Foundation Testimonials
advertisement

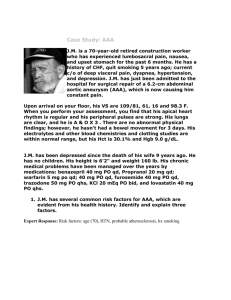
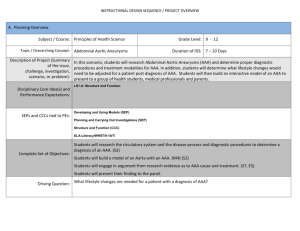
How SVS Foundation-Funded Grants Directly Result in Improved Clinical Practice Rabih Chaer, M.D. I am a 2012 R03 and GEMSTAR award recipient. I was awarded the funding to research vascular wall behavior as a predictor of aortic aneurysm growth and rupture. My study focuses on longitudinal imaging of the aortic wall in patients with a small AAA using contrast enhanced ultrasound. In addition to ultrasound imaging, serum biomarkers testing and immunohistochemistry examination of the aortic wall in patients who require open repair will be used to determine the ability of contrast enhanced ultrasound and serum biomarker testing to detect AAA growth and rupture. The study is ongoing and has recruited 68 patients to date with multiple serial testing intervals. The results of this study will, hopefully, assist the vascular surgeon in clinical practice in determining which AAA requires repair based on the biologic risk of growth and rupture and not only based on the aneurysm diameter alone. Non-invasively detecting the potential of AAA growth and rupture will advance the understanding of the pathophysiology of AAA, allow for the individualized treatment based on the biologic potential for growth and rupture, and potentially improve the outcomes of AAA repair. Gregory Landry, M.D. I am a 2005 K23recipient. I was awarded the funding to research functional outcomes of critical limb ischemia. My study found that patients undergoing revascularization for critical limb ischemia experience significant improvement in isometric muscle strength, which directly correlates with quality-of-life improvements. Traditional methods of evaluating functional improvement in patients with intermittent claudication, such as walking distance, walking speed and balance, were less reliable predictors of improvement in patients with critical limb ischemia, most likely reflecting their increased baseline disability. These findings provide new potential markers for evaluating patients with critical limb ischemia, which is an ever-growing patient demographic Christopher L. Skelly, M.D. I am a 2009 Jointly Sponsored Mentored Clinical Scientist Development Award recipient. I was awarded the funding to research and develop a therapeutic virus (R7020) that is efficacious in the prevention of vein graft failure from intimal hyperplasia. Through the support of the Foundation, I was able to perform work that was proof of principal and demonstrated (1) the stimulation of vascular smooth muscle cell proliferation appears to be an early and transient process and responds to a single dose of therapeutic R7020, (2) the target tissue is directly accessible during the therapy and (3) R7020 was demonstrated to preferentially infect and inhibit the proliferation of vascular smooth muscle cells that form the scar tissue. As the research progressed, I was able to focus more on the mechanistic components of the virus to explain the antiproliferative effect. In a series of studies, I demonstrated that R7020 blocks caspase-3 dependent apoptosis (PNAS ) of smooth muscle cells; different strains are dependent on activated MEK (Gene Therapy 2013) depending on the number of copies of the gene γ1 34.5 genes; most recently we demonstrate that R7020 induces syncytia formation in vitro and in vivo which serves as a mechanism to distribute the virus, to evade immune detection and to reduce inflammation by fusing immune cells into the syncytia (PLOS ONE 2015). Based on these results I have formed a company, Maji Therapeutics, whose mission is to improve clinical outcomes for patients undergoing cardiovascular surgery by using a novel, ex vivo approach employing therapeutic viruses that prevent pathologic vein graft failure due to restenosis. This pathway of bench to bedside is challenging. Maji Therapeutics is currently raising money to initiate a Phase 1 clinical trial. The entity of intimal hyperplasia remains an unmet clinical need and translation of innovation in this field has been slowed by the failure of the PREVENT trials. With the help of the foundation, I have been able to demonstrate a proof of principal to Industry and have received valuable feedback. Work continues on this project to ensure that I successfully navigate the “Valley of Death” to make therapy a clinical reality.