Aerobic vaginal flora influence on preterm delivery, preterm
advertisement
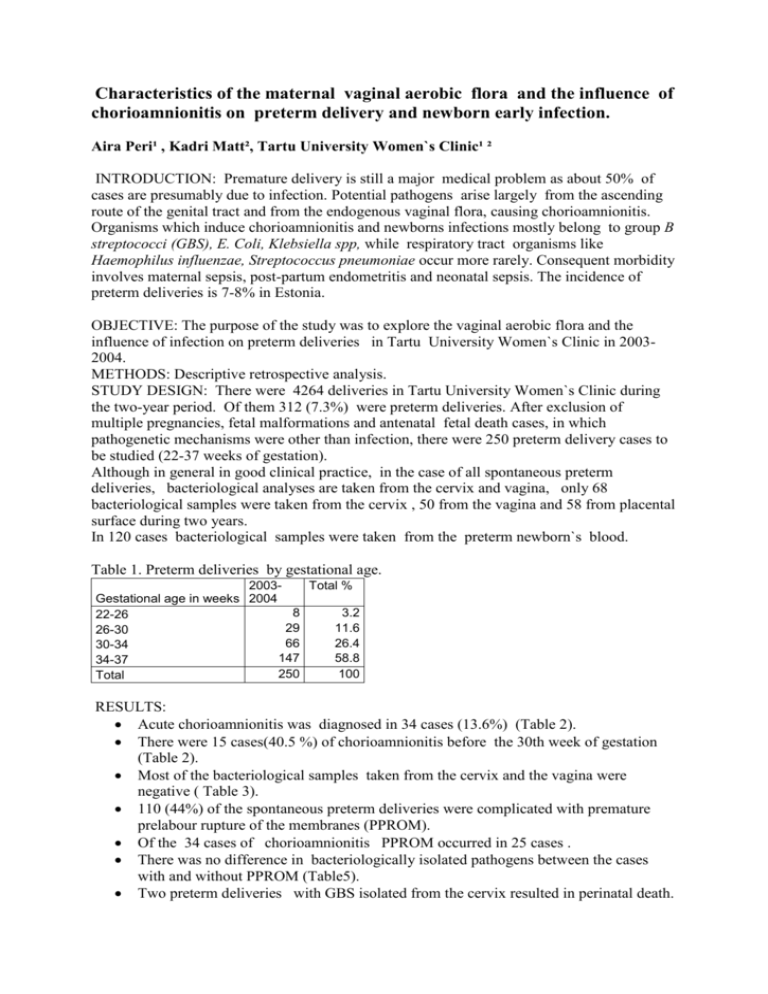
Characteristics of the maternal vaginal aerobic flora and the influence of chorioamnionitis on preterm delivery and newborn early infection. Aira Peri¹ , Kadri Matt², Tartu University Women`s Clinic¹ ² INTRODUCTION: Premature delivery is still a major medical problem as about 50% of cases are presumably due to infection. Potential pathogens arise largely from the ascending route of the genital tract and from the endogenous vaginal flora, causing chorioamnionitis. Organisms which induce chorioamnionitis and newborns infections mostly belong to group B streptococci (GBS), E. Coli, Klebsiella spp, while respiratory tract organisms like Haemophilus influenzae, Streptococcus pneumoniae occur more rarely. Consequent morbidity involves maternal sepsis, post-partum endometritis and neonatal sepsis. The incidence of preterm deliveries is 7-8% in Estonia. OBJECTIVE: The purpose of the study was to explore the vaginal aerobic flora and the influence of infection on preterm deliveries in Tartu University Women`s Clinic in 20032004. METHODS: Descriptive retrospective analysis. STUDY DESIGN: There were 4264 deliveries in Tartu University Women`s Clinic during the two-year period. Of them 312 (7.3%) were preterm deliveries. After exclusion of multiple pregnancies, fetal malformations and antenatal fetal death cases, in which pathogenetic mechanisms were other than infection, there were 250 preterm delivery cases to be studied (22-37 weeks of gestation). Although in general in good clinical practice, in the case of all spontaneous preterm deliveries, bacteriological analyses are taken from the cervix and vagina, only 68 bacteriological samples were taken from the cervix , 50 from the vagina and 58 from placental surface during two years. In 120 cases bacteriological samples were taken from the preterm newborn`s blood. Table 1. Preterm deliveries by gestational age. 2003Total % Gestational age in weeks 2004 8 3.2 22-26 29 11.6 26-30 66 26.4 30-34 147 58.8 34-37 250 100 Total RESULTS: Acute chorioamnionitis was diagnosed in 34 cases (13.6%) (Table 2). There were 15 cases(40.5 %) of chorioamnionitis before the 30th week of gestation (Table 2). Most of the bacteriological samples taken from the cervix and the vagina were negative ( Table 3). 110 (44%) of the spontaneous preterm deliveries were complicated with premature prelabour rupture of the membranes (PPROM). Of the 34 cases of chorioamnionitis PPROM occurred in 25 cases . There was no difference in bacteriologically isolated pathogens between the cases with and without PPROM (Table5). Two preterm deliveries with GBS isolated from the cervix resulted in perinatal death. ( Table 6). In 1 case with maternal GBS colonisation the newborn had congenital sepsis, but the pathogen isolated from the newborn`s blood was Haemophilus influenzae( Table 6). In most cases of congenital neonatal sepsis cases bacteriological cultures from the mother had been negative, or the samples had not been taken ( Table 6). In 8 of 20 congenital sepsis cases pathogens were isolated from the newborn`s blood (E. Coli, Citrobacter, Klebsiella pneumoniae, Enterococcus faecalis, αhemolytical Streptococcus, Haemophilus influenzae, CONS, Streptococcus epidermidis). Mother and newborn need not share the same pathogens. In many clinical complication cases the bacteriological sample is negative owing to method related difficulties ( Tab. 4; 6). Table 2. Relationship between acute chorioamnionitis and gestational age. Age group 22-26 26-30 30-34 34-37 Total Acute chorioamnionitis 5 10 8 11 34 Proportion (%) of