Health Hazards of Solvents Case Study
advertisement

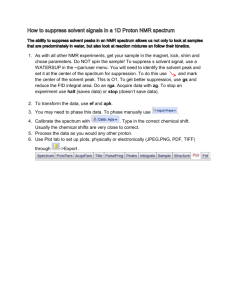
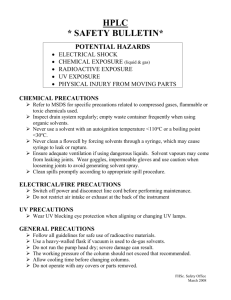
Health Hazards of Solvents Case Study #1 SLIDE #1: Teaching objectives for this case are: (1) To understand the steps in diagnosis of toxic peripheral neuropathy related to solvent exposure. (2) To be able to elicit a useful exposure history from a solvent-exposed worker. (3) To be aware of the types of biological monitoring that may be indicated in solvent-exposed workers. (4) To understand the concept of potentiation of n-hexane neurotoxicity by other solvents. (5) To recognize the importance of reporting of occupational disease to local and state public health authorities, and potential public health implications of a case of occupational disease. SLIDE #2: NO NOTES SLIDE #3: The first case is a 24-year-old male automotive technician who had worked in the auto repair industry during September 1995–April 1997. In January 1997, numbness and tingling developed in his hands and feet then spread proximally to his forearms and to his waist. SLIDE #4: He had no prior medical problems such as diabetes or thyroid disease. No recent viral upper respiratory infection. Alcohol history: one drink per week. He did brake repair, and was the 'star' worker for the previous 10 months, based on the number of jobs performed in each day. SLIDE #5: He had reported using from 5-10 12-ounce aerosol cans of brake cleaner per day. In addition to cleaning brakes, the technician sprayed the product on tools, small spills, and engine surfaces. He occasionally used a rag. He reported wearing latex gloves daily. (Latex gloves provide poor protection from solvents in general due to rapid breakthrough). No prior industrial hygiene or biological monitoring was reported. He had no hobbies with solvent exposure. He previously used a brake cleaner that contained perchloroethylene mixed with other solvents. This was phased out due to Environmental Protection Agency and Regional Air Quality Management District regulations largely due to its carcinogenic risk. 1 SLIDE #6: This brake cleaner contains 50%–60% hexane (composed of 20-80% n-hexane), 20%– 30% toluene, and 1%–10% each of methyl ethyl ketone (MEK), acetone, isopropanol, methanol, and mixed xylenes. Which of these solvents have been associated with toxic peripheral neuropathy? (hexane, toluene – cases of optic neuropathy in glue sniffers, methyl ethyl ketone, acetone, isopropanol) Would the effects of exposures to mixtures of these solvents be additive? (Yes) Synergistic? (Possibly) Do methyl ethyl ketone, acetone and isopropanol potentiate the effects of n-hexane on peripheral nerves? (Yes – all have been reported to potentiate n-hexane effects). SLIDE #7: The MSDS simply states, "Acute overexposure can cause serious nervous system depression". Is this adequate warning, given what you know about the risks of n-hexane? SLIDE #8: Physical examination of the skin, head, ears, nose, throat and gastro-intestinal systems were normal. SLIDE #9: Neurological examination was abnormal with marked sensory deficits, loss of position sense in both lower extremities, positive Romberg test, abnormal tandem gait and absent deep tendon reflexes. SLIDE #10: Mental status examination (serial 7’s – subtracting 7 sequentially beginning from 100), short term recall (3 objects @ 5 minutes), and digit span (numbers recalled forward and backward) were normal. SLIDE #11: Liver function showed normal serum aspartate aminotransferase (AST) and mildly elevated serum alanine aminotransferase (ALT). The AST/ALT ratio is less than 1.0. Reported Causes of polyneuropathy include inflammatory (e.g., Guillain-Barr Syndrome), metabolic (diabetes, uremia), nutritional (Beri-beri Thiamine deficiency, pellagro or niacin deficiency), neoplastic, infectious (leprosy, diphtheria, measles, mumps, brucellosis, HIV), toxic (alcohol, lead, arsenic, mercury, thallium, insecticides, acrylamide, n-hexane), drugs (INH, nitrofurantoin, vincristine, metronidazole), genetic. Guillain-Barr syndrome (GBS) is an acute inflammatory polyneuropathy that in some patients follows an upper respiratory viral infection. Maximum weakness usually is seen 10-14 days after onset (unlike this case where symptoms progressed over several months). CSF examination usually shows elevated protein without elevated cell counts. Other possible diagnoses include acute myesthenia gravis and poliomyelitis (CSF typically has elevated cell count). 