On line supplements - Springer Static Content Server
advertisement

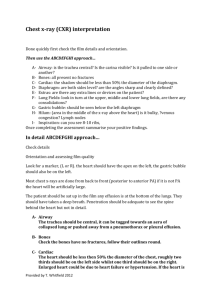
Electronic Supplementary Material Lung Ultrasound in Critically Ill Patients – Comparison with Bedside Chest Radiography Nektaria Xirouchaki*, Eleftherios Magkanas+, Katerina Vaporidi*, Eumorfia Kondili*, Maria Plataki*, Alexandros Patrianakos++, Evaggelia Akoumianaki*, and Dimitrios Georgopoulos* *Department of Intensive Care Medicine, +Department of Radiology and ++ Department o Cardiology, University Hospital, Heraklion, University of Crete, Greece Address for correspondence: D. Georgopoulos, Professor of Medicine, Director, Department of Intensive Care Medicine, University Hospital of Heraklion, University of Crete, Heraklion, Crete, Greece Fax: +30-2810-392636 E-mail: georgop@med.uoc.gr METHODS Chest radiography Anterior chest x-ray was performed with the patients in supine position using portable X-Ray equipment (Siemens polymobile, Erlangen, Germany). The evaluation of chest x-ray was performed by an expert radiologist, unaware of the ultrasound and thoracic computed (CT) findings. Consolidation, interstitial syndrome (including alveolar edema), pneumothorax and pleural effusion were defined using the terminology of the Nomenclature Committee of the Fleishner Society [1]. For regions location the anatomic landmarks used were lung apex, mid-axillary line, hilar line, external limit of the rib cage, mediastinal border and diaphragm, as previously described [2]. The “silhouette sign” was also used to facilitate regions locations. Multiple Detector Computed Tomography (MDCT) MDCT was performed with a Siemens Somatom Sensation (16 slices, Erlangen, Germany). Scans were obtained in the supine position from the apex of the thorax to the lung bases. Iodine contrast material was administered to differentiate pleural effusion from alveolar consolidation and atelectasis. The decision to use iodine contrast material was made by the patient’s attending physician. Assessment included thin MDCT high Resolution Computed Tomography (MDCT-HRCT) and spiral MDCT scans. Thin MDCT-HRCT scans consisted of 1mm section thickness at 10 mm intervals, were used to reveal diffuse lung parenchymal involvement as ground glass opacities, septal or non-septal lines and fibrotic changes (architectural distortion). MDCT consisted of contiguous axial 7mm thickness slices reconstructed from the volumetric data of the MDCT software. MDCT scans were evaluated for mediastinal and pleural pathology (pleural effusion, pneumothorax) and lung lesions 1 (consolidation, atelectasis, parenchymal bands), as described by the Nomenclature Committee of the Fleischner Society [1]. To facilitate comparison between methods interstitial syndrome was defined as the presence of ground glass opacities, septal or non-septal lines or fibrotic changes. Similarly consolidation was defined as the presence of atelectasis, consolidation or parenchymal bands. Lung regions were located using the same anatomical landmarks with x-ray. Two individual radiologists, unaware of lung-ultrasound and CXR findings studied the MDCT-HRCT and MDCT images and decisions were reached by consensus. Lung-ultrasound Visualization of the lungs was performed using a microconvex 5-9 MHz transducer appropriate for transthoracic examination, (HITACHI EUB 8500). Lung-ultrasound was performed by a single operator (N.X.) who was unaware of CT and chest radiography information. The operator had more than 4 years of extensive experience in lung-ultrasound. The main preset parameters were custom made by the same operator (N.X.). Filters suppressing lung sliding were by-passed. Access to standardized images (seashore sign, stratosphere sign) was possible. Lungs were divided in 12 regions as previously described [2]. The anterior surface of each lung was defined by clavicle, parasternal, anterior axillary line, and diaphragm and was divided in two areas, upper and lower. The lateral surface was defined by the anterior and posterior axillary lines and divided in an upper and lower area. Finally, the posterior lung surface was defined by the posterior axillary and the paravertebral lines and divided in an upper and lower area. The apex was scanned from supraclavicular space. Patients were studied in the supine position. The lateral position was used for posterior lung surface examination. 