Oxidative stress relevant genes and the risk of
advertisement
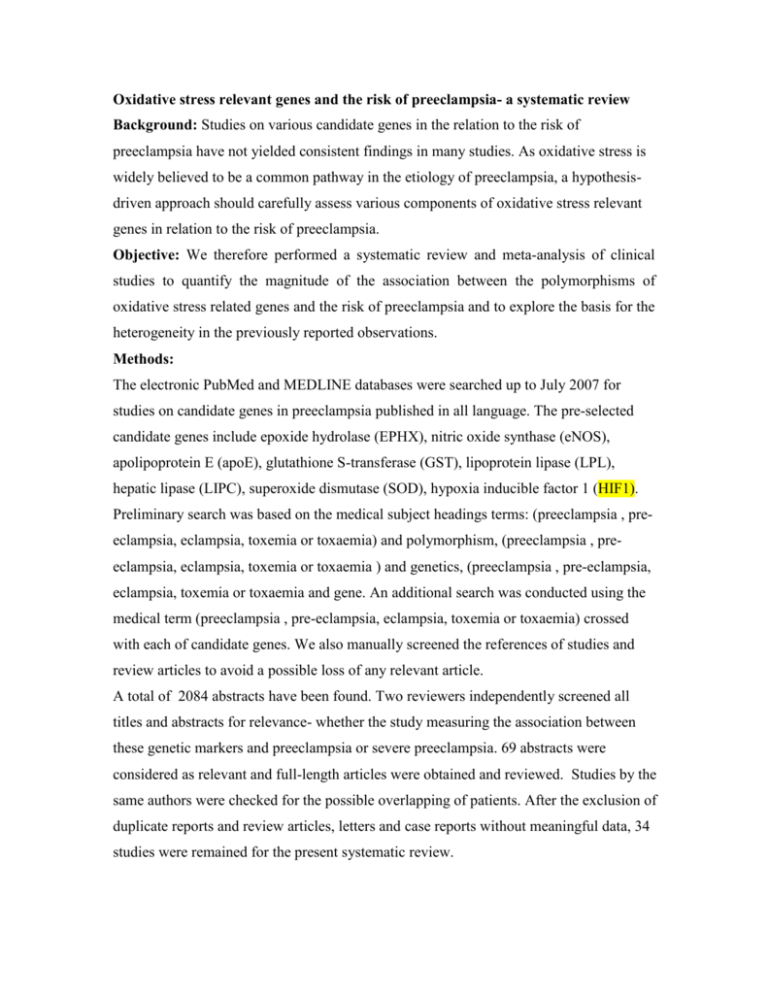
Oxidative stress relevant genes and the risk of preeclampsia- a systematic review Background: Studies on various candidate genes in the relation to the risk of preeclampsia have not yielded consistent findings in many studies. As oxidative stress is widely believed to be a common pathway in the etiology of preeclampsia, a hypothesisdriven approach should carefully assess various components of oxidative stress relevant genes in relation to the risk of preeclampsia. Objective: We therefore performed a systematic review and meta-analysis of clinical studies to quantify the magnitude of the association between the polymorphisms of oxidative stress related genes and the risk of preeclampsia and to explore the basis for the heterogeneity in the previously reported observations. Methods: The electronic PubMed and MEDLINE databases were searched up to July 2007 for studies on candidate genes in preeclampsia published in all language. The pre-selected candidate genes include epoxide hydrolase (EPHX), nitric oxide synthase (eNOS), apolipoprotein E (apoE), glutathione S-transferase (GST), lipoprotein lipase (LPL), hepatic lipase (LIPC), superoxide dismutase (SOD), hypoxia inducible factor 1 (HIF1). Preliminary search was based on the medical subject headings terms: (preeclampsia , preeclampsia, eclampsia, toxemia or toxaemia) and polymorphism, (preeclampsia , preeclampsia, eclampsia, toxemia or toxaemia ) and genetics, (preeclampsia , pre-eclampsia, eclampsia, toxemia or toxaemia and gene. An additional search was conducted using the medical term (preeclampsia , pre-eclampsia, eclampsia, toxemia or toxaemia) crossed with each of candidate genes. We also manually screened the references of studies and review articles to avoid a possible loss of any relevant article. A total of 2084 abstracts have been found. Two reviewers independently screened all titles and abstracts for relevance- whether the study measuring the association between these genetic markers and preeclampsia or severe preeclampsia. 69 abstracts were considered as relevant and full-length articles were obtained and reviewed. Studies by the same authors were checked for the possible overlapping of patients. After the exclusion of duplicate reports and review articles, letters and case reports without meaningful data, 34 studies were remained for the present systematic review. Where data available, we calculated the unadjusted odds ratios (OR) with 95% confidence intervals (CI) for each study based on reported crude numbers of events. Compliance to the Hardy-Weinberg equilibrium in the control samples from the included studies was also evaluated. Pooled ORs and their 95% confidence intervals were calculated using the DerSimonian and Laird random effects model. The DerSimonian and Laird Q test was used to evaluate the heterogeneity between studies and I2 were used to describe the percentage of variability in variability in effect estimates due to heterogeneity rather than sampling error. A visual inspection of the funnel plot and the Egger regression asymmetry test were used to assess the potential publication bias. In the presence of significant heterogeneity, several pre-defined stratified analyses by ethnicity, disease severity, and use of blinding of genotyping staffs to case-control status were conducted to investigate the source of heterogeneity. All analyses were conducted using STATA software (version 9.2) meta-analysis procedures. Results Methodology quality assessment of included studies 1. Hardy-Weinberg equilibrium A significant number of studies have not tested the HWE. 2. Blinding of genotype test staff Only a few studies have demonstrated the genotype test was conducted by blinded staff. 3. Definition of phenotype Various definitions of preeclampsia have been used in the included studies although they all used clear and standard definitions. 4. Study design and selection of control All studies used a case-control study design. The selection of controls varied across studies. Some use healthy pregnant women, some selected healthy non pregnant women. Some used women that were randomly selected from the population. 5. Adjustment of confounders Most of studies only conducted the simple chi-square test for investigating the associations between genetic polymorphism and the risk of preeclampsia. Only a small number of studies have assess the role of these oxidative stress polymorphisms on the risk of preeclampsia by adjusting the potential confounding such as high BMI, smoking, etc and as well as investigating the genetic polymorphisms and other maternal predisposing factors and environmental factors. eNOS polymorphism and the risk of preeclampsia 1.1 Glu298Asp polymorphism and preeclampsia. A total of 13 studies have investigated the Glu298Asp polymorphism and the risk of preeclampsia. Based on the evidence to date, we were unable to find the association between Glu298Asp polymorphism and the risk of preeclampsia using various genetic models (additive, recessive and dominant). Significant heterogeneity was found between studies and it exist even after the stratification by the ethinic group and disease severity. 