Chlamydia and Gonorrhea - Berkshire Health Systems
advertisement
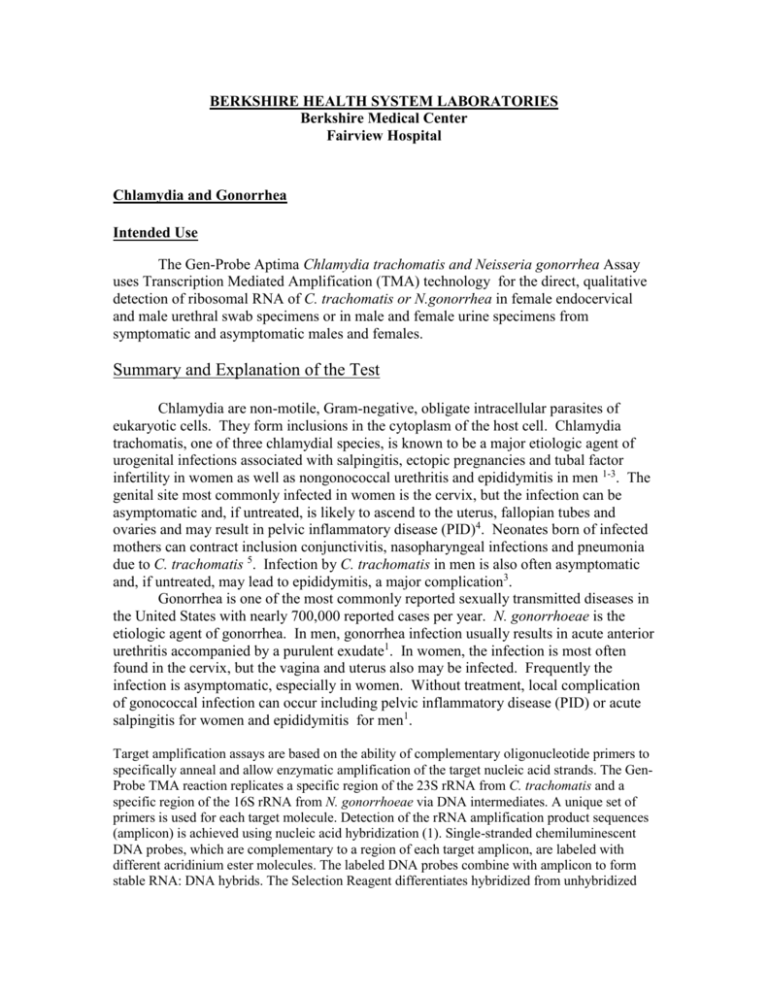
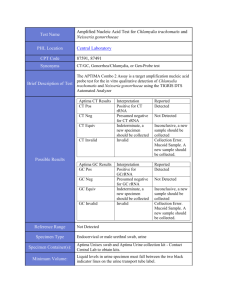
BERKSHIRE HEALTH SYSTEM LABORATORIES Berkshire Medical Center Fairview Hospital Chlamydia and Gonorrhea Intended Use The Gen-Probe Aptima Chlamydia trachomatis and Neisseria gonorrhea Assay uses Transcription Mediated Amplification (TMA) technology for the direct, qualitative detection of ribosomal RNA of C. trachomatis or N.gonorrhea in female endocervical and male urethral swab specimens or in male and female urine specimens from symptomatic and asymptomatic males and females. Summary and Explanation of the Test Chlamydia are non-motile, Gram-negative, obligate intracellular parasites of eukaryotic cells. They form inclusions in the cytoplasm of the host cell. Chlamydia trachomatis, one of three chlamydial species, is known to be a major etiologic agent of urogenital infections associated with salpingitis, ectopic pregnancies and tubal factor infertility in women as well as nongonococcal urethritis and epididymitis in men 1-3. The genital site most commonly infected in women is the cervix, but the infection can be asymptomatic and, if untreated, is likely to ascend to the uterus, fallopian tubes and ovaries and may result in pelvic inflammatory disease (PID)4. Neonates born of infected mothers can contract inclusion conjunctivitis, nasopharyngeal infections and pneumonia due to C. trachomatis 5. Infection by C. trachomatis in men is also often asymptomatic and, if untreated, may lead to epididymitis, a major complication3. Gonorrhea is one of the most commonly reported sexually transmitted diseases in the United States with nearly 700,000 reported cases per year. N. gonorrhoeae is the etiologic agent of gonorrhea. In men, gonorrhea infection usually results in acute anterior urethritis accompanied by a purulent exudate1. In women, the infection is most often found in the cervix, but the vagina and uterus also may be infected. Frequently the infection is asymptomatic, especially in women. Without treatment, local complication of gonococcal infection can occur including pelvic inflammatory disease (PID) or acute salpingitis for women and epididymitis for men1. Target amplification assays are based on the ability of complementary oligonucleotide primers to specifically anneal and allow enzymatic amplification of the target nucleic acid strands. The GenProbe TMA reaction replicates a specific region of the 23S rRNA from C. trachomatis and a specific region of the 16S rRNA from N. gonorrhoeae via DNA intermediates. A unique set of primers is used for each target molecule. Detection of the rRNA amplification product sequences (amplicon) is achieved using nucleic acid hybridization (1). Single-stranded chemiluminescent DNA probes, which are complementary to a region of each target amplicon, are labeled with different acridinium ester molecules. The labeled DNA probes combine with amplicon to form stable RNA: DNA hybrids. The Selection Reagent differentiates hybridized from unhybridized probe, eliminating the generation of signal from unhybridized probe. During the detection step, light emitted from the labeled RNA: DNA hybrids is measured as photon signals in a luminometer, and are reported as Relative Light Units (RLU). In DKA, differences in the kinetic profiles of the C. trachomatis and N. gonorrhoeae labeled probes allow for the differentiation of signal; kinetic profiles are derived from measurements of