CHAPT 05 Intestinal Absorption
advertisement

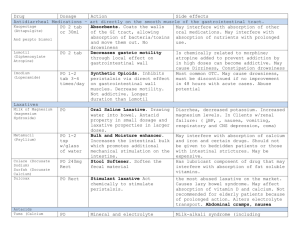
Chapter 5. Digestion and Absorption of Minerals K ey : Minerals present in food are part of a food matrix consisting mainly of protein, complex carbohydrate and fat. Digestion is targeted at the matrix structure, using hydrolytic enzymes to degrade and eventually liberate the minerals from there captive surrounding. Macrominerals tend not to be bound firmly in such complexes. In contrast, microminerals are more firmly fixed to the matrix molecules and hence complete release is not in the offing. The acidity of the stomach aids in both releasing the mineral from the matrix and rendering it into a free and soluble form. Very little absorption, however, takes place in gastric cells and hence the bulk of mineral absorption must await entrance into the duodenum and mucosa beyond. There is a danger, however. Entrance into the duodenum is accompanied by a drastic rise in pH, from an acidic environment of gastric juice to the modest alkaline environment of the duodenum. As noted in Chapter 2, an alkaline environment works against solubility of many minerals and thus without the assistance of solubilizing factors, many microminerals, and to some extent macrominerals tend not to be absorbed. DIGESTION 1. General Principles The purpose of digestion is to render large composite macromolecules in food into smaller more manageable components. This is achieved by a group of hydrolase enzymes that are present through out the digestive tract and within the membranes of absorbing cells. There are three distinct stages in the digestion process, (1) salivary, which involves amylases secreted from the salivary gland that breakdown glycogen and starch, , (2) gastric, which concerns mainly pepsin secreted from chief cells that attack proteins (3) mucosal, which involves both trypsin and chymotrypsin synthesized in the pancreas and released into the duodenum to digest proteins. The second phase of mucosal digestion uses peptidase and glycosidase that are embedded in the membranes of the absorbing mucosal cells as a final phase by attacking smaller peptides and di-and trisaccharides allowing them to enter as individual amino acids and monosaccharides. Incidental to the action of these enzymes is the release of the minerals such as iron, calcium, magnesium that were in the food matrix. Spared from the digestion are amino acids and monosaccharides, which can function in aiding the solubility and absorbability of minerals. ABSORPTION I. General Principles Postdigestion processes in the absorbing region of the intestine expose minerals to a whole new environment of cells. Cells that line the intestine are basically columnar epithelialcells with a pronounced microvillus lining their exposed surface. Passage into the system confronts first the microvilli on the outer boundary which form the absorbing surface supported by a membrane that regulates movement into the cytoplasmic interior. Absorption is not complete until the passage from the entry portal release from the opposing surface is completed. Once thought to be a simple oozing through a mucosal barrier, minerals absorption in the small intestine is now regarded as a highly complex, energy-driven process tuned to the prevailing mineral content within the system. Understandably absorption is a key site for mineral-mineral interactions, and mineral sequestering, which potentially can disrupt the orderly flow of minerals into the system. It is at the intestinal stage that the system is at its highest level of vigilance against excessive mineral intake. To approach absorption we key on membrane transport systems that pass minerals across intestinal cells. We also key on the energy factors driving these processes as well as their regulation and mechanism. Intestinal absorption and bioavailability are at the heart of nutritional need and both decide the difference between a healthy outcome or a not- so-healthy mineral deficiency. O bjectives: 1. To characterize specific intestinal transport systems for minerals, 2. To gain insight into the mechanism for moving a mineral across the barrier, 3. To learn what regulates the action of membrane transporters, 4. To identify factors in the diet that impede or aid the absorption of specific minerals. Guiding Principles of Absorption Control of a mineral’s homeostasis within the system begins at the absorption stage. Below is a list of 6 key factors that must be addressed when deciding the absorption of minerals. All of these factors have been determined by careful studies of the absorption process relative to particular minerals. 