RENAL REGULATION OF ACID BASE BALANCE
advertisement

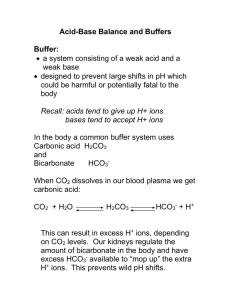
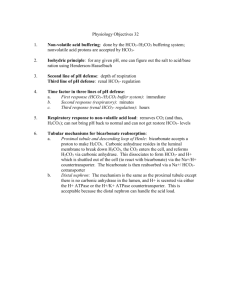
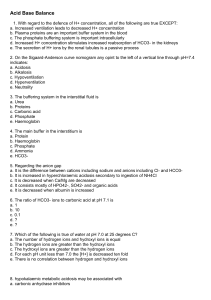
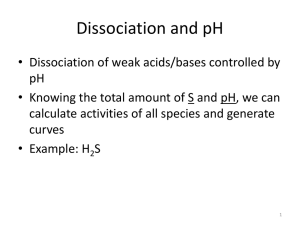
ACID BASE BALANCE (INCLUDING RENAL REGULATION) Stephen P. DiBartola, DVM Learning Objectives/Study Questions 1. 2. 3. 4. 5. 6. 7. 8. Why is CO2 considered an acid in biological systems? Why is HCO3- the most important buffer in the extracellular fluid? Why is phosphate an important buffer in the urine? Understand the importance of the Henderson-Hasselbach equation in its clinically relevant form for the assessment of acid base balance. Know the primary acid base disturbances and their secondary compensatory responses. Explain in detail the body's compensation for an added load of fixed acid. Explain in detail the body's compensation to hypoventilation. How do these responses differ? What single process in the kidney is ultimately responsible for the reabsorption of filtered HCO3- and the net excretion of acid? Why is NH4+ excretion by the kidney not considered part of titratable acidity? What factors affect HCO3- reabsorption by the kidney? I. Introduction A. Definition of terms 1. pH a. most electrolytes in the extracellular fluid are present in milliequivalent quantities (i.e. 10-3) but H+ ions (see note A at end of handout) are present in nanoequivalent quantities (i.e. 10-9) b. to facilitate discussion of such small quantities of H+ ions, the concept of pH was established: pH = -log[H+] c. in the normal animal, [H+] = 40 nEq/L or 4 X 10-8 Eq/L: pH = -log(4 X 10-8) = 7.4 d. the pH of blood is normally maintained in the narrow range of 7.37-7.42 and the extreme range compatible with life is 6.8-8.0 2. Acids and their origin in the body a. an acid is a substance which can donate a proton (H+ ion) i. the concept of CO2 as an acid is difficult since it is not an obvious proton donor. However, through interaction with water it forms H2CO3 which (under body conditions) immediately dissociates into H+ and HCO3- and thus a proton is "donated" ii. because the carbonic H2CO3-HCO3- system is in equilibrium with a gas (CO2), CO2 is called a volatile acid. Carbon dioxide is the major source of acid which is produced daily in the body from oxidative metabolism and accounts for 15,000-20,000 mEq of acid production per day. This CO2 is transported to the lungs (largely as HCO3because the associated H+ ions are buffered by hemoglobin in the red cells) and removed from the body by pulmonary ventilation. iii. the metabolism of the sulfur-containing amino acids in proteins results in the production of sulfuric acid and the metabolism of phospholipids results in the production of phosphoric acid. Metabolic production of organic acids such as lactic acid and ketones constitutes an additional source of acid. These are called fixed or nonvolatile acids and account for about 40-80 mEq of acid production per day in humans eating a Western diet. This figure likely is higher in carnivores and, in herbivores metabolic utilization of H+ occurs as organic anions are metabolized and HCO3- is produced. In herbivores, the nonvolatile component is a net loss of H+ ions. Table 1: External balance for H+ ions Input ! ! ! ! CO2 production in tissues from oxidative metabolism (volatile acid) Production of non-volatile (fixed) acid from metabolism of proteins (sulfuric acid) and phospholipids (phosphoric acid) Gain of H+ ions from loss of HCO3- in gastrointestinal secretions Gain of H+ ions from loss of HCO3- in urine (normally very little HCO3- is lost in urine 99.9% is reabsorbed) Output ! ! ! ! CO2 removal by pulmonary ventilation (volatile acid) when H+ ions recombine with HCO3in the lungs Utilization of H+ ions during metabolism of organic anions (e.g. lactate, citrate) Loss of H+ ions in vomitus Loss of H+ ions in urine 3. Buffers a. a buffer is substance that can accept protons (H+ ions) and minimize (but not eliminate) a change in pH b. a physiologic buffer pair consists of a weak acid and its salt. When a strong acid is added to such a system, the dissociated protons from the strong acid are donated to the salt of the