Neolymphangiogenesis in diabetic kidney disease
advertisement
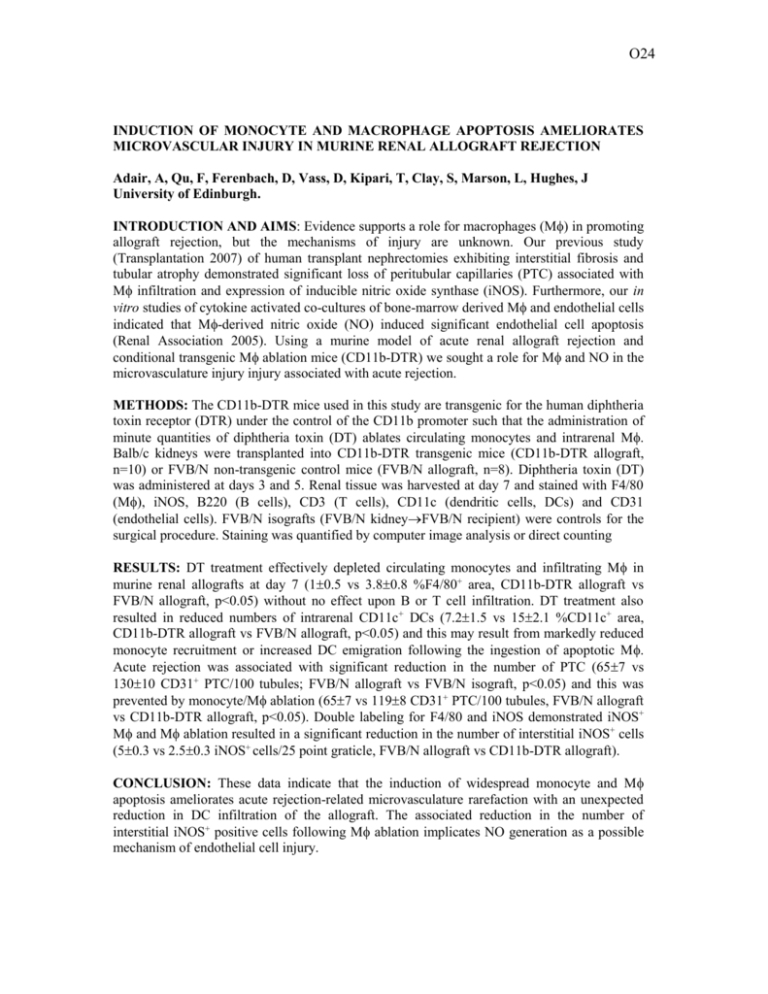
O24 INDUCTION OF MONOCYTE AND MACROPHAGE APOPTOSIS AMELIORATES MICROVASCULAR INJURY IN MURINE RENAL ALLOGRAFT REJECTION Adair, A, Qu, F, Ferenbach, D, Vass, D, Kipari, T, Clay, S, Marson, L, Hughes, J University of Edinburgh. INTRODUCTION AND AIMS: Evidence supports a role for macrophages (M) in promoting allograft rejection, but the mechanisms of injury are unknown. Our previous study (Transplantation 2007) of human transplant nephrectomies exhibiting interstitial fibrosis and tubular atrophy demonstrated significant loss of peritubular capillaries (PTC) associated with M infiltration and expression of inducible nitric oxide synthase (iNOS). Furthermore, our in vitro studies of cytokine activated co-cultures of bone-marrow derived M and endothelial cells indicated that M-derived nitric oxide (NO) induced significant endothelial cell apoptosis (Renal Association 2005). Using a murine model of acute renal allograft rejection and conditional transgenic M ablation mice (CD11b-DTR) we sought a role for M and NO in the microvasculature injury injury associated with acute rejection. METHODS: The CD11b-DTR mice used in this study are transgenic for the human diphtheria toxin receptor (DTR) under the control of the CD11b promoter such that the administration of minute quantities of diphtheria toxin (DT) ablates circulating monocytes and intrarenal M. Balb/c kidneys were transplanted into CD11b-DTR transgenic mice (CD11b-DTR allograft, n=10) or FVB/N non-transgenic control mice (FVB/N allograft, n=8). Diphtheria toxin (DT) was administered at days 3 and 5. Renal tissue was harvested at day 7 and stained with F4/80 (M), iNOS, B220 (B cells), CD3 (T cells), CD11c (dendritic cells, DCs) and CD31 (endothelial cells). FVB/N isografts (FVB/N kidneyFVB/N recipient) were controls for the surgical procedure. Staining was quantified by computer image analysis or direct counting RESULTS: DT treatment effectively depleted circulating monocytes and infiltrating M in murine renal allografts at day 7 (10.5 vs 3.80.8 %F4/80+ area, CD11b-DTR allograft vs FVB/N allograft, p<0.05) without no effect upon B or T cell infiltration. DT treatment also resulted in reduced numbers of intrarenal CD11c+ DCs (7.21.5 vs 152.1 %CD11c+ area, CD11b-DTR allograft vs FVB/N allograft, p<0.05) and this may result from markedly reduced monocyte recruitment or increased DC emigration following the ingestion of apoptotic M. Acute rejection was associated with significant reduction in the number of PTC (657 vs 13010 CD31+ PTC/100 tubules; FVB/N allograft vs FVB/N isograft, p<0.05) and this was prevented by monocyte/M ablation (657 vs 1198 CD31+ PTC/100 tubules, FVB/N allograft vs CD11b-DTR allograft, p<0.05). Double labeling for F4/80 and iNOS demonstrated iNOS+ M and M ablation resulted in a significant reduction in the number of interstitial iNOS+ cells (50.3 vs 2.50.3 iNOS+ cells/25 point graticle, FVB/N allograft vs CD11b-DTR allograft). CONCLUSION: These data indicate that the induction of widespread monocyte and M apoptosis ameliorates acute rejection-related microvasculature rarefaction with an unexpected reduction in DC infiltration of the allograft. The associated reduction in the number of interstitial iNOS+ positive cells following M ablation implicates NO generation as a possible mechanism of endothelial cell injury.