1) Absorption can be highly selective for the form of the mineral, 2) Absorption of a particular mineral is greater when there is a nutrition need for that mineral, 3) Most dietary factors that impede a mineral’s utilization by the system exert their action at the absorption phase, 4) Metal antagonism can arise when two minerals compete for a common portal, 5) Vitamins and hormones that facilitate the passage of specific minerals (Ca2+, HPO4=, Mg2+, Fe2+) generally work at the level of intestinal absorption, 6) For many minerals, especially microminerals, absorption depends on the movement of vesicles that cycle between the luminal surface membranes and an internal compartment. 2. Absorption of Macrominerals 1) Sodium and Chloride Macrominerals such as Na+ and Cl- have the advantage of occurring in bulk amounts in the diet and are present in foods mainly as unattached ions. Consequently, digestion aimed at liberating sodium and chloride from the food matrix is not a major concern. A second point to consider is that sodium ions being present in bulk amounts are a major force driving other components inward via a co-transport mechanism. Figure 5.1 shows transporters for glucose and amino acids use the energy from sodium gradients to drive glucose and amino acids into the mucosal cells. A third uses an ATP-driven hydrolysis of water to Blood Apical (lumen) side Na+ Na+ Cl- Glucose Glucose cotransporter Amino acids Amino acid transporter Na+ H+ Na+/H+ antitporter H+ Carbonic anhydrase H+ + HCO3- H2CO3 CO2 CO2 H2O Cl- HCO3Anion antiporter Intestinal Enterocyte Figure 5.1. Absorption of Na+ and Cl- across the intestine. create and then drive the exchange of Na+ for H+ thus maintaining electroneutrality. The glucose- and amino acid cotransporters aptly demonstrate the power of simple diffusion in intestinal absorption, which accounts for about 50% of the Na+ taken in through the intestine; electroneutral cotransport accounts for only about 20%. Both the sodium-glucose and the sodium-amino acid transporter systems are on the apical surface of the enterocyte and show interdependence to one another. This illustrates an important nutritional point, that glucose and amino acids themselves are powerless to penetrate the enterocyte without sodium ions providing the energy. In contract to Na+, the absorption of Cl- relies on an exchange reaction replacing bicarbonate anion with Cl- (Fig. 5.1). The bicarbonate (HCO3-) is a synthesized from CO2 via the enzyme carbonic anhydrase. HCO3- arises by dissociating a proton from carbonic acid (H2CO3) which positions the H+ to partake in the Na+/H+ exchange. In general the amount of Na+ and Cl- taken into the organism is not regulated at the intestinal stage. Maintaining homeostasis within the system, therefore, shifts to the kidney and to a lesser extent, biliary secretions and sweat glands. The co-transport with glucose renders carbohydrate- rich diets competent to raise the sodium intake, which makes organic components in the food source a deciding factor in the amount of sodium taken into the system. 2) Potassium Potassium is the most abundant cation in the body with the body load estimated at between 3000-4000 millimoles. Nearly 98% of this is within cells. It is no wonder, therefore, that there is an exceptional need for potassium in the diet and absorption systems for potassium operate at nearly 100% efficiency with both proximal and distal parts of the intestine taking an active part. In contrast to sodium, there is no glucose or amino acid co-transport with potassium. Rather, potassium relies on conductance channels across the membrane with energy provided by a H+/K+-ATPase similar to the H+/Na+ mentioned earlier, but selective for potassium ions. Potassium is also absorbed through a K+/Cl- cotransporter. As with sodium, potassium absorption is unregulated at the intestinal stage and requires the kidney to maintain homeostasis. Indeed, it has been estimated that the kidney will eliminate the daily dietary load of potassium in a 24 hour period. Figure 5.2. Potassium channel in the membrane. The V-shaped funnel has the cytoplasmic side facing down. A channel is formed by the interaction of 4 proteins with identical subunits. 