Residency Training Benchmark – Hepatic and Renal Disease
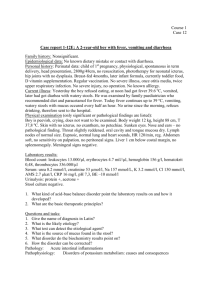
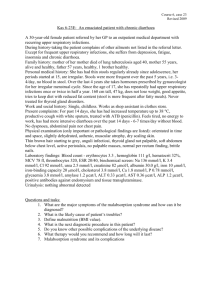
advertisement

ACVECC Small Animal Residency Training Benchmark November 2010 A 5-year old female Rottweiler weighing 42kg was referred to your hospital for vomiting of two days’ duration. Her past medical history is benign. Her physical examination reveals a dog with a good body condition and hair coat. She is approximately 5% dehydrated and splints somewhat on dorsal abdominal palpation. There are no other abnormalities. Blood biochemistry results: Glucose: 96 mg/dL (60 – 115) 5.33 mmol/l (4-6) Sodium: 132 mmol/L (139 – 150) Potassium: 4.9 mmol/L (3.4 – 4.9) Chloride: 102 mmol/L (106 – 127) Phosphorous: 15.1 mg/dL (2.9 – 5.3) 5.01 mmol/l (0.9-1.7) Total Protein: 4.9 g/dL (5.5 – 7.5) 49 g/l (55-75) BUN > 200 mg/dL (10 – 29) >71.4 mmol/l (3-10) Creat: 13.9 mg/dL (0.6 – 1.6) 1229 umol/l (70-130) ALT: 18 IU/L (10 – 120) ALP: 15 IU/L (0 – 140) Basic Complete Blood Count results: WBC: 11,100 (6000 – 17,000) / uL 11.1 x109 /l (6-17x109) HCT: 54% (37 – 55) PLT: 314,000 (200,000 – 500,000) / uL 314 x109 /l (200-500x109) Urinalysis: SpGr: 1.013 Protein: 500 mg/dL pH: 6.0 Gluc: neg Ketones: neg Bili: neg Blood: 2+ Sediment: See image below Abdominal radiographs show no abnormalities. 1. What is the large structure seen in the urine sediment? 2. Give this dog’s extended problem list 3. This dog has evidence of renal failure. a.) Is this more likely acute or chronic? b.) Explain your rationale for this diagnosis using at least one piece of information from the history, physical exam, and each diagnostic procedure listed above. 4. Please list at least 5 broad categories of possible predisposing causes for this dog’s renal failure. Please list at least three examples under each category. 5. What diagnostic tests could be performed to help determine the etiology of acute renal failure in the dog? Prioritize these tests into first tier (would recommend on all patients with renal failure), second tier (will recommend on many cases based on results of first tier, geographic location, or other indications), and third tier (will only recommend if indicated based on results of other tests) a. First tier b. Second tier c. Third tier 6. Design a specific preliminary treatment plan (fluid therapy and other treatments) for this patient. What are some concerns in this patient regarding fluid therapy? Design a preliminary monitoring plan while pending diagnostic test results. Explain your rationale for each. Fluid therapy: Concerns for fluid therapy: Medications: Monitoring: 7. You place a urinary catheter to measure her urine output. a. What conditions must be met prior to making a diagnosis of pathologic oliguria or anuria in this patient? b. What is normal urine output? c. What is the definition of oliguria? d. What is the definition of anuria? e. What is the definition of polyuria? 8. Below is a list of medications that can be used in acute renal failure to potentially increase urine output. List the different mechanisms of action for each medication and the possible adverse effects that it may cause. a. Diltiazem i. MOA ii. Adverse effects b. Lasix (Furosemide) i. MOA ii. Adverse effects c. Mannitol i. MOA ii. Adverse effects d. Dopamine (<5mcg/kg/min) i. MOA ii. Adverse effects e. Fenoldopam i. MOA ii. Adverse effects 9. Please describe the difference between peritoneal and intermittent hemodialysis in the following areas. (10 points) a. Dialysate preparation and composition b. Anticoagulation c. Ultrafiltration d. Blood pump mechanism e. Exchange surface 10. List four potential complications of peritoneal dialysis: 11. List four potential complications of hemodialysis: 12. Please answer the following questions regarding Continuous Renal Replacement Therapy a. What is the definition and purpose of CRRT? b. List and describe the four different possible modes of operation in CRRT. c. What are some potential advantages of CRRT over intermittent hemodialysis and peritoneal dialysis? What are some potential disadvantages? Please answer the following questions regarding Ethylene Glycol toxicity 13. What is the minimum lethal dose of ethylene glycol that has been reported in dogs and cat? 14. List in order the 5 major metabolites of ethylene glycol that develop after ingestion 15. Which metabolite is the most nephrotoxic? 