weak acid and the change in pH is minimized c. as demonstrated by the sigmoidal (i.e. flat at the top and bottom, steep in the middle) nature of the titration curve for a buffer (see Figure 1), a buffer is most effective (i.e. can resist pH changes best) in the pH range from 1.0 pH unit above to 1.0 pH unit below its pKa. Figure 1: Titration curve of buffer solution. Note: (1) the pKa is equal to the pH at which there are equal concentrations of the weak acid and its conjugate salt (i.e. [salt]/[acid] = 1.0 and log 10(1) = 0); (2) the change in pH per unit of added acid or base is least in the steep linear portion of the curve in the region of the pKa; and, (3) the most effective chemical buffering zone extends approximately 1.0 pH unit on either side of the pKa (that is, a buffer is most effective within + 1.0 pH units of its pKa). Modified from Figure 10-2, page 282, Rose BD, ed 4, 1994. B. Biologically important buffers The effectiveness of a buffer in biological systems is determined by its concentration, its pKa, and any special circumstances which affect its chemistry in the body. 1. HCO3a. its pKa is 1.3 units below physiologic pH and thus is outside the most effective range b. however, its concentration in the extracellular fluid is very high (24 mEq/L) c. furthermore, it is in equilibrium with the volatile acid, CO2, the concentration of which can be regulated by pulmonary ventilation. This special circumstance makes HCO3- the most important buffer in the extracellular fluid: CO2 + H2O = H2CO3 = H+ + HCO32. phosphate a. important intracellularly where its concentration is high b. less important extracellularly where its concentration is low (2 mEq/L) c. important in the urine where it functions in the excretion of titratable acidity (see later) d. the pKa for the reaction: H2PO4- = H+ + HPO4-2 is 6.8 which contributes to the effectiveness of phosphate as a buffer in the distal tubular fluid where pH is 6.0-7.0 3. proteins a. plasma proteins play a limited role in extracellular buffering b. intracellular proteins (especially hemoglobin in red blood cells which buffers CO2 produced by cellular metabolism until it can be removed in the lungs) play an extremely important role in buffering 4. bone carbonate plays an important role in the longterm response to acidosis C. Henderson-Hasselbach equation 1. this equation is derived by solving the formula for the dissociation constant of an acid for pH: Ka = [H+][A-]/[HA] By rearranging and taking the logarithm of both sides of the equation: pH = pKa + log ([A-]/[HA]) For the HCO3- system: pH = pKa + log ([HCO3-]/[H2CO3]) a. dissolved CO2 can potentially form carbonic acid and thus the equation can be modified: pH = pKa + log ([HCO3-]/[dissolved CO2 + H2CO3]) b. at the temperature and ionic strength of extracellular fluid, there are approximately 6,800 HCO3- ions and 340 molecules of dissolved CO2 for every molecule of H2CO3. Thus, the concentration of H2CO3 can be safely neglected. c. the concentration of dissolved CO2 (in mEq/L) can be calculated from the partial pressure of CO2 (pCO2 in mm Hg) by using the solubility coefficient for carbon dioxide which is 0.03. Normally, pCO2 is about 40 mm Hg which equals 1.2 mEq/L (0.03 X 40). d. thus, the Henderson-Hasselbalch Equation simplifies to: pH = 6.1 + log ([HCO3-]/[0.03pCO2]) Where, 6.1 is the pKa for this system under conditions prevailing in the extracellular fluid e. This is the clinically relevant form of the equation and demonstrates clearly that body pH is regulated by the ratio of the plasma [HCO3-] (the metabolic component of the system) and pCO2 (the respiratory component of the system). Normally, this ratio is approximately 20:1. D. Physiologic lines of defense 1. physicochemical buffering by extracellular and intracellular buffers (seconds) 2. alterations in ventilation to change pCO2 (seconds to minutes) 3. renal readjustment of body HCO3- stores (hours to days; maximal by 2-6 days) E. Definitions of the primary acid base disorders 1. Metabolic acidosis: A decrease in plasma [HCO3-] and low pH due either to HCO3- loss or buffering of a non-carbonic fixed acid by HCO3-. 