3) Calcium In the realm of the divalent cation transport, there is an increasing propensity for dietary factors to be more influential in the absorption process. One reason is because divalent as opposed to monovalent cations form stable complexes with proteins and other factors in the diet. Thus, divalent cations such as Ca2+, Mg2+ do not share the same high absorption efficiency as monovalent ions. Researchers have attempted to elucidate the mechanism of calcium absorption across the intestine with this thought in mind. Magnesium predictably has some overlap with calcium. Calcium absorption, however, unlike magnesium is clearly dependent on vitamin D, specifically the 1,25 dihydroxy derivative of the vitamin. Calcium crosses the intestine by two major avenues; through the cell barrier or around it. Through the cell (transcellular) accounts for most of the calcium absorbed. Around the cell (paracellular) is mostly by diffusion and is unregulated. Transcellular is a metabolically active, Figure 5.3. A calcium channel protein in the membrane. The channel for calcium is formed by a single polypeptide chain crossing the membrane in four different locations. -Vit D - Vit D + 1,25-(OH)2-D3 100 100 Calcium Absorbed Non-Saturable 50 50 Saturable 0 0 0 100 200 Dietary Calcium 0 100 200 Dietary Calcium Figure 5.2. Absorption of Calcium in the Duodenum of the Rat oxygen-dependent process that moves calcium against a concentration gradient. Vitamin D is required for this system. Studies with intestinal segments suggest that the proximal end of the intestine is most active in transporting calcium. In the presence of 1,25 dihydroxy-D3 (the most active form of vitamin D) calcium uptake is curvilinear with increasing dietary calcium as seen in Figure 5.4. The response is suggestive of a saturable system, suggesting a carrier. Without the vitamin, calcium still enters the cell but the uptake is by diffusion and is no longer regulated. In Figure 5.3, its can be seen that other than the duodenum, the jejunem is the only other segment of the intestine that shows saturable uptake in the presence of vitamin D. One may surmise that it is within these regions most of the calcium is absorbed. 1) Calbindin as a mediator of calcium uptake It could be argued from kinetic analysis that diffusion alone cannot account for the rapidity with which calcium ions move across the intestine. Instead, the data imply the existence of a rapidly moving carrier facilitating the transfer. Efforts to identify the carrier led to the discovery of a small, 9 kilodalton protein that appeared to be specific for calcium. The protein was given the name calbindin. Biochemical studies have since identified two high affinity binding sites for calcium in calbindin, showing that a modest calcium input can still lead to major calcium incorporation. Calbindin concentration in cells can be as high as 0.2-0.4 mM, which suffices to augment calcium movement under conditions prevailing in cells. Moreover, it now appears that the enhancement of calcium transport correlates strongly with the level of calbindin in the transporting cell. Recently, 1,25-dihydroxy-D3 has been shown to control the synthesis of calbindin at the level of transcription and post-transcription, thus suggesting that calbindin is the agent that makes possible vitamin D-dependent calcium transport. Linking vitamin D with calbindin has thus help explain how vitamin D controls calcium uptake. It should also be noted that calbindin null mice (those unable to make the protein because of the inactivation of the calbindin gene) do not lose the ability to transport calcium, which suggests other calcium transporters are present. Moreover, calbindin is also expressed in a variety of tissues including uterus, kidney, pituitary gland, and bone and thus may be regulated by other factors in a tissue-specific manner. Duodenum Jejunum Ileum 100 Non-saturable 50 Saturable 0 Saturable 0 0 100 200 0 0 100 200 0 100 200 Calcium Instilled, mM Figure 5.3. Uptake of Calcium in Different Regions of the Intestine. Only the ileum of the intestine is incapable of absorbing calcium in a regulated manner. 