2 In lung-ultrasound the normal lung displays the “lung sliding” and A lines. Lung sliding indicates sliding of the visceral pleura against the parietal pleura and A lines are repetitive horizontal artifacts parallel to the pleural line generated by subpleural air [3, 4]. Consolidation was defined as an iso-echoic tissue-like structure which is caused by the loss of lung aeration [5, 6]. Power Doppler was used in order to differentiate tissue like structures (e.g. echoic pleural effusion) from consolidation [7]. (Video 1). The shred sign, specific for consolidation, was not used. [3] Interstitial syndrome was defined as presence of multiple B-lines in a specific lung area. B-lines are well defined hyperechoic comet–tail artifacts, arising from pleural line and spreading up indefinitely, erasing A lines and moving with the lung sliding when lung sliding is present [3]. The B-lines 7+1 mm apart indicate thickening of the interlobular septa (B7-lines) and 3+1mm apart indicate ground glass areas (B3-lines), as previously described [4, 8, 9]. Pneumothorax was diagnosed when the A-line sign (only A-lines visible), was associated with the stratosphere sign (complete abolition of lung sliding). Local lung sliding or B-lines exclude the diagnosis of pneumothorax [10]. The lung point, (defined as inspiratory synchronized changes from lung patterns to pneumothorax patterns), was additionally used for diagnosis of pneumothorax [11]. (Fig. S1). Pleural effusion was determined as a hypo echoic or echoic structure, containing iso-echoic particles or septations in inflammatory pleural diseases. In addition to power Doppler the quad and sinusoid signs which indicate pleural effusion regardless of its echogenicity, were also used. [9, 12]. Power Doppler may not be mandatory for proper lung ultrasound examination, providing that shred sign [3], quad sign and sinusoid sign [9, 12] are used. Data analysis 3 Each lung region was evaluated and characterized as positive or negative for each abnormality. A hemithorax was characterized as positive for an abnormality if it presented at least one positive region, and negative if all regions were negative. The results of CXR and lung-ultrasound were compared with the corresponding CT scan results. Sensitivity, specificity, positive and negative predictive values and diagnostic accuracy were calculated using standard formulas. RESULTS Regional analysis A total of 504 lung regions (12 in each patient) were evaluated by the three imaging techniques. Sensitivity, specificity, positive and negative predictive values, and diagnostic accuracy of lung-ultrasound and chest x-ray for each region and for each pathologic entity are shown in table S1. It is of interest to note that in 23 cases CT identified in the same region both consolidation and interstitial syndrome, while lung-ultrasound recognized only one pathology (either consolidation or interstitial syndrome). Interstitial syndrome Interstitial syndrome was identified in 228 regions with CT scan, in 67 regions with x-ray and in 233 regions with lung-ultrasound. Lung-ultrasound correctly identified this entity in 204 regions, and x-ray in 49 regions. (Fig. S2, Fig. S3). Lungultrasound had 29 false positive regions and 22 of them (76%) were adjunct to regions 4 positive for this abnormality both in lung-ultrasound and CT. It follows that is discrepancy between lung-ultrasound and CT findings was mainly due to overlap. The difference in time between the two imaging techniques (up to 4 hours) might be an additional cause of some false positive cases, (Fig. S4). Lung-ultrasound had 24 false negative regions. The presence of pneumothorax in some cases (2 patients) interfered with the ability of lung-ultrasound