2. Metabolic alkalosis: An increase in plasma [HCO3-] and high pH due to H+ loss or HCO3- administration. 3. Respiratory acidosis: Impaired pulmonary excretion of CO2 resulting in an increase in pCO2 (hypercapnia). 4. Respiratory alkalosis: Hyperventilation resulting in a decrease in pCO2 (hypocapnia). 5. The terms acidemia and alkalemia refer specifically to the pH of blood whereas acidosis and alkalosis refer to the processes which cause acids and alkali to accumulate in the body. For example, a patient may have acidosis but technically not be acidemic. 6. A simple acid base disorder refers to a single initiating abnormality with its accompanying secondary compensatory response. The secondary response involves the system opposite the one disturbed and returns the pH in the direction of (but not completely to) normal. That is, the respiratory component compensates for the metabolic component and vice versa (e.g. primary metabolic acidosis with secondary respiratory alkalosis). Overcompensation does not occur. See Tables 2 and 3 for the expected compensatory responses and their magnitude. 7. A mixed acid base disorder refers to the presence of two independent acid base abnormalities and is diagnosed when the secondary compensatory response is not as predicted. See Table 3 for the magnitude of the expected compensatory responses. F. Physiologic compensation for the primary acid base disorders 1. Compensation for metabolic acidosis (e.g. addition of fixed acid) Table 2: Characteristics of the primary acid base disorders Disorder pH [H+] Primary Compensatory disorder response -------------------------------------------------------------------------------------------Metabolic acidosis [HCO3-] pCO2 Metabolic alkalosis [HCO3-] pCO2 Respiratory acidosis pCO2 [HCO3-] Respiratory alkalosis pCO2 [HCO3-] Give this table some thought. It looks simple, but many people are confused by it. Remember (1) CO 2 is an acid by virtue of its ability to combine with H2O and form H2CO3, and (2) the body's compensatory efforts are directed at maintaining the ratio of [HCO3-]/.03pCO2 as close to 20:1 as possible (i.e. the compensatory component will change in the same direction as the primary component to keep the ratio as constant as possible). a. within seconds to minutes, some added H+ titrates HCO3- in plasma (12%) and a little H+ enters red cells and is buffered by hemoglobin there (6%). Plasma proteins and plasma phosphate play negligible roles in the initial buffering process (1-2%). b. within minutes, ventilation increases to lower the pCO2 and remove the CO2 produced by titration of HCO3-. Hyperventilation further lowers the pCO2 below normal as the body attempts to return the HCO3-/.03pCO2 ratio toward 20:1 and the pH toward 7.4. c. within 30 minutes, H+ has entered the interstitial space and interstitial HCO3- has contributed to the buffering process (30%). d. within several hours, H+ has entered other cells in the body where intracellular proteins and phosphate contribute to buffering (50%). e. within 2-6 days, the renal regeneration of HCO3- and net excretion of the added acid is completed. Ventilation slowly returns to normal and the pCO2 increases back to normal. Acid base balance has now returned to normal. 2. Compensation for metabolic alkalosis is generally the reverse of the process described above but hypoventilation in response to increased plasma [HCO3-] is not as effective as hyperventilation in response to decreased plasma [HCO3-] and renal excretion of excess HCO3- occurs more rapidly than renal excretion of excess H+ 3. Compensation for respiratory acidosis a. within seconds to minutes, HCO3- is formed as the following equilibrium is moved to the right: CO2 + H2O = H2CO3 = H+ + HCO3-. The H+ formed enters red cells and is buffered by hemoglobin (29%) and a little is buffered by plasma proteins (3%). b. within hours, H+ from this reaction has entered other cells and is buffered by intracellular proteins and phosphate (68%) c. meanwhile, the HCO3- that has been produced increases the HCO3/.03pCO2 ratio toward 20:1 and the pH toward 7.4. d. if hypoventilation persists, over a period of 2-6 days, there is increased renal regeneration of HCO3- and excretion of H+ so that the HCO3/.03pCO2 ratio is increased closer to 20:1 and the pH closer to 7.4. 