4) Magnesium and phosphate On first impression one may consider the absorption of magnesium to mimic calcium. Such is not the case, however. Isotopes of magnesium (28Mg2+) tend to support the conclusion that the ileum and colon, not the jejunum, are more active in absorption of this metal ion. Like calcium, however, magnesium employs both active (energy-dependent) and passive (diffusiondriven) transport. Active is characterized by saturation with increased intake. Generally the response to magnesium is curvilinear, suggesting saturation at the higher levels and diffusion at the lower. Diffusion, however, only accounts for 7-10% of the magnesium taken in. This signals involvement of a mediated factor that conducts the movement across the membrane. Unique to magnesium that was not seen with either sodium or potassium was the lowering of the fractional absorption with increasing amounts in the diet. For example, raising dietary magnesium from 0.3 mmoles (7 mg) to 1.5 mmoles (36 mg) lowered the fractional absorption from 65-75% to 11-14%. Unlike Na+ and K+, Mg2+ intake is clearly subject to regulation at the absorption stage. One other striking observation is the apparent interference of Mg2+ absorption with Ca2+ and phosphorous (as phosphate). That observation infers the two divalent cations may share a common carrier or entry portal and could be subject to the same regulation. Long term studies, however, dismiss interference between the two, but in the short term the fractional uptake of Mg2+ is clearly influenced by the presence of Ca2+. Isolated segments of the intestine suggest magnesium absorption is greatest in the ileum and not the jejunum, which is the opposite of what is seen with calcium. As noted, phosphorous seems to antagonize both calcium and magnesium (Fig. 5.4). Evidence supporting commonality between magnesium and calcium is the observation made with phosphorous. Phosphorous hinders absorption of both magnesium and calcium. Conversely, magnesium inversely affects phosphate and to a lesser extent absorption of magnesium. 7 3.2% Ca, 0.8% P 6 0.9% Ca, 0.8% P (normal) 5 Daily weight 4 gain (g) 3 2.5% Ca, 1.7% P 2 1 0 0 30 60 120 180 240 360 600 1200 Log of Dietary Mg (mg/100g) Figure 5.6. Uptake of Calcium in the Presence of Magnesium and Phosphorous. Guinea pigs were fed increasing amounts of magnesium in diets that were fixed in calcium and/or phosphorous. Daily weight gain was determined for each amount. It is hard to conclude that all three minerals vie for a common carrier, certainly not an anion vying for a cation carrier or entry portal. The last argument for magnesium and calcium having their own unique systems of entry comes with the role of vitamin D on the two. Although there is some disagreement among laboratories, the overwhelming opinion appears to be that neither vitamin D nor any of its metabolites at physiological doses influence the 3. MICROMINERAL ABSORPTION Microminerals display a variety of transport systems for movement across the intestine. Some recognize more then one mineral. All adapt to the form of the mineral in the lumen and work closely with factors that allow penetration on the apical surface and release on the basal surface of the enterocyte. Because of the selectivity each micromineral must be discussed separately. IRON Valance state and organic form are the two major determinants of iron penetration into a mucosal cell. Organic iron in a food digest is present as heme, a complex of iron with porphyrin and representing the most common biochemical form of iron in the diet (Chapter 4). Inorganic iron, often referred to as non-heme iron, is dependent on valence. As we noted in Chapter 2, iron present as Fe2+ is more soluble that Fe3+ . The Fe2+ is generally the preferred form for effective uptake, although oxygen in the water can readily oxidize Fe2+ to Fe3+, which then precipitates out as an insoluble polyhydroxy complex. A further concern is that because of its redox activity, iron is a highly toxic and can poison a system and through its peroxidant activity. This especially true for free iron that can become localized on the membrane surface of cells in a lipid-rich environment. These factors must be taken into account when considering the mechanism for iron penetration across the intestine. Heme iron is derived mostly from meat and blood proteins such as cytochromes and hemoglobin. Iron in this form is basically soluble and stable, which means it readily passes through the cell membrane as an intact complex. A strongly acidic medium such as stomach acid can cause some of the bound iron to dissociate from the porphyrin ring, but the bulk, however, stays intact. Heme undergoes a quick efficient passage through the mucosa, possibly involving no carrier of mediator and therefore is basically unregulated. These observations form the basis for considering heme iron more bioavailable to the organism. More concern is directed at the passage of non-heme iron or so-called inorganic or free iron. Because this form is insoluble at the pH of the intestine and iron in this form has prooxidant properties, enterocytes release gastroferrin, a mucous protein that coats the absorbing surface and villae of the enterocyte. Gastroferrin retards the polymerization of the non-heme iron keeping the ion in a quasi free singular form for easy passage into the cell at the same time protecting the cell from wanton prooxidant activity. Pathways of inorganic iron uptake Depending of valence of the iron, there are two pathways for inorganic iron uptake into intestinal cells. 