. Decentralization shall be realized through transfer of the major parts of decision-making, health care
organization, capacity building, planning, implementation and monitoring to the regions with clear definition
of roles.
3. lntersectoral collaboration shall be emphasized particularly in:
3.1 Emiching the concept and intensifying the practice of family planning for optimal family health and
planned population dynamics.
3.2 Formulating and implementing an appropriate food and nutrition policy.
3.3 Accelerating the provision of safe and adequate water for urban and rural populations,
3.4 Developing safe disposal of human, household, agricultural, and industrial wastes, and encouragement of
recycling.
3.5 Developing measures to improve the quality of housing and work premises for health.
3.6 Participating in the development of community based facilities for the care of the physically and mentally
disabled, the abandoned, street children and the aged.
3.7 Participating in the development of day-care centres in factories and enterprises, school health and
nutrition programmes,
3.8 Undertakings in disaster management, agriculture, education, communication, transportation, expansion
of employment opportunities and development of other social services.
3.9 Developing facilities for workers' health and safety in production sectors.
4. Health Education Shall be strengthened generally and for specific target populations through the mass
media, community leaders, religious and cultural leaders, professional associations, schools and other social
organizations for:
4.1 Inculcating attitudes of responsibility for self-care in health and assurance of safe environment .
4.2 Encouraging the awareness and development of health promotive life-styles and attention to personal
hygiene and healthy environment.
4.3 Enhancing awareness of common communicable and nutritional diseases and the means for their
prevention.
4.4 Inculcating attitudes of participation in community health development.
4.5 Identifying and discouraging harmful traditional practices while encouraging their beneficial aspects.
4.6 Discouraging the acquisition of harmful habits such as cigarette smoking, alcohol consumption, drug
abuse and irresponsible sexual behaviour.
4.7 Creating awareness in the population about the rational use of drugs.
5. Promotive and Preventive activities shall address:
5. I Control of common endemic and epidemic communicable and nutritional diseases using appropriate
general and specific measures.
5.2 Prevention of diseases related to affluence and ageing from emerging as major health problems.
5.3 Prevention of environmental pollution with hazardous chemical wastes.
6. Human Resource Development shall focus on:
6.1 Developing of the team approach to health care.
6.2 Training of community based task-oriented frontline and middle level health workers of appropriate
professional standards; and recruitment and training of these categories at regional and local levels.
6.3 Training of trainers, managerial and supportive categories with appropriate orientation to the health
service objectives.
6.4 Developing of appropriate continuing education for all categories of workers in the health sector .
6.5 Developing an attractive career structure, remuneration and incentives for all categories of workers
within their respective systems of employment.
7. Availability of Drugs, Supplies and Equipment shall be assured by:
7.1 Preparing lists of essential and standard drugs and equipment for all levels of the health service system
and continuously updating such lists.
7.2 Encouraging national production capability of drugs, vaccines, supplies and equipment by giving
appropriate incentives to firms which are engaged in manufacture, research and development.
7.3 Developing a standardized and efficient system for procurement, distribution, storage and utilization of
the products.
7.4 Developing quality control capability to assure efficacy and safety of products.
7.5 Developing maintenance and repair facilities for equipment.
8. Traditional Medicine shall be accorded appropriate attention by:
8.1 Identifying and encouraging utilization of its beneficial aspects.
8.2 Co-ordinating and encouraging research including its linkage with modem medicine.
8.3 Developing appropriate regulation and registration for its practice.
9. Health Systems Research shall be given due emphasis by:
9.1 Identifying priority areas for research in health.
9.2 Expanding applied research on major health problems and health service systems.
9.3 Strengthening the research capabilities of national institutions and scientists in collaboration with the
responsible agencies.
9.4 Developing appropriate measures to assure strict observance of ethical principles in research.
10. Family Health Services shall be promoted by:
10.1 Assuring adequate maternal health care and referral facilities for high risk pregnancies.
10.2 Intensifying family planning for the optimal health of the mother, child and family.
10.3 Inculcating principles of appropriate maternal nutrition.
10.4 Maintaining breast-feeding, and advocating home made preparation, production and availability of
weaning foods at affordable prices .
10.5 Expanding and strengthening immunization services, optimisation of access and utilization.
10.6 Encouraging early utilization of available health care facilities for the management of common
childhood diseases particularly diarrhoeal diseases and acute respiratory infections.
10.7 Addressing the special health problems and related needs of adolescents.
10.8 Encouraging paternal involvement in family health.
10.9 Identifying and discouraging handful traditional practices while encouraging their beneficial aspects.
11. Referral System shall be developed by:
11.1 Optimizing utilization of health care facilities at all levels.
11.2 Improving accessibility of care according to need.
11.3 Assuring continuity and improved quality of care at all levels.
11.4 Rationalizing costs for health care seekers and providers for optimal utilization of health care facilities
at all levels.
