Suicide Prevention in New Zealand
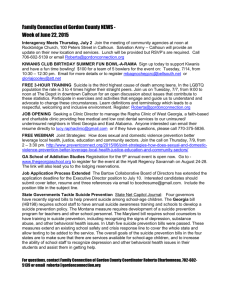
advertisement

Suicide Prevention in New Zealand A contemporary perspective: Social explanations for suicide in New Zealand Authors: Dr Sunny Collings, Departments of Psychological Medicine and Public Health, Wellington School of Medicine and Health Sciences, University of Otago, New Zealand and Associate Professor Annette Beautrais, Christchurch School of Medicine and Health Sciences, University of Otago, New Zealand Citation: Collings S and Beautrais A. 2005. Suicide Prevention in New Zealand: A contemporary perspective. Wellington: Ministry of Health. Published in May 2005 by the Ministry of Health PO Box 5013, Wellington, New Zealand ISBN 0-478-28373-3 (Book) ISBN 0-478-28374-1 (Internet) HP 4108 This document is available on the Ministry of Health’s website: http://www.moh.govt.nz/suicideprevention Preface Social explanations for suicide in New Zealand: utilising trend data to 1999 This paper is, in part, a summary of the suite of reports that the Ministry of Health commissioned from the Wellington School of Medicine and Health Sciences between 2001 and 2004. The suite of reports explores a range of possible social explanations, analyses and evidence about New Zealand’s suicide trends. Due to a three-year time lag in coroner statistics being available, most of the reports address suicide trends up to 1999. National Suicide Prevention Strategy The suite of reports aims to inform discussion on the New Zealand’s proposed national suicide prevention strategy: A Life Worth Living: New Zealand Suicide Prevention Strategy. Report no. Topic Author/s Title 1 Literature review (2002) Caroline Maskill Ian Hodges Velma McLellan Dr Sunny Collings Explaining Patterns of Suicide: A selective review of studies examining social, economic, cultural and other populationlevel influences 2 Review of routine data (2002) Stuart Ferguson Assc Prof Tony Blakely Bridget Allan Dr Sunny Collings Suicide Rates in New Zealand: Exploring associations with social and economic factors 3 Mäori (2004) Paul Hirini Dr Sunny Collings Whakamomori: He whakaaro, he korero noa. A collection of contemporary views on Mäori and suicide 4 New Zealand– Finland comparison (2003) Assc Prof Philippa Howden-Chapman Dr Simon Hales Dr Ralph Chapman Dr Ilmo Keskimaki The Impact of Economic Recession on Youth Suicide: A comparison of New Zealand and Finland 5 Data analysis from the New Zealand Census–Mortality Study (2004) Dr Sunny Collings Assc Prof Tony Blakely June Atkinson Jackie Fawcett Suicide Trends and Social Factors in New Zealand 1981–1999: Analyses from the New Zealand Census-Mortality Study 6 Summary of reports 1–5 (2004) Dr Sunny Collings Assc Prof Annette Beautrais Suicide Prevention in New Zealand: A contemporary perspective Suicide Prevention in New Zealand iii Authorship and Context of this Document The findings of the five reports are drawn together with other material in this sixth document, Suicide Prevention in New Zealand: A contemporary perspective, with the aim of describing the context for and interpreting the main findings of the supporting papers, using these materials and others to examine the contribution of social factors to suicide rates in New Zealand, and discussing the relevance of these to suicide prevention. This report is divided into sections, each of which has its own attribution of authorship, as follows: Executive Summary (Collings) Introduction (Collings) Suicide: A Recent Historical Context (Beautrais) Suicide: Contemporary Themes (Collings and Beautrais) Contemporary Approaches to Suicide Prevention (Collings and Beautrais) Social Interventions: Public Health, Social Epidemiology and Suicide (Collings) Social Epidemiology in Practice: Interpretation of the Supporting Papers (Collings) Suicide Prevention: What Do We Know About What is Effective? (Beautrais) Conclusion (Collings). Acknowledgements The peer reviewers for this paper are acknowledged with great thanks: Dr Joanne Baxter, Professor Robert D Goldney, and Dr Keren Skegg. Dr Sunny Collings had a project management and editorial oversight role for the whole project. She acknowledges the members of the Advisory Group with gratitude for their various contributions to the development of this challenging project, and for their critical review of the individual reports: Dr Rees Tapsell, Associate Professor Philippa Howden-Chapman, Dr Annette Beautrais, and Mr Don Smith. Disclaimer This report was prepared under contract to the New Zealand Ministry of Health. The copyright in this report is owned by the Crown and administered by the Ministry. The views of the authors do not necessarily represent the views or policy of the New Zealand Ministry of Health. The Ministry makes no warranty, express or implied, nor assumes any liability or responsibility for use of or reliance on the contents of this report. iv Suicide Prevention in New Zealand Contents Preface iii Authorship and Context of this Document iv Acknowledgements iv Disclaimer iv Executive Summary vii Overview of suite of suicide explanations Reports 1 to 5 Report 6 Introduction 1 Suicide in New Zealand Individual risk factor profiles through the life span International variations in suicide rates 1 2 7 9 Suicide: A Recent Historical Context 11 Sociocultural theories Psychoanalytic theories Philosophical theories Moral views of suicide 2 11 12 13 13 Suicide: Contemporary Themes 14 Conceptualising suicide: three theories Culture and ethnicity Learning from ethnic and cultural diversity Suicide among Mäori The issue of ‘youth’ 3 14 16 17 20 21 Contemporary Approaches to Suicide Prevention Mental health Injury prevention and restricted access to means of suicide Social interventions Debates about the best approach 4 vii viii Social Interventions: Public Health, Social Epidemiology and Suicide What is social epidemiology? Social epidemiology and the public health Social epidemiology, mental health and suicide Mental health, suicide and domains of influence 23 23 23 24 24 26 26 26 27 28 Suicide Prevention in New Zealand v Interactions between social factors at different levels Limitations to the application of social epidemiology to suicide and its prevention Cardiovascular disease and suicide: moving the population distribution of risk Targeting high-risk groups An integrated approach to suicide prevention An integrative conceptual model of risk and resilience 5 Social Epidemiology in Practice: Interpretation of Reports 1 to 5 1 Explaining patterns of suicide: a selective review of studies examining social, economic, cultural and other population-level influences 2 Suicide rates in New Zealand: exploring associations with social and economic factors 3 Whakamomori: He whakaaro, he korero noa: a collection of contemporary views on Mäori and suicide 4 The impact of economic recession on youth suicide: a comparison of New Zealand and Finland 5 Suicide trends and social factors: New Zealand 1981 to 1999: analyses from the New Zealand CensusMortality Study Conclusions 6 Suicide Prevention: What We Know Now about What is Effective Risk factors for suicidal behaviour Protective factors for suicidal behaviour Universal population-based programmes Selective programmes for high-risk sub-groups Other aspects of psychological intervention 7 Conclusion References 29 29 32 33 34 35 39 39 41 43 44 46 48 50 50 51 54 60 63 64 66 List of Tables Table 1: Table 2: Major causes of death for the New Zealand population, by sex, 1996 and 2000 Four-country comparison of the prevalence of mental disorder and suicide rates 7 27 List of Figures Figure 1: Age-standardised rates of suicide in New Zealand, by sex, 194899 2 Figure 2: Age-specific rates of suicide in the 1524-year-old age group, by sex, 194998 3 Figure 3: Age-specific rates of suicide in the 2544-year-old age group, by sex, 194998 4 Figure 4: Figure 5: Mäori suicide rate compared to non-Mäori suicide rate, 197899 Suicide rates in New Zealand, by age and sex, 2001 5 6 vi Suicide Prevention in New Zealand Executive Summary Suicide rates vary significantly between countries, between population groups within countries and across time. Factors such as differences in the ascertainment and reporting of deaths by suicide are unlikely to account for all these observed differences. Most recent research into the causes of suicide has focused at the level of the individual, in the domains of psychological theory, psychiatric epidemiology and behavioural genetics. Important advances in the understanding of individual cases of suicide have been made as a result of improved knowledge about individual-level risk factors such as mental illness, substance abuse and psychosocial disorders in youth. However, an in-depth understanding of what causes differences in suicide rates between countries and between population groups within countries has been limited by explanatory models that focus on such individual-level risk factors. Overview of suite of suicide explanations Reports 1 to 5 The broad consensus arising from the suite of reports for this project is that social factors are relevant to suicide. This is consistent with international opinion that suicide prevention cannot be left entirely to clinical interventions. However, it is not clear which social-level interventions (if any) will have a demonstrable an specific effect on suicide rates, either in the population as a whole, or in specific sub-populations. The linkages between macrosocial, cultural and macroeconomic factors and individual suicidal behaviours still remain unclear. Having said this, it is important to state that many social interventions need to be considered in their own right, independent of any potential effect on suicide rates. This is because some factors known to be linked to risk factors for suicide (such as substance abuse, child abuse and neglect) may be amenable to either targeted interventions or whole population initiatives. There are broader benefits to individuals and to society from interventions to improve social conditions, such as reducing high unemployment rates and economic disparities between population groups. A selective sociological review of the international literature (Report 1 in this suite of six reports) showed that although a range of characteristics of society are associated with suicide rates, it has been difficult to establish causal relationships. Examination of the available New Zealand data (Report 2) yielded the same conclusion. An original study comparing New Zealand’s and Finland’s responses to a global economic recession (Report 4) yielded evidence suggestive but not conclusive of differing impacts of economic conditions on male youth suicide rates, mediated through inequality. A qualitative study of the views of selected Mäori with expertise in the area of suicide (Report 3) on the key social contributors to suicide among Mäori was congruent with existing literature in emphasising social change and cultural alienation. Individual psychological risk factors were acknowledged, but were regarded as the mediating factors between broad social conditions and suicide. The importance of differentiating the effects of ethnicity bias, cultural characteristics and material deprivation was discussed. Suicide Prevention in New Zealand vii A quantitative study of the relationships between trends in New Zealand suicide rates and a range of indicators of socioeconomic position for the whole population, in four similar cohorts over a 20-year period (Report 5), revealed amongst other things that among men aged 2564 suicide trends varied by income, with the association of low income with suicide strengthening over time. An important proportion of the excess risk of suicide among Mäori men was shown to be due to socioeconomic factors. These five reports are summarised in further detail in Chapter Five of this paper. On the basis of these studies and the international literature it was not possible to make specific recommendations about social policies that could directly and demonstrably influence suicide rates in New Zealand. However, this work complements the existing evidence about suicide prevention initiatives focused on individual-level risk factors. Report 6 This final report in the project’s suite of papers (Report 6) reviews current knowledge about suicide prevention strategies that show effectiveness or promise of effectiveness. Although research into suicide has developed a relatively clear if by no means complete picture of the risk and protective factors that contribute to suicidal behaviours, less is known about translating this knowledge into effective prevention programmes. There is no single programme for suicide prevention that will achieve a significant reduction in suicide rates. However, despite some overly pessimistic views about the effectiveness of interventions, this final report concludes that there are a number of areas that show promise as programmes for suicide prevention. The approaches that stand out include: population-based programmes that address depression and alcohol use promoting mental health and problem-solving skills, in the community at large and in school students community-level suicide prevention programmes using the USAF model educational programmes for professionals such as GPs to enhance their ability to identify, treat and manage depressed and suicidal individuals programmes that integrate and enhance community and primary care psychotherapeutic and pharmacotherapeutic treatments for mood disorders and other mental illnesses linked with suicidality. Suicide prevention initiatives should continue to use interventions effective at targeting those known to be at risk, within the current preventive framework of selective and indicated interventions. This targeting of at-risk groups should occur in the context of approaches to social and economic policy development that take into account the possible effects on the mental health of vulnerable people. viii Suicide Prevention in New Zealand Given the difficulties of using deaths from suicide as the sole outcome measure for populationwide strategies, consideration should be given to monitoring other direct indicators of the mental health of the population, for example in the routine New Zealand Health Survey. It should also be recognised that the characteristics of society influence the physical, mental and social health status of individuals. This means that policy initiatives directed at features of society that are known to have an impact on one area of health may have the potential to influence other health domains including suicide. Suicide Prevention in New Zealand ix Introduction In the decade since the Public Health Commission recommended that the New Zealand government make a commitment to reduce deaths by suicide (Public Health Commission 1994), the reduction of suicide rates has become an explicit objective (Public Health Commission 1995; Ministry of Health 1998), with a particular focus on youth suicide (Ministry of Youth Affairs et al 1998). This project was commissioned in response to concern about the trends in New Zealand’s suicide rates, and sits alongside previous work exploring the importance of the broad social determinants of health (Howden-Chapman and Cram 1998; National Health Committee 1998). The Ministry of Health wished to gain a better understanding of how social factors may have influenced suicide rates in New Zealand over the past 30 years. In particular, they wanted to improve their understanding of factors contributing to suicide rates at the population level, so that potentially modifiable population-level factors could be identified. This project is part of the government’s cross-agency work towards expanding research and information systems to ensure suicide prevention activities can be advanced, where appropriate, and targeted for the best outcomes (Ministry of Health 2004). It makes an important contribution to the development of the New Zealand All-Ages Suicide Prevention Strategy. The task of the overall project was to identify possible social explanations for the comparatively high suicide rates in New Zealand and, where possible, to signal the potential for prevention. Of particular interest was the observation that although we have a clear understanding of risk factors for suicide at the level of the individual, it remains unclear why suicide rates vary so much between countries and between population groups within countries. The emergent discipline of social epidemiology offered a framework ideally suited to an enquiry of this type. The key feature of this approach is that it links epidemiological analysis of population-level associations and individual-level risk factors with sociological theory or evidence, to provide either testable hypotheses or a theoretically robust account of the links between the characteristics of a society and the health of the individuals in that society. Social factors that have been proposed as having links with suicide rates in New Zealand include changes in the levels and distribution of wealth, the impact of structural and social policies on Mäori, levels of social integration or fragmentation, the impact and pace of modernisation, media portrayal of suicide, changes in family structure, and a lessening of shared moral values. The time and resources available did not permit the undertaking of an original study to discover whether such factors could be said to ‘cause’ suicide in New Zealand. Indeed, even if resources were available, there are significant methodological barriers to generating timely findings from such a study. As a result, this project was restricted to the use of existing data and evidence already produced from other studies. Suicide Prevention in New Zealand 1 Suicide in New Zealand Suicide is an important cause of death in New Zealand. It is a significant cause of avoidable mortality between the ages of 15 and 44 (Ministry of Health 1999a), with suicide and selfinflicted injury causing more deaths than traffic accidents in 2000 (Ministry of Health 2004). Reducing the rate of suicides and suicide attempts is one of the 13 priority objectives in the New Zealand Health Strategy (Ministry of Health 2000). For the past 125 years suicide has also been considered an indicator of the mental health (Goldney 2004) and social health (Durkheim 1897; Hassan 1998; Eckersley and Dear 2002) of populations. More recently, suicide rates have been identified in an international comparative study as one of 21 indicators of the quality of health care, in part because suicide is considered to be an outcome of care that can be directly affected by health care policy or health care delivery systems (Hussey et al 2004). The economic costs of suicide and attempted suicide are substantial (Coggan 1995). Figure 1: Age-standardised rates of suicide in New Zealand, by sex, 194899 Suicide rate (per 100,000 population) 25 Males Females 20 15 10 5 0 1948 1952 1956 1960 1964 1968 1972 1976 1980 1984 1988 1992 1996 Note: Rates are standardised to the Segi world population. Source: Ferguson et al in press (Report 2 of Social Explanations for Suicide in New Zealand). In New Zealand total suicide rates rose from 1950 to 1998 (Beautrais 2003a), when they peaked, but they are now declining (see Figure 1). The rate of increase accelerated in the 1970s (Ministry of Health 2001; Ministry of Health 2004), largely because of a sudden increase in suicides among men aged 15–44 (Beautrais 2003a; Ferguson et al in press [Report 2 in this suite of reports]) (see Figures 2 and 3). A cohort effect was seen in men, with increasing risks of suicide in the young for successive birth cohorts born from 1957 onwards (Skegg 1991). 2 Suicide Prevention in New Zealand International comparison reveals that New Zealand’s all-age suicide rates are moderately high compared to rates in similar countries (Ministry of Health 2004), particularly among men aged 1544 years (Cantor 2000; de Leo et al 2001), but that they are mid-range in an overall international comparison (Lester 2003). Male and female youth suicide rates (ie, suicides among those aged between 15 and 24 years) are particularly high in comparison with similar OECD countries (Ministry of Health 2004). However, the suicide rate of young men has declined since its peak in the mid-1990s (Beautrais 2003a; Ministry of Health 2004) (see Figure 2). In contrast, the suicide rate has been rising for young women since the 1980s, and they now account for almost one-third of suicides in this age group (Beautrais 2003a) (see Figure 2). Figure 2: Age-specific rates of suicide in the 1524-year-old age group, by sex, 194998 Suicide rate (per 100,000 population) 45 40 Males Females 35 30 25 20 15 10 5 0 1949 1953 1957 1961 1965 1969 1973 1977 1981 1985 1989 1993 1997 Note: Rates used are three-year smoothed rates. Source: Ferguson et al (Report 2 in Social Explanations for Suicide in New Zealand). Suicide Prevention in New Zealand 3 Figure 3: Age-specific rates of suicide in the 2544-year-old age group, by sex, 194998 Suicide rate (per 100,000 population) 40 Males Females 35 30 25 20 15 10 5 0 1949 1953 1957 1961 1965 1969 1973 1977 1981 1985 1989 1993 1997 Note: Rates used are three-year smoothed rates. Source: Ferguson et al (Report 2 in Social Explanations for Suicide in New Zealand). Plots of suicide rates among men and women in the 4564 and 65-plus age groups show an overall fall in rates since the 1940s. The suicide rate among Mäori for both sexes combined was similar to the non-Mäori rate up until the mid-1990s, although the rate for Mäori women may well have been lower than for nonMäori women (Skegg 1995). After the mid-1990s the Mäori rate increased to greater than the non-Mäori rate. As with the general population, Mäori male suicide rates are consistently higher than the rates for females (see Figure 4). 4 Suicide Prevention in New Zealand Figure 4: Mäori suicide rate compared to non-Mäori suicide rate, 197899 Suicide rate (per 100,000 population) 24 22 Mäori suicide rate Non-Mäori suicide rate 20 18 16 14 12 10 8 6 4 2 0 1978 1980 1982 1984 1986 1988 1990 1992 1994 1996 1998 Notes: Rates are standardised to the Segi world population. The Mäori and non-Mäori rates are adjusted for misclassification of Mäori deaths (also known as numeratordenominator bias) based on findings from New Zealand CensusMortality Study). Source: Ferguson et al (Report 2 in Social Explanations for Suicide in New Zealand). The most recent figures available at the time of writing show a small increase for Mäori women, non-Mäori women and non-Mäori men between the ages of 15 and 24 between 2000 and 2001 (Ministry of Health 2004). It can be seen from Figure 5 that suicide remains predominantly a male problem, with men aged between 20 and 45 having the highest rates and with a further peak in rates for men in late life. Suicide Prevention in New Zealand 5 Figure 5: Suicide rates in New Zealand, by age and sex, 2001 Suicide rate (per 100,000 population) 45 42.8 Males Females 40 35.8 34.4 35 31.2 33.5 30.9 29.9 30 27.0 25 20.5 20.3 18.9 20 17.4 17.0 15.3 15 13.9 12.8 12.3 9.5 10 7.8 7.9 7.6 6.6 6.8 7.3 5.7 4.2 5 0.6 4.5 4.7 5.5 1.4 0.0 0 10–14 15–19 20–24 25–29 30–34 35–39 40–44 45–49 50–54 55–59 60–64 65–69 70–74 75–79 80–84 85+ Age group (years) Source: New Zealand Health Information Service Suicide is usually considered in terms of differences in rates for different subgroups of the population. However, it is also important to note the proportion of deaths attributable to suicide in these subpopulations. In New Zealand, among men aged between 20 and 35 years, suicide accounts for one-third of all-cause mortality (Beautrais 2003a). Overall, suicide is a significant cause of death for men of all ages in New Zealand, as shown in Table 1. 