to evaluate the affected lung regions. Consolidation Consolidation was identified in 120 regions with CT scan, in 47 regions with x-ray and in 149 regions with lung-ultrasound. Lung-ultrasound correctly identified this entity in 101 regions, and x-ray in 27 regions. (Fig. S5). Lung-ultrasound had 48 false positive regions (Fig. S6) and 38 of them (79%) were adjunct to regions positive for this abnormality both in lung-ultrasound and CT. (Fig. S7, Fig S8).These results indicate that overlapping between acoustic windows of adjuncts regions is the main reason of false positive results with lung-ultrasound. Lung-ultrasound was negative for consolidation while CT was positive in 19 regions (false negative). The reasons of this discrepancy was due to 1) the presence of pneumothorax, (Fig S9) 2) the peripheral location of consolidation (consolidation which did not reach lung surface), and 3) difficulties to delineate the consolidation borders. Pleural effusion Pleural effusion was identified in 116 regions with CT scan, in 64 regions with x-ray and in 150 regions with lung-ultrasound. Lung-ultrasound correctly identified this entity in 106 regions, and x-ray in 46 regions. Lung-ultrasound had 10 false negative regions. All of them were located in upper posterior field. We believe that 5 the lateral position of the patient (due to lung-ultrasound protocol we followed) and the scapula were the main reasons of this discrepancy. Lung-ultrasound was positive for pleural effusion where CT was negative in 44 regions, mostly in the lower lateral field, but in 91% of the cases a pleural effusion was identified by both techniques in the lower posterior region. (Fig. S7, Fig. S8). Pneumothorax Pneumothorax was identified in 13 regions with CT, in 2 regions with x-ray and in 13 regions with lung ultrasonography. Lung-ultrasound correctly identified this entity in 8 regions. Chest x-ray did not recognize any regions which was positive for this abnormality with CT (zero true positive). Lung-ultrasound had 5 false negative and 5 false positive regions for pneumothorax. The 5 false positive regions occurred in three patients with subcutaneous emphysema due to chest trauma and in two patients with acute exacerbation of COPD and hyperinflation, (Fig. S10). The pneumothoraces missed by lung-ultrasound were small, located in the apex and did not require any intervention. 6 Table S1: Regional analysis Sensitivity, specificity, positive and negative predictive values and diagnostic accuracy of chest x-ray (CXR) and lung-ultrasound (LU) compared to thoracic computed tomography (CT) scan for each abnormality and for each lung region. PPV; positive predictive value, NPV; negative predictive value, DA; Diagnostic accuracy. +; positive for the abnormality. -; negative for the abnormality. Pathology Consolidation Pneumothorax Pleural Effusion Interstitial Syndrome LU/CXR LU + LU CXR + CXR LU + LU CXR + CXR – LU + LU CXR + CXR LU + LU CXR + CXR - CT + CT - 101 19 27 93 8 5 0 13 106 10 46 70 204 24 49 179 48 336 20 363 5 486 2 489 44 344 18 370 29 247 18 258 Sensitivity Specificity (%) (%) PPV (%) NPV (%) DA (%) 84 88 68 95 87 23 95 57 80 78 62 99 62 99 98 0 100 0 97 97 91 89 71 97 89 40 95 72 84 83 89 89 88 91 89 21 93 73 59 61 Sensitivity = (TP /TP+FN) ×100. Specificity = (TN/TN+FP) ×100. Positive Predictive Value = (TP/TP+FP)×100. Negative Predictive Value = (TN/TN+FN) ×100. Diagnostic accuracy= (TP+TN/ TP+TN+FP+FN) ×100 TP; True Positive. TN; True Negative. FP; False Positive. FN; False Negatives 7 References 1. Austin JH, Muller NL, Friedman PJ, Hansell DM, Naidich DP, Remy-Jardin M, Webb WR, Zerhouni EA, (1996) Glossary of terms for CT of the lungs: recommendations of the Nomenclature Committee of the Fleischner Society. Radiology 200: 327-331 2. Lichtenstein D, Goldstein I, Mourgeon E, Cluzel P, Grenier P, Rouby JJ, (2004) Comparative diagnostic performances of auscultation, chest radiography, and lung ultrasonography in acute respiratory distress syndrome. Anesthesiology 100: 9-15 3. Lichtenstein DA, Meziere