1) The ferric pathway. This pathway is mediated by the protein mobilferrin. Mobilferrin is localized in the cell membrane, more specifically in the apical surface of the villae, where a majority of the protein appears to be bound to the gastroferrin in vesicles near the surface. As the name implies, mobilferrin is free to move through the cell with iron trapped within a vesicle. By encapsulating the iron mobilferrin is capable of transcellular movement to the exporting surface on the serosal side where it becomes anchored to integrin, an all-purpose non-specific membrane protein that participates in adhering non-membrane protein to cell surfaces. The complex is further stabilized by HFE, a protein originally found in leucocytes and now speculated to be essential for iron as well as zinc movement from enterocytes. 2) The ferrous pathway. Iron as Fe2+ is the more soluble form. The ferrous pathway features a unique membrane transporter, DMT-1 (divalent metal ion transporter) sometimes called DCT-1 (divalent cation transporter) and formerly Nramp2. The transport is not specific for iron but instead can serve to transport a variety of divalent cations. Movement is from the apical surface of the villae to the basolateral surface. In the ferrous pathway transport can only occur if the iron is in the Fe2+ form. For this reason Vitamin C is capable of facilitating iron uptake by converting iron to the ferrous form (Fe2+) which is the more soluble form. This explains why vitamin C, a strong reductant, tends to enhance iron uptake. As a consequence, a large percentage of iron taken in is able to pass into the mucosal cells. Once inside the mucosal enterocyte, the iron is subject to being trapped by mucosal ferritin which further delays its movement into the system and forms the basis for only a small fraction of the iron taken in diet ever reaching the blood. The DMT-1 transporter for ferrous iron also recognizes other ions in the 2+ form. The latter include Cu2+, Mn2+, Zn2+ and perhaps some macrominerals (Ca2+, Mg2+). This multi-recognition property of DMT-1 form the basis for competition between these metals and forms the foundation of metal ion antagonism. Export stage of iron absorption Passage out of the cells is the final stage of iron transmembrane movement. Mobileferrin mentioned earlier in the uptake is also a component in the release of iron from the cells. The major protein conducting the release is ferroportin. The importance of ferroportin was shown in mice that carried a disabled ferroportin gene (referred to a knockout mutant). The mice were capable of absorbing iron into enterocytes but could not excrete iron from the cells implicating and establishing ferroportin as indispensable for the release of absorbed iron into the system. The discovery of ferroportin draws parallels to the discovery of a protein called IREG (iron-regulatory protein) and MPT1 (metal ion transport protein), which may be one in the same protein. Ferroportin, however, has been shown to have functional and regulatory links to hepcidin, which many investigators in iron absorption have considered to be the master regulatory protein controlling iron absorption at the export stage. ZINC Because zinc transporters need recognize only one valence state, Zn2+, the passage of zinc into the cell would appear to be less complex than multi-valence state ions. This is not the case. The omni presence of zinc in tissues and fluids and cell compartments dictates a need for many different transporters that operate in a variety of cellular environments. Such is the case with the zinc family of transporters, referred to as Zip1-5. Of these, Zip4 is involved in zinc uptake from the intestinal lumen. Most of the other Zip family zinc transporters are located in tissues other than the intestine. Most are designed to operate in environments that vary