AAA
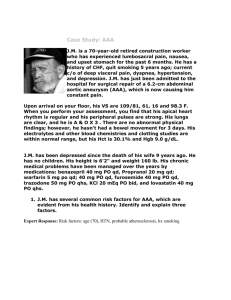
advertisement

Abdominal Aortic Aneurysm These are the commonest form of arterial aneurysm, and occur in 2-10% of patients over the age of 50, with a 5:1 male:female ratio It’s defined as a prolonged abnormal dilatation of the artery to greater than 1.5 times its normal diameter (in an adult, normal diameter is 2cm). 95% are due to atherosclerotic disease. They can be fusiform (diffusely dilated) or saccular (like a berry aneurysm) most commonly. 95% are infrarenal and 30% will also involve the iliacs. This is thought to be due a decreased elastin content in the arterial wall as you move away from the heart. The aorta is retroperitoneal, located just to the left of midline (left of the IVC). Important branches include: - Paired visceral – supra-renal, renal and gonadal - Unpaired visceral – coeliac, SMA, IMA - Paired somatic – inferior diaphragmatic, numerous lumbar spinal - Unpaired somatic – median sacral Risk Factors - Smoking - HTN - Hyperlipidaemia - COPD - Age - Gender - Collagen disorders - Family history Presentation Can be found incidentally on abdominal US, on CT or calcifications may be seen on x-ray While 75% are asymptomatic, symptomatic AAA will present with: - Deep, boring abdominal pain, radiating to the back, or may be solely back pain - May be aware of an abdominal pulsation The other presentation is either due to rupture, or from a complication – e.g. embolic disease of the lower limb (ischaemic leg, trash foot) With a rupture they will have: - Sudden collapse - Nausea & vomiting - Abdominal pain - Pulsing sensation in the abdomen - May have signs of shock - Abdominal rigidity - Abdominal mass - Tachycardia - Bruising in the flanks - Check peripheral perfusion as an indicator of status and check distal pulses If a patient makes it to hospital with a rupture there is still a 50% mortality rate Very rarely, patients may present with symptoms of local compression Differential diagnosis of a rupture - MI Perforated DU Pancreatitis Renal colic Mesenteric ischaemia Indications for surgery - Aneurysm >/= 5.5cms in men (>/= 5cm in women), with or without symptoms Aneurysm < 5.5cms which is symptomatic Any rupture 4cm aneurysm has a 10% 5yr rupture risk 8cm aneurysm has an 80% 5yr rupture risk Investigations - FBC – look for low Hb U&E – check renal status Amylase Group and cross-match - 6 units Coags Urinalysis ABG (if there’s time) ECG +/- cardiac enzymes Erect CXR CT – only if stable (they might die inside if they’re not) If you’re comfortable with the diagnosis, call ahead to theatre Acute treatment - - IV access and fluids – keep systolic below 100mmHg – if the patient has formed a temporary clot around a rupture, raising their BP could make them blow it off. Hypotension will keep them alive! Urinary catheter Oxygen May need central line Arterial line if you have time Try to get consent In the emergency situation an open AAA repair is indicated. In elective cases, an EVAR may be more appropriate Open AAA repair This is done by a midline laparotomy using a PTFE (polytetrafluoroethylene) graft or a Dacron graft, which is stitched into the artery. The graft may be bifurcated to treat iliac disease as well. Important medications during surgery are antibiotics at induction and heparin when the aorta is clamped. Early complications: - Bleeding - Infection – wound, intra-abdominal, graft and LRTI - Ileus – most will have an ileus for up to 48 hours due to handling of the bowel - 15% will have a cardiac event of some sort - Mesenteric ischaemia - Lower limb ischaemia - Renal impairment - Paraplegia – due to damage to some spinal arteries – this is more common in emergencies - Stroke Late complications: - Graft rupture or leak - Erectile dysfunction – due to sympathetic nerve damage - Rarely there can be a fistula between the graft and the bowel causing massive haematemesis There is no follow up required with open repairs. EVAR This is pretty much the same idea as above except – uses a graft to bypass the aneurysm. The differences are that: - The access is through the femorals – if the iliacs are very diseased, EVAR may not be possible due to the size of the deployment devices. Also, can’t do if very tortuous iliacs. - Both femorals have to be cannulated - The graft isn’t stitched in, it’s just deployed - It can be done under spinal - Isn’t rarely used in emergencies Advantages of open repair - Less follow up Available to more patients Longer follow up research data Advantages of EVAR - Doesn’t need a GA Don’t clamp the aorta Less invasive – no post-op ileus Less post-op pain Less ICU time Can be used in riskier patients – i.e. those who may be unsuitable for open surgery Disadvantages of EVAR - No long-term data about the longevity of the operation The graft can migrate The patients require serial CT to watch for endoleak – because the graft isn’t stitched in, blood can leak around into the aneurysm Mr McGreal’s notes Mortality rate in ruptured AAA - 90% in the community o If don’t die immediately, will bleed retroperitonealy and become hypovolaemic. This will cause the bleeding to stop. Management: patient should be minded, kept calm, oxygen, and don’t give fluids. Hypotension will keep the patient alive! - 50% if make it to hospital The big causes of death in general surgery are ruptured AAA and big GI bleed. Risk of rupture depends on - diameter - sex – women are actually more likely to rupture an aneurism at a smaller diameter. Hence, in men repair AAA when >5.5cm, but in women when >5. Mortality of EVAR – 1-2% Mortality of open repair – 5% Why do patients die after repair? – renal failure, MI, pneumonia, bowel ischaemia, graft infection (1%)