1.2 Intron 4 A/B polymorphism and the risk of preeclampsia Five studies investgated the intron 4 A/B polymorphism and the risk of preeclamsia. The summary OR estimate for individuals homozygous for rare allele (A) compared with homozygous frequent allele (B) was 4.40 (1.60-12.07). The summary OR estimate for individuals homozygous for rare allele (A) compared with carries of B alleles (AB+BB) was 4.03 (1.48-10.99). 1.3 –786T/C polymorphism and the risk of preeclampsia Four studies examined the association between –786T/C polymorphism and the development of preeclampsia. The summary OR estimate for individuals homozygous for the C allele compared with homozygous frequent allele (T) was 2.01 (1.32-3.05). The summary OR estimate for individuals homozygous for C allele compared with carries of T alleles (recessive model) was 1.79 (1.22-2.61). The summary OR estimate for individuals homozygous for C allele plus heterozygous TC individulas compared with homozygous of T allele (dominant model) was 1.31(1.06-1.61). EPHX polymorphism and the risk of preeclampsia Four studies evaluated the epoxide hydrolase gene polymorphism and preeclampsia, including two variants -113 Tyr- His in exon 3 and 139 His-Arg in exon 4. For the Tyr113His polymorphism, the only significant finding was the homozygous Tyr113 versus His113 (OR 1.43, 95%CI 1.06-1.94). With respect to the His139Arg polymorphism, the genotype contrasts of Arg139Arg139 versus His139His139 (OR 2.60, 95%CI 1.11-6.08) and recessive model of Arg139Arg139 versus His139Arg139 plus His139His139 (OR 2.37, 95%CI 1.02-5.49) were found to be significant. Polymorphisms in the glutathione S-transferase (GST) genes and the risk of preeclamsia No significant association was found between the polymorphisms in the glutathione Stransferase genes including GSTP1-Ile105Val, GSTT1-deletion, and GSTM1-deletion and the risk of preeclampsia. apoE polymorphism in preeclampsia A total of seven studies have examined the association between these apoE genetic polymorphisms and the risk of preeclampsia. Only one study found that apoE genotype distribution was associated with the risk of preeclampsia. There was no significant association between apo E genotype using various genetic models. Other SNPs and the risk of preeclampsia. We were unable to find the other oxidative stress relevant genes polymorphisms and the risk of preeclampsia incuding lipoprotein lipase (LPL), hepatic lipase (LIPC), superoxide dismutase (SOD), and hypoxia inducible factor 1 (HIF1). However, a very limited number of studies have investigated those polymorphisms and generally involved very small sample size. Haplotype analysis Among 34 studies, seven studies used haplotype analysis and found that certain haplotype (a panel of mutiple polymorphisms) are associated with the increased risk of preeclampsia. Main finding 1) So far, However, the findings from previous studies are inconsistent. A single polymorphism is unlikely to explain the variety in the systematic changes in the pathogenesis of preeclampsia. 2) The methodolgy of the previous studies is relatively poor. Only a few studies have tested the Hardy-Weinberg equilibrium, a few studies have calcuated the adjusted odds ratios for the association between genetic polymorphism and the risk of preeclampsia. Very few studies used to blinded staffs to do genotype testing. 3) To date, most of studies only examined the relationship between maternal genes and the risk of preeclampsia. Few studies have simutaneously investigated the contribution of maternal and fetal (paternal) genetic polymorphisms on the pathogenesis of preeclamsia. The fact that preeclampsia is a disease of pregnancy suggests that the fetus and/or placenta interacts with maternal factors to contribute to the disease. Interactions between maternal and fetal (or paternal) genes or between these genes and environmental factors may influence the risk of disease. Further investigation of polymorphisms affecting biotransformation enzymes is necessary before ruling out them as promising candidates in the contribution to the development of preeclamsia. 4) Based on our literature review, a panel of mutiple polymorphisms in the proposed candidates genes seem to be are of more value in the search for the associations with the disease. It may be preferable to use haloptype analysis to investigate the possible association between candidate genes and the risk of preeclampsia. Questions: 1. Are there any other oxidative stress relevant genetic polymorphism that you would recommend to be included in the present systematic review other than that are mentioned above? 2. For three alleles, how would you build genetic models for the comparison? 3. What is your proposition on the genome wide scan approach and candidate genes approach? Should we abandon the candidate gene approach and go for fishing (genome wide scan)? Should be basic scientists closely work with methodologists (ie. Epidemiologist) to improve the quality of study design and analysis before ruling out any promising candidate genes?