widely from cell to cell. As an example consider zinc in the brain cells as compared to the zinc in the intestine works in the environment of synaptic vesicles. Neurons with these vesicles in certain brain regions must handle high amounts of zinc and therefore be less sensitive than transporters that work in an extremely sparse zinc environment, which typifies the intestine after a meal. We will discuss the other Zip transports in the chapter on Zinc. Absorption Sites and Zip4 Transporter The absorption of zinc is strongest in the upper intestine which includes the duodenum and ileum. Lower rates occur in the stomach and large intestine. Amino acids, dipeptides, and organic acids present in the lumen tend to hasten absorption whereas slower rates occur when energy is deprived. Entry into the enterocyte, like iron, is facilitated by mucous proteins and carbohydrates secreted by the absorbing cells. As noted Zip4 is the major player in zinc absorption. DMT-1 appears to play a less critical role for zinc entry. The focus on the Zip4 protein and gene represented the outcome of studies aimed at identifying the defective gene in a condition known as acrodermitis enteropathica (AE). Patients with AE display all of the symptoms of zinc deficiency, which include impaired growth, immune system dysfunction and mental disorders. Fibroblasts from these patients are unable to absorb zinc, which points to a zinc-binding protein as the factor. Of the various zinc-binding proteins, most AE patients were found to have mutations in the gene that coded for the Zip4 protein. Zip4 is located in the absorbing surface of the cell or an internal compartment. With a diet deficient in zinc, Zip4 remains mostly on the surface of the enterocyte. Low zinc impairs the inward endocytosis of Zip4 and hence the protein remains strategically positioned to absorb more zinc. In contrast, a high or normal zinc diet leaves most of the Zip4 protein in an intracellular compartment out of contact with luminal surface and in a position where absorbing zinc is prohibited. The movement of the Zip4 protein in AE patients cannot be controlled by zinc and hence these patients are in a chronic zinc-deprived state. Intracellular Movement Movement of zinc through the enterocyte involves more than Zip family proteins. Based on the rate of passage, there appears to be at least two pools of zinc in the enterocyte. One shows a rapid displacement of zinc through the cell; the other a slower movement and a tendency to actively exchange with endogenous zinc. The latter pool represents a more controlled zinc uptake and may even be considered a stopgap response to high zinc influx . The regulated path is controlled by the protein metallothionein. This small, cysteine-rich protein binds and sequesters zinc (not unlike the ferritin with iron). High zinc influx causes metallothionein levels to rise because zinc is a transcription factor for inducing metallothionein synthesis. Blocking the outflow path with a zinc-binding protein is seen as a response that protects the system from absorbing potentially toxic levels of zinc. A second a protein called CRIP (cysteine-rich intestinal protein) binds zinc when zinc input is low and tends to be the factor that gives rapid throughput. The interaction of the two is seen in Figure 5.6. Higher absorptive efficiency correlates with a higher proportion of absorbed zinc bound to CRIP, which strengthen the case for CRIP being the factor that allows rapid uptake. Lower efficiency is seen when zinc is in excess or when the internal supply of zinc is adequate. Thus, the competition between CRIP and metallothionein for zinc is tuned to the zinc status of the individual and the diet and is regulated at the level when zinc enters the intestinal cell. Lumen CRIP Rapid Export Zn Zn Zn Zip4 Exchange Metallothionein Storage Figure 5.6. Intracelluar zinc storage and transport. CRIP (cysteine-rich intestinal protein) COPPER Copper once again reintroduces the importance of valence state in the movement across the intestine. Only about half of the dietary copper enters the system. The lower valence state (Cu+) is the state that is least soluble and could account for most of this loss. Like iron, however, there is a special transporter that recognizes only one valence state of the ion, the Cu+ ion. Although it is likely that some Cu2+ enters the enterocyte via DCT1, Cu+ is form taken in through the uptake channel protein, CTR1 (copper transporter 1). CTR1 that