Running head: APA TYPING TEMPLATE
advertisement

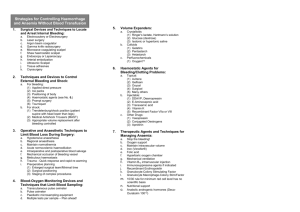
Running head: PROFESSIONAL COMMUNICATION Professional Communication: Cultural Sensitivity Claudette D. Johnson Grand Canyon University: NUR 502 January 11, 2012 1 PROFESSIONAL COMMUNICATION Personal Communication Cultural Sensitivity: Care of Jehovah Witnesses Increase diversity in nursing has created a challenge for caregivers. The concept of diversity advocates understanding the uniqueness of each individual taking into consideration personal differences in language, traditions, moral and religion, and spiritual choices (Hood, 2006). The constitution of the World Health Organization’s states that the highest attainable standard of health is one of the fundamental rights of every human being without regard to race, religion, political belief, economic or social condition (Barker, 2009, p.494). Understanding one’s culture will enable caregivers to holistically care for patients of different cultures contributing to positive outcomes (Hood, 2010). Jehovah Witnesses have cultural beliefs that have nursing implications unique to their culture. Cultural awareness and sensitivity will enable nurses to support choices differing from their own to improve patient outcomes. This paper will analyze the article, The Pregnant Jehovah’s Witness: How Nurse Executives Can Assist Staff in Providing Culturally Competent Care with focus on cultural differences and nursing intervention aimed to address cultural and practice issues with the Jehovah Witnesses population (Trovarelli & Valenti, 2005). Healthcare professionals must possess the cultural general knowledge and skills that will support them in a rapidly changing healthcare system. Summary of Article Overview The article from the Journal of Nursing Administration’s (JONA) Healthcare Law, Ethics, and Regulation; The Pregnant Jehovah’s Witness: How Nurse Executives Can Assist Staff in Providing Culturally Competent Care discusses the role of nurse executives in facilitating cultural awareness in the care of Jehovah Witnesses (Trovarelli & Valenti, 2005). 2 PROFESSIONAL COMMUNICATION 3 The Federal Patient Self-Determination Act, passed in 1991 requires health care providers to uphold patient’s right to make decisions even if the decision has life threatening impact (Barker, 2009). Healthcare providers are required to respect patient’s informed decisions even if it conflicts with science and opinions. Background Jehovah's Witnesses started in Pennsylvania in 1870 led by Charles Taze Russell. The Watchtower Bible and Tract Society was founded in 1886 and due to a split in the organization, it was renamed the Jehovah’s Witnesses (Witness for Jehovah, 2011). Jehovah's Witnesses believe that the Bible prohibits the eating of blood. They believe that injecting blood into their veins is the same thing as eating it. They believe they are showing respect for blood by refusing blood transfusions, thus, showing respect for human life and God by refusing blood transfusions (Jehovah’s Witnesses Official Media Website, 2012). Article summary The article discusses the fate of a 28 year old Jehovah’s Witness pregnant woman in sickle cell crisis on her twenty-ninth (29th) week of pregnancy and the ethical dilemma during her care. The woman’s refusal to receive blood and undergo a C-section resulted in the woman’s death 11 days after delivery and the demise of her baby girl shortly after birth (Trovarelli & Valenti, 2005). It reexamines the care provider (specifically nurse executives) alternatives and options in addressing patient care. Discussing Bloodless Program, use of advance directives and durable Power of attorney papers to outline wishes, ensuring that enough albumin or other blood alternatives are available during surger, advocate for patient by upholding their decision, policy advocacy in one’s institutions, educator and resource of clinicians, patient and doctors to diffuse PROFESSIONAL COMMUNICATION 4 difficult situations and more importantly create a trusting environment free from condemnation for Jehovah witness patients and an environment for staff to be heard (Trovarelli & Valenti, 2005). Cultural and ethical differences Facing decisions that may result in death is never easy. It is even harder when the life of the unborn is involved, creating ethical and religious dilemma for all parties involved. The question of who is advocating for the unborn complicates this situation. In the eyes of the patient and families it is seen as devotion their faith as influenced by religious and cultural factors. On the