2 SLIDE #12: From ACGHI TLV BEI Handbook 2002 SLIDE #13: While the willingness of this employer to stop using n-hexane containing products is admirable in this case, evaluation of potential substitutes for additional health risks is also necessary. Substitute with water-based processes where these exist is usually preferable to use of other organic solvent – based products. SLIDE #14: The occupational medicine physician’s diagnosis is toxic peripheral neuropathy, most likely due to n-hexane. We also need to consider the potentiation of n-hexane toxicity by other solvents such as isopropanol and acetone. Chronic n-hexane exposure produces a gradual sensorimotor neuropathy with demyelinating features. The most common initial complaint is numbness and tingling of the toes and fingers; a progressive loss of motor function may develop. Chronic polyneuropathy with demyelinating features also is associated with other underlying conditions. Other causes of peripheral neuropathy should be considered when evaluating persons with possible n-hexane-related peripheral neuropathy. Removal from n-hexane exposure is the only known treatment for n-hexane-related neurotoxicity. The prognosis for n-hexane neuropathy generally is favorable, but recovery may take months to years, depending on disease severity. The current Occupational Safety and Health Administration permissible exposure limit (PEL) for n-hexane, adopted in 1971, is 500 ppm in air. NIOSH established a recommended PEL of 50 ppm in 1989; the PEL for ACGIH TLV and California are 50 ppm. What public health prevention measures might be considered as a result of this case? Cases of n-hexane--related neuropathy in the automotive repair industry could be prevented through reformulation of hexane-containing products and greater use of aqueous cleaning systems. 3 Health Hazards of Solvents Case Study #2 SLIDE #1 Objectives of this case: (1) Understand the health effects and physical as well as psychological sequelae of acute solvent overexposure. (2) Recognize hazards of confined space entry and what employer recommendations may be indicated following a case of solvent intoxication. SLIDE #2 Your patient, a 24 year old male electrical parts manufacturing worker, entered a vapor degreasing tank to clean the tank, noted dizziness and fell unconscious to bottom of tank. His co-worker noted that he had fallen, climbed in after him and tried to lift him out of tank. He was able to get out of the tank before becoming a second victim. (photo: used by permission, US Army, http://safety.army.mil/pages/lessonslearned/industrialphotos.ppt ) SLIDE #3 There was a 5-8 minutes delay until paramedics arrived. Initial examination by paramedics at the scene found that the index case was cyanotic, pulseless, no spontaneous respirations. Paramedics donned SCBA and protective clothing and lifted both patients out of tank. A review of the degreaser MSDS revealed 1,1,1-trichloroethane. 1,1,1-trichloroethane levels measured in the bottom of tank = 20,000 ppm. Measured oxygen levels in tank were low due to displacement by solvent vapor. 1,1,1-trichloroethane (methyl chloroform) has a TLV of 300 ppm and a STEL of 450 PPM. BEI are trichloroethane in blood 1 mg/l in urine 30 mg/l. ASTDR lists trichloroethane as an intoxicant with CNS and anesthetic effects. No blood levels were obtained in this case. SLIDE #4 The index case was intubated and CPR initiated. His initial ECG shows episodes of complete heart block. P waves are not conducted to the ventricles because of block at the AV node. The ventricles are depolarized by a ventricular escape rhythm. O2 saturation was reduced. AST and ALT were both mildly elevated. CPK, CPK-MB fraction and troponin were persistently normal, making myocardial infarction unlikely. (ECG -thanks to: Dean Jenkins, Specialist Registrar, UWCM, Cardiff, Wales, http://www.ecglibrary.com/ecghome.html) 4 SLIDE #5 Your patient reports ongoing symptoms in follow-up clinic visit: lightheadedness, trouble with speech, memory and sleep disturbance. Shortness of breath on exertion, wheezing. Nightmares about the incident. Physical Examination was normal except he had wheezing on forced expiration, abnormal mental status (Digit span forward = 6, reverse=4). SLIDE #6 Neuropsychological testing showed decreased grip strength on left. Otherwise normal. PFTs were normal with a FVC 5.48 (116% of predicted), FEV1 4.48 (114%), FEV1/FVC 84%. Methacholine challenge showed increased responsiveness to methacholine. Psychiatric evaluation revealed fear, tension, anxiety, recurrent ruminations and dreams about incident, with anger and depression. SLIDE #7 What diagnoses do these results suggest? Is the patient disabled? His vocation rehabilitation counselor asks whether he would be a good candidate to be a floor refinisher? What do you say? What recommendations would you give to the employer? SLIDE #8 This is a clear case of failure to follow OSHA’s recommended confined space procedures (29 CFR 1910.146 ) The scenario is in keeping with historical presentations of confined space problems where one individual enters a tank and collapses and the individual who attempts to save the first victim enters the tank and quickly is also overcome. His diagnoses include: s/p cardiopulmonary arrest due to solvent intoxication and likely acute asphyxiation in degreasing tank Reactive airways disease most likely due to acute solvent overexposure Post-traumatic stress disorder (PTSD) He is unlikely to be able to return to his prior employment as a vapor degreaser. He probably should avoid future exposures to respiratory irritants or high levels of solvents. Thus, he would not be a good candidate to be a floor refinisher. Recommendations to employer: A more adequate confined space program including certification / permits, ventilation, continuous gas sampling and control of environment, training, surveillance, standby worker, self-contained breathing apparatus. 