drives intestinal copper transport is present in the membrane as a trimer (three identical subunits) that extends through the bilayer. The trimeric protein forms a hole in the membrane through which copper ions move inside. How copper ion move through the channel is unknown, but since Cu+ behaves more like a closed shell ion, the driving force is likely to be provided by the membrane potential. Working in conjunction with CTR1 is a reductase enzyme that converts Cu2+ to Cu+ preparatory to being taken in by CTR1. Once inside the enterocyte the Cu+ ion can be sequestered by metal-binding proteins which either transfer the copper to other regions or store the copper as metallothionein-bound copper. ATP7A The counter part to the zip4 protein for zinc is a membrane-bound copper transporting protein designated ATP7A. ATP7A is a member of large family of membrane proteins, which as a class use the energy of ATP hydrolysis to drive ions into and out of cells. ATP7A is a membrane bound enzyme that localizes in both the membrane surface as well as internal vesicle compartments, i.e., is found in the membrane of movable vesicles. It is the primary factor exporting copper from the cell as part of the cellular release mechanism. The discovery of AT7A came to light with studies that probed the cause of Menkes’ disease in children. Children with the disease, nearly always males, were unable to absorb copper across the intestine and in so doing developed a severe copper deficiency that proved fatal at about the third year post natal. The disease is actually manifested in utero. A search for the factor led to the discovery of a unique protein that had been described earlier in bacteria and was shown to be involved in the preventing the bacteria from toxic exposure to copper. When the gene for ATP7A, the human form, was isolated and sequence it bore an amazing resemblance to the sequence of the bacterial protein. The research culminated with the discovery that Menkes sufferers had a defect in the gene for this protein. The lesion was found to be in the ATP binding site and in the channel of the protein. More recent data has revealed that ATP7A gene is subject to numerous mutations, most of which are harmless to function. Those that are, however, tend to strike at specific sub-functions of the protein. For example, mutations in the exons coding for the C-terminal region tend to inhibit the protein from localizing to the export surface. Hence, the role of the C-terminal amino acids could clearly be linked to vesicle movement and docking. Studies linking other regions of the protein to function continue today. SELENIUM Selenium in the diet is primarily present as selenocysteine and selenomethionine. One can expect these seleno amino acids to use the same carrier system that are for their sulfur counterparts. In addition, the system can absorb inorganic selenium such as selenate and here the concern is with the solubility. SUMMARY The varieties of minerals that are present in foods present no advantage to the organism until they are freed from surrounding by digestion and absorbed across the intestine into the system. Different minerals employ different mechanisms for accessing the interior of the system, a fact that has made it a necessity to treat each mineral in a novel way and call attention to generalities only rarely when they emerge. The absorption of macro- and to a greater extent micromineral is carefully regulated through adjustments in absorption efficiency. Sodium absorption is coincidental to the absorption of carbohydrates and amino acids. The energy for effecting movement is provided by a diffusion-driven sodium gradient across the membrane as well as ATP hydrolysis. Working to their advantage, macrominerals are highly soluble in the environment of the lumen and move easily in the aqueous phase. Solubility is only one consideration in rationalizing a need for a ligand. Because they lack the quantity, microminerals rely on proteins to bring about absorption. This is tantamount to saying that diffusion-controlled mechanisms do not apply to the intestinal absorption of microminerals and shifts emphasis to the role of membrane factors that represent portals for entrance. These portals work in conjunction with energy driven movement provided by ATP. The release phase of absorption is critical to bringing the absorbed components into the system. Here, the concern is regulation and control of entry to safe guards against excess uptake.