6 Suicide Prevention in New Zealand Table 1: Major causes of death for the New Zealand population, by sex, 1996 and 2000 Rate (per 100,000 population) Males Females 1996 2000 1996 2000 185.0 143.8 90.6 74.3 Stroke 50.9 45.2 46.8 41.6 All other cardiovascular diseases 38.4 32.0 30.0 25.4 – 0.1 28.5 23.9 Lung cancer 43.6 37.6 20.2 20.0 Chronic obstructive lung disease 45.8 35.9 22.8 19.7 Colorectal cancer 28.8 25.0 20.8 19.0 Diabetes 15.0 18.0 10.5 12.3 Dementia 7.6 8.2 9.0 7.3 Motor vehicle accident 20.6 16.0 8.1 7.1 Aortic aneurysm 11.1 10.5 6.5 4.7 Suicide 23.7 20.9 6.1 4.3 Stomach cancer 8.6 8.1 4.5 4.1 Prostate cancer 23.9 25.2 – – All other causes 251.9 203.0 163.8 141.5 Ischaemic heart disease Breast cancer Source: Ministry of Health 2004 Individual risk factor profiles through the life span A significant amount of research has identified the individual-level risk factor profiles distinguishing those who attempt or die by suicide from those who do not. These risk factor profiles vary across the age span. New Zealand research has consistently demonstrated patterns of risk factors commonly seen in young people who die by suicide, including: disturbed or unhappy family background educational and social disadvantage mental health or behavioural problems, including mood disorders, substance abuse, individual vulnerabilities such as impulsiveness and poor problem-solving abilities a stressful life event prior to the suicidal act, such as relationship break-up, court appearance or family crisis (Beautrais 2000). Importantly, many young people who are depressed are not suicidal, but the addition of the social risk factors described above to pre-existing depression adds significant extra risk (Fergusson et al 2003). Suicide Prevention in New Zealand 7 As people mature into adulthood, the risk factor profile changes so that the contribution of current mental illnesses such as depression and non-affective psychosis becomes more prominent, and distant antecedent factors such as childhood adversity become relatively less important (Ministry of Health 2004). However, it may be that early experiences of adversity do confer additional risk for mood disorders and associated suicidality in adulthood (Mullen et al 1993; Beautrais 2002). For mid-age and older adults, current mental illness is more strongly associated with suicide attempts than for those under the age of 30 years (Beautrais et al 1996). Among older people, serious and chronic physical illness is relevant (Waern et al 2002, 2003), but current mental illness is still the single most important risk factor (Harwood and Jacoby 2000; de Leo et al 2001). In all age groups, social isolation confers additional risk, and negative life events may act as immediate precipitants in those already at risk (Beautrais 2003b). Mäori The state of knowledge about the causes of suicide among Mäori has developed differently to that in relation to suicide among non-Mäori. In contrast to the dominant discourse on suicide among non-Mäori there is a focus on social factors, especially those in the ‘cultural’ domain, such as past and current colonisation effects, and loss of traditional social structures and processes. However, although the fact of the colonisation of Māori is inarguable, it is much less clear how processes such as ‘acculturative stress’ or the state of ‘cultural alienation’ or ‘cultural affiliation’, all of which are commonly used terms, might relate to suicidal behaviour at the individual level. This is not to say these things are not important, or even critical, in the generation of risk of suicide in some Mäori, but that the links between these high-level constructs and the individual behaviour that leads to death have not been well established. Unfortunately, in regard to individual risk factors there is no published research that rigorously compares the profiles of Mäori and non-Mäori. Neither is there robust research that examines risk and protective factor profiles among Mäori with the same explanatory power as has been used in studies of the wider population. While there is no reason to suspect that the core risk factors would differ in major ways from those described above, because there is agreement on what these are among international studies (Hawton and van Heeringen 2000) and in relation to Mäori (Bridgeman 1997), the influence of cultural and other social factors is important (Skegg 1997; Lawson-Te Aho 1998). Thus for some Mäori there may be a different pattern of vulnerabilities: (a) because additional factors may have an influence (such as ethnic bias in daily living) (b) because the risk factors (such as material deprivation) that are not unique to Mäori may have a different pattern of impact on Mäori compared with non-Mäori. There is evidence of this in the ethnic patterning of other causes of death in New Zealand (Ajwani et al 2003). 8 Suicide Prevention in New Zealand The nature of the interaction between higher-order social factors and factors at the individual level is not well understood, but it has been observed that the current dominant explanatory paradigm for suicide has not considered cultural issues for indigenous peoples to be a core domain of concern. Rather, cultural and historical processes such as colonisation and assimilation have been regarded as ‘additional’ risk factors. One view is that the links between risk factors in the mental illness and cultural domains cannot be understood adequately unless the cultural domain is considered as the foundation (Lawson-Te Aho 1998). An alternative to this is the proposition that what is meant by ‘cultural factors’ needs to be teased out for further investigation if it is to be meaningful. Culture is, after all, not only related to our ethnicity but also to our gender, our age and our upbringing. There are also potential dangers in invoking a general ‘cultural’ risk factor for Māori suicide. Firstly, and in common with risk factor thinking in general, potential protective factors may be overlooked. Secondly, implicit in the model of cultural risk as most commonly applied at present is the assumption of cultural homogeneity among Māori, whereas Māori are a diverse group, both culturally (Durie 2001) and ethnically (Robson 2000). International variations in suicide rates The patterns of suicide rates in population subgroups within countries vary markedly between countries. Over the past decade there has been a move to study more or less culturally homogeneous groups of countries in the hope that any observable patterns might provide some insights into the possible reasons for such variation (Cantor 2000). A brief descriptive example of such inter-country variation is afforded by the stratification by age and gender reported by Cantor (2000). Striking rises in suicide rates among men aged between 15 and 24 occurred between 1960 and 1990 in many countries with general cultural attributes similar to those of New Zealand (some Western European and Scandinavian countries and Australia, Canada and the USA), although the most rapid rises have not occurred at exactly the same time. At the other extreme of age, suicide rates among men over the age of 75 have decreased in New Zealand, Australia and the USA over the same period, but increased in all Scandinavian countries. Another example is seen in the East Asian countries. A comparison of suicide trends in Taiwan, Hong Kong and Beijing (Yip 1996) revealed that all-age suicide rates in Taiwan and Beijing decreased between 1981 and 1994 but increased in Hong Kong. Different sociopolitical environments have been postulated as being relevant to this within-group variation (Yip 1996; Cheng and Lee 2000). These pattern variations within groups of arguably similar countries can be compared with different pattern variations between groups of countries with distinctly different cultural, political and economic characteristics. Using the previous country groupings as an example, the suicide rates are much higher among the elderly in places such as Hong Kong, Taiwan and Beijing than among the elderly of Western countries, but Hong Kong and Singapore have not witnessed the steep rise in suicides among 1524-year-olds that many Western countries have seen in recent decades (Cheng and Lee 2000). Suicide Prevention in New Zealand 9 We need to be cautious when comparing countries because of local differences in ascertainment and reporting of deaths by suicide. There may also be differences in rates of individual-level risk factors, such as mental illness and access to effective treatments. However, such factors are unlikely to account for all the observed differences in rates, and in patterns of changes in rates over time. This is a key issue for increasing our understanding of the causation of suicide. Finding robust causal explanations for differences in suicide rates among population subgroups within a country, between countries and across time is extremely challenging, but such explanations have the potential to shape our thinking about suicide prevention. These explanations are unlikely to be revealed by research programmes that focus on a narrow range of factors without reference to the broader picture of what is known about suicide, just as unidimensional approaches to prevention are unlikely to be successful (Bertolote et al 2003). 10 Suicide Prevention in New Zealand 1 Suicide: A Recent Historical Context In the last two decades the volume of international research into suicide has increased exponentially. Much of this research has been developed in an empirical framework in which investigators have examined the role of likely causes and risk factors for suicidal behaviour. In contrast to this approach, suicide research in earlier times centred on a number of theoretical models. A large literature on suicide was produced in Europe in the 18th and 19th centuries, acknowledging both social and psychological factors (Goldney 2000). To provide a background for understanding current approaches to suicide research and prevention, this chapter provides a brief overview of the dominant theories and approaches to suicide research during the past 100 years. The explanatory models of suicide developed over the past century may be broadly classified as sociocultural, psychoanalytic and philosophical theories. Sociocultural theories Although accounts of suicide date from Greek and Roman times, the most well-known contemporary approach to the study of suicide began little more than a century ago with the publication of Durkheim’s Le Suicide (1897). Durkheim attempted to explain suicide rates in terms of social conditions, and argued that the incidence of suicide varies with the extent of social integration within a given society. He described four types of suicide that he thought could be related to the degree of social integration and social regulation within a society. These, along with a brief explanation, are as follows. i. Altruistic suicide. Durkheim (preceded by George Savage [Goldney 2001]) suggested that an altruistic suicide occurs when individuals view the society of which they are a part as more important than themselves, and kill themselves as a matter of honour, moral duty or self-sacrifice. This type of suicide would appear to be particularly a feature of Asian suicides. The custom of hari-kari in Japan, for example, involving ritual suicide upon dishonour may be regarded as altruistic suicide, where societal traditions and expectations shape individual suicidal behaviour. In a similar manner, cultural expectations govern the Indian custom of suttee, in which a widow is expected to throw herself on her husband’s funeral pyre and die by immolation, thereby affording prestige to her and her husband’s family and good fortune to those present, in the course of joining her husband in paradise. It is worth noting that the tradition of martyrdom by suicide is still relevant in some contemporary cultures, with the rise of the suicide bomber in relation to the Middle Eastern crises being of particular interest. ii. Egoistic suicide. Durkheim proposed that, in contrast to altruistic suicide, there is a type of suicide that may be characterised as ‘egoistic’ (this idea was also proposed earlier by Savage [Goldney 2001]), which typically occurs when an individual is alienated from society, has poor social linkages and support, and is not influenced by societal expectations. Most suicides that occur in the context of a depressive illness could be regarded as examples of egoistic suicide. Suicide Prevention in New Zealand 11 iii. Anomic suicide. Durkheim described ‘anomic’ suicides as those that tend to occur among individuals who are insufficiently regulated by society. They may have suffered recent and sudden life difficulties or stresses that disrupt or sever their links with society. Suicides that occur following financial loss, being made redundant, or marital separation could be examples of anomic suicide. iv. Fatalistic suicide. As a footnote, Durkheim added a fourth category, ‘fatalistic’ suicide, which he applied to those suicides that occur when an individual feels he has no control over his life. Examples of fatalistic suicide include the suicide of a prisoner or of someone diagnosed with a terminal illness. Subsequent work by a series of sociologists extended Durkheim’s sociocultural theory of suicide to include the effects of particular social variables on suicide. Henry and Short (1954), for example, confirmed Durkheim’s findings on the correlation between suicide rates and economic cycles, but extended his theory to incorporate a theoretical construct of aggressive behaviour. These authors argue that an individual’s tendency to blame external societal sources for problems is likely to result in externally directed aggressive behaviour, whereas a tendency to blame internal factors leads to internally directed aggression that is more likely to result in suicidal behaviour. Durkheim’s original theory was further extended by Gibbs and Martin (1964), who hypothesised that the extent of an individual’s ‘status integration’ in society determines his or her tendency to suicidal behaviour. Gibbs and Martin argue that a society in which individuals are well integrated in their societal roles is likely to have a lower suicide rate. There have been further attempts to refine this aspect of Durkheim’s theory, with suggestions, for example, that suicide is related not so much to social status as to the loss of such status (Breed 1963; Maris 1975), or that it is related to relative misery compared to one’s peers (Barber 2001). A more extensive review of sociological theories of suicide may be found in Report 1 in this suite of reports, Explaining Patterns of Suicide: A selective review of studies examining social, economic, cultural and other population-level influences (Maskill et al in press). Psychoanalytic theories Psychological and psychoanalytic theories of suicide were developed in the last part of the 19th and first half of the 20th century. These theories challenge the sociocultural basis of Durkheimian theory, and instead argue that suicidal behaviour arises from individual and intrapsychic sources that are essentially invulnerable to social forces. Using psychoanalytic terminology, Freud (1917) described suicide as a behaviour arising from an unconscious wish to kill an introjected love object (ie, one who has been internalised as part of one’s own ego). Psychoanalytic theory contends that every individual has the potential for suicidal behaviour, with this potential shaped by childhood experiences. The American psychoanalyst Menninger (1938) expanded the Freudian model of suicide, hypothesising that all suicides involve three fundamental dimensions: hate, depression and guilt. He suggested that suicide, therefore, involves ‘a wish to kill’, ‘a wish to die’ and ‘a wish to be killed’. Menninger described suicide as ‘murder in the 180th degree’. 12 Suicide Prevention in New Zealand These original psychoanalytic theories of suicide have been extended by others including, for example, Zilboorg (1939), who suggested that suicide results from an individual’s unconscious identification with someone who has died and their wish to be reunited with that person. Object relations theorists have suggested that suicide results from a failure to negotiate the transition from the symbiotic attachment to the mother to the separation or individuation phase. Other schools of psychotherapy have contributed a range of variations on these themes. For example, interpersonal theorists have stressed the contribution of an individual’s sociocultural environment to determining the tendency to suicidal behaviour. Philosophical theories A third contemporary approach to explaining suicide has been the philosophical or existential. Camus began The Myth of Sisyphus by stating: ‘There is but one truly serious philosophical problem and that is suicide’ (Camus 1940). The moral issues surrounding suicide have been a major focus for a series of philosophers including Hume (1783), Sartre (1956), Kant (1909), Nietzsche (1989), Heidegger (1962) and Wittgenstein (1953), with the latter claiming that ‘the main ethical issue for man is suicide’. Existential issues have centred on explaining, as Camus suggested, ‘the apparent absurdity, meaninglessness and despair of life’. Moral views of suicide Parallel to theories of suicide there have been various moral positions about the desirability or undesirability of suicide. These positions date from the classical Greek and Roman philosophers, who maintained a permissive view of suicide, encouraging suicide in particular circumstances including ill health, insanity or poverty. In contrast to this liberal approach, the religiophilosophical view has been increasingly negative. Originally, the early Christian church was divided about the issue of suicide the tradition of martyrdom, in fact, encouraged suicide. From the early fifth century, however, Augustine’s interpretation of the sixth commandment and the subsequent linkage of suicide with crime and with sin introduced a Christian prohibition against suicide. Since then the Church has maintained that suicide is morally wrong, with this view continuing to the present time. Within the last two decades medical advances that permit assisted suicide, and the emergence of patient advocacy interests, have reopened philosophical discussions of suicide, assisted suicide, ‘right to life’ arguments and euthanasia. Suicide Prevention in New Zealand 13 2 Suicide: Contemporary Themes It is clear that the way suicide is conceptualised by societies is shaped by their prevailing shared spiritual, cultural and scientific beliefs. Scientific and medical enquiry is also shaped by social forces. The paradigms within which scientific and medical researchers develop their work are influenced by social and political systems (Hollis 1994: 86) and by the shared beliefs of the scientific community itself about what kinds of research questions, methods and knowledge are of value (Mulkay 1991; Hollis 1994:86; Martin 2004; Dean 2004). Furthermore, the statistical methods and other technologies available to make discoveries related to the causation and prevention of illness are applied in ways that are determined by these contextual factors (Dean 2004). This environment in turn shapes the development of new technologies. Two dominant characteristics of the development of Western societies in the past century are pertinent to an understanding of the contemporary Western conceptualisation of suicide and its causation and prevention. One is the centrality of the individual (Eckersley and Dear 2002); the other is a model of the production of health and the prevention of disease based on a ‘bottom-up’ focus on the cellular and molecular mechanisms of disease. While this approach has been enormously fruitful, it has had its critics, its application in public health being criticised as merely being ‘biophysiological reductionism’ (McKinlay 1994, cited in Pearce 1996), or the ‘atomistic fallacy’ (Marmot 1998). This context can contribute to our understanding of the three most notable contributions to the dominant Western conceptualisation of suicide in the latter half of the 20th century. Conceptualising suicide: three theories Psychological theories The first of these came from Shneidman (1985), who developed a psychological theory of the aetiology of suicide. Shneidman suggested that all suicides tend to share 10 common psychological features, which have become known as the 10 ‘commonalities’ of suicide: seeking a solution to life problems by suicide wanting to stop mental pain and anguish suffering intolerable psychological pain frustration at not having some of life’s basic needs met hopelessness about life and the future, and feeling helpless to do anything about it ambivalence about dying constricted, limited options wanting to leave a painful life communicating suicidal intent lifelong poor coping patterns that tend to be self-destructive. Overall, Shneidman regarded ‘psychological pain’ or ‘psychache’ as the single key common feature of all suicides. He believed that suicide is the human response to extreme psychological pain, and that suicide prevention should focus on meeting the emotional needs of suicidal individuals. 