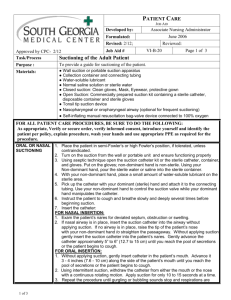
Suggested Sequence of NGT Insertion
advertisement

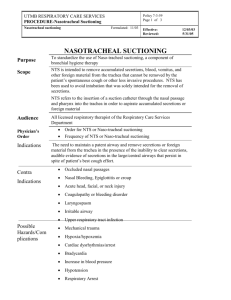
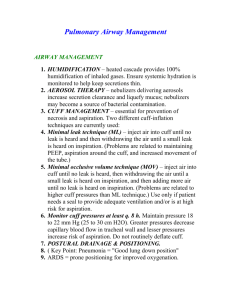
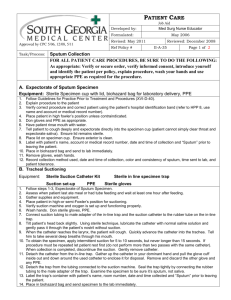
Learning Guide for Oxygenation 1. Define the following: Acidosis Adventitious Alkalosis Apnea Atelectasis Bronchietasis Crackles Cyanosis Dyspnea Expectorant Hemothorax Hyperventilation Hypoventilation Hypoxemia Hypoxia Intubation Narcosis PEP Pneumothorax Spirometer Sputum Tension pneumothorax Tracheostomy Ventilation Wheezes 2. Describe how the brain stem controls ventilation. 3. Describe how clients with COPD stimulate breathing. 4. Name three basic factors which can interfere with adequate ventilation. 5. What type of disease can lead to alterations in diffusion? 6. Discuss pathology that affects perfusion. 7. List seven clinical manifestations of inadequate ventilation. 8. List nursing interventions to prevent pulmonary problems, are at risk for pulmonary complications, or have had surgery. 9. Compare and contrast suctioning with single-use catheters, multi-use catheters in sleeves, and closed suctioning systems. 10. Discuss maintenance of chest drainage systems. Student Name__________________________ Campus Lab Activity: Oxygenation At the end of the laboratory session the student will have completed all of the following skills. Each student will work with a partner who will initial each section as it is completed. After completing the checklist, the student and the partner must sign that the skills have been completed. The student must have the instructor verify and sign that the unit is complete before leaving the lab. Respiratory Assessment: perform a focused assessment of the respiratory system. 1. __ Gather appropriate equipment 2. __ Conduct respiratory history 3. __ Vital signs, including pulse-oximetry 4. __ Assess lung sounds in all fields 5. __ Assess chest excursion and shape of chest 6. __ Assess tactile and vocal fremitus Oxygen administration 1. __ O2 cylinders a. Check pressure gauge b. Tighten flow regulator c. Attach tubing to Christmas tree d. Open valve e. Open regulator and set rate 2. __ Nasal cannula a. Attach tubing b. Verbalize maximum flow rate 3. __ O2 masks a. Simple b. Mask with reservoir c. Venturi mask with adaptors 4. __ Humidifiers/nebulizers Nasotracheal Suctioning 1. __ Gather appropriate equipment 2. __ Assess client for signs of airway obstruction a. Coughing b. Secretions in airway c. Labored breathing d. Restlessness or irritability e. Decreased oxygen saturations or level of consciousness f. Lung sounds 3. __ Prepare equipment a. Open kit or catheter using aseptic technique b. Using aseptic technique, don gloves and pour NS into basin c. Attach nonsterile suction tubing to sterile catheter, keeping dominant hand sterile d. Check suction and wet catheter by suctioning NS from basin 4. __ Suctioning a. Use dominant hand to insert catheter into nares approximately 6 1/2 inches for adults (about the distance from nose to base of earlobe) or until client coughs or obstruction is met b. Apply suction ONLY ON WITHDRAWAL of catheter and rotate catheter to include as much surface area as possible. Do not apply suction for more than 10 to 15 seconds. c. Assess client for heart rate and lung sounds and repeat after one minute up to 3 times total d. Rinse catheter and tubing before disconnecting and disposing of equipment Tracheostomy Tubing Suctioning 1. __ Gather appropriate equipment 2. __ Assess client (see above). DO NOT suction if HR is <80 or >120 3. __ Prepare equipment – see above 4. __ Suctioning (follow ADN nursing skills videos and check off sheets) Tracheostomy Care 1. __ Suction trach as needed prior to tracheostomy care 2. __ Have appropriate trach care equipment ready at bedside 3. __ Care (follow ADN nursing skills videos and check off sheets) Chest drainage systems 1. __ Examine chest drainage system ________________________________ Student Signature ________________ Date ________________________________ Partner Signature ________________ Date ________________________________ Instructor Signature ________________ Date Tracheostomy Suctioning (Note * Indicates Critical Element in Skill Performance) S/U 1. Assess/determine need for suctioning AEB: a. Audible, gurgling respirations b. Obvious mucous at trach. site c. Restlessness, distress d. Pulse oximeter reading of <90 and/ or e. Patient request *2. Demonstrate safety prep measures. 3. Check suction equipment, setting pressure at 80 to 120 mm/Hg continuous suction 4. Assist client to high fowlers or semi-fowlers position. * 5. Loosen cap on sterile saline Open suction kit and sterile receptacle for saline. *6. Pour saline into sterile receptacle Don sterile gloves * 7. Use non-dominant hand to attach suction tubing to sterile suction catheter.. * 8. Wrap catheter in dominant sterile hand to maintain sterility *9. Lubricate tip of suction catheter with saline. *10. For non-ventilated client, assess need for hyperoxygenation and do so if necessary: a. Have client take 2 or 3 deep breaths or b. Hyperoxygenate with Ambu bag. For ventilated client: Hyperoxygenate * 11. Open suctioning: a. Without suctioning, use dominant sterile hand to insert suction catheter into tracheostomy until cough reflex is stimulated or resistance is met. Do not force catheter if an obstruction is met. c. Apply intermittent suctioning while rotating sterile catheter between thumb and index finger as catheter is withdrawn. In-line suctioning: a. Open access valve and insert catheter located in plastic sleeve into tracheostomy. b. Apply intermittent suction while rotating and withdrawing completely back into plastic sheath.catheter . *12. Limit each suction pass to 10 seconds *13. Assess cardiopulmonary status after each suction pass. e.g. radial pulse, apical pulse, breath sounds, and/or oxygen saturation 14. Repeat suctioning steps based on assessment. Limit suctioning to 3 passes 15. D/C suction, discard equipment and perform hand hygiene 16. Document assessment, procedure, and client response Tracheostomy Care (Note: * indicates a critical element in skill performance) S/U 1. Assess need for trach. care *2. Perform Safety Prep measures 3. Check suction equipment (if ordered) and set suction per orders 4. Position patient in high fowlers. 5. Don clean gloves, remove dressing and assess for drainage. 6. Discard dressing, remove gloves. Perform hand hygiene. 7. Loosen caps on cleaning solutions (e.g.normal saline and hydrogen peroxide) *8. Open tracheostomy kit, remove and don sterile gloves *9. Remove sterile drape from kit and place on client’s chest. *10. Set up sterile field and arrange contents of kit onto sterile field 11. Pour saline and hydrogen peroxide into separate containers with nondominant hand 12. Remove trach collar *13. Remove inner cannula with non-dominant hand by grasping the outer ring of the cannula, and immerse in hydrogen peroxide *14. Clean inner cannula with brush, maintaining sterility *15. Immerse and rinse cannula in saline or sterile water *16. Remove cannula from rinse solution, dry with pipe cleaners, and/or tap gently to remove excess droplets *17. Replace inner cannula *18.Clean stoma site with sterile cotton tipped applicator and/or sterile gauze moistened with saline 19. Assess stoma for evidence of irritation, erosion, edema 20. Clean flanges and outer cannula using gauze square moistened with saline 21. Apply new dressing to trach site. If trach ties are soiled, replace 22. Discard equipment and gloves; perform hand hygiene 23. Document assessment, procedure and client response