patients with chorioamninitis 62 34.5 12.1 7.5 13.6 Table 3. Relationship between gestational age and presence of pathogens in the cervix and the vagina before threatened or during preterm delivery. Gestational age 22-26 26-30 30-34 34-37 Total E. coli 5 1 6 GBS 1 1 1 5 8 Other aerobic Candida pathogens albicans * 1 1 1 1 7 4 9 6 Number of Number of negative investigated samples samples 5 7 17 19 29 37 38 55 89 118 *other aerobic pathogens (Klebsiella pneumoniae, Staphylococcus pneumoniae, Citrobacter kreundii; Streptococcus pyogenes, Enterobacter cloacae, Streptococcus pyogenes) Table 4. Relationship between presence of placental surface pathogens and number of acute chorioamnionitis cases. Bacteriological pathogens from placental surface Number of acute Number of chorioamnionitis positive samples cases E. coli 9 4 GBS 3 1 Candida albicans 1 Other aerobic pathogens 6 2 Sample negative 39 11 Sample was not taken 192 16 Total 250 34 Table 5.Relationship between PPROM and presence of pathogens in the cervix and vagina before threatened or during preterm delivery. PPROM No Yes Total E. Coli Candida albicans GBS 3 3 6 4 4 8 Other aerobic organism 4 5 9 2 4 6 Negative 38 51 89 Total number of investigated patients 140 110 250 Table 6. Relationship between presence of pathogens isolated from the mother`s cervix during pregnancy and preterm newborn`s perinatal infection. Organism from cervix Perinatal death Infectio Without Cong. Cong. sepsis pneum. Omphalitis Conjunct. nonspec. infection Nosocom. Total E. coli 2 GBS Candida albicans Other aerobic pathogens Sample negative Sample was not taken 2 Total 1 2 1 1 4 1 6 6 2 4 2 8 1 7 4 2 26 2 52 4 10 3 32 10 9 108 6 182 8 20 4 41 14 11 144 8 250 Table 7. Relationship between gestational age and preterm newborn´s perinatal infection. Gestational Perinatal age death Infectio Without Cong. Cong. sepsis pneum. Omphalitis Conjunct. nonspec. infection Nosocom. Total 22-26 1 5 1 26-30 2 4 1 30-34 2 10 34-38 3 1 Total 8 20 1 8 3 1 2 10 6 29 17 2 1 33 1 66 2 21 11 8 100 1 147 4 41 14 11 144 8 250 Conclusions: 1. The number of performed bacteriological investigations is too small for making reliable general conclusions. 2. In most congenital sepsis cases the mother´s bacteriological culture had been negative, or samples had not been taken. 3. GBS colonisation can be associated with early-gestation preterm delivery, perinatal death and congenital sepsis, although GBS need not be detected in the newborn´s blood. 4. In clinical infection cases with a negative bacteriological result it can be assumed that the method of bacterial investigation is insensitive or inadequate. 5. Further randomised trials with more sensitive methods of bacterial investigation should be conducted in order to reduce the incidence of preterm deliveries and newborn early infection. Literature: 1. S. M. Garland, F.N Chuileannain, C.Satze, R. Robins-Browne . Mechanisms, organisms and markers of infection in pregnancy. Journal of Reproductive Immunology 57, 2002;169-183 2. R. L ,Goldenberg, J.C. Hault ,W.W Andrews. Mechanism of Disease:Intrauterine Infection and Preterm Delivery. The New England Yournal of Medicine.Vol 342 2002 May; 1500-1507 3. Tucker JM, Goldberg RL, Davis RO, Copper RL; Winkler CL Hautch JC. Etiologies of preterm birth in an indigent population: is prevention a logical expectation?ObstetrGynecol 1991; 77:343-7 4. Kimberlin DF, Hautch JC, Owen J, Bottoms SF, Iams JD, Mercer BM, Thom EA, Moawad AH, Van Dorsten JP, Thurnau GR. Indicated versus spontaneous preterm delivery.Am J Obstetr Gynecol 1999; 180(3pt1):683-9 5. Gilles R.G Monif; David A. Baher Infectious Disease in Obstetrics and Gynecology 2004:451-461