11.5 Strengthening the communication within the health care system.
12. Diagnostic and Supportive Services for Health care shall be developed by:
12.1 Strengthening the scientific and technical bases of health care.
12.2 Facilitating prompt diagnosis and treatment.
12.3 Providing guidance in continuing care.
13. Health Management information system shall be organized by:
13.1 Making the system appropriate and relevant for decision making, planning, implementing, monitoring
and evaluation.
13.2 Maximizing the utilization of information at all levels.
13.3 Developing central and regional information documentation centres.
14. Health Legislations shall be revised by:
14.1 Up-dating existing public health laws and regulations.
14.2 Developing new rules and regulations to help in the implementation of the current policy and addressing
new health issues.
14.3 Strengthening mechanisms for implementation of the health laws and regulations.
15. Health Service Organization shall be systematized and rationalized by:
15.1 Standardizing the human resource, physical facilities and operational systems of the health units at all
levels.
15.2 Defining and instituting the catchment areas of health units and referral systems based on assessment of
pertinent factors.
15.3 Regulating private health care and professional deployment by appropriate licensing.
16. Administration and Management of the health system shall be strengthened and made more effective and
efficient by:
16.1 Restructuring and organizing at all levels in line with the present policy of decentralization and
democratization of decision making and management.
16.2 Combining departments and services which are closely related and rationalizing the utilization of human
and material resources.
16.3 Studying the possibility of designating under-secretaries to ensure continuity of service.
16.4 Creating management boards for national hospitals, institutions and organizations.
16.5 Allowing health institutions to utilize their income to improve their services.
16.6 Ensuring placement of appropriately qualified and motivated personnel at all levels.
17. Financing the Health Services shall be through public, private and international sources and the
following options shall be considered and
evaluated.
17.1 Raising taxes and revenues .
17.2 Formal contributions or insurance by public employees.
17.3 Legislative requirements of a contributory health fund for employees of the private sector .
17.4 Individual or group health insurance.
17.5 Voluntary contributions .
Publication of this issue was financially supported by:The Ethiopian Public Health Association (From a Canadian Public Health Association Grant)
Ethiopian Science and Technology Commission (From a Swedish Agency
for Research Cooperation with developing Countries Grant)
McGill-Ethiopia Community Health Project (From Canadian
International Development Agency Grant)
and Addis Ababa University.
The Ethiopian Journal of Health Development
Volume 8 Number 2 August 1994
DEDICATED TO THE SOCIAL GOAL OF
HEALTH FOR ALL
THROUGH THE PRIMARY HEALTH CARE APPROACH
CONTENT
ORIGINAL ARTICLES
HEALTH IN ETHIOPIA: A SUMMARY OF 52 DISTRICT HEALTH PROFILES
Charles P. Larson, Tadele Desie …………………………………………………87
SOME CHEMICAL CONSTITUENTS OF SELECTED WATER SOURCES
IN AND AROUND ADDIS ABABA AND AMBO
YesehakWorku, SinkneshEjigu………………………………………………… 97
CARE GIVERS' KNOWLEDGE, BELIEFS, ATTITUDES AND PRACTICES
ON CASE MANAGEMENT OF ACUTE RESPIRATORY ILLNESSES
IN A RURAL DISTRICT IN ETHIOPIA
Saba Woldemichael, DennisG. Carlson, DeregeKebede ………………………103
THE IN VITRO ANTIBACTERIAL ACTIVITY OF "T AZMA MAR "
HONEY PRODUCED BY THE STINGLESS BEE
Mogessie Ashenafi ……………………………………………………….……109
BRIEF COMMUNICATION
RETROSPECTIVE STUDY OF CERVICAL CARCINOMA: 1988-1992
Feleke Bojia, Amare Dejene, Yared Mekonnen …………………….………119
UPDATE
AIDS CASE SURVEILLANCE IN ETHIOPIA: APRIL 30, 1994
National AIDS Control Program, Ministry of Health
EXCERPTS FROM TRANSITIONAL GOVERNMENT'S PROCLAMATION
NO41/1993ANDHEALTHPOLICY .………………………………………139
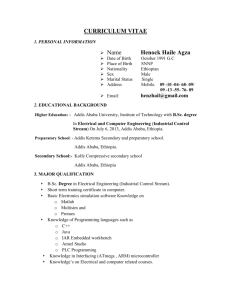

![[SENDER`S ADDRESS]](http://s3.studylib.net/store/data/007552927_2-f74ba3398a02c0a6fcf578f457395e63-300x300.png)