14 Suicide Prevention in New Zealand Psychiatric epidemiology A second major recent contribution to knowledge about suicide has come from research conducted in the field of psychiatric epidemiology. This research has tended to explain suicide almost exclusively in terms of observed associations between a range of psychobiological risk factors and suicidal behaviour. In this respect, suicide research within the last few decades has followed trends in psychiatric epidemiology that have focused on the development of statistical models of individual-level risk and resilience. The major finding from psychiatric epidemiological research is the central role that current psychiatric status plays in determining suicide risk, with estimates suggesting that up to 90% of suicides can be attributed to a series of common mental disorders that span mood disorders, substance use disorders, anxiety disorders, antisocial and conduct disorders, and less common disorders such as bipolar disorder and non-affective psychosis. These studies have consistently shown that the relative contributions of social and economic factors, at the individual level, to the suicide risk of individuals are smaller than the contribution of mental illness. Neurobiology and behavioural genetics A third line of research that is likely to assume an increasing importance in the explanation of suicidal behaviours has been provided by work on biological substrates such as the serotonergic system, and in particular by recent work in behavioural genetics. There is growing evidence from twin studies to suggest the genetic heritability of suicidal behaviour (Statham et al 1998). Furthermore, recent studies have identified a number of genetic and biological factors associated with suicidal behaviours (Mann et al 2001). Although this research is still in its infancy, it suggests that suicidal behaviours are not simply a response to environmental adversity but also reflect individual genetically determined vulnerabilities to these behaviours. This strand of research is clearly linked to advances in technology. These three major contributions to our understanding of the aetiology of suicide are all, to a large extent, located at the level of the individual. The importance of the work exploring this domain of influence cannot be underestimated. It has without any doubt generated strong evidence that individual-level risk factors are of the utmost importance in the generation of suicidal behaviour in individuals. Nevertheless, it should be noted that the assumption that the individual level is most relevant to the causation of suicide is consistent with the current dominant paradigm of the production of health and the prevention of disease, which is that the most important risk factors are those that have direct effects at the level of the individual. This means that research questions about prevention have been shaped around risk and protective factors and interactions between them that occur at the level of the individual. While this approach has made an enormous contribution to our understanding of the suicidal behaviour of individuals (ie, cases of suicide), it has not significantly improved our understanding of suicide rates and the reasons why rates vary between countries and subpopulations within countries. This focus on one aspect of the phenomenon of suicide has the potential to overlook other types of influences on suicidal behaviour. Suicide Prevention in New Zealand 15 The best explanation is likely to derive from several types of enquiry. To use an example from social psychiatry, a stress-vulnerability model of the aetiology of mental illness is not incompatible with a biological model (Rogers and Pilgrim 2003). Of course, the prevention or treatment of a mental illness might be most effectively carried out by integrating knowledge derived from several perspectives, and likewise in the case of suicide. Culture and ethnicity Another critical domain of thinking about suicide is culture. As a concept this is often conflated with ethnicity because often members of a distinct ethnic group share a common culture. However, shared cultures exist in groups other than those defined by ethnicity, and there can be considerable cultural diversity within an ethnic group. It has been argued that more can be learnt about suicide by considering it from a cultural perspective than by exploring patterns of suicide by social structure (Makinen, in Bille-Brahe 2000), which is the thrust of Durkheim’s work and much of the research still conducted. This is because culture, which is a product of people living together and creating a ‘conglomeration of ideas, habits, thoughts, traditions, norms and values that manifests as a … pattern in specific group of people’ (Bille-Brahe 2000:198) powerfully shapes and constrains the behaviour of the individuals in the group, in ways the structural aspects of society may not do. Thus, just as the structural elements of a society set up particular conditions for the existence of subgroups of the population (Rogers and Pilgrim 2003), cultural currents also influence people’s choices and decisions for action. In New Zealand the cultural perspective has a prominent place among suicide prevention initiatives (Ministry of Youth Affairs et al 1998), but elements of the thinking about this are underpinned by ethnicity (eg, the use of ethnicity statistics). New Zealand shares with other countries (including Australia and Canada) the fact that the same groups (most notably young men) among the indigenous population are at particularly high risk of suicide. Some countries have other significant cultural or ethnic minorities whose suicide risk profiles differ from those of the general population. In New Zealand such groups include Pacific peoples and people of East Asian origin. Suicide among these groups in New Zealand is difficult to study at a population level because the numbers are statistically small (Ministry of Health 2001; see also Report 2 in this suite of reports, Ferguson et al in press). This project, Social Explanations for Suicide in New Zealand, considers only comparisons between non-Mäori and Mäori, who are the indigenous people of New Zealand and who make up 14.3% of the New Zealand population (Statistics New Zealand 2002). 16 Suicide Prevention in New Zealand Mäori youth are more at risk of suicide than non-Mäori youth of the same sex, with young Mäori males having the highest rate (Ministry of Health 2004). However, it is difficult to interpret long-term trends in the rates of suicide deaths among Mäori because of inaccuracies and inconsistencies in ethnicity classification generated by the census prior to 1986 (affecting the denominator) and improvements to the definition of ‘Mäori’ used in ethnicity coding for births and deaths that occurred in 1995 (affecting the numerator) (Statistics New Zealand 1996). Part of the technical work of the New Zealand Census Mortality Study has been to generate rates for causes of death by ethnicity that more accurately reflect the real picture (Ajwani et al 2002, 2003). This means that the ethnic trends in suicide rates described in Report 5 in this project suite of reports (Collings et al in press) are the most accurate available. Learning from ethnic and cultural diversity Comparison across cultural and ethnic groups must always be done with caution. It is inevitable that one group will become the comparator, either explicitly or implicitly, and it is then challenging not to consider one group as the ‘norm’ against which others are to be compared. Nevertheless, we consider that some degree of comparison between cultures can make an important contribution to an understanding of suicidal behaviour. The important question to ask when considering the examples of other cultural or ethnic groups is: What can be learnt from this example that could inform our thinking about – in this case Mäori?’, rather than simply, What is different? or What is the same? If our understanding of suicide in Mäori is to be informed by studying suicide in other ethnic or cultural groups, a full understanding of similarities and differences across social, economic, historical and cultural contexts in both Mäori and other ethnic groups is required. For example, Mäori are often considered alongside other indigenous peoples who have experienced colonisation because of similarities in experiences of colonisation, including becoming a minority ethnic group within their own countries, and relative social and economic inequalities with dominant majority populations. With regard to cultural practices in common with other countries, Mäori culture shares some feature in common with other Pacific cultures (King 2003). Therefore, just as cross-country comparisons are informative about suicide rates for the whole population, they can also be useful for increasing our understanding of suicide among Mäori in New Zealand. Two examples are given below. Western Samoa Beginning close to home, there are few published studies of suicide among Pacific Island populations living in their country of origin. However, one such study was reported by Bowles (1995). This is an account of an ‘epidemic’ of suicides in Western Samoa, a small country with (at that time) a relatively homogeneous, traditionally structured society. Suicide was held to be rare in traditional Samoan society, but in 1981 the suicide rate in Western Samoa peaked at 31.3 per 100,000, high by international comparison. It had been increasing marginally since 1965, but from 1975 there was a steep increase, mainly due to an increase in the incidence of paraquat self-poisoning by people under the age of 30. The highly toxic herbicide paraquat was imported into Western Samoa in 1972, and the first deaths from paraquat poisoning occurred in 1973. Suicide Prevention in New Zealand 17 For most cases, information about preceding events was available from family, allowing what the author described as a ‘primitive’ psychological autopsy. The precipitating factor was commonly a critical and rejecting response from a person in authority following a breach of the accepted code of behaviour. In terms of the social context, attempted suicide by self-poisoning with low toxicity substances had already become more common among people under the age of 30, often in association with the binge drinking of alcohol. These suicide attempts occurred in the absence of mental illness but against a background of dysphoria thought to be related to social factors particularly affecting this age group, including powerlessness, hopelessness and a sense of frustration about selfdetermination. In traditional Western Samoan society only a few gain high social status through the Matai system, but an additional opportunity to increase social status had become available to some in this age group: out-migration to countries such as New Zealand, Australia and the US. For young adults in Samoa this represented a path to a better life and to increased status within the family or village, due to the ability to send money home. From 1976 to 1981 there was a loss of 28% of the people aged between 15 and 24 years, with similar losses over adjacent census periods. These are huge and highly disruptive losses for a small, close-knit society. Family and village expectations of young people to migrate rose at least temporarily at a time when recipient countries began to impose immigration controls, making this more difficult achieve. This led to a sense of failure and guilt among those who remained behind. A reduction in the availability of the lethal means, a reduction in its lethality by the addition of an emetic and a local campaign to raise awareness of the lethality of paraquat coincided with a reduction in these self-poisonings. Also coinciding with the reduction in rates was the hosting of the South Pacific Games by Western Samoa, which generated a powerful but temporary sense of shared national identity. The author does not claim a specific effect on rate reduction from any one of these factors. This example does, however, illustrate the complexity of the possible interactions of cultural practices and beliefs, social, psychological and environmental factors from the level of society to the level of the individual in the causal pathway to suicide. A number of hypotheses can be generated to explain the observations. For example, because of a health selection effect, those who remained behind were more at risk of mental illness and therefore to suicide. A health selection effect could operate in several ways. At a social or regulatory level only the very healthy may have been permitted to migrate. Alternatively, only the most psychologically robust and adaptable may have chosen to leave. However, there was no evidence of mental illness among those who died by suicide, and such selection does not on its own explain the sudden increase in numbers (rather than rate) of suicides, as such people would have been in the population prior to the out-migration. Perhaps a collective sense of hopelessness pervaded the group who remained, people who would otherwise have been regarded as being in their prime period for making a contribution to society but who considered themselves to be failures. 18 Suicide Prevention in New Zealand Another possible explanation is the increase in alcohol consumption among those remaining, possibly related to the sense of purposelessness but providing a new context for social interaction. The resulting disinhibition would have increased the likelihood of impulsive suicide attempts. The increased stress of having to carry out the functions of able-bodied adults to support and sustain the community, with much reduced numbers to do so, might be another explanation. Those charged with trying to stem the increasing incidence of suicide could not unravel the web of ‘causes’ and then intervene. What occurred was a practical response; namely, reducing the lethality of the immediate proximal risk factor – the paraquat. Fortuitously there was also a supply problem, which reduced public access to the poison. It is clear that there were individuallevel and social-level influences on the suicidal behaviour, but that the most immediate available means of reducing the number of deaths was a public health response, by reducing access to the means of suicide. This approach, probably without exception, has the immediate effect of reducing suicide rates, although the effect on rates in the long term is less certain because of substitution with other methods (Appleby 2000). Australian Aboriginals A different kind of comparative example is offered by the Aboriginal people of Australia, where suicide rates among young men are very high compared to non-Aboriginal men of comparable age (Baume et al 1998; National Health and Medical Research Council and the Mental Health Branch 1999). This has been said to be due to the disruption of their cultural and social institutions, meaning that the capacity to regulate and reproduce social life has been destroyed, causing increased rates of substance use and mental illness (Singh and Judd 1995), which increase the risk of suicide. Young Aboriginal men are also at greater risk of using more lethal methods such as hanging. In a comparative study of methods of suicide among 950 males in Queensland between 1994 and 1996, Aboriginal males accounted for 9% of the suicides but 19% of the deaths by hanging (RR = 7.7; 6.09.6). Furthermore, 12% of deaths by hanging among Aboriginal men occurred in prison compared to 4% of such deaths for non-Aboriginal men (de Leo et al 2002). In simplistic terms this might be explained by a lack of access to other means, but non-Aboriginal men in prison would also have lack of access to other means. It has therefore been suggested that for Aboriginal males, hanging may have come to be an ‘acceptable’ method of suicide, having been established as a social norm (Hunter et al 1999). This example illustrates the fact that it is not just cultural change that can affect individuals, but also the nature of the modified cultural practices that arise. Aboriginal culture has adapted to its new conditions, and in doing so new norms of behaviour towards others and expectations of kinship groups and for the future have been established. Young Aboriginal men appear to be particularly vulnerable to the effects of this, perhaps because women are more protected by kinship with their children a relationship from which many young men are excluded. Suicide Prevention in New Zealand 19 These two examples demonstrate that the complexity of factors surrounding the causation of suicide for Mäori, and young Mäori men in particular, is to be expected. These complexities are also seen in relation to suicide in the indigenous populations in other post-colonial New World countries, including Canada and the USA. Although in each case there will be unique local factors (as in the examples above), there is a clear pattern, especially for youth, of association between multiple general risk factors (such as depression, substance abuse, disturbed family backgrounds and poor problem solving abilities), which may in turn arise from what has been called cultural disintegration (Lawson-Te Aho 1998). Suicide among Mäori Suicide among Mäori is challenging to study at the population level because the numbers are too small for in-depth statistical analyses (eg, by multiple subgroups such as sex and age). In Report 5 in this suite of reports, Suicide Trends and Social Factors: New Zealand 1981 to 1999: Analyses from the New Zealand Census Mortality Study, Collings et al show some of the difficulties in elucidating cause and effect (among social factors) for Mäori suicide even when considering only one domain of social factors socioeconomic factors. Several strands of action are required to improve our knowledge. Firstly, we need methodologically rigorous studies of Mäori suicide using the models that have served our knowledge of suicide among non-Mäori so well. Such methods include the psychological autopsy as part of a case-control design, which is a powerful tool for investigating rare outcomes. Where population-based studies are done, researchers need to ensure that sample sizes of Mäori are sufficient to answer questions about Mäori outcomes with sufficient explanatory power. Secondly, other methods that have the potential to contribute to our understanding of suicide among Mäori should not be overlooked. These include qualitative studies and the judicious use of cross-cultural comparison, such as that by Lawson-Te Aho (1998). Thirdly, social epidemiology provides an important avenue for exploring broader social impacts on Māori health and mental health; for example, it allows powerful exploration of ethnic disparity, which has the potential to increase our understanding of the effects of perceived discrimination. Finally, just as with other suicide research, much could be gained by exploring resilience in both individual and cultural domains, and by studying those who make serious suicide attempts. An important area of investigation for Māori suicide is to disentangle the relationship between ethnicity, socioeconomic status and suicide, as is being done in studies of risk factors for physical morbidity and mortality. There is potential to learn from a systematic case study of the steep rise in suicides among young Mäori men, which began in the context of a cultural renaissance and rapidly increasing numbers of Mäori in the population, and which continued during a time of social and economic reform that disproportionately affected Mäori. Mäori were especially affected in terms of increasing social and economic inequalities with non-Mäori, including increasing unemployment compared to non-Mäori. There is also potential to add much to the general understanding of the relative roles of ethnicity, culture, socioeconomic and other factors as risk and protective factors for suicide. 20 Suicide Prevention in New Zealand In the same macrosocial context, age seems to be a protective factor for Mäori older than 45 years (see Report 5), but the significance of this has not been explored. Macrosocial and intra-group changes in values, norms, and gender and social roles have been well described and have become part of the dominant discourse about suicide among Mäori, and among young Mäori in particular (see Report 3). The role of mental illness as a precursor to suicide among Mäori has received less attention, in part because little is known about the epidemiology of mental illness among Mäori. However, there are indicators that the level of psychological morbidity among Mäori is high. Work on common mental illnesses among Mäori presenting in primary care (MaGPIE Research Group in press) reveals that the rates of anxiety, depressive and substance use disorders were all higher for Mäori than for others attending GPs. This study also shows that differences between Mäori and non-Mäori in terms of social and material deprivation did not account for the higher rates of mental disorder among Mäori attending GPs. Although mental illness is almost certainly relevant to suicide among Mäori (Skegg 1997), it has been suggested that the common Western notion of mental illness may not characterise a kind of psychological disorder related to a combination of collective grief, acculturative stress, and the intergenerational transmission of substance abuse and dysfunctional relationships to which some Mäori are exposed (Lawson-Te Aho 1998). In order for this theory to be developed in ways that have the potential to lead to preventive interventions, the components of processes such as acculturative stress need to be characterised better so that clearer links can be made with individual suicidal behaviour. An improved understanding of the aetiology of suicide among Mäori will most likely come from an integration of causal models, with acknowledgement of the importance of mental illness and ethnic and socio-cultural factors. Such a model may provide an improved focus for suicide prevention among Mäori. The issue of ‘youth’ A further contemporary issue the development of which has been significantly driven by the media and popular culture, and in part by academics and policy makers, and which demands consideration in any suicide prevention efforts is the emphasis in recent years on suicide as a problem of youth. (The previous discussion on culture is also relevant here.) It may be that in New Zealand suicide has become a theme in the discourse of young people about themselves. Young people in New Zealand consider suicide among their peers to be much more common than it is (Beautrais et al 2004), with one-quarter of a sample of 25-year-olds believing youth suicide was 10 times as frequent as it actually is, and two-thirds believing that more than half of all suicides occur in young people. Anecdotal evidence suggests that among some groups of young women, self-harm such as superficial cutting is widespread and openly discussed. Suicide Prevention in New Zealand 21 Social processes that bring the topic of suicide into the open among young people may have converged with other influences such as that of the media (in emphasising New Zealand’s youth suicide rates and publicising instances of youth suicide) and the occasional high-profile instance of celebrity suicide to bring a prominence to the discourse about suicide in New Zealand youth culture. It is possible that this prominence could influence the suicidal thinking and behaviour of some at-risk young people, although it is important not to overemphasise the size of this effect (Goldney 2001). It could also lead to some who are on the borderline of risk entering the high-risk group because suicide becomes either an ‘option’ for problem solving, or ‘normalised’, especially in the context of certain broader social conditions. This may be more likely to occur if discussion about suicide occurs outside clinical or other structured supportive settings such as guidance counselling. An example of the kind of broad social conditions that may act as promoting factors for increasing suicidal risk among those who are vulnerable is that in a period of high youth unemployment in Australia young people about to leave school experienced more stress and anxiety than in a period of lower youth unemployment (Winefield and Tiggemann 1993). In such a context, if the school leavers who are now more worried about their futures and carry other risk factors (Goldney et al 2000) are also subject to a youth culture where suicide is a prominent motif, some could be tipped into a more high-risk state. In terms of broad social conditions, a negative construction of ‘youth’ in contemporary society may also be relevant (Bourke 2003). However, while this idea may have intrinsic appeal as a way of linking characteristics of society with individual risk factors, it cannot be supported in all settings. In the European Union, for example, youth suicides rates rose during a period of high employment (Rutter and Smith 1995), although youth employment was not specifically explored. 