5 References: Intentional and accidental inhalation of 1,1,1-trichloroethane has resulted in human fatalities as reported in several case studies (Hall and Hine 1966, MacDougall et al. 1987, Stahl et al. 1969). Estimations for fatal exposure concentrations range from 6000 to 20,000 ppm (ATSDR 1995). Death has been attributed to either depression of the central nervous system, resulting in respiratory arrest (Hall and Hine 1966, Jones and Winter 1983, Stahl et al., 1969), or sensitization of the heart to epinephrine, resulting in cardiac arrhythmia (Guberan et al. 1976, MacDougall et al. 1987, Travers 1974). Cited in ATSDR Toxicological Profile, 1,1,1-Trichloroethane. 6 Health Hazards of Solvents Case Study #3 SLIDE #1: Teaching Objectives of this Case: (1) Understanding the risk factors and characteristics of chemically-induced headaches (2) Recognizing the options for diagnosis and treatment of solvent-related disease. SLIDE #2: The patient works in a chemical barn for a chemical company. He was working next to a 2000 gallon chemical storage tank containing lasso-atrazine (triazine herbicide), which was recirculating and a high pressure hose broke and sprayed chemical into his face. SLIDE #3: First aid and eye wash was provided. His complaints initially included eye irritation and visual difficulties, headaches. An eye exam by ophthalmologist showed that the corneal stain was + on L eye. Acuity testing showed he was able to see at 20/70 L eye, 20/70 R eye. SLIDE #4: Review of the material safety data sheet revealed that the exposure to benzene chloride is probably most significant given his symptomatology. Other ingredients are eye and skin sensitizers, but are unlikely to result in his headache symptoms. SLIDE #5: Headaches start predictably after he starts work at the plant in the same area. They resolve on weekends, and several hours after going home from work. One type of headache was bitemporal, constant and mild in character (3/10). The second type was much more intense (9/10), pulsating, associated with nausea and vomiting, and required him to stop whatever he was doing at the time and rest. Other triggers should be inquired about: alcohol, foods, sunlight, medications. None were reported in this case. SLIDE #6: He was evaluated at the University Clinic, and treated with amitriptyline and trilafon. He had no prior history of headaches. No family history of headaches / migraine. He reports sleep disturbance: early awakening and intrusive thoughts. ETOH: occasional wine with dinner. He reports multiple prior mild acute intoxication episodes characterized by dizziness. 7 SLIDE #7: Laboratory testing included neuropsychological evaluation that showed difficulty with verbal memory, and complex visual memory especially memory storage of new information Full scale IQ 78 Premorbid estimate 106 Mild loss of cognitive integrative functions Personality: severe depression. After six months, a CT scan of brain is performed and is normal. CT scan is indicated to evaluate patient for potential other anatomic causes (benign cysts, other tumors, hydrocephalus). His visual acuity gradually returned to 20/20 in both eyes. SLIDE #8: Diagnoses: 1. Chemical headache from solvent exposure. 2. Mild chronic toxic encephalopathy, likely a sequelae of acute and chronic solvent exposure. 3. Post-traumatic stress disorder and reactive depression. Features of chemical headache: A. Occurs within a specified time after substance intake. B. A certain required minimum dose should be indicated. C. Has occurred in at least ½ of exposures and at least 3 times. D. Disappears when substance is eliminated or within a specified time thereafter. In this case, the chemical most likely responsible is the solvent carrier, benzene chloride. Other chemicals often associated with headaches include nitroglycerin, tyramine and phenylethylamine, aspartamine (NutraSweet®, contained in migraine medication Maxalt® can trigger headaches in a small % of persons), nerve agents (Organophosphate pesticides, CX), monosodium glutamate (MSG), sodium nitrate (“Hot Dog Headache”), carbon monoxide, excessive levels of vitamin A, other solvent mixtures. Prognosis: Fair for improvement over several years if he avoids solvent exposure and alcohol ingestion. Toxic encephalopathy may also manifest as headache, complicating the presentation in this case. Additional treatment recommendations that may be considered: A trial of biofeedback. 8