GA, (2008) Relevance of lung ultrasound in the diagnosis of acute respiratory failure: the BLUE protocol. Chest 134: 117-125 4. Lichtenstein DA, (2009) Ultrasound examination of the lungs in the intensive care unit. Pediatr Crit Care Med 10: 693-698 5. Lichtenstein DA, Lascols N, Meziere G, Gepner A, (2004) Ultrasound diagnosis of alveolar consolidation in the critically ill. Intensive Care Med 30: 276-281 6. Yang PC, Luh KT, Chang DB, Yu CJ, Kuo SH, Wu HD, (1992) Ultrasonographic evaluation of pulmonary consolidation. Am Rev Respir Dis 146: 757-762 7. Yang PC, (1996) Color Doppler ultrasound of pulmonary consolidation. European journal of Ultrasound 3: 169-178 8. Lichtenstein DA, Meziere GA, Lagoueyte JF, Biderman P, Goldstein I, Gepner A, (2009) A-lines and B-lines: lung ultrasound as a bedside tool for predicting pulmonary artery occlusion pressure in the critically ill. Chest 136: 1014-1020 8 9. Bouhemad B, Zhang M, Lu Q, Rouby JJ, (2007) Clinical review: Bedside lung ultrasound in critical care practice. Crit Care 11: 205 10. Lichtenstein DA, Meziere G, Lascols N, Biderman P, Courret JP, Gepner A, Goldstein I, Tenoudji-Cohen M, (2005) Ultrasound diagnosis of occult pneumothorax. Crit Care Med 33: 1231-1238 11. Lichtenstein D, Meziere G, Biderman P, Gepner A, (2000) The "lung point": an ultrasound sign specific to pneumothorax. Intensive Care Med 26: 14341440 12. Remerand F, Dellamonica J, Mao Z, Ferrari F, Bouhemad B, Jianxin Y, Arbelot C, Lu Q, Ichai C, Rouby JJ, Multiplane ultrasound approach to quantify pleural effusion at the bedside. Intensive Care Med 36: 656-664 9 Legends of Video Video 1. Power Doppler application in one of the studied patients in order to differentiate echoic pleural effusion from lower lobe consolidation. Legends of Figures Figure S1. Top: The lung point. Lung point was used as guide for pneumothorax location. Bottom: Stratosphere sign. This is the intercostal space where chest tube was placed. Figure S2. Left: MDCT at the upper lung fields revealed ground glass opacities. Right: Lung-ultrasound examination revealed B3 lines at the upper anterior regions in a patient suffered from cardiogenic pulmonary oedema. Figure S3. Top: MDCT at the left middle lung revealed ground glass opacities. Bottom-right: Lung-ultrasound examination revealed lung rockets at the same region. Bottom-Left: Multiple B-lines in the left anterior upper region. Images were received from supraclavicular space. Figure S4. Lung-ultrasound examination of left lower lateral region revealed B-lines in a polytrauma patient with chest trauma. CT was negative for the same pathology at the same region. False positive result. Figure S5. Left: MDCT after iv contrast material revealed bilateral consolidations with air bronchogram associated with pleural effusions. Right: Lung-ultrasound longitudinal scan at the lower lateral regions. The main ultrasound features included bilateral consolidations with air bronchogram and pleural effusions. Figure S6. False positive case of lower lobe segmental consolidation. MDCT didn’t identify the same pathology. Figure S7. Top: MDCT revealed pleural effusion at the left costophrenic angle and a small consolidation with air bronchogram. Bottom: Lung-ultrasound longitudinal 10 scan at the left base corresponding at the left lower lateral region. The main ultrasound features included consolidation with air bronchogram and pleural effusion. Figure S8. Top: MDCT after iv contrast material displayed pleural effusion at the left posterior region and a small consolidation. Right: Lung-ultrasound longitudinal scan at the left lower lateral region revealed consolidation and pleural effusion. Radiological and ultrasound findings were identical at the contrary hemithorax. Figure S9: Top: MDCT shows pneumothorax and nodular consolidation. Bottom: Stratosphere sign and lung point. In the lung-ultrasound examination the consolidation was not observed due to the presence of pneumothorax. Figure S10: False positive test for pneumothorax in a COPD patient with over inflation. 11