22 Suicide Prevention in New Zealand 3 Contemporary Approaches to Suicide Prevention Suicide has been identified as an issue for political concern as a result of the increasing availability of good-quality suicide statistics, which indicate rises in suicide rates. The World Health Organization (WHO) has for some time clearly identified suicide as an important global public health issue, given that it is in the top three causes of death among those between 15 and 34 years of age in all countries that provide data (WHO 2004b). In countries where increases have been particularly notable among young people (such as New Zealand and Australia), there has been considerable political support for the development of suicide prevention programmes, and in New Zealand suicide prevention has the status of a government policy initiative (Wilson 2001). This began with the New Zealand Youth Suicide Prevention Strategy (Ministry of Youth Affairs et al 1998), but an all-ages strategy is to be launched in 2005 (Ministry of Health 2004). As a recognised issue for government, suicide has become identified as a public health problem, the prevention of which properly fits within a public health, or population health, framework. Within this overall framework three dominant explanatory models have contributed to the international development of a range of strategies for suicide prevention. Mental health Most suicide prevention initiatives of the past two decades have emphasised psychiatric explanations for suicide. The fundamental assumption, well supported by robust research (eg, Beautrais, Joyce, Mulder et al 1996; Mortensen et al 2000; Beautrais 2002), is that mental illness is a necessary precursor to lethal suicide attempts in the majority of cases. In terms of the causal chain, mental illness is the key risk factor close to the outcome (suicide), although the suicidal act itself may be precipitated by a stressor such as a relationship break-up, or an altered psychological state such as intoxication. Better identification, treatment and management of mental disorders are the primary routes to suicide prevention within this framework. Injury prevention and restricted access to means of suicide A second model or theoretical perspective on suicidal behaviour has come from injury prevention. This approach is based on the assumption that suicide can be conceptualised as a form of intentional injury, self-directed violence or deliberate self-harm that may be explained within an injury prevention framework. The injury prevention approach initially tended to focus on regulating access to means of suicide (eg, gun restriction) as a way to prevent suicide, and has had particular currency in the US because of this (Conner and Zhong 2003). In fact, the Centers for Disease Control in the US has located suicide in its violence portfolio. Recent work in the injury prevention area has broadened in scope and has tended to incorporate a greater range of social, psychological and psychiatric factors (Silverman 1997). Suicide and deliberate self-harm are priority areas for the New Zealand Injury Prevention Strategy. Suicide Prevention in New Zealand 23 The approach of restricting access to means has had some success, a good example being the substitution of natural gas for coal gas in UK domestic supplies (Cantor 2000). However, choice of method is not only dictated by availability but also by factors such as social and individual acceptability and deterrents such as messiness, consequences of failure and who might make the discovery (Clarke and Lester 1989). Simple restriction of means does not address such factors. Nevertheless, if the most readily lethal methods can be restricted there is some possibility of reducing rates. However, in the New Zealand setting the most common method among those at highest risk (males) is hanging, followed by motor vehicle exhaust. Most young women who die by suicide also do so by hanging or strangulation, having increasingly adopted this method rather than the less dangerous self-poisoning (Beautrais 2000a). It is difficult to see how access to these means can be completely restricted, although catalytic converters do reduce carbon monoxide emissions and may mean those who are discovered are more likely to be successfully resuscitated (Beautrais 2000a), and it is possible to fit baffles to exhaust pipes to preclude the attachment of hoses, or carbon monoxide sensors to the interiors of cars, linked to the ignition. Social interventions Another approach, based on sociological and macroeconomic theories, has led to an emphasis on population-level change in the social, economic and related structures that are believed to foster the development of suicidal behaviours. One prominent example has been the emphasis on the potential role of unemployment as a major factor in the aetiology of suicide (Qin et al 2003). This extensive domain of research area has been reviewed by Platt and Hawton (2000) in an update of Platt’s original 1984 review. They conclude that the area is still fraught with methodological difficulties which make it difficult to interpret the literature with any certainty, although it does seem likely that there are a range of interactive effects that are yet to be understood between labour market characteristics (rather than unemployment status) and other factors. Of note, they suggest that qualitative modes of enquiry have the potential to make an important contribution to our understanding of the relationship between suicidal behaviour and the labour market. Debates about the best approach In addition to these differing emphases, there have also been debates about different approaches to the delivery of suicide prevention strategies (Diekstra et al 1995; Lester 2000). These debates have centred around the question of whether prevention is better delivered via universal, population-level public health interventions, or with interventions targeted at high-risk populations (Mrazek and Haggerty 1994; Lewis et al 1997). Of course it is likely that the delivery strategy will depend on the target of the intervention. The prevention framework differentiating universal, selective and indicated prevention strategies forms the basis of major suicide prevention strategies such as that of the USA (US Department of Health and Human Services 2001). New Zealand’s new all-ages suicide prevention strategy, which this suite of reports provides supporting evidence for, acknowledges this range of prevention strategies. 24 Suicide Prevention in New Zealand In the first author’s experience of leading the project that has produced these reports, a tension exists in New Zealand between the proponents of these various explanatory and prevention models. Such tensions are not new, having been documented since before Durkheim (Guarnieri 1988), and certainly occurring as a result of Durkheim’s work (Berrios and Mohanna 1990). Nor are these tensions peculiar to the study of suicide: the epidemiology of mental disorder has been said to exist within an ideological struggle (Rogers and Pilgrim 2003). Yet when these models are examined, it is clear that, at a practical level at least, they are best regarded as complementary rather than competing, because they may lead to different but complementary prevention strategies. Furthermore, some prevention strategies are suited to immediate design and implementation, while others can only come about as a result of a more long-term social and political process. Detailed information on suicide prevention programmes and outcomes is available elsewhere (eg, Ministry of Youth Affairs et al 1998; National Health and Medical Research Council and the Mental Health Branch 1999; US Department of Health and Human Services 2001). Suicide Prevention in New Zealand 25 4 Social Interventions: Public Health, Social Epidemiology and Suicide What is social epidemiology? Social epidemiology is an emerging discipline within public health. It is a quantitative science, but one that embraces other disciplines. Fields that are making an important contribution to its development include the sociology of health and illness, health psychology, biostatistics, traditional epidemiology, and the basic life sciences such as physiology, biochemistry, neuroendocrinology and genetics. These fields are increasingly linked as the result of advances in the theory of health and disease causation and the testing of this theory demonstrating that we are at once biological, psychological and social beings, affected by the social, cultural and political environments we collectively create. Social epidemiology is not just one method. It is the application of a range of methods within a broad framework, which can produce sophisticated and robust analyses of the relationships and causal pathways between exposures at different levels and at different points in the life span, and health outcomes (Berkman and Kawachi 2000). Social epidemiology also provides an intellectual framework for asking questions about the complex causation of disease and for integrating findings from diverse research methods. Social epidemiology and the public health During the 20th century, traditional epidemiology moved away from its original population health paradigm to focus on the biological, psychological and social characteristics that were said to determine an individual’s health status. The development of epidemiology and its relationship to public health has been well described by Beaglehole and Bonita (1997). They observed that the change in focus was in part due to the epidemiological transition (in wealthy countries) from a high prevalence of infectious diseases to a high prevalence of non-communicable diseases, and in part due to progress in the relevant technology in this case, statistics. Key developments included the ability to estimate measures of risk, quantify confounding and interaction, and manipulate large data sets. Although the principle of a complex ‘web of causation’ was understood to be important, the focus was on ‘the agent, host and environment as the principle determinants of disease occurrence’ (Beaglehole and Bonita 1997: 98). The possible effects of social structures and systems received less attention. More recently, however, epidemiology and public health have turned their gaze back towards populations as the unit of observation, each with their own history, culture and economic and social structure (Pearce 1996). The public health approach, which is quite firmly a multidisciplinary enterprise, now requires practitioners to consider the links between these explanatory paradigms of health and disease that have been separated by disciplinary boundaries. The practical application of the new information about the causation of health and disease will also require cross-disciplinary thinking. For example, policies influencing the distribution of wealth in a country may need to be made with health outcomes in mind (Wilkinson 1999). Epidemiology, public health and health policy are entering a new phase (Susser 1996a, 1996b), and social epidemiology is helping to shape it. 26 Suicide Prevention in New Zealand Social epidemiology, mental health and suicide In the case of mental health and suicide, the separation between disciplines was never as complete as in some other areas of health, and within psychiatry and psychology the domains of social psychiatry/psychology have, while tending towards an individual-level focus (Rogers and Pilgrim 2003), maintained links with disciplines such as sociology. Indeed, when Rose (1985) elaborated on one of the central tenets of epidemiology that the incidence of a disease is related to the continuous distribution of its risk factors across the population, and that the greatest number of cases occur in the mid-range of the distribution of risk factors he used mental health as an example (Rose 1989, 1992; Anderson et al 1993). He urged that attention be paid to understanding and influencing the mass determinants of population means, prevalence rates, and incidence rates of psychiatric morbidity (Rose 1993). He observed that the determinants of variations in the risk of individuals becoming ‘cases’ of a disease may be different from the determinants of the variations in rates of the disease between populations (Marmot 1998). Another way of expressing this is to say that there are two important but separate questions to ask: Why do some people get a disease? Why do some populations have high rates of the disease? (Rose 1985). This distinction is important for any consideration of why suicide rates in one country or in one subgroup of a population are different to those in another country or subpopulation. A simple comparison between several countries will serve as an example. Table 2: Country * Four-country comparison of the prevalence of mental disorder and suicide rates 12-month prevalence of any mental disorder (%)* Total suicide rate per 100,000 (latest year data available)** USA 26.4 21.7 Ukraine 20.5 62.1 Belgium 12.0 40.1 France 18.4 35.5 CIDI 12-month prevalence from WHO World Mental Health Survey Consortium (2004) Epidemiology Study. ** World Health Organization 2004c. Studies in any of these countries would almost certainly reveal that most individual instances of suicide were preceded by mental illness of some kind. However, while the variation in the prevalence of mental disorder between countries is marked, the variation in suicide rates is even greater. Differences in the reporting of suicide deaths may account for some of this. Variations in the link between mental illness and death by suicide (which would be moderated by access to mental health services, for example) may also account for some of the difference. It is important not to over-interpret such variations, not least because of the variable origins and quality of the data and the fact that these are population-based data sets, not studies of individuals. Suicide Prevention in New Zealand 27 Nevertheless, the question does arise as to why, for example, suicide rates should be so high in the Ukraine when, even if somewhat under-reported, the prevalence of mental disorder (including substance abuse) is within the range of what has been reported in many countries, such as the USA. Response rates for the WHO study were similar in the USA and Ukraine (70.9%, 78.3%). France and Belgium both had lower response rates (45.9%, 50.6%), but an interesting comparison is still possible, with Belgium having substantially lower rates of mental disorder but a higher suicide rate. An increasing appreciation of the history of public health has contributed to recent developments in the public health approach to prevention (Perdiguero et al 2001), and there are important lessons in this for suicide prevention. It has been claimed that Durkheim was one of the early proponents of the social epidemiology approach, through his aim of showing that social dynamics explain individual pathology (Berkman and Glass 2000). However, it has also been observed that although Durkheim made an important contribution to our understanding of suicide as a social phenomenon, in downplaying the importance of individual suffering he ‘drew attention … away from the only practicable way of improving … [the] predicament [of the sufferers]’ (Berrios and Mohanna 1990). Rose also noted that Durkheim’s assertion of ‘complete independence between the characteristics of society as a whole and of its individual members’ (Rose 1992:62) was too extreme to accommodate a proper understanding and application of the principles of disease prevention. This view is especially relevant to the understanding of suicide and its prevention: it is not useful for those working in suicide prevention to consider the genetic and social determinants of suicide as independent of each other. Mental health, suicide and domains of influence It is now acknowledged that health status in general is the result of the interplay of factors from different domains, and different levels of influence (ie proximal or distal to the individual) including the biological, the psychological and the social.105 Clearly health status, including mental health status and suicidal behaviour, is profoundly influenced by biological processes. However, these processes occur within personal, social and cultural milieux, which can influence the underlying biological processes in individuals. There is increasing evidence to support this contention. A few salient examples are given here. Recent advances in neuroimaging and basic science techniques have shown that the immediate social environment influences the brain development of infants and young children (Goldsmith et al 1997; Siegel 1999; Johnston 2001), and that psychological therapies influence brain metabolism (Martin et al 2001; Brody et al 2001; Gabbard 2000; Paquette et al 2003). There has been work demonstrating a relationship between social class and job grade and the hypothalamicpituitary-adrenocortical axis hormones which mediate stress responses, and that this relationship varies with social class (Kunz-Ebrecht et al 2004). This type of observation is increasingly linked to health outcomes (Brunner and Marmot 1999). Biological substrates for suicidal behaviour itself have been mooted (Traskman-Bendz and Mann 2000). 28 Suicide Prevention in New Zealand Interactions between social factors at different levels There may also be short- or long-term interactions between individual-level risk factors in the social domain. Examples from the unemployment literature demonstrate that emotional and social support during periods of unemployment is associated with less psychological distress among adults and youth (Bjarnason and Sigurdardottir 2003). Another example is where low socioeconomic status in childhood has been shown to increase the risk of depression in adulthood, and make a contribution to the higher risk of depression among women (Gilman et al 2002). Yet another example is provided by the work of Kendler, who has demonstrated that heritable behavioural and psychological attributes influence the social environment individuals create around themselves, rendering aspects of the social environment, in effect, heritable (Kessler et al 1992; Kendler 1997; Eaves et al 1999; Kendler 1996). Furthermore, other social characteristics usually measured or determined at the level of the individual such as being unemployed or divorced, or growing up in a single-parent household may, when aggregated, also act as properties of the wider social or cultural environment, and influence health status from this level (Marmot 1998). There may also be interaction between population- and individual-level risk factors (Susser 1996b). A possible example of the former can be found in studies of unemployment. The association between unemployment (as an individual characteristic) and all-cause mortality has been shown by some studies to weaken as the unemployment rate in the population increases (Martikainen and Valkonen 1996), although the opposite has also been demonstrated. With regard to suicide, studies have shown both that suicide rates tend to fall in periods of high unemployment (Platt et al 1992; Preti and Miotto 1999a), and the opposite (Preti and Miotto 1999b). It is possible that population-level or contextual factors such as social cohesion or stigma against the unemployed, as well as macroeconomic conditions, exert differential influences on the suicide risk of certain individuals in the population, depending on other risk and resilience factors (Platt 1984; Wolff 1995; Stack 2000a) accruing to the individuals. Limitations to the application of social epidemiology to suicide and its prevention It is worth noting that the general theme of research into the social causation of ill health and health inequalities, which is supported by the social epidemiology approach and is contributing to the calls for prevention strategies aimed at altering aspects of society such as the distribution of wealth, is not without its critics. One argument is that the justification for this research theme is based on constructs such as social cohesion and social capital which are inherently flawed (Forbes and Wainwright 2001), because they are not well defined or operationalised and are often ‘measured’ using proxies. This means that there may be substantial measurement error, rendering apparent associations or lack of them spurious. In general, measurement error leads to a reduction in the strength of any apparent association (Rothman 1998). This is relevant to the thinking on suicide prevention because the notion of social cohesion and other characteristics of society having an influence on suicide rates is a key strand in suicide prevention literature. Suicide Prevention in New Zealand 29 A counter argument is that sufficient evidence is accumulating to justify including notions of social collectivity, however defined, as important contributors to physical and mental health (Kawachi and Berkman 2001; McKenzie et al 2002). The utility of a construct such as social capital is that it enables consideration of the social environment in an alternative way. In most studies of social risk factors for mental illness or suicide, the social exposures are characterised at the level of the individual (eg, individual socioeconomic status or an individual’s social support). The construct of social capital and other characteristics of society allows for the possibility that there are important interactions between the social environment and connected groups of individuals (WHO 2004a), which have an impact on health and mental health. Another argument is that even if features of society do shape the health status of its members, these are not risk factors that can be altered in the manner of a traditional public health intervention. However, it is obvious that governments daily make decisions that influence the characteristics of societies. The rise in income inequality over the past 20 years in countries with mixed market economies demonstrates this. The characteristics of societies can be shaped. So, what of the technical challenges to applying the principles of social epidemiology to suicide and its prevention? There is general agreement that contextual factors are relevant to the problem of suicide (Beautrais 2000c), and its prevention is increasingly being considered from this kind of perspective (van Heeringen et al 2000). However, as stated above, wider social and cultural environments are difficult to characterise and more difficult to quantify than other risk factors in ways that meet the requirements of methodologically sound studies. From an epidemiological perspective, there is a tension between the ability to conduct in-depth enquiries of relatively few people which yield much detail about individual-level exposures, and the ability to conduct less in-depth enquiries of large populations. However, studies of large populations (such as national populations) do provide an opportunity to scrutinise the wider milieu created by the collective characteristics of individuals. Although the ability to directly control for some factors is lost, alternative techniques such as sensitivity analyses of the ‘missing’ factors can offset some of the disadvantage (Blakely et al 2003). Longitudinal designs are of particular value in this regard. As well as the technical problems, the framework from which prevention activities are derived must also be considered. Prevention strategies are directed at modifiable risk factors, in mental health just as in other domains of public health activity. It has been relatively easier to obtain strong evidence about individual-level risk factors for suicide such as mental illness and individual-level social exposures (eg, losing one’s job or getting divorced). This does not mean that risk factors exerting their effects at other levels are neither important nor modifiable. The problem is that if the effect is only measured at the level of the individual (ie, cases of a disease), risks accruing from widespread exposures are more weakly associated with the outcome. In fact, a risk factor for Disease A, which affects everyone in a population, has no influence on the distribution of Disease A in that population (Rose 1985), yet it may still be a cause of the disease. If the risk factor is not only widespread but is also distant in the causal chain, then because of intervening modifying factors in addition to the ‘diluting’ effect of the factor being common, any association between the hypothesised risk factor and the outcome for individuals is likely to be weak. 30 Suicide Prevention in New Zealand The implications of this for prevention are related to the evidence-based framework currently in use. This approach is related to the evidence-based philosophy that has also influenced health service provision. In the public health arena it constrains public health interventions to those that are consistent with the available evidence. One limitation of this approach is that it has tended to focus on single disease outcomes or single risk factors, although more recent developments in cardiovascular disease prevention have been broader in scope. Finally, a lack of evidence for a purported risk factor does not mean it is not a risk factor; it means we do not yet know if it is one. There are a variety of reasons for an apparent lack of evidence, including: the appropriate studies have not been done, or those with negative