4. Compensation for respiratory alkalosis is mediated by a process which is the reverse of that described above. Table 3: Compensatory Response in Simple Acid Base Disorders in Dogs (from DiBartola SP, Fluid Therapy in Small Animal Practice, edition 2, 2000). Metabolic acidosis Metabolic alkalosis Acute respiratory acidosis Chronic respiratory acidosis Acute respiratory alkalosis Chronic respiratory alksosis For each 1 mEq/L decrease in HCO3-, pCO2 decreases 0.7 to 1.2 mm Hg (average of 1 mm Hg) For each 1 mEq/L increase in HCO3-, pCO2 increases 0.7 mm Hg For each 1 mm Hg increase in pCO2, HCO3- increases 0.15 mEq/L For each 1 mm Hg increase in pCO2, HCO3- increases 0.35 mEq/L For each 1 mm Hg decrease in pCO2, HCO3- decreases 0.25 mEq/L For each 1 mm Hg decrease in pCO2, HCO3- decreases 0.55 mEq/L Food for thought: Why are there TWO rules of thumb for the respiratory disorders but only ONE for the metabolic disorders? II. Renal Regulation of Acid Base Balance The role of the kidney in acid base balance is the preservation of body HCO3- stores. This role is accomplished by reabsorption of 99.9% of filtered HCO3- and regeneration of titrated HCO3- by excretion of titratable acidity (phosphate salts) and NH4+ salts. All of these things are accomplished by the secretion of H+ ions. If secreted H+ ions combine with filtered HCO3- ions, HCO3- is reabsorbed. If secreted H+ ions combine with phosphate or ammonia, net acid excretion and regeneration of new HCO3- occurs. Clearly understanding (not memorizing) these concepts is essential to fully appreciate the role of the kidneys in acid base balance. See below for explanation. A. Renal reabsorption of HCO3- (see Figure 2) 1. Sites a. 70-85% of filtered HCO3- is reabsorbed in the proximal tubule and 1020% is reabsorbed in the loop of Henle b. the remaining 4-7% is in the distal tubule and collecting ducts c. very little (perhaps 2 mEq) HCO3- is excreted in the urine (99.9% is reabsorbed) 2. Luminal transport systems for secretion of H+ ions a. Na+-H+ counter transport (anti-port) system in the proximal tubule and loop of Henle (quantitatively most important) b. H+-ATPase in all H+-secreting tubular segments c. H+-K+-ATPase in type A intercalated cells of the collecting ducts (quantitatively less important for H+ secretion but mediate active potassium reabsorption) 3. Mechanism (see Figure 2) a. CO2 in the cytoplasm of the tubular cell combines with water via cytoplasmic carbonic anhydrase to form H2CO3 (see note B at end of handout) b. This H2CO3 immediately dissociates into H+ and HCO3c. the H+ is actively secreted into the tubular fluid at the luminal membrane and Na+ enters passively for electroneutrality via the counter transport carrier system described above d. the HCO3- is reabsorbed by facilitated diffusion into the peritubular fluid along with Na+ for electroneutrality e. the secreted H+ encounters filtered HCO3- and combines to form H2CO3 which immediately is converted to H2O and CO2 by carbonic anhydrase located in the luminal membrane of the tubular cell f. the CO2 thus formed diffuses across the luminal membrane into the tubular cell and the process is repeated beginning with step a. above g. it is critical to note that filtered HCO3- has been reclaimed by this mechanism but no net H+ excretion has occurred (no new HCO3- has been formed). Thus, by secretion of H+, filtered HCO3- is reclaimed (see Figure 2). Figure 2: Renal tubular reabsorption of bicarbonate. From DiBartola SP: Fluid Therapy in Small Animal Practice, edition 2, WB Saunders Co, Philadelphia, 2000, page 205. 