16. List diagnostic tests or measurements that can be used to support a diagnosis of ethylene glycol toxicity? 17. List the mechanisms by which isosthenuria occurs in ethylene glycol toxicity. A 6 year old 9 kg MC DSH presents for a 3 day history of progressive lethargy and intermittent vomiting. The cat stopped eating approximately 4 days ago, shortly after the owner left town (the cat is presented by the pet sitter). On physical examination, the cat is mentally depressed, body condition score 8/9, temperature 99.2°F (37.3°C), pulse rate 168/min, rate 28/min, mucous membranes pale pink and icteric, capillary refill time 1.5 sec, with moderate and synchronous pulses. The abdomen is difficult to palpate due to the obesity, but there is probable cranial organomegaly. Complete Blood Count RBC 7.01 x 106/uL (5.0-10.0) HBG 10.4 g/dL (9.8-15.4) HCT 31.5% (30-45%) MCV 44.9 fl (40-55) MCH 14.9 pg (13-17) MCHC 33.2 g/dL (30-36) Platelets est: adequate, some clumps WBC 18.7 x 103/uL (5.5-19.5) Segs 14.3 x 103/uL (3.5-12.5) 3 Bands 0.36 x 10 /uL (0-0.3) Lymphs 3.26 x 103/uL (1.5-7.0) 3 Monos 0.18 x 10 /uL (0-0.9) Eos 0.00 x 103/uL (0-0.2) 3 Baso 0.00 x 10 /uL (0-0) Chemistry Screen Glucose 125 mg/dL BUN 4 mg/dL Creatinine 0.8 mg/dL Phosphorus 4.2 mg/dL Calcium 10.1 mg/dL Sodium 150 mmol/L Potassium 4.6 mmol/L Chloride 114 mmol/L Total Protein 6.1 g/dL Albumin 2.8 g/dL ALP 969 U/L ALT 199 U/L GGT 4 U/L T. Bili 7.5 mg/dL Cholesterol 201 mg/dL (65-112) (20-34) (0.9-1.8) (3.6-6.0) (9.8-11.7) (149-156) (3.6-4.9) (113-125) (6.0-7.7) (3.0-4.3) (14-50) (31-104) (0-4) (<0.2) (128-147) 6.94 mmol/l 1.43 mmol/l 70 umol/l 1.36 mmol/l 2.53 mmol/l (4-6) (3-10) (80-130) (0.9-1.8) (2.3-2.8) 61 g/l (60-77) 28 g/l (30-43) 128.3 umol/l (0-3) 5.21 mmol/l (2.3-4.3) Urinalysis (table top) Color: yellow, hazy USG 1.011 pH 7.5 protein neg glucose neg ketone neg bilirubin large blood negative Sediment: 0 RBC, 0 WBC, few bilirubin crystals Few squamous epithelial cells Coagulation Screen PT 8.5 sec aPTT 12.8 sec (8.2-11.4) (11.6-18.4) 18. What is the most likely diagnosis? 19. Describe the normal production, catabolism and excretion of bilirubin. 20. Bile salts are reabsorbed in which of the following locations? a. b. c. d. e. 21. Duodenum Jejunum Ileum Cecum Colon Where and how is albumin produced and how is its production regulated? 22. Calculate RER for this patient. 23. Describe in detail the procedure to properly place an esophagostomy tube. 24. Please list three (3) advantages and one (1) disadvantage of esophagostomy tube placement: 25. Please list at least four potential complications of esophagostomy tube use or placement: 26. Justify the use each of these medications in the management of a patient with hepatic lipidosis: a. L-carnitine b. Taurine c. Ursodeoxycholic acid d. Silymarin e. s-Adenosylmethionine f. Thiamine and Cyanocobalamine g. Vitamin K1 h. Vitamin E 27. Which ONE of the following decreases the activity of hormone-sensitive lipase? a. b. c. d. Growth hormone Insulin Thyroxin Epinephrine 28. Which ONE of the following is NOT a requirement for the formation of very low-density lipoproteins (VLDL) particle dispersal? a. b. c. d. Transport of the particle out of the hepatocyte into the perisinusoidal space Intact lipid transport through subcellular compartments Formation of a secretory particle Particle combination with pro-adipose 29. List the mechanism of action for each of the following anti-emetics: a. Maropitant b. Phenothiazines c. Metoclopramide d. Ondansetron and Dolasetron 30. Ammonia is one of the key participants in hepatic encephalopathy. In cats hyperammonemia can develop in the absence of liver disease or porto-systemic shunt due to limited reserves in which essential amino acid? a. Tryptophan b. Glutamine c. Arginine d. Leucine 31. Describe the effects of ammonia on the brain. 32. Discuss the benefits of using the following therapeutics in patients with hepatic encephalopathy a. Mannitol b. Lactulose c. Rifaximin d. Flumazenil 33. Discuss how the following 4 factors can contribute to the severity of hepatic encephalopathy a. Inflammation b. Gastrointestinal hemorrhage c. Hypokalemia d. Metabolic alkalosis