findings have not been published the demonstrated effect is small (for the reasons discussed above, or simply because it is, in fact, a small effect) if the variable of interest is poorly characterised and/or measured, then it will be difficult to observe any associations. Arguments in support of potential preventive interventions are easier to make if the mechanism of effect of the risk factor is understood. Unfortunately, the mechanisms of effect of social factors such as unemployment, alcohol consumption or divorce, which may operate either as individual-level exposures or as exposures at the level of the social milieu, are not yet well understood (Stack 2000a, 2000b). However, effective population-level prevention programmes do not have to wait for an understanding of causal mechanisms if causation can be adequately demonstrated or other supporting evidence adequately marshalled. The case against tobacco smoke as a cause of lung cancer was thoroughly demonstrated long before the mechanisms of effect were understood. These observations support the contention that the best understanding of the causation and prevention of suicide will arise from exploration of a number of kinds of causal pathways (Hawton and van Heeringen 2000) that have effects at different levels of organisation (molecular, individual, social/cultural) (Pearce 1996), and the ability to account for these different aspects simultaneously. Whatever model is eventually found to best simultaneously explain suicide at the individual and population level, it will inevitably contain some domains where intervention might reduce suicide rates, and other domains where interventions directed specifically at suicide prevention are not practical. This means we need to pay attention to two distinct frameworks of thinking: an explanatory framework and an intervention framework. The intervention framework would be based on accepted types and levels of evidence, and practicality and cost/benefit considerations, and would be modified when new evidence was derived from the continuing development of the explanatory framework through the research process. Suicide Prevention in New Zealand 31 Cardiovascular disease and suicide: moving the population distribution of risk The recent public health focus on suicide prevention has been developed from parallels drawn between cardiovascular disease and suicide. In the case of cardiovascular disease, Rose’s theorem that a large number of people at small risk may give rise to more cases of disease than a small number at high risk’ (Rose 1992: 24) implies that prevention will be successful only when it moves from a clinical focus on treating high-risk patients who have already manifested the disease, to a population-based approach focusing on changing knowledge, attitudes, behaviours and cultural norms to prevent the development of cardiovascular disease in the population at large (Sanddal et al 2003; Knox et al 2004). The intention of this approach is to lower the entire population distribution of risk; that is, to reduce the mean value for the risk factors in question (Marmot 1998). It has been argued that because suicidal behaviour, like cardiovascular disease, has a multifactorial aetiology, suicide prevention would, like the prevention of cardiovascular disease, benefit from population-based approaches aimed at changing attitudes, norms and behaviours which predispose people to suicide and other adverse outcomes linked with suicide (eg, substance abuse and violent, antisocial and offending behaviours). However, it should be noted that there are important distinctions between cardiovascular disease and suicide, which affect the applicability of this model as it is usually described. First, there is an issue with the ability to precisely test the model in the case of suicide. Cardiovascular disease is almost ubiquitous in our society, and deaths related to it are very common, whereas suicide is a statistically rare outcome of a group of psychosocial disorders. This difference means that for suicide, small fluctuations in numbers can give rise to large fluctuations in rates, which are difficult to interpret. As the papers by Collings et al (Report 5 in this suite of reports) and Howden-Chapman et al (Report 4) show, the small numbers mean it is difficult to explore the risk factors for suicide at a population level, even when studying the whole New Zealand population. This also means that interpreting the results of evaluations of suicide prevention initiatives at a population level will be challenging if suicide is the only endpoint of interest. Second, suicide is the end result of a behaviour, not an illness in itself. In a causal pathway model, suicide is not analogous to cardiovascular disease; it is more analogous to the cardiac arrythmia that kills a person after their heart attack, or to the massive stroke that stops them breathing. Third, prevention efforts related to cardiovascular disease are focused on preventing or reducing the severity of the associated clinical syndromes (such as stroke, myocardial infarct, angina, cardiac arrythmias, hypertension and its sequelae). When we consider suicide prevention, we are considering the endpoint of a fatal illness. If the cardiovascular disease prevention model is to be usefully used to think about suicide prevention, there is a strong logical argument for adopting a new target of interest – namely mental illness, which, in the model, is analogous to cardiovascular disease. Fourth, there is a range of proximal risk factors for cardiovascular disease, many of which are suitable points for intervention, either by targeted interventions to high-risk people, or by population-level interventions, or both (hypertension is a good example; obesity is another). At present the single most important known proximal risk factor for suicide is mental illness (especially depression and substance abuse). 32 Suicide Prevention in New Zealand Finally, the idea of reducing the case rate in the population by moving the population distribution of the factor of interest (ie, lowering its mean value) makes best sense when the characteristic in question has a two-tailed distribution. For physiological measures (such as risk factors for cardiovascular disease) this is usually the case, and often the distribution approximates normality. However, for psychological characteristics this is often not the case, with distributions often having a long tail into the ‘abnormal’ spectrum. People who commit suicide are most commonly over the diagnostic threshold on such distributions: they will be somewhere in the tail of the distribution, say, of symptom severity, intensity of suicidal ideation or hopelessness. They are a clear target for preventive interventions. People who are near the threshold could potentially be pushed over it by other supervening risk factors, such as social factors like relationship break-up or behavioural disinhibition, such as when intoxicated. It is not clear how much extra benefit would be gained in terms of lives saved if suicide prevention were to be directed at the whole population, most of whom are not at risk of suicide. The Rose population-based prevention model may have some utility in suicide prevention, but the strategy needs to be clearer than simply drawing a parallel between suicide and cardiovascular or similar pathology. It is more logical to use it as an approach to modifying risk factors for specific prevalent illnesses such as depression, anxiety disorders or substance use, as these are the main proximal risk factors for suicide. However, no clear population-wide strategies have been identified for modifying the known risk factors for depression or anxiety disorders (Ellis and Collings 1997). In relation to subgroups of the general population, such as Māori, the whole population approach to improving the determinants of health (including mental health) needs to be considered with some caution. This is because particular subgroups within the general population may respond differently to population-wide initiatives. For example, if an intervention designed to decrease the prevalence of a particular health problem in the whole population is less effective for one subgroup, it will have the effect of increasing population disparity in terms of that problem. The challenge for whole population initiatives is to link equity of outcome with the population change by devising diverse programmes within a coherent whole population strategy that will be equally effective for all groups. Another potential criticism of the application of this framework to suicide prevention is that it locates suicide as a sequel to poor mental health, and the notions of mental health and illness have, of course, been subject to dispute for many reasons over many years (Szasz 1961, 1971; Helman 1990; Anleu 1998; Rogers and Pilgrim 2003). However, the weight of evidence strongly supports mental health status as a key final common pathway to most deaths by suicide. Targeting high-risk groups The targeting of high-risk groups is a traditional public health strategy and is complementary to the whole population model of prevention. Where such groups are identifiable and accessible it can be a powerful tool. The debate about whether it is best to use a whole population strategy to alter the population mean or to target at-risk groups is best resolved by considering how much of the population burden of the outcome (in this case, suicide) is compressed into an identifiable group where high exposure confers high individual risk (Rose 1992). This group, once identified, must be able to access the preventive intervention. Suicide Prevention in New Zealand 33 It has been argued that the most appropriate approach to suicide prevention is simply to more effectively identify and treat the proximal risk factor that confers the most risk mental illness (Isacsson 2000) and that evidence is accumulating in favour of this approach (Joyce 2001). The mental illnesses associated with most cases of suicide (depression, anxiety disorders and substance abuse) are highly prevalent and are recurrent for many people (Andrews 2001). Importantly, however, the factors predicting non-response to treatment for depression in a primary care setting include suicidal ideation and the presence of a social factor such as not working, which is not entirely accounted for by illness severity (Sherbourne et al 2004). In addition, people’s use of the services that are available is limited by a number of factors, including their understanding of mental health issues (Jorm 2000; Jorm et al 2000; Goldney et al 2001). Given the high prevalence and recurrent nature of mental illness, unless there is significant movement of resources from other sectors or other health services, the goal of eliminating most common mental illnesses by treating them will not be achieved (Sainsbury 2001). Therefore, while improved access to appropriate treatments is logically an important part of suicide prevention, it would not be sufficient on its own. More attention should also be given to serious deliberate self-harm (Hawton and van Heeringen 2000; Goldney et al 2000). This is a prevention strategy that targets those at high risk. It targets suicidal behaviour rather than the broader category of mental illness, and as such has merit. Suicidal behaviour is much more common than suicide, but represents a subset of those with more serious mental illness. There is considerable common ground between the features of those who die by suicide and those who attempt it (Beautrais 2001b). Because all suicides follow from suicidal ideation and suicidal behaviour, there is merit in considering suicidal behaviour as a potential target for public health interventions (Jenkins and Singh 2000). Given that one-third of those who attempt suicide repeat the attempt, that in the year following a suicide attempt the risk of actual suicide is increased by 100-fold, and that the risk of fatal repetition is highest in the year following the first attempt, this is an important and somewhat more identifiable high-risk group (Sakinofsky 2000). It may be particularly relevant for the prevention of youth suicide, given that proximal social factors are prominent in the risk factor profile for this age group. An integrated approach to suicide prevention Given the current knowledge base, it is not surprising that most countries have, or plan to develop, national suicide prevention strategies advocating a cross-sectoral approach, placed within a public health framework designed to permit a broad range of social, economic, health, mental health, cultural and other risk factors to be integrated and targeted (Jenkins and Singh 2000; Jenkins 2002; US Department of Health and Human Services 2001). This type of framework is increasingly favoured for developing and implementing the types of policy changes that have the potential to generate population shifts of risk, sufficient to make an impact on rates of suicidal behaviour. Such strategies include attempts to prevent the development of risk factors such as depression and psychosocial disorders (Mental Health Branch Commonwealth Department of Health and Family Services 1997; US Department of Health and Human Services 2001; Ministry of Youth Affairs et al 1998). 34 Suicide Prevention in New Zealand However, risk factors which, if modified, could potentially alter the distribution of risk in the population as a whole present other difficulties. Often the modification of such factors requires social change, which can only be legislated for in part. In general, changes in attitudes and social structures would be expected to take some time, although factors such as alcohol consumption and wealth distribution can be influenced more quickly by regulation. It is notable that the limited number of instances of reductions in suicidal behaviour that have occurred appear to have been effective at a population level. For example, reducing population access to a particular means of suicide, coal gas, reduced both overall suicide rates as well as suicide rates by that method (Kreitman and Platt 1984). The United States Air Force Suicide Prevention Programme is reported to have resulted in a reduction in suicides after the introduction of a community-based programme designed to raise awareness of suicide, promote help-seeking and increase access to mental health services and other sources of support (Knox et al 2003). There is, nonetheless, a strong case for more targeted interventions. Recently, the widespread introduction and use of the class of antidepressants known as selective serotonin re-uptake inhibitors (SSRIs) has been credited with reducing suicide rates by reducing the fraction of the population with depression, the most common risk factor for suicide (Olfson et al 2003; Isacsson 2000; Hall et al 2003), although others debate this claim (de Leo 2004). As described earlier, individuals who make suicide attempts are a relatively readily identifiable high-risk population characterised by ongoing mental health problems and high mortality (Beautrais et al 2000; Beautrais 2004a, 2004b). Attempted suicide is now regarded as an important aspect of research on suicide (Hawton et al 2003). It is likely that population-based programmes will need to be supplemented by more targeted and intensive programmes for high-risk groups such as those making serious suicide attempts. The enhancement of the recognition, treatment and management of depression, substance abuse and violent and offending behaviours will also make a contribution, but will require significant additional investment. An integrative conceptual model of risk and resilience The risk and resilience approach has been adopted in a number of recent New Zealand studies, and analyses of risk factors for suicide have not been based specifically on the general theories of suicide described earlier but more on a general conceptual model of the way in which suicidal behaviour is influenced by various domains of risk factors. (See, for example Beautrais 2001b; Fergusson et al 2003; Skegg et al 2003). Beautrais, for example, uses a framework that organises risk factors into a series of domains of conceptually similar factors: psychiatric morbidity genetic and biological factors social and demographic factors family characteristics and childhood experiences personality traits and cognitive styles environmental and contextual factors. Suicide Prevention in New Zealand 35 This approach views all domains of factors as making salient contributions to suicide risk and relies on observed patterns of association to estimate the relative contributions of these factors. This feature is important, since it allows comparison of the explanatory power of various hypotheses. The framework allows for the influence of protective factors, which is an area of increasing interest in mental health research and has been identified as an important new strand of suicide research (Hawton and van Heeringen 2000). It can also accommodate variation in the relative importance of different domains of influence between population groups, which is important from the social epidemiological perspective. This framework may be viewed from a social epidemiology perspective as being located in a milieu of population-level factors, which might include features such as characteristics of the labour market, social cohesion, the constraining power of shared social norms and values, levels and patterns of drug and alcohol consumption, and number of firearms per capita. These factors may have direct and indirect effects on variables more proximal to the outcome of suicidal behaviour and suicide. In addition, the relationships between various domains of influence are variable across time and, as they vary, determine or alter other elements of the model. Such a framework invites an appreciation of the obvious complexity of the aetiology of suicide. It also makes it clear that, in practical terms, prevention efforts can only be directed at those aspects of the model that can be most readily influenced in the short to medium term, and that are reasonably proximal to suicide in the causal chain. This is the case for several reasons. First, in the long term, changes in relationships between distal causal factors and suicide rates are difficult to predict, because distal causal factors are often difficult to measure and their effects may be more context-dependent than those of more proximal risk factors. Second, the available evidence shows that for most suicides the strongest effects are those of more proximal risk factors (Jenkins and Singh 2000; Beautrais 2003b). In some cultures, in specific situations, social factors such as expectations of behaviour may act as proximal risk factors. An example of this is the custom of suttee, referred to earlier. Shared social expectations about behaviour may also confer protection; for example, suicide rates are typically low among those of the Islamic faith (Cheng and Lee 2000), although there is no reason to believe that rates of risk factors such as depression would be hugely different in such populations (WHO World Mental Health Consortium 2004). A potential criticism of this model is that it gives primacy to mental health status as the most proximal risk factor. In itself this is not a problem, because the weight of evidence is that for the majority of suicides poor mental health status is the final common pathway of influence. However, some claim that restricting the notion of ‘at risk’ mental health status to the presence of mental disorder is problematic (van Praag 2003; de Leo 2004). The difficulty lies more with the definition of ‘mental disorder’, which itself is a problematic construct (Rogers and Pilgrim 2003), evolving over time and determined by complex factors, including culture-specific explanations for deviant behaviour and personal distress. This may be particularly relevant in the case of youth suicide, where psychological and social factors other than mental illness are also important risk factors for suicide. 36 Suicide Prevention in New Zealand However, in order to pursue a coherent approach to suicide prevention, some kind of framework must be employed which is consistent with the existing evidence about risk factors of any type for the population the preventive measures are being applied to. As previously discussed, prevailing ideological and scientific paradigms shape research directions, so it is important that any framework has some flexibility to accommodate new developments, if necessary. The choice of intervention points is not value-neutral, but the values on which the choice is based can readily be made explicit. Having a framework also provides a basis for the evaluation of suicide prevention activities, which is a critically underdeveloped area (Hawton and van Heeringen 2000). The causation of suicide at the individual level and as a social phenomenon is so complex, especially over time, that research enquiry should not be directed to one part of the explanatory framework alone or to a few restricted research questions. On the other hand, prevention efforts are best directed to areas where there is strong evidence in support of particular points of intervention. This includes the reduction of the associated suffering for the suicidal person and those close to them. The clinical focus of the last 20 years of suicide research has provided much information about the risk and protective factors for suicidal behaviour. Although the focus has been on the individual, there is evidence accumulating that the nature of our communities and of society is also important. Social and economic disadvantage may also have important roles. These broad social factors may act as wide-reaching contextual influences whose effects are largely mediated via individual psychiatric states, or they may serve as markers of other correlated risk factors. However, our understanding of the pathways and mechanisms of effect for such factors is less developed. This means the immediate application of this knowledge to something as specific as suicide prevention is limited. However, work on integrated models of the effects of individual and contextual factors is emerging. For example, Goldney has hypothesised that there is a base rate of deaths from suicide in all communities, which is determined by biological and psycho-social factors, and that where suicide rates diverge from this base rate psychosocial factors (including macrosocial factors) are likely to be important (Goldney 2003). On the basis of a model such as this, it may be possible to quantify the impact of various psycho-social factors on the base rate. Such a model may also contribute to the allocation of suicide prevention resources (Goldney 2003). The complexity of the relationship between factors that influence suicide rates exists not only in cross-section (that is, at one point in time, or over short periods) but also over longer periods of time such as decades. The rapid changes in suicide rates among particular population subgroups serves to illustrate this well. Although this may seem obvious, from the perspective of prevention it needs to be remembered because it means that suicide prevention initiatives that are effective in one time and place may not be effective in another (de Leo 2002). Suicide Prevention in New Zealand 37 The task that faces suicide prevention in the 21st century is to translate the robust research findings about individual- and social-level risk factors into preventive interventions. An important aspect of this is the further development of multisectoral prevention strategies centred around the management and reduction of common mental disorders at both the individual and population levels. Further exploration of the mechanisms of effect of broad social factor influences is also required, and needs to be integrated with what is known about biological and psychological influences on suicidal behaviour. Suicide among Mäori needs further research and intervention attention in both spheres. New and existing strategies must be implemented adequately and evaluated systematically. 