4. Factors affecting HCO3- reabsorption a. amount of HCO3- filtered i. the reabsorption of HCO3- is closely tied to the reabsorption of sodium which in turn is closely tied to the need of the animal to maintain a normal extracellular fluid volume (ECFV) ii. if GFR and ECFV are constant, the amount of HCO3- reabsorbed is nearly equal to the amount filtered iii. when alterations in the ECFV occur, changes in HCO3- reabsorption may also occur (see below) b. extracellular fluid volume (ECFV) i. expansion of the ECFV results in a decrease in HCO3- reabsorption and this decreases plasma [HCO3-] slightly (so-called "expansion acidosis") ii. expansion of the ECFV decreases proximal tubular sodium reabsorption and, because HCO3- reabsorption is closely tied to sodium reabsorption, proximal tubular HCO3- reabsorption also decreases iii. contraction of the ECFV has the opposite effect causing increased proximal tubular reabsorption sodium and HCO3- (so-called "contraction alkalosis") iv. thus, the apparent Tmax for HCO3- is sensitive to changes in ECFV, increasing with volume depletion and decreasing with volume expansion v. if volume depletion and metabolic alkalosis coexist (e.g. animal vomiting stomach contents), HCO3- continues to be reabsorbed as if it had no Tmax and metabolic alkalosis is perpetuated (this likely is due to the critical need to reabsorb sodium and restore ECFV) c. prolonged changes in arterial pCO2 i. HCO3- reabsorption is increased by a prolonged increase in arterial pCO2 (increase in apparent Tmax for HCO3- and decreased by a prolonged decrease in arterial pCO2 (decrease in apparent Tmax for HCO3-) ii. mechanisms include an increased filtered load of HCO3- resulting from the buffering of the volatile acid (CO2) load, increased availability of CO2 within tubular cells (due to hypercapnia) for combination with water, and stimulation of H+- and H+-K+-ATPases in tubular cells. This leads to increased H+ secretion and HCO3- reabsorption by the mechanism described in 3. above iii. this is the mechanism by which the kidney increases plasma [HCO3-] during hypoventilation and compensates for respiratory acidosis. The effect is greater during chronic than during acute respiratory acidosis (see Table 3) d. plasma chloride concentration (see Figure 3) i. there is an inverse relationship between plasma chloride concentration and the rate of HCO3- reabsorption ii. this may result from the requirement for electroneutrality during the reabsorption of sodium (Cl- and HCO3- are the two major anions available for reabsorption with sodium) iii. decreased plasma [Cl-] will lead to a decreased filtered load of Cl- and the tubules will reabsorb relatively more HCO3- with sodium for electroneutrality iv. increased plasma [Cl-] will lead to an increased filtered load of Cl- and the tubules will reabsorb relatively more Cl-with sodium for electroneutrality v. this effect comes into play in the pathophysiology of metabolic alkalosis in chronic vomiting of stomach contents. Vomiting causes ECFV and Cl- depletion so that relatively more HCO3- is reabsorbed by the kidneys along with sodium which is being avidly conserved to increase ECFV Figure 3:Potential effects of chloride and potassium depletion on acid base balance. From DiBartola SP: Fluid Therapy in Small Animal Practice, edition 2, WB Saunders Co, Philadelphia, 2000, page 234. e. plasma potassium concentration (see Figure 3) i. hyperkalemia is associated with decreased HCO3- reabsorption in the collecting ducts and hypokalemia is associated with increased HCO3reabsorption in the collecting ducts ii. these observations are consistent with competition between H+ and K+ for exchange with Na+ at the luminal membrane of the collecting duct cells, an exchange process which is responsive to the mineralocorticoid aldosterone iii. remember that for every H+ ion secreted into the tubular fluid, one HCO3- ion will be reabsorbed into the extracellular fluid iv. in hyperkalemia, potassium ions enter the cells from the extracellular fluid while H+ ions exit the cells and enter the extracellular fluid (see handout entitled, "Tubular Secretion and the Renal Handling of Potassium"). Thus, in the tubular cells of the collecting ducts, there are more K+ ions to be exchanged with Na+ ions at the luminal membrane, fewer H+ ions are secreted by this mechanism, fewer HCO3- ions are returned to the ECF, and more HCO3-ions remain in the urine v. an opposite sequence of events occurs in hypokalemia and probably contributes to the occurrence of "metabolic alkalosis with paradoxical aciduria" which is observed in animals with chronic vomiting