other hand, caregivers may see the patient’s choice in the context of science; saving lives, using evidenced- based intervention with the best options for improving one’s health, and conflicted by the oath to do no harm (nonmalificience) and the decisions to honor patient’s autonomy and religious belief may differ from that of the patient. These views and the nurse’s drive to improve patient outcomes can over shadow the patient/family’s wishes. Application to Practice Self- assessment of one’s feelings about religions will promote acceptance of patient’s choices. One does not need to approve to accept differing choices. Respecting once decision even if it may not agree with our belief is important in differing cultures. Institute of medicine (IOM) report on safety attributed the growing number of errors resulting from miscommunication (IOM, 2000). Unclear orders, lack of critical information and misinterpretation of information all can lead to medical errors (O’Daniel & Rosenstein, n.d.). Communication errors are identified by the Joint Commission as the primary root cause of sentinel events across all categories. Improving the effectiveness of communication among healthcare providers is listed as one of the Joint Commission National Patient Safety Goals since PROFESSIONAL COMMUNICATION 5 2005 (O’ Daniel & Rosenstein, n.d.). Clear communication is the key in providing a caring environment for Jehovah Witnesses. Communicating information with accuracy, clarity during admission and discharge of patient can prevent readmission (Institute of Healthcare Improvement (IHI, 2011). Readmission is not only costly but it also decreases patient satisfaction and increases length of stay (IHI, 2011). Communication of risks with use of accurate, concise information and language understood by patient and family is important. In the book, What’s Practical about Technical Writing, the authors referred to professional communication as not simply workplace activity but as human conduct in those activities that maintain the lives of our patients and our community (Bertie, Fearing & Keats Sparrow, 1989). Professional communicators use strategies, theories, and technologies to effectively communicate in the business side of nursing which is vital not only for safety but for our profession. According to American Psychological Association (2010), one can achieve accurate and concise communication by way of orderly presentation of details. Respectful and nonjudgmental acknowledgement of their choices should be the foundation of care. The Joint Commission holds hospitals accountable for addressing and maintaining patient rights. Furthermore, the American Nurses Association in its Code of Ethics for Nurses where it states, provision 1, demands that the nurse in professional relationship should practice with compassion and respect for the dignity, worth and uniqueness of every individual (ANA, 2012). Cultural sensitivity and awareness by understanding the Jehovah Witness’ religion enables caregiver to put parental decision in perspective. Knowing before-hand the Jehovah Witnesses’ preferences can prepare the institutions to minimize risks. Preparation can be planned ahead to ensure enough blood alternatives are available. The use of specialists ensure safety of patient and baby (the article suggested a PROFESSIONAL COMMUNICATION 6 hematologist and perinatologist presence during crisis). Jehovah Witnesses has the option of auto-infusion of their own blood, thus, some may store their own blood for planned procedures, referred to as salvaging (JW-Media 2012). Proactive approach can help the cultural and ethical issues faced during this trying time. Plan to use resources such as the Ethics committee, Ethicist, or Chaplain to support the family and patient should be foremost. Reaching out to the Jehovah’s Witness elders and community to support the psychological and spiritual needs of the family is highly encouraged by the church and elders (Trovarelli & Valenti, 2005). The availability of a 24/7 hotline is an option to support the patient, family and staff. Elders have access to libraries national and international which can be faxed to hospitals (Trovarelli & Valenti, 2005). The ability to communicate in the language of the client is critical for clarity and accuracy when educating the patient (Barker, 2009, p. 496). Educating staff not only on honoring patient choices care options as outlined by the bloodless program which includes respectful acceptance of patient choices, use of blood replacement products and familiarizing staff with the consent forms that