38 Suicide Prevention in New Zealand 5 Social Epidemiology in Practice: Interpretation of Reports 1 to 5 This section summarises and interprets the key points from each of the supporting reports. The broad questions examined in these reports are: What are the social, economic, cultural and other population-level influences on suicide which have been described in the international literature? (Report 1) What are the relationships between changes in such factors in the New Zealand context, and in New Zealand suicide rates? (Report 2) What are the key explanatory frameworks used by Mäori experienced in Mäori mental health practice and theory? (Report 3) Can a cross-country comparison of economic contextual factors help our understanding of the relevance of these factors to suicide rates in New Zealand? (Report 4) How do the associations between suicide rates and socioeconomic factors in four New Zealand population cohorts change over time, and can this be linked to broad contextual factors? (Report 5) See the Preface section for the titles and authorship of these five reports. 1 Explaining patterns of suicide: a selective review of studies examining social, economic, cultural and other population-level influences Authors: C Maskill, V McClellan, I Hodges and S Collings. This selective review had two purposes: to identify societal factors that it may be possible to examine in relation to suicide in New Zealand if data were available to provide a general summary resource on the scope of the sociological literature on suicide, to complement existing extensive reviews of individual-level risk factors for suicide. It is not a technical review or a Cochrane-style systematic review. There is a diverse range of sociological theories purporting to explain the phenomenon of suicide. Three relevant streams of sociological thought were identified: the structurefunctionalist, the conflict or critical, and the interpretive streams. There is no agreement as to which has the most explanatory power. Suicide Prevention in New Zealand 39 Many quantitative studies have investigated the relationship between social and cultural variables and suicide. There are four main types of study: cross-sectional studies of individual-level associations, cross-sectional studies of aggregate-level associations, cross-sectional cross-level studies, and studies that investigate changes over time. The results of studies using these different methods to explore the same domains cannot be assumed to be interchangeable, because they are answering different questions. For example, a study revealing an association between unemployment rates and suicide rates over time does not confirm the results of a study comparing suicide rates among employed and unemployed individuals. High consistency was found between studies for the association between mental illness and suicide, supporting the findings of New Zealand studies in this area (although this was not the focus of the review, it was deemed important enough to be briefly described). Some consistency emerged between studies for the importance of: the gender and age distribution of suicide in countries with similar degrees of economic development availability of method imitation and cluster suicides (especially among the young) cohort and period effects on risk factors at the societal level (eg, acceptance of a range of family structures and higher divorce rates, which are perhaps a proxy for a loosening of broad social constraints) and the individual level (eg, depression) minority indigenous cultural status high rates of migration within countries, and higher rates of suicide in recipient countries for between country migration religious belief and participation social prestige and occupational standing periods of economic depression, periods of modernisation, economic development and structural economic reform temporal and seasonal effects wars and political events chronic and serious physical illness. Inconsistent results were found for an effect on suicide for: population fertility rates differences in urban and rural suicide rates across countries education levels income inequality unemployment rates female labour-force participation periods of economic expansion crime, homicide and violence 40 Suicide Prevention in New Zealand the quality and availability of mental health services. Even where study results are consistent, we cannot, however, infer that any one of these factors actually causes suicide, due to the complexity of the relationships being investigated (such as confounding factors common to different studies) and the limitations of data and methods. However, where studies produce consistent findings, the weight of evidence is increased even if the individual studies do not have explanatory power. The exception to this is the individuallevel studies of mental illness and substance use as a risk factor, because many of these studies were able to apply robust designs that do permit inference about causation. This review did not include the risk/resilience model, because in general this model is applied at the individual level. At this level it has been shown that protective effects occur for young people in the presence of positive configurations of factors such as high self-esteem and low neuroticism (Fergusson et al 2003). Few studies have explored resilience in adults (Beautrais 2003b). Some of the social and economic indicators described in this review as having possible associations with increases in suicide rates may point to the relevance of reduced social integration and social constraint as a characteristic of society. However, it may be that what is most relevant here is not the absolute characteristics of society within this type of domain, but the pace and extent of social change and the life trajectories of particular subgroups of the population within changing macrosocial circumstances. Potentially relevant features of New Zealand society (and that of other Western countries) that have emerged from the social change of the last 50 years include: a youth culture that is subject to more powerful transmission and self-perpetuating mechanisms than in the past the influence of the media a changed notion of ‘the family’ decreasing social constraints on individual choice and behaviour increasing substance use. 2 Suicide rates in New Zealand: exploring associations with social and economic factors Authors: S Ferguson, T Blakely, B Allan and S Collings. This report provides a simple visual overview of patterns in New Zealand suicide trends over time, as they relate to certain social factors for which there were available data. It is comparable to the type of simple visual data presentation used by the World Health Organization, and is limited in its interpretation to general observations and hypotheses that could either be explored by reference to the extensive international literature existing for most of these factors, or by testing in future studies. Suicide Prevention in New Zealand 41 The time periods of observation range from 1948 to 1999 for suicide, to shorter periods within this range for other factors. The shortest period of observation is 14 years, for unemployment and age-specific suicide rates. Although further time has passed since the retrieval of the data sets, at the time this document was prepared only a further two years of suicide data would have been available. The results and conclusions are unlikely to have been significantly affected by the inclusion of this data, given that the interest is in long-term trends, not year-by-year changes. Following is a brief summary of the main findings. No findings of statistically significant correlated changes were made in this analysis. Because these are time-series data over a relatively short period, the analysis is being applied to relatively few observations and is therefore underpowered to detect any except very large associations. Furthermore, because the intention was to show simple visual presentations of what are, essentially, raw data, formal time-series analysis using regression models has not been done. The standard analysis of suicide by gender, age group and ethnicity yielded the same results as official statistical analyses, but is presented for completeness. Suicide rates have gone up overall during the period in which markers of social change have also changed in generally consistent directions. The markers investigated here were marriage rates, female labour-force participation rates, fertility rates, crime violence and homicide, and immigration patterns. Economic indicators explored were unemployment rates, the economic business cycle and income inequality. There was no simple association between any of these factors and suicide rates in New Zealand. There is variation in regional suicide rates within New Zealand. This cannot be interpreted as a simple urbanrural difference, because both the highest and lowest regional rates were in the provinces. The differences are more likely to be attributable either to the very small numbers of suicides in some District Health Boards or to people living in different areas having different characteristics. However, fluctuations from year to year can be large when numbers are small (Ministry of Health 2004), and comparisons are difficult because District Health Boards have such diverse characteristics. The methods of suicide are changing because previously available means are restricted. Between 1977 and 1996 in New Zealand, suicide by hanging and motor vehicle exhaust became more common, while suicide by firearms and self-poisoning decreased. The observations in this report provide a degree of support for the notion that change in social conditions in general might be linked with suicide rates, but this would require confirmation with appropriately designed analyses. These observations alone do not support the simple proposition that economic indicators are directly causally related to suicide rates. 42 Suicide Prevention in New Zealand 3 Whakamomori: He whakaaro, he korero noa: a collection of contemporary views on Mäori and suicide Authors: P Hirini and S Collings. Suicide rates rose rapidly for Mäori between 1957 and 1991, and remain higher than those for non-Mäori. This is consistent with higher suicide rates among indigenous peoples in other countries, particularly young indigenous people. The aim of this study was to use a Mäori development framework to devise a qualitative study describing the relevance of social conditions and historical events to suicide among Mäori, as understood by a selected group of five Mäori experienced in mental health theory and practice. A Mäori development approach was integrated with the basic principles of qualitative research using a social constructivist perspective. A study was then designed to describe the key elements of the discourse on social factors and suicide by interviewing five selected Mäori with particular expertise or experience in issues of Mäori mental health and suicide. In the literature, the key variables associated with indigenous and Mäori suicide include individual risk factors demonstrated by epidemiological studies, and the influence of historical, political and social processes. A number of key domains were identified as important to the understanding of suicide among modern Mäori: the historical effects of New Zealand social and economic change on the Mäori population, with cultural alienation and social disadvantage suggested as symptomatic of rapid colonisation and later urbanisation of Mäori the re-emergence of a Mäori cultural identity and its dynamic nature in a changing world poorer mental health outcomes for Mäori compared to non-Mäori rapid social and intra-group changes in social values and norms, and in social and gender roles the influence of some aspects of modern international ‘youth culture’ the impact of negative social contructions of Mäori alienation from both ‘traditional’ Mäori culture and social institutions, and from mainstream society poor self-concept among Mäori, and Mäori youth in particular. The dominant theme of mental illness in mainstream suicidology literature was placed in a wider cultural context, to argue that Mäori pathways to mental illness and suicide may be linked to social and cultural conditions in different ways for Mäori and non-Mäori. Similarly, suicide rates among Mäori may be seen more as a marker of the health of contemporary Mäori society rather than of individual Mäori. It was suggested that improving the collective self-concept or cultural identity of Mäori, and increasing positive expectations about roles for Mäori in modern society, might contribute broad protective factors against suicide. Drawing distinctions between the effects of systematic bias against Mäori in social institutions, the characteristics of Mäori culture, and material deprivation may assist with the development of Mäori-specific or Mäori-responsive social interventions to reduce suicide rates among Mäori. The importance of better integration between the socio-cultural and mental health models of suicide is argued. Suicide Prevention in New Zealand 43 4 The impact of economic recession on youth suicide: a comparison of New Zealand and Finland Authors: P Howden-Chapman, S Hales, R Chapman and I Keskimäki. The purpose of this study was to examine the institutional arrangements and policy conditions that may have contributed to any differences in suicide rates among young men in New Zealand and Finland. Finland and New Zealand were compared because they have similar population sizes, and governments that support redistributive welfare policies, deregulated economies and trade liberalisation. Male and female all-age suicide rates in Finland have been consistently higher than in New Zealand since the 1960s. In the 1990s, suicide rates rose among young men in New Zealand so that for the first time they exceeded those of young men in Finland, although they had been high in both countries when compared to other countries. The two governments dealt differently with a major economic recession in the late 1980s and early 1990s. Such cross-country comparisons offer the opportunity to study the health effects of divergent policies when the global macroeconomic context is shared and a common method is used in suicide research (Cantor 2000). This study assumes that suicide is more immediately responsive than other causes of death to economic change resulting from policy responses to external economic shock. Using this assumption, suicide is considered as an early indicator of the effects of policy change on health and subsequent mortality. A theoretical explanatory model of the relationship between external economic shock (a global recession) and suicide rates was subjected to preliminary testing using available data. In the decade prior to the recession, New Zealand’s welfare state changed to a ‘safety net’ model, whereas Finland maintained a more comprehensive approach. In New Zealand during the 1980s and 1990s income inequality increased, whereas in Finland it did not. Unemployment in Finland peaked at 19% in 1994, and in New Zealand it was at its highest, at 10%, in 1991. In both Finland and New Zealand, youth unemployment was consistently higher than adult rates. In terms of at least one known individual-level risk factor for suicide, alcohol abuse, it is known that per capita alcohol consumption is high in both countries and binge drinking is a pattern common to both. This may account for at least some of the similarity in high youth suicide rates. For each country, statistical modelling of the available data series that is, annual change in GDP, Gini coefficients and unemployment rates against suicide rates among males aged 15–24 was done. Unemployment rates added no explanatory power and so were discarded from the models. Income inequality and GDP growth were associated with youth suicide in New Zealand in the expected direction, although these associations were statistically significant only at the 10% level (p = .062). In the model for Finland there was no such association. 44 Suicide Prevention in New Zealand The study concludes, on the basis of the exploratory model, that it is possible that the divergent policies of the two countries had differing impacts on male youth suicide rates in the face of an external economic shock, because of their effects on income inequality. This study does not provide evidence that any such relationship is directly causal. Nor does it link the early institution of a broad-based suicide prevention programme in Finland to the overall reduction in suicide rates (albeit after an initial increase). Neither does the study indicate whether the time-series data for youth suicide rates in New Zealand and Finland were subject to statistical tests for trend, or whether any demonstrated trends were significantly different. (Caution is urged elsewhere in this report with regard to the interpretation of time-series data where apparent fluctuations can be large because of the relatively small numbers.) It is important to note that because both individual-level risk factors and temporal patterns in suicide rates differ between age groups, the findings of this study may not be applicable across the life span. The model does not account for attempted suicide. The overall attempted suicide rate in Finland remained stable during the recession (Ostamo and Lonnqvist 2001), although it did not actually fall. This is consistent with Kreitman’s (1990) finding on attempted suicide rates during an economic recession in the population of Edinburgh, Scotland. This is important because there is considerable overlap in the characteristics of those who commit suicide and those who attempt suicide (Beautrais 2001b). If attempted suicide rates among youth were stable or fell and suicide rates rose, it is likely this would be largely due to an increased frequency of choice of a lethal method. As mentioned previously, choice of method is influenced by a wide range of factors. This study does not describe or account for other known risk factors for suicide in youth, such as life course adversities, mental health problems and adverse life events. A cumulative risk model where suicide is the endpoint of a combination of such factors has been shown to fit with what is known about these individual-level risk factors in both Finland (Kotila and Lonnqvist 1987, 1988; Suokas and Lonnqvist 1991; Marttunen et al 1991, 1992, 1993) and New Zealand (Martin 2004; Pearce 1996; Statistics New Zealand 2002; Baume et al 1998; Conner and Zhong 2003). Inclusion of these factors would strengthen the theoretical model. Such a model would also need to reconcile with the work of Rutter and Smith (1995). This examined trends in psychosocial disorders in European young people over a 50-year period, finding that increases in these disorders are unlikely to be simply attributable to economic adversity because many of these problems increased most during times of prosperity and high employment. On the other hand, there is increasing recent evidence in support of the hypothesis that high income inequality has an adverse effect on general health outcomes (Shaw et al 1999; Crampton and Howden-Chapman 1997; Beaglehole and Bonita 1997; Kawachi 2000), including mental health outcomes (Rogers and Pilgrim 2003). Suicide Prevention in New Zealand 45 A useful refinement of the statistical modelling would include all age groups, an indicator of other known risk factors relevant to each age group, and possibly an indicator of access to treatment, such as prescription of antidepressant medication. Techniques such as sensitivity analysis could be used where factors cannot be quantified with certainty (Blakely et al 2003). Further work could provide estimates of the impact of the recession and accompanying economic policies on youth and adult male suicide rates in New Zealand. This is an approach used increasingly to assist decision-making about where suicide prevention efforts should be directed (Lewis et al 1997), just as it is applied in public health more generally (Bruzzi et al 1985; Northridge 1995). However, it is likely that, as with other studies of risk factors that may be more distal in the causal chain, the attributable risks will be small compared to those for proximal risk factors. Finally, when only two countries are compared it is more difficult to draw firm conclusions about possible explanations than when a number of countries are compared. 5 Suicide trends and social factors: New Zealand 1981 to 1999: analyses from the New Zealand CensusMortality Study Authors: S Collings, T Blakely, J Atkinson and J Fawcett. This study investigated the relationship between trends in suicide rates and a range of indicators of socioeconomic position in New Zealand during four intervals in the 1980s and 1990s: 198184, 198689, 199194 and 199699. In order to do this, New Zealand Census data were linked with mortality data for the four cohorts. The study populations consist of the entire population of New Zealand selected into four cohorts on census night in 1981, 1986, 1991 and 1996. The study examines whether people in some socioeconomic groups were more or less vulnerable than others to background secular trends in suicide rates. The socioeconomic factors explored were ethnicity, marital status, household income, car access, highest educational qualification and labour-force status. The study extends a previous analysis of the 199194 cohort, which showed an association between socioeconomic position and unemployment and suicide among 2564-year-olds. The four intervals span a period of rapid macrosocial change in New Zealand, during which there was deregulation of the financial sector, reorganisation of the state sector, introduction of a flattened tax system, privatisation of major utilities, user charges for government services and a restructured labour market. Three analytical models of how social context may influence suicide are described, along with general approaches to the quantitative analysis of such relationships. Analyses consisted of: comparing suicide rates over time within different socioeconomic levels comparing the social gradient in suicide across time (eg, exploring whether the association of income with suicide changed over the four cohorts) multivariable analyses, using Poisson regression, to answer specific questions generated by the stratified univariate analyses. 