of stomach contents that have ECFV, chloride, and potassium depletion. f. hormones i. mineralocorticoids and, to a lesser extent glucocorticoids, increase the rate of reabsorption of HCO3- in the collecting ducts by increasing the rate of H+ and K+ secretion in exchange for Na+ ii. as an example, hypoadrenocorticism (in which there is deficient production of steroids by the adrenal glands) is characterized by hyperkalemia and metabolic acidosis B. Replenishment of titrated HCO31. excretion of titratable acidity (see Figure 4) a. Sites: throughout the nephron (proximal tubule, distal tubule, collecting duct) but primarily important in the distal tubule and collecting ducts (after most of the filtered HCO3- has been reabsorbed as described above) b. Mechanism i. intracellular CO2 is combined with water by the action of carbonic anhydrase to form H2CO3 which immediately dissociates to H+ and HCO3- (see note B at end of handout) ii. the H+ is secreted into the tubular fluid as sodium enters the cell for electroneutrality and the secreted H+ titrates filtered HPO4-2 yielding H2PO4-1 (see note C at end of handout) iii. the HCO3- is reabsorbed into the peritubular fluid along with sodium for electroneutrality iv. note that this mechanism is responsible for the generation of a new HCO3- ion which aids in the replenishment of body HCO3- stores and for the net excretion of acid in the form of H2PO4-1 v. the term titratable acidity refers to the amount of strong base needed to titrate the acid urine back to a pH of 7.40 which in turn represents the amount of acid excreted in the urine as H2PO4-1 vi. approximately 40% (15-30 mEq) of the daily load of fixed acid is excreted by this mechanism c. factors affecting excretion of titratable acidity i. quantity of filtered phosphate reaching the distal tubule and collecting duct (A) a function of plasma phosphate concentration (B) affected by the fact that > 75% of filtered phosphate is reabsorbed by the tubules and not available for buffering the urine (C) relatively constant in the normal individual but increased in patients with hyperphosphatemia due to renal failure ii. pKa of phosphate buffer system and pH of tubular fluid (A) a buffer is most effective within the range of 1.0 pH unit on either side of its pKa (B) the pKa of the phosphate system is 6.8, the pH of glomerular filtrate 7.4, and that of the distal tubular fluid 6.0-7.0 thus phosphate is an effective buffer under these circumstances Figure 4: Regeneration of bicarbonate via titration of phosphate by secreted hydrogen ions in the renal tubul (titratable acidity). From DiBartola SP: Fluid Therapy in Small Animal Practice, edition 2, WB Saunders Co, Philadelphia, 2000, page 205. 2. excretion of NH4+ salts (see Fig 4) a. Sites i. the enzyme glutaminase deaminates glutamine to produce αketoglutarate and 2 NH4+ ions that are secreted in the proximal tubule (further metabolism of the α-ketoglutarate produces 2 new HCO3- ions that can be reabsorbed) ii. the concentration of NH4+ in the medullary interstitium is increased by countercurrent multiplication in the loop of Henle iii. nonionic diffusion of NH3 and trapping of NH4+ in the tubular fluid occurs in the collecting ducts Figure 5: Regeneration of bicarbonate by ammonium excretion in renal tubules (ammonium excretion). From DiBartola SP: Fluid Therapy in Small Animal Practice, edition 2, WB Saunders Co, Philadelphia, 2000, page 207. b. Mechanism i. ii. iii. iv. v. vi. vii. NH3 is non-ionized and lipid soluble and diffuses passively from the medullary intersititium and across the luminal membrane into the tubular fluid of the collecting duct (passive non-ionic diffusion) intracellular CO2 is combined with water by the action of carbonic anhydrase to form H2CO3 which immediately dissociates to H+ and HCO3the H+ is secreted into the tubular fluid of the collecting duct by means of H+- and H+-K+-ATPases in the luminal membranes of αintercalated cells of the collecting duct. the secreted H+ is immediately bound by NH3 in tubular fluid and converted to NH4+ which, being ionized, cannot diffuse back into the tubular cell. the HCO3- is reabsorbed into the peritubular