they usually present during admission. This ensures that proper, accurate and important information is relayed to ensure safe patient care and positive outcomes (Hood, 2010). Clear handoff to next caregiver with sensitivity to the information and choices in their care must occur for consistency in nursing practice. Since communication in our present society is a rapidly changing area, advances in technology seems too often outpace the availability of expert practitioners (Bertie, Fearing & Keats-Sparrow, 1989). This creates a demand for skilled communicators which continues to exceed the supply of trained professionals, not to mention that nursing serves a diverse population which is a constant challenge to our profession. To PROFESSIONAL COMMUNICATION 7 some, communication does not come easy. It is one to be practiced and learned. In as much as most institution focus on changing processes for safety, they should also invest on people to be able to communicate information accurately for safety. Conclusion The increasing diversity of our population makes the art of caring a challenge. Cultural awareness, knowledge and competence can help bridge the gap. Awareness of cultural differences in health care is the realization that communication walls are breaking down. With nursing practice dedicated to caring for the patient’s physical, emotional, psychological and social needs, awareness of cultural will help breakdown communication walls. As nurses we are the catalyst in this process. This opens up doors for nurses and patient to understand one another to achieve a common goal: optimal outcome for the patient and family. PROFESSIONAL COMMUNICATION 8 References American Nurses Association. (2001). Code of ethics for nurses with interpretive statements. Nursing World. Retrieved from http://www.nursingworld.org/MainMenuCategories/EthicsStandards/Tools-YouNeed/Code-of-Ethics.pdf American Psychological Association. (2010). Publication manual of the American Psychological Association (6th ed.). Washington, DC: Author. Barker, A. M. (2009). Advanced practice nursing – Essential knowledge for the profession. Boston: Jones and Bartlett Publishers. 494 - 496. Bertie, E., Fearing, E. and Keats Sparrow, W. (1989) What's Practical about Technical Writing?” Technical Writing: Theory and Practice. New York: Modern Language Association. Caminha-Bacote, J. (1991). The Process of Cultural Competence in the Delivery of Healthcare Services, Retrieved from http://angel04.gcu.edu/section/default.asp?id=1065151 Hood, L. (2010). Conceptual Bases of Professional Nursing (7th ed.). Philadelphia, PA: Lippincott Williams & Wilkins. Illinois Department of Public Health (IDPH). (2010). Statement of Illinois law on Advance Directives and DNR orders. Retrieved from http://www.idph.state.il.us/public/books/advin.htm Institute of Healthcare Improvement (IHI). (2011). Reducing Avoidable Readmissions By Improving Transition Of Care. Retrieved from http://www.ihi.org/offerings/Training/ReduceReadmissions/July2011ReducingReadmissi PROFESSIONAL COMMUNICATION 9 ons/Pages/default.aspx Institute of Medicine. (2000). To Err is Human: Building a Safer Healthcare System. Retrieved from http://iom.edu/~/media/Files/Report%20Files/1999/To-Err-isHuman/To%20Err%20is%20Human%201999%20%20report%20brief.pdf Jehovah’s Witnesses Official Media Website. (2012). Our View of Medical Care: Blood Transfusions. Retrieved from http://www.jw-media.org/aboutjw/article01.htm McFarland, M. M. and Eipperle, M. K. (2008). Culture care theory: A proposed practice theory guide for nurse practitioners in primary care settings. Contemporary Nurse. 28(1-5), 4863. Retrieved from http://angel04.gcu.edu/section/default.asp?id=1065151 Northwest Community Hospital (NCH). (2011). Jehovah Witness Bloodless Program Policy. NCH Policy and Procedure: Policy 105. O’Daniel, M. and Rosenstein, A. (n.d.). Professional Communication and Team Collaboration. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Retrieved from http://www.ahrq.gov/qual/nurseshdbk/docs/O%27DanielM_TWC.pd Trovarelli, T. and Valenti, J. (2005, October-December). The Pregnant Jehovah’s Witness: How Nurse Executives Can Assist Staff in Providing Culturally Competent Care. Journal of Nursing Administration’s Healthcare Law, Ethics, and Regulation. 7(4), 105-109. Retrieved from http://library.gcu.edu:2048/login?url=http://gateway.ovid.com/ovidweb.cgi?T=JS&NEW S=N&PAGE=fulltext&AN=00128488-200510000-00004&LSLINK=80&D=ovft Witness for Jehovah (2011). Jehovah's Witness Beliefs and History. Retrieved from PROFESSIONAL COMMUNICATION www.4jehoouah.org 10