46 Suicide Prevention in New Zealand Data limitations restricted the multivariable analyses to men aged 2544 and 4564. The major finding was that no socioeconomic groups in these age groups were protected from background trends in suicide rates. Suicide rates rose and fell in concert over time. The only exception to this pattern was found among income groups, where, over time, suicide trends varied by income. Among 25–44 and 4564–year-olds the association of low income with suicide risk strengthened over time. The fact that in men this association was largely removed once other socioeconomic factors were controlled for in the multivariable analysis may indicate that multiple factors associated with suicide became more concentrated with low income over time. Not being married was a strong and independent predictor of suicide, a finding which is consistent with many international studies (Cantor 2000). Being unmarried is associated with increased risk of mental ill health and with poorer social integration for men. It appeared that a large proportion of the excess risk of suicide among Mäori men was due to socioeconomic factors. In some instances, once these were controlled for Mäori ethnicity was protective in those over the age of 25 years in the earlier periods. Cultural affiliation has been hypothesised as being protective against suicide for indigenous people in some other countries. This requires investigation in the New Zealand context. Interestingly, suicide rates increased at least as much among the employed as the unemployed for men aged 18–44 and women aged 18–24 years, and the greater proportion of suicides occurred among the employed. It is suggested that the excess increased risk of suicide among the employed may be associated with changes in the nature of work (eg, the increasing casualisation of labour, the increasing number of part-time short-term jobs and the increasing need for people on low wages to work more than one job) during the study period. Compared to other risk factors commonly examined in epidemiology, many associations were strong – but not as strong as the association of mental illness with suicide. The findings are consistent with the existence of causal pathways between social conditions and death by suicide. However, explanations about such pathways, by which marital status and socioeconomic position might influence suicide risk, cannot be inferred from this study. Individual-level studies have repeatedly shown that socioeconomic factors make a smaller contribution to suicide risk compared to other risk factors such as mental illness. A possible explanation for this is that socioeconomic factors are more distal in the causal chain. This study has some technical limitations that mean the analysis should be interpreted cautiously. These include the inevitable collinearity of the measures of socioeconomic status, and measurement error of the social factors. Strictly speaking, this means that if these variables are simultaneously adjusted for, apparent independent effects may not be what they appear. Also, because follow-up was over a short period of three years, some degree of health selection is likely within each cohort (ie, people at risk of suicide because of another risk factor such as depression are likely to move into more socioeconomically disadvantaged groups, thus apparently increasing the association between socioeconomic exposures and suicide). Incomplete record linkage was a problem, particularly in the youngest age group. Because of this, interpretation of results for those aged 15–24 years should be very cautious. Finally, the Suicide Prevention in New Zealand 47 results of the multivariable analysis may not be generalisable to men under the age of 24 or over the age of 64, or to women of any age. One important strength of the study is the repeated examination of socioeconomic factors every four years in near-identical studies. This offsets potential problems with the internal validity of each of the individual studies, because these are likely to be relatively standard across all four cohorts, meaning that comparisons across time are valid. Conclusions These five reports were generated by a multi-method approach to the exploration of relationships between suicide and a range of social factors in the New Zealand context. With the available data and resource limits it was not possible to conduct multi-level analyses or to investigate within-level causal pathways. Instead, they constitute a New Zealand sample of the kind of evidence that exists about relationships between socioeconomic and cultural factors in some other countries. The papers have not focused on individual-level risk factors because New Zealand evidence about these is already of high quality. In regard to contextual factors, while some higher-quality evidence exists for other countries, nothing shown here is inconsistent with international findings. The broad consensus arising from these papers is that social factors are relevant to suicide. This is consistent with international opinion that suicide prevention cannot be left entirely to clinical interventions (ie, highly targeted prevention, also known as indicated prevention activities) (de Leo 2004). However, it is not clear from these, or from international studies, which sociallevel interventions (if any) will have a demonstrable and specific effect on suicide rates, either in the population as a whole or in specific sub-populations. Preventing any health problem depends on evidence generated by research. The social epidemiology perspective is a useful model for a public health research approach to the causes of suicide, because it can accommodate the different kinds and levels of evidence generated by different types of enquiry. This means it invites research into suicide from a range of perspectives, and also different types of intervention, ranging from those that might influence social and economic structures to those that target people with high risk due to individual-level factors. Referring back to the analogy of preventing deaths from cardiovascular disease, it is worth noting that this has had most success where prevention efforts are spread over a range of intervention types at different levels of influence in the causal chain. However, other New Zealand health statistics provide a good example of how health outcomes for different groups in society can soon diverge when important distal factors are ignored in prevention efforts. For example, deaths from cancer are strongly patterned by socioeconomic status, and this is likely to be due to a combination of differential access to care, differential environmental and lifestyle exposures and more subtle but powerful influences on attitudes, behaviour and choice, which can be understood within the constraints of socioeconomic context (University of Otago and Ministry of Health 2005). 48 Suicide Prevention in New Zealand In the case of suicide, research into causation and prevention across different levels of the causal chain is less developed than for, say, cardiovascular deaths. It has been argued that internationally there has been a lack of commitment by governments to provide adequate financial resources to do research into the causes and prevention of suicide (Wasserman 2004). The perspective afforded by social epidemiology provides a structure within which a range of types of research findings can be integrated, and with further theoretical and methodological development hopefully linked in future. However, with the data available to this project it was not possible to generate evidence to increase the specificity of any policy recommendations beyond what is already available in the New Zealand and international literature. Having said this, it is also important to state that many social interventions need to be considered in their own right, independent of any potential effect on suicide rates. This is because some factors known to be linked to risk factors for suicide (such as substance abuse, child abuse and neglect) may be amenable to either targeted interventions or whole-population initiatives. In addition, there are broader benefits to individuals and to society from interventions that improve adverse social conditions such as high unemployment rates and economic disparities between population groups. Suicide Prevention in New Zealand 49 6 Suicide Prevention: What We Know Now about What is Effective In recent years, increasing and widespread concern about the problem of suicide has generated a dramatic increase in the volume of research about the causes and risk factors for suicidal behaviour. Despite this, there is relatively little evidence-based information about the types of programmes and interventions that successfully reduce or prevent suicidal behaviour. This chapter reviews current knowledge about suicide prevention strategies that show effectiveness, or promise of effectiveness, in reducing or preventing suicidal behaviour. It also discusses problems in demonstrating the effectiveness of such programmes. Risk factors for suicidal behaviour There has been an increasing amount of research into the factors that place people at risk of taking their own lives. This research is beginning to present a clear picture of the mix of conditions that contribute to the endpoint of suicide. These factors include the following. Mental disorders: including depression, bipolar disorder, substance use disorders (alcohol, cannabis and other drug abuse and dependence), antisocial and offending behaviours, schizophrenia and anxiety disorders. New Zealand and international studies based on large case control designs and longitudinal studies have found that approximately 90% of people who die by suicide or make serious suicide attempts will have one or more mental disorders at the time of their attempt, with these disorders typically being accompanied by other sources of life stress and difficulty (Beautrais, Joyce, Mulder et al 1996; Beautrais 1998a, 2001b, 2002; Cheng 1995; Cheng and Chen 2000; Fergusson et al 2000, 2003; Risk factors for suicide over the life course 1998). Exposure to childhood adversity and trauma: numerous studies suggest clear linkages between exposure to childhood adversity and risk of later suicidal behaviour (Fergusson and Mullen 1999; Johnson et al 2002; Beautrais, Joyce and Mulder 1996). In general, experiences of childhood adversities tend to act cumulatively, with those most at risk of suicidal behaviour being characterised by multiple childhood disadvantage (Beautrais 1996; Fergusson and Lynskey 1995; Blakely et al 2003). Socioeconomic and educational disadvantages: population-based nested case control studies using national registers have found that factors including mental illness requiring hospital admission, unemployment and low income are linked to suicide (Qin et al 2003; Mortensen et al 2000; Blakely et al 2003). Exposure to recent stresses or life difficulties: case control and prospective longitudinal studies suggest that exposure to stressful events and circumstances, including (particularly) relationship breakdowns and difficulties, increases suicide risk (Fergusson et al 2003; Brent et al 1993; Beautrais et al 1997). Tendencies to react impulsively and aggressively under stress: studies of the familial transmission of suicide attempt behaviour show it is more likely among offspring with increased impulsive aggression (Prevention of familial transmission of early-onset suicidal behaviour 2003). 50 Suicide Prevention in New Zealand Genetic and biological predispositions to suicidal behaviour, aggressive and impulsive behaviour, and the mental disorders with which suicide is associated: using twin designs, studies have suggested that up to 45% of the variance in suicidal behaviour may be genetic in origin (Prevention of familial transmission of early-onset suicidal behaviour 2003; Statham et al 1998). In addition, researchers have attempted to identify biological and genetic markers for suicidality, focusing particularly on those involving the serotonergic system (Mann et al 2001). Interactions between genetic vulnerabilities and life stresses: a prospective longitudinal study has reported a gene-by-environment interaction in which an individual’s genetic makeup moderates his or her response to exposure to environmental stress (Capsi et al 2003). Access to lethal means of suicide: numerous studies have reported that access to a range of lethal methods of suicide leads to increased rates of suicide by that method (Brent and Bridge 2003; Beautrais 2001a). Sensationalised media reporting of suicide: reviews of media reporting styles suggest that glorified, and highly publicised and sensationalised, reporting of suicide is associated with increased risk of suicide (Gould et al 2003; Pirkis and Blood 2001). The risk factors for suicide and attempted suicide tend to vary with age (risk factors for suicide over the life course 1998). Factors such as childhood adversity and recent life stress tend to be more influential for younger people. Mood disorder plays an increasingly significant role with increasing age and makes a greater contribution to suicide risk among older adults than youth. The typical profile of youth (under 25 years) suicide is one of predominantly young males, characterised by family and social disadvantage, a history of suicide attempt, current mood disorder, and stressful interpersonal and legal life events. Among adult suicides, males predominate, and mental disorder (particularly mood disorder) and a history of psychiatric hospitalisation play a dominant role. Against this background of mental health problems, recent interpersonal and legal life events increase suicide risk. Among older adults, depression and a history of psychiatric hospitalisation make the major contributions to suicide risk (Beautrais 2002). It is important to recognise, however, that while most people who die by suicide or make suicide attempts will experience a recognisable mental disorder, often accompanied by other life difficulties, it is not the case that most people experiencing mental disorders and/or life difficulties will attempt to take their own lives. Likewise, few who experience suicidal thoughts go on to commit suicide (Gunnell 2004). Protective factors for suicidal behaviour Less is known about protective factors that encourage resilience to suicidal behaviour. However, a number of factors have been suggested as playing a potentially protective role for young people, including: good coping skills and problem-solving behaviours positive beliefs and values feelings of self-esteem and belonging connections to family or school secure cultural identity Suicide Prevention in New Zealand 51 supportive family/whānau, hapū and iwi responsibility for children social support holding attitudes against suicide (Fergusson et al 2003; Coggan and Bennett 2002). For older adults, a range of potentially protective factors have been suggested, including: a confiding, supportive relationship social support, social connectedness and interaction, including participation in organisations and having a hobby good coping and adaptive skills good physical and mental health adequate pain relief good palliative care, and treatment of depression for those with terminal illnesses early, adequate and sustained treatment and management of depression strong religious and/or spiritual values adequate support following bereavement recognition of, and respite from, family discord and conflict restricted access to means of suicide, especially guns, for older adult males (Conwell 2001; Pearson and Conwell 1995; Szanto 2003; Caine and Conwell 2001; Waern et al 2002, 2003; Rubenowitz et al 2001). Population-attributable risk While the large volume of information from social and psychiatric epidemiological, genetic and biological research now gives a generally coherent and consistent picture about the risk factors for suicidal behaviour, there is still debate about the underlying causes of suicidal behaviour, the ways in which these risk factors interact, and the life pathways to suicide and suicide attempt. Furthermore, the linkages between macrosocial, cultural and macroeconomic factors and individual suicidal behaviours still remain unclear. Nevertheless, the research evidence clearly suggests that the causation of suicide is multifactorial and complex, so there seem to be a range of different populations and sites for potential interventions to prevent or reduce suicide. Moreover, suicide is an emotive and tragic issue that has captured public attention, with the result that a range of public groups have developed a series of suicide programmes which, although well intentioned, are supported more by advocacy than evidence. Such programmes may have unintended iatrogenic effects. This raises the issue of how best to make decisions about what types of suicide prevention programmes to support. 52 Suicide Prevention in New Zealand One means of addressing this issue is to use the findings from risk factor research to compute the population-attributable risk (PAR) (Bruzzi et al 1985; Benichou 1991). The PAR gives an estimate of the percentage reduction in the rate of suicide that would occur if: the association between the risk factor and suicide represents the causal contribution of the risk factor the risk factor were eliminated from the population. Calculation of PAR estimates for a range of risk factors can give some sense of the relative importance of various risk factors to rates of suicidal behaviour, and, in turn, indicate the relative importance of various approaches to suicide prevention. Unfortunately, many studies do not report PAR estimates or the information necessary to compute these estimates. Also, in many cases the odds ratio estimates required to compute the PAR statistics have not been adjusted for confounding, and thus may overestimate the causal contributions of risk factors. Nevertheless, a series of studies has calculated PARs for a range of risk factors for suicidal behaviour. In one of the first studies to report the PAR statistic, Beautrais, Joyce, Mulder et al (1996: 1013) suggested that the: elimination of all mental disorders considered in the analysis (mood disorders, substance use disorders, anxiety disorders, antisocial behaviours, eating disorders, and non-affective psychosis) would result in a reduction of 76.2% in the total number of suicide attempts. In a further study, Beautrais (Beautrais 1999) estimated PARs for three widely reported case control studies of youth suicidal behaviour (Shaffer et al 1996; Gould et al 1996; Gould et al 1998; Brent, Perper, Moritz, Allman et al 1993; Brent, Perper, Moritz, Baugher et al 1993; Brent, Johnson et al 1993; Brent, Perper, Moritz, Baugher, Roth et al 1993; Beautrais, Joyce, Mulder et al 1996; Beautrais et al 1998a, 1998b, 1998c; Beautrias 1998). From each of these studies it was possible to obtain a series of PAR estimates for specific risk factors. All three studies were consistent in generating PAR statistics that suggested that mental health factors (including mood disorders, substance use disorders, antisocial disorders, previous suicidal behaviour and previous psychiatric care) made the strongest and most consistent contributions to the risk of suicidal behaviour. More specifically, these estimates make it clear that mood disorders, previous suicidal behaviour and previous psychiatric history make strong contributions to the risk of suicidal behaviour in the population, with substance abuse and antisocial behaviours making smaller but consistent contributions to suicide risk (Beautrais 2000b). Subsequently, Australian researchers reported PARs for suicidal ideation and suicide attempt using data from the large Australian National Survey of Mental Health and Wellbeing. This population-based study estimated that the PARs for mood disorders in suicidal ideation and suicide attempt were around 40%, implying that elimination of mood disorders would reduce suicidal ideation and suicide attempt by almost half (Pirkis et al 2000). Similar findings have been reported by Goldney et al (2000). In a population study they found that major depression made the largest contribution to risk of suicidal ideation, with a PAR of 57%. Recently, findings from a national register-based nested case control study of suicide in Denmark showed that a history of hospitalisation for mental disorder was associated with the highest populationattributable risk for suicide (40%) (Qin et al 2003). By comparison, PARs for unemployment, having a sickness-related absence from work, being in the lowest income group, and being on a disability or age pension were 10% or lower. Suicide Prevention in New Zealand 53 The perspective provided by studies that have estimated PARs suggests that although a wide range of personal, social, family and related factors make contributions to risks of suicidal behaviour, by far the largest contributions come from mental health measures; in particular, measures of mood disorders, previous suicidal behaviour, mental health history and prior treatment. The clear implication of these results is that the major focus of suicide prevention efforts should be directed at minimising rates of psychiatric disorders and addressing the risk factors and life pathways that lead to these disorders. The individual prediction of suicide on the basis of risk factor data is not practicable, simply because suicide and serious suicide attempts occur so infrequently in the general population. The low base rate of suicidal behaviour in turn imposes limitations on predictive power. These considerations suggest that the best application of existing research to risk factors for suicide is for identifying effective population-based approaches for minimising suicide risk rather than for predicting individual suicide risk. For example, rather than attempting to identify those at risk of making suicide attempts, it may be better to implement broad population-based strategies aimed at the better recognition, treatment and management of depression and substance abuse, which are frequent precursors of suicide. To examine these issues, the discussion below focuses on both population-level and targeted interventions, examining those interventions that have shown some evidence of efficacy or effectiveness. Each approach is illustrated by examples. To provide a framework for this review, the prevailing prevention model of universal, selective and indicated (USI) interventions is used (Mrazek and Hagerty 1994). Within this model, universal programmes are those that address the general population regardless of risk status, selective programmes address high-risk sub-groups within the population, and indicated programmes address high-risk individuals within the population. Universal population-based programmes As noted above, universal strategies focus on the population as a whole, without targeting highrisk individuals. A series of population-based approaches has been shown to reduce suicide or has shown promise of effectiveness. These approaches include: restricting access to means of suicide macrosocial interventions public awareness education and mental health literacy careful media coverage of suicide improving control of alcohol promoting mental health/resilience national suicide prevention programmes community-level suicide prevention programmes school-based suicide awareness and peer support programmes. 