photon output during the detection read time. The chemiluminescent detection reaction for C. trachomatis signal has very rapid kinetics and has the "flasher" kinetic type. The chemiluminescent detection reaction for N. gonorrhoeae signal is relatively slower and has the "glower" kinetic type. Assay results are determined by a cut-off based on the total RLU and the kinetic curve type. Specimen Collection and Transport to Test Site Time and temperature conditions for storage must be adhered to during transport. Transport to the BHS lab within 24 hours of collection. For swab specimen collection, use only the Gen-Probe Unisex Swab Specimen Collection Kit for Endocervical and Urethral Swab Specimens. Note: Do not use the Large-tipped Cleaning Swab for Specimen Collection. Endocervical Swab Specimen Collection 1. Remove excess mucus from the exocervix with the large-tipped cleaning swab provided in the LCx STD Swab Specimen Collection System and discard. 2. Insert the small-tipped, specimen swab into the endocervix and rotate the swab for 15 - 30 seconds to ensure adequate sampling. 3. Verify that all Swab Specimen Transport Buffer is at the bottom of the tube. If necessary, tap or shake the solution down to the bottom of the tube. Unscrew the cap of the transport tube, insert the swab into the transport tube and break the swab at the score line. Replace the cap securely making sure that the swab fits into the cap and then screw on the cap until it clicks into place. 4. Label the transport tube with the patient's ID number and date of collection. Male Urethral Swab Specimen Collection 1. 2. Insert the small-tipped, specimen swab 2 to 4 cm into the urethra and rotate the swab for 3 - 5 seconds to ensure adequate sampling. Verify that all Swab Specimen Transport Buffer is at the bottom of the tube. If necessary, tap or shake the solution down to the bottom of the tube. Unscrew the cap of the transport tube, insert the swab into the transport tube and break the swab at the score line. Replace the cap securely making sure that the swab fits into the cap and then screw on the cap until it clicks into place. 3. Label the transport tube with the patient's ID number and date of collection. Swab Specimen Transport 1. Swab specimens can be shipped to the laboratory or testing site at ambient temperature. Swab specimens must arrive at the test site within 24 hours of shipment. Urine Specimen Collection and Transport Urine specimens can be transported to the laboratory at 2to 30C in either the primary collection device (urine cup) or in the urine specimen transport tube. Urine specimens must be transferred into the GENPROBE specimen transport tube within 24 hours of collection and before being assayed. After transfer, urine specimens can be stored at 2to 30C for up to 30 days after collection. 3. Urine specimens a. The patient should not have urinated for at least one hour prior to specimen collection. b. Direct patient to provide a first-catch urine (approximately 20 to 30 mL of the initial urine stream) into a urine collection cup free of any preservatives. Collection of larger volumes of urine may result in specimen dilution that may reduce test sensitivity. Female patients should not cleanse the labial area prior to providing the specimen. Turnaround Time: 3-5 days Approved by: Medical Director: C. Abbott, MD Approved by: Technical Director: R. Intres, PhD Prepared by: R. Intres, PhD Bhshlp/LabProc/OP/MB/GC-Chlam Adopted: 5-25-06 Revised: Reviewed: 1-27-12 RI