Myalgic Encephalomyelitis/Chronic Fatigue Syndrome:
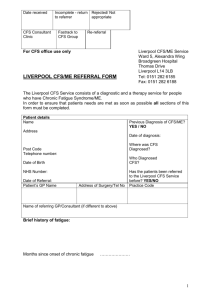
advertisement

Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Clinical Working Case Definition, Diagnostic and Treatment Protocols BM Carruthers et al. Journal of Chronic Fatigue Syndrome Volume 11, Number 1, 2003 ______________________________ LIST OF CONTENTS ABSTRACT 7 INTRODUCTION 8 DIAGNOSTIC PROTOCOL 11 Clinical Working Case Definition 11 General Considerations in Applying the Clinical Case Definition to the Individual Patient Discussion of Major Features of ME/CFS Fatigue Post Exertional Malaise and/or Fatigue Sleep Dysfunction Pain Neurological/Cognitive Dysfunctions Autonomic Manifestations Neuroendocrine Manifestations Immune Dysfunctions Positive Diagnosis Using Suggestive Signs 13 14 14 15 16 16 17 18 19 20 21 Features of ME/CFS in Children 21 Clinical Evaluation of ME/CFS 22 Differences Between ME/CFS and FMS (Fibromyalgia Syndrome) 26 Differences Between ME/CFS and Psychiatric Disorders Depression Somatization Disorder 27 27 28 Assessing Prognosis 29 Assessing Occupational Disability Requirements of the Occupational Disability Assessment Assessing Symptoms of Person’s Disability Assessing Rehabilitative Potential Medical Documentation and Opinion 30 31 32 34 35 TREATMENT PROTOCOL 36 General Considerations 36 Page numbers locate the headings as they appear in the published journal article. [Document 5] Goal and Guidelines for Management/Treatment Programs 36 Individualizing Management Programs: Lifestyle Practices and Self-help Therapies Patient Education Self Development Maximizing Sleep Balanced Diet and Nutritional Considerations Appropriate Body Movement and Fitness 39 39 41 41 42 42 Individualizing ME/CFS Exercise Programs Initial Patient Evaluation Optimize Medical Management Before Introducing an Exercise Program Principles of Treatment Write an Individualized Exercise Program in Conjunction with the Patient Cautions Regarding Exercise/Rehabilitation Programs 43 44 44 44 45 46 Cognitive Behavior Therapy (CBT) and Graded Exercise Therapy (GET) 46 Treatment of Symptoms Causing Major Impairment and those Causing or Aggravating Other Symptoms 49 Therapeutic Principles Sleep Disturbance Pain Fatigue Cognitive Dysfunctions Dizziness/Orthostatic Intolerance Irritable Bowel Syndrome Anxiety States Depression Others (NADH, Magnesium, Simple Symptomatic Relief) Treatment Directed to Possible Pathogenic Mechanisms 49 51 52 55 57 58 60 60 61 64 64 Immune Dysfunction Central Nervous System/Autonomic Dysfunction RESEARCH OVERVIEW ME/CFS Symptoms: Description and Research Findings Post Exertional Malaise and Fatigue Sleep Pain Associated with Neuropathy Neurocognitive Dysfunctions Memory Management of SensoryInformation Autonomic Dysfunctions 65 67 68 68 68 69 70 70 71 72 73 73 Page numbers locate the headings as they appear in the published journal article. [Document 5] Cardiac/Circulatory Abnormalities and Neurally Mediated Hypotension (NMH) Neuroendocrine Dysfunctions Immune Dysfunctions Antiviral Defense Pathway Dysregulation Infectious Agents Differences between ME/CFS and Depression Future Research 73 76 76 77 78 79 80 AUTHORS’ NOTE 81 Consensus Panel 81 Consensus Coordinator 82 Acknowledgements 82 NOTES 83 REFERENCES 83 LIST OF APPENDICES 1. Glossary of Acronyms 98 99 2. ME/CFS Symptom Prevalence and Severity 101 3. Symptom Severity and Severity Hierarchy Worksheet 102 4. Signs and Symptoms 104 5. ME/CFS Clinical Diagnostic Worksheet 105 6. American College of Rheumatology 1990 Criteria for the Classification of Fibromyalgia 107 7. ME/CFS Patient Evaluation Worksheet 108 8. Protocol for Therapeutic Medication Trials 9. Poor Balance, NMH (Neurally Mediated Hypotension), POTS (Postural Orthostatic Tachycardia Syndrome) and Vertigo 112 10. Karnofsky Performance Scale 114 11. Work Place Aggravators 115 12. Tests That May Be Used Inappropriately in the Assessment of ME/CFS 115 113 Page numbers locate the headings as they appear in the published journal article. [Document 5]