54 Suicide Prevention in New Zealand Restricting access to means of suicide The WHO has placed strong emphasis on restricting access to means of suicide as a major approach to suicide prevention (Bertolote 2000). Of the six basic steps for the prevention of suicide identified by the WHO, four relate to means restriction (guns possession control, detoxification of domestic gas, detoxification of car emissions, control of toxic substances availability). The findings on which the WHO approach is based span the following examples. Detoxification of domestic gas in the United Kingdom led to a decrease in suicides by this method, and a reduction in total suicides (Kreitman 1976). The reduction in total suicides endured for 15 years before other methods were substituted for domestic gas (McClure 1984). Various levels of restriction of access to guns are associated with reductions in suicides by firearms. In some cases, guns are not replaced with other methods of suicide, leading to reductions in the total number of suicides (Loftin et al 1991). Imposing controls on emissions of carbon monoxide in vehicle exhaust gas has been shown to reduce suicides by that method (Clarke and Lester 1987; Lester 1989). Preliminary findings following the introduction of legislation designed to reduce the pack size of analgesics especially paracetamol, which are potentially toxic and fatal in overdose suggest reductions in both morbidity and mortality associated with this method (Hawton et al 2001, 2003; Hawton 2002). Erecting barriers at specific sites which have become identified as suicide jumping sites decreases suicides from those sites (O’Carroll and Silverman 1994). Macrosocial interventions Research evidence suggests consistent linkages between family, social and economic disadvantage and suicide risk. This observation has led to frequent calls for macrosocial and macroeconomic policies to improve social equity in a range of areas, including enhancing educational and employment opportunities and reducing poverty, in order to reduce the fraction of the population at risk of developing mental disorders and encountering the stressful life circumstances associated with suicide. The strength of this approach is that is argues for the creation of a macrosocial environment in which more targeted approaches to suicide prevention will have the best opportunity to be effective. However, a common distortion of this approach is the view that improved economic, employment or educational conditions can, in and of themselves, resolve individual problems. In work commissioned by the European Union, Rutter and Smith (1995) have pointed out that youth suicide rates in Europe rose from 1950 onwards, despite increasing rates of employment, clearly indicating that there are other risk factors at play besides the solely economic. Although there is no research evidence to clearly demonstrate that achieving social equity in targeted areas, including, for example, poverty, employment, racism and gender equity, reduces suicide, nevertheless it seems sensible to advocate for macrosocial changes in such areas in order to provide the optimal environment for more targeted prevention programmes for high-risk groups or individuals to have the best chance of success. In addition to social equity issues, there are general population strategies in other social policy areas that may minimise suicidal behaviour. These address suicide-inclusive rather than suicide-specific risk factors (Burns 2000) and include social welfare, strengthening families, reducing family violence and child abuse, and providing adequate care including mental health care for children who need welfare service and care. Suicide Prevention in New Zealand 55 Public awareness education and mental health literacy There is considerable evidence that members of the public have generally poor or limited knowledge about mental disorders, in particular, depression (Jorm et al 2000; Goldney et al 2001; Paykel et al 1997). The term ‘mental health literacy’, defined as ‘knowledge and beliefs about mental disorders which aid their recognition, management or prevention’ (Jorm et al 1997: 182), has recently come into widespread use to describe this situation. Improving the public’s mental health literacy has been recognised as an important public health goal, one which may make a contribution to suicide prevention by changing public and health care provider recognition and perceptions of, and attitudes towards, mental illnesses and their treatment and management (Regier et al 1988; Jane-Llopis et al 2003). For example community-based education programmes and mass-media campaigns may reduce levels of public stigma and discrimination and contribute to more supportive attitudes. Currently in New Zealand, a media campaign, Like Minds Like Mine, is contributing to this change (Ministry of Health 2003). For example, enhanced public knowledge about signs and symptoms of depression, and its treatment and management, may encourage more people to recognise depression (in themselves and others), to seek treatment for themselves, and to support others to get treatment. Such enhanced public understanding of depression was the aim of the British Defeat Depression Campaign (Paykel et al 1997, 1998). This campaign included informational materials, media publicity and dissemination of information, and efforts to improve GPs’ ability to identify, treat and manage depression. The programme was evaluated by surveys of public attitudes, which showed significant improvements in some areas (eg, understanding the biological causes of depression), but it was unable to influence public perceptions in other areas. Public views of antidepressant medications as addictive, for example, remained unchanged despite the educational campaign. While the national suicide rate fell by a little more than 10% during the five years of the Defeat Depression campaign, the extent to which this could be attributed to the programme remains unclear, since the design of the evaluation permitted no more than a limited number of outcome measures to be assessed. More recently, a depression awareness campaign was instigated in Nuremberg. This campaign included dissemination of information to the public, improved training for GPs, and the development of self-help support groups. Preliminary findings suggest that the number of suicide attempts fell in Nuremberg compared with a control city without a depression awareness campaign (preventing suicide by improving the care of patients suffering from depression 2003). A recent meta-analysis reported a weighted mean effect size of 0.22 (equivalent to an 11% improvement in the intervention compared to the control groups) for depression prevention programmes (Jane-Llopis et al 2003). Although both universal and treatment programmes were included in this meta-analysis, the effect size for universal programmes is likely to be smaller than the mean effect size because the population such programmes reach includes people who may or may not be at risk of depression. However, there is strong evidence to suggest that depression is substantially undertreated (Hirschfeld et al 1997), and strategies to enhance public understanding of depression may result in more people being treated, with a consequent reduction in the fraction of the population with depression and thereby at risk of suicide. More generally, we know very little about the impacts of public health messages about suicide. Certainly, research evidence relating to media coverage of suicide suggests the need for a very 56 Suicide Prevention in New Zealand cautious approach to this issue. This is an area in which further research and evaluation are required to determine the safest and most effective approaches to improving mental health literacy about mental illness and suicide, and to develop public health messages about mental illness and suicide prevention (public awareness campaigns to prevent suicide 2003). Media coverage of suicide A number of studies have reviewed the impact of various types of media coverage and fictional and non-fictional portrayal of suicide on actual suicide rates (Pirkis and Blood 2001; Gould et al 2003; Jamieson 2003; Velting and Gould 1997; Hawton and Williams 2002; Schmidtke and Schaller 2000). These studies present substantial evidence to suggest that certain ways of presenting and portraying suicide in the media appear to provoke suicidal behaviour in vulnerable individuals. However, there is less knowledge about the exact conditions under which imitative behaviour occurs. This evidence has led to most national suicide prevention strategies developing guidelines for media reporting and coverage of suicide (Ministry of Health 1999b; WHO 2000).1 Most of these guidelines include two approaches: information and recommendations designed to educate and influence journalists to report and cover suicide issues in ways that minimise the risk of imitative suicidal behaviour education for those in health and related professions to enable them to better respond to journalists’ approaches for information and stories about suicide. Despite the proliferation of media guidelines, there have been few evaluations of the impact of such guidelines. However, Michel et al (2000) have reported that the introduction of media guidelines in Switzerland resulted in fewer sensationalised stories about suicide. Improving control of alcohol There is substantial evidence to suggest that in many countries alcohol makes a strong contribution to suicidal behaviours. This contribution comes from two sources: alcohol abuse and dependence are mental disorders, which increase the risk of suicidal behaviour the disinhibiting and facilitating effects of acute alcohol intoxication increase the likelihood of impulsive and aggressive suicide attempts. 1 See www.afsp.org/education/recommendations/index.html Suicide Prevention in New Zealand 57 National strategies that seek to improve control of alcohol may reduce suicidal behaviour by decreasing the risk of acute alcohol intoxication, and by reducing the fraction of the population with alcohol use disorders. There is evidence from a study of state minimum drinking-age policies that higher legal drinking ages are associated with lower suicide rates in young people (Birckmayer and Hemenway 1999). The pronounced decline in suicide rates during perestroika in the former USSR has been attributed to the strong anti-alcohol policy introduced during this period. Although the policy was introduced to address the problem of widespread alcoholism, its impact on suicide rates was so striking that it has been described as one of the most effective suicide prevention programmes in modern history (Wasserman and Varnik 1998; Wasserman et al 1998). Finland has included clear proposals to address alcohol abuse as part of its national suicide prevention strategy (National Research and Development Centre for Welfare and Health 1993). Promoting mental health / resilience WHO (1993), the United Nations and many national suicide prevention strategies including, for example, those of the United States (US Department of Health and Human Services 2001), Sweden (National Council for Suicide Prevention 1995) and New Zealand (Ministry of Youth Affairs et al 1998), embrace mental health promotion as an approach to suicide prevention. These promotional activities include programmes to enhance factors that might protect against suicide or mitigate the effects of risk factors. Such approaches can be applied nationally, or within communities or workplaces. The Finnish National Suicide Prevention Programme, for example, includes a public education campaign to enhance personal resources and coping abilities, promote good parenting styles, and prepare people for retirement (National Research and Development Centre for Welfare and Health 1993). National suicide prevention programmes Although a number of countries now have national suicide prevention strategies, in most cases their development has been too recent for their impact to have been assessed. However, Finland was the first country to develop a national suicide prevention programme, and in that country the strategy has been systematically evaluated. The evaluation shows that after an initial increase when the strategy was implemented, suicide rates fell to 9% less than the original rate. The research component of the strategy, which included a national psychological autopsy study, stimulated interest in suicide and suicide prevention among health and related professionals and in the general population. Implementation of the strategy had more positive impacts on organisations and professionals in the social services than the health sector. However, suicide prevention programmes did not appear to have been embedded well enough within local government organisations and professional organisations to ensure their survival. Two particular issues (suicide in older adults and addressing access to means of suicide) were assessed as not having been addressed well in the national strategy, and medical knowledge about suicide was not conveyed to the public well enough to change sociocultural views of the aetiology of suicidal behaviour (Kerkhof 1999). 58 Suicide Prevention in New Zealand More recently, Sri Lanka developed a national suicide prevention strategy in response to a sixfold increase in suicide rates between 1950 and 1985. The strategy focused on decriminalising suicide, reducing access to pesticides (a common means of suicide), minimising sensationalistic media coverage of suicide, and improving mental health services. From 1995 to 2000 the number of suicides nationally decreased from 8514 to 5412. Although the decrease cannot be unequivocally attributed to the national strategy, it seems reasonable to assume that the dramatic reversal in suicides is linked, to some extent, with the measures introduced as part of the strategy. Although most national suicide prevention strategies include an intention to evaluate the programme, the American Foundation for Suicide Prevention has recently begun an international study of national strategies, which aims to identify the effective components of these strategies and determine useful ways of evaluating and comparing strategies. Community-level suicide prevention programmes Recently, the United States Air Force (USAF) Suicide Prevention Programme has received considerable publicity as an example of a population-based suicide prevention programme (Knox et al 2003). In this programme, a combined effort by community agencies was followed by a significant reduction in suicides among USAF personnel. The programme focused on public education, promoting social support and help-seeking, improved surveillance of suicidal behaviour, critical incident stress management and integration of community health and support services. Although various advantageous features of the USAF institution (including, for example, pre-screening for mental disorders, a hierarchical structure to enforce treatment, and a range of community gatekeepers) clearly enhanced the implementation and penetration of the programme, the programme still has broad principles that make it potentially transferable to civilian communities. School-based suicide awareness and peer support programmes There are a range of school-based didactic and peer support suicide awareness programmes based on the premise that young people are more likely to divulge suicidal ideation to peers than adults (Hazell and King 1996; Kalafat and Elias 1994). However, these programmes have been controversial, with some evaluations showing improvements in knowledge, attitudes and helpseeking (Ciffone 1993; Kalafat and Elias 1994; Silbert and Berry 1991) and others finding no gains, or undesirable effects, including more maladaptive behaviour, reluctance to refer friends for help, and a potentially harmful change in attitudes (Vieland et al 1991; Shaffer 1991; Overholser et al 1989; Kalafat and Elias 1994). On balance, there is currently insufficient evidence of safety to support suicide awareness programmes in schools (Guo and Harstall 2002; Bennett et al 2003). Suicide Prevention in New Zealand 59 Selective programmes for high-risk sub-groups Selective programmes focus on high-risk subgroups within the population. The following selective programmes have been shown to reduce suicide or have shown promise of effectiveness: improving access to mental health services, crisis centres and telephone hotlines enhancing treatment and support screening programmes informational and educational programmes for professional groups school-based skills promoting programmes. Improving access to mental health services An approach to suicide prevention advocated in most national suicide prevention strategies focuses on improving access to mental health care. This approach is underwritten by research evidence which suggests that most of those who die by suicide have mental disorders at the time of their death, which are often unrecognised or undertreated (Hirschfeld et al 1997). For example, Appleby and Shaw (1999) found that only 24% of those who died by suicide had seen mental health professionals in the year before their death. A lack of continuity of clinical care has been reported in young people who die by suicide (Hulten and Wasserman 1998). In the well-reported Gotland study, Rutz and colleagues showed lower suicide rates among females, fewer sick leave days for depression, increased numbers of anti-depressant prescriptions, and reduced inpatient care for depression after a programme to train GPs to better recognise and treat depression (Rutz, von Knorring et al 1992; Rutz, Carlsson et al 1992). There has been debate about the implications of this study for suicide prevention, as the suicide rate may have been falling prior to the intervention starting, so it will be important to attempt to replicate this approach, preferably using larger communities than Gotland. Crisis centres and telephone hotlines Since the majority of suicide attempts are precipitated by stressful life events, crisis centres and telephone hotlines were developed to provide support in times of crisis. However, several evaluations of crisis hotlines have failed to find clear evidence of their efficacy in reducing suicidal behaviour (Dew et al 1987; Shaffer et al 1988; Seeley 1997). However, one analysis of a number of studies did report a small positive effect (Lester 1997). Enhancing treatment and support Several treatment approaches offer enhanced treatment and support for people who are depressed and/or suicidal. These programmes incorporate elements of both mental health and community care. For example, Katon and colleagues evaluated an intervention in which GPs and mental health professionals collaborated to manage patients with depression (Katon et al 1996, 1997). Findings suggested increased patient satisfaction with care, improved compliance with medication and reduction in depressive symptomatology. 60 Suicide Prevention in New Zealand In Italy, de Leo et al (2002) introduced a home-based telephone support system for older people who had been identified by social services and other providers as being at risk of suicide. Evaluation of this programme suggested lower suicide rates, reduced demand for home visits by family doctors, and reduced hospital admissions and depressive symptomatology among users of the service compared with a wait-list comparison group. A similar approach to supporting depressed and potentially suicidal older people makes use of individuals who come into contact with older adults in their work (eg, meter readers, bank staff, postal delivery staff). These ‘community gatekeepers’ have been provided with a small amount of training and education to enable them to refer to appropriate clinical resources those older people they regard as dependent, socially isolated and at risk of suicidal behaviour (Florio et al 1997; Quinnett 1995). Although these types of programmes have not been formally evaluated, they offer potentially useful models for developing relatively low-cost interventions for older adults. In the US a collaborative care trial is under way to determine whether using a depression health specialist in primary health care settings can reduce rates of depression, hopelessness and suicidal ideation in older patients with histories of depression (Reynolds et al 2001; Bruce et al 2004). While there is a need to develop innovative interventions and models of care, and to carefully evaluate these promising approaches in real-world settings with individuals who may be suicidal, there are ethical difficulties in conducting such research. Previously there has been a tendency to exclude suicidal individuals from such trials, which means the results have limited generalisability to clinical and real-world populations. More recently some promising approaches to address issues of the tension between ethics and research design have been instituted (Reynolds et al 2001). Screening programmes In an effort to avoid the risks shown by some school-based suicide awareness programmes, some researchers have focused on developing screening programmes to identify young people suffering from mental illness and at risk of suicide. Those identified are then linked to mental health services. The Columbia TeenScreen is an example of this type of programme, which can be administered to young people in schools or community settings (Shaffer et al 2004). Participating voluntarily, young people use confidential, computer-based questionnaires that have been shown to be effective in identifying individuals with mental illness and at risk of suicide. The concept of mental health screenings has been endorsed by the (US) President’s New Freedom Commission on Mental Health, which nominated TeenScreen as a model programme.2 2 See www.teenscreen.org/newsroom/downloads/Annualreport3.pdf, accessed 5 May 2004. Suicide Prevention in New Zealand 61 Informational and educational programmes for professional groups Most national suicide prevention strategies include programmes designed to enhance the ability of various professional groups to better identify, treat and manage depression and suicidal behaviour. These professional groups include teachers and school counsellors, GPs, social workers, and staff in emergency departments and acute mental health settings. For GP training programmes, both supportive and negative findings have been reported. As noted above, the Gotland study raised the possibility that training GPs may successfully reduce rates of suicidal behaviour (Rutz, von Knorring et al 1992). In Australia, training of GPs resulted in an improvement in the rate of GP inquiry about suicidal ideation and identification of suicidality (Pfaff et al 2001). Other programmes examining the possibility of enhancing the detection of suicidal ideation among adults by GPs and other doctors have suggested generally poor results (Lin et al 1989; Carson et al 2000). There is a need for further, large-scale evaluations of such programmes using a range of outcomes measures. The impact on suicidal behaviour of the introduction of guidelines and information programmes for other professional groups has not been well evaluated. School-based skills-promoting programmes Given the difficulties with suicide awareness programmes in schools, a range of skill-enhancing and competency-promoting programmes have been developed as a safer approach to addressing suicide in schools. These programmes focus on increasing self-esteem, and improving coping and problem-solving skills. It is hoped that enhancing these skills may protect vulnerable young people against a range of adverse outcomes, including suicidal behaviour, depression and substance abuse. Eggert and colleagues, for example, have shown reductions in risk factors and enhancement of protective factors among young people at risk of school failure or dropout who were provided with social support and skills training (Eggert et al 1995; Thompson et al 2000; Return visits to the emergency department after a suicide attempt 2001). Indicated programmes for high-risk individuals Indicated programmes target individuals within the population who are at high risk of further suicide attempt behaviour. Such groups include those who have made a suicide attempt, and those recently discharged from inpatient psychiatric care (Beautrais 2004a, 2004b; Owens et al 2002; Appleby 2000; Appleby and Shaw 1999; Appleby et al 1999). However, there is little empirical evidence for specific treatments or interventions for people who have made a suicide attempt to reduce the risk of further suicidal behaviour. In general, research in this area has been limited by single studies, and by studies with small numbers of highly selected participants. There is a need for randomised controlled studies of therapies and interventions that have shown promising findings, and for the replication of single studies that have shown effectiveness (Hawton et al 2000). The following interventions have shown some effectiveness or promise of effectiveness: pharmacological approaches behavioural therapies. 62 Suicide Prevention in New Zealand Pharmacological and physical approaches A limited number of psychopharmacological treatments for specific mental illnesses have been shown to reduce suicidality in patients with these illnesses. Specifically, long-term maintenance therapy with lithium has been shown to reduce suicide and suicide attempts in patients with