Rodent Viral Containment
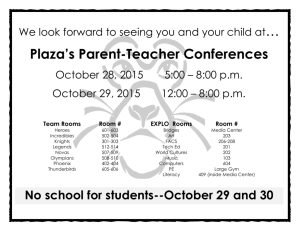
advertisement
Rodent Viral Containment Date Issued: May 29, 1998 Date Revised: April 14, 2009 (4) Ed.: D. Larsen Comparative Medicine Resources A. PURPOSE The purpose of this SOP is to describe a plan of action to contain and eliminate adventitious viral infections. B. RESPONSIBILITY Communicate 1. Veterinary technician in consultation with veterinary staff will confirm results with reference laboratory; seek secondary testing and ensure samples or labeling was correct. 2. Veterinary technical staff will identify and tour affected rooms, collect names of investigators, and use previous rodent transfer forms to track relocations of animals from infected rooms to other rooms or institutions. 3. Veterinary technical staff will under direction from veterinarians condense similarly affected rooms where possible. 4. Veterinary staff will update Rodent Room Order 5. Veterinary staff will notify Assistant Director for Operations of outbreak; Supervisor(s) to reassign room duties as needed. 6. Veterinary technicians will post room door alert signs re: breeding, transfer, transport, hygiene, cross-contamination in the lab and where and how to discard contaminated PPE. [See Sample] 7. Director’s executive assistant will notify Principal Investigator via mass email [See Sample] 8. Veterinary staff will call each Principal Investigator by telephone; leave voicemail if not available. Get commitment of final terminal use of rodents via experimental attrition Contain and Eliminate 9. Director will determine viral elimination by: a) attrition versus b) “burn-out” 6-8 weeks, then 3 negative results if “burn-out” was used or immediate if the room undergoes complete depopulation and sanitation. 10. Husbandry supervisor will review cage-wash performance via temperature log to ensure cage-wash was performing optimally. Cage wash repair will be immediately called by the Facility manager or Facility supervisors if cage wash temperature problems are subsequently detected. 11. Upon initial detection of the virus, rodent breeding pairs must be separated within 7 days by PI staff or will occur by CMR personnel. No breeding is allowed in an animal room once a viral infection is detected. 12. If room where pathogen is detected is conventionally housed, conversion to individually-vented caging should be done by husbandry staff promptly when available, otherwise micro-isolator cages. At 60 days post-detection, when technically possible, remaining rodent cages will be converted to barrier housing by CMR husbandry personnel and billed at the barrier per diem rate. Rodent Enrichment: 2 January, 2009 (6) 13. Research staff must return soiled empty cages to infected room. 14. After all clean rooms are attended at the end of the business day, CMR staff will transport soiled cages to the cage-wash and promptly clean them before the next day. 15. All infected soiled cages moved inside dirty cage-wash nightly. 16. Order new sentinels for affected rooms when depopulation and complete room sanitation has occurred or when viral “burn out” is presumed. Follow-up 17. Check once monthly at time of cage census per protocol number to evaluate for decrease in number of cages. Tour each affected room rather than rely on census data. 18. After the initial detection husbandry and veterinary technical staff will check once weekly for pregnant females or litters. All apparently pregnant female rodents will be immediately sacrificed by laboratory personnel within 24 hours of detection. 19. Once room is vacated, husbandry staff will thoroughly disinfect all surfaces of the room especially sink knobs, phones, log-books, light-switches, switch plates, supplyand exhaust-grills and door handles. When possible, CMR will re-populate with a species that cannot be infected with the pathogen previously identified i.e. rats to replace mice infected with mouse hepatitis virus. 20. Animal rooms will remain empty a minimum of 24 hours prior to repopulation. C. SAMPLE LETTER [EDITcontent i.e. room numbers, dates, affected investigators, viruses] Dear Dr. Smith and Staff, Yesterday the Research Animal Facility detected mouse parvovirus (MPV) in Room A632 via our sentinel surveillance program. This room tested positive for mouse rotavirus (EDIM) in July 2008 and continues to test positive for EDIM this quarter. The next testing will be in January 2009. These viruses are non-zoonotic since they only infect mice. Parvovirus affects lymphoid tissue and the rapidly-dividing cells of the gastrointestinal tract. Clinical signs of disease are not apparent and the primary concern for interference in research is immune modulation. The virus may contaminate cell lines including tumors. Transmission of both viruses is by mouse fecal-oral contact of mouse feces to their fur, caging, bedding or your gloves and lab equipment that is in direct or indirect contact with another mouse. Rotavirus can alter results of studies with infant mice, and increased morbidity (diarrhea from birth to ~day 14) and mortality of mouse pups may be observed. As with any pathogen, the immune response of the animal may also be altered. Disease Control. Mouse parvovirus can only be eliminated through attrition of the mouse colony or by caesarean or preferably embryo rederivation. Rotaviral infections are self-limiting after 4-6 weeks unless naive animals (born or newly housed) are introduced into the colony room. We recommend that newly acquired valuable or irreplaceable mice that are housed long-term to be housed in the barrier for heightened biosecurity. Rodent Enrichment: 2 January, 2009 (6) Visits or mouse shipments with colleagues at other institutions must be carefully evaluated. Please note that other research animal may be infected with thse viruses. Because we can transport these infectious agents among institutions via fomites on skin, hair, clothing, paper or equipment,, consult veterinarians in the laboratory animal departments at each institution. CMR Staff Will: Continue to require separation of breeding rodent pairs in the conventional facility. Euthanize pregnant females upon detection Reassign future rodent vendor shipments and post-operative transfers to Room XXX or a clean non-affected room. Encourage euthanasia of non-essential affected rodents Euthanize all parvovirus infected rodents 90 calendar days after the date on this letter. Furnish disposable garb Return soiled caging from Room XXX to the dirty side of cagewash All CMR and Research Laboratory Staff Will: Continue USING disposable garb: gown, shoe covers, gloves, mask and bonnet Follow strict room order each day as described in Rodent Room Entry without return to rooms higher on the list Spray MB-10 (Vimoba) to all equipment and supplies that leave the room or have been in contact with infected mice in the room or in the laboratory. Spray wheels of carts. After hours (4 p.m. to 9 a.m.), place soiled caging including wire food racks, water bottles and cagecards on cart or rack in each room. (CMR staff will relocate the caging materials to the dirty side of cage-wash daily). During business hours, placed soiled caging in dirty side of cage-wash--do not leave in hallway. NOT transport rodents TO either of these rooms from other rooms. NOT transport rodents FROM either of these rooms to other rooms. Avoid fecal contamination in the laboratory. Clean laboratory equipment in contact with mice thoroughly and spray with chlorine dioxide solution e.g. Vimoba ® or MB-10 ® or autoclave. REQUEST chlorine dioxide AS NEEDED FOR DECONTAMINATION OF LAB SURFACES AND LAB EQUIPMENT PLEASE NOTE THAT Vimoba ® and MB-10 ® MUST BE MADE FRESH ONCE WEEKLY Please forward this message to all personnel who handle the animals, their carcasses or caging or enter the animal facility. New sentinel mice will arrive soon. I will keep you posted of the most recent sentinel test results. Your cooperation helps to protect everyone’s research. Thank you