fluid in exchange for Cl- at the basolateral membranes of the α-intercalated cells of the collecting ducts, Na+ filtered with the HCO3- is reabsorbed by the principal cells of the collecting ducts, and NH4+ is excreted in the urine as the SO4-2 or Cl- salt note that this mechanism is responsible for the generation of new HCO3- ions which aids in the replenishment of body HCO3- stores and for the net excretion of acid in the form of NH4+ salts at 9.2, the pKa of the NH3/NH4+ system is almost 2.5 pH units higher than that of the phosphate system (pKa 6.8) and about 3.0 pH units higher than a carnivore's urine pH of 6.0-6.5 thus essentially all of the H+ ions excreted by this mechanism are in the viii. form of NH4+ ions (i.e. the [NH4+]/[NH3] ratio is 1000:1 at urine pH 6.2) and large amounts of H+ ions can be excreted by this mechanism without additional lowering of urine pH (see Figure 6) more acid is excreted by the kidneys as NH4+ salts than as titratable acidity (approximately 60% or 25-50 mEq of the fixed acid load is excreted by this mechanism) and the NH4+ system plays the primary role in renal adaptation to chronic acidosis Figure 6: Explanation of how ammonium excretion allows removal of acid without affecting urine pH. From DiBartola SP: Fluid Therapy in Small Animal Practice, edition 2, WB Saunders Co, Philadelphia, 2000, page 207. c. Factors affecting NH4+ excretion i. the degree of urinary acidity (A) the more acidic the urine, the greater the amount of ammonia existing in the NH4+ form, the greater the concentration gradient for the passive diffusion of NH3 into the tubular fluid, and the more acid that can be excreted as NH4+ salts (B) there is a limit (pH = 4.4.) to how acidic the urine can become because the luminal H+- and H+-K+-ATPases in the collecting duct are inhibited by low pH and consequently cannot transport H+ ions against a concentration gradient of more than 1000 to 1 ii. severity and duration of acidosis (A) At any urine pH, the rate of NH4+ salt excretion is higher in the presence of acidosis (B) This is due to an adaptive increase in NH4+ production in the kidney that occurs as a result of stimulation of glutaminase during chronic acidosis (C) this mechanism is very adaptable and in chronic renal failure, NH4+ production increases on a per nephron basis by a factor of 4 to 5 fold iii. relative rates of flow of peritubular blood and tubular fluid (A) the flow rate of peritubular blood is much greater than that of tubular fluid and might be expected to act as a concentration sink for ammonia (B) When tubular fluid is acid, however, the trapping of ammonia as NH4+ in the tubular fluid prevents this from occurring REFERENCES 1. Valtin H: Renal Function: Mechanisms Preserving Fluid and Solute Balance in Health (ed 3), Little, Brown & Co, Boston, 1995. Chapters 9 (H+ Balance) & 10 (Role of Kidneys in Acid-Base Balance: Renal Excretion of H+ and HCO3-). 2. Koushanpour E & Kriz W: Renal Physiology: Principles, Structure, and Function (ed 2), Springer-Verlag, New York, 1986. Chapter 11. 3. Guyton AC: Textbook of Medical Physiology (edition 9), W.B. Saunders Co, Philadelphia, 1996. Chapter 30: Regulation of Acid Base Balance. 4. Rose BD: Clinical Physiology of Acid-Base and Electrolyte Disorders (ed 4) 1994. Chapters 10, 11 & 17. 5. Vander AJ: Renal Physiology (ed 5), McGraw-Hill, New York, 1995. Chapter 9: Renal Regulation of H+ Balance. Notes (A) H+ in aqueous solutions probably exist as hydronium ions (H 3O+) but for simplicity we will continue to talk about them as if they simply were protons (H+). (B) The reaction catalyzed by carbonic anhydrase probably is OH - + CO2 = HCO3- but for simplicity and ease of understanding we will continue to use the reaction: CO2 + H2O = H2CO3. In the former scheme, the secreted H+ comes from the dissociation of H2O. In the latter it comes from the dissociation of H2CO3. (C) Other compounds potentially contribute to titratable acidity including creatinine and organic anions such as ketones, citrate, and lactate. Their contribution however usually is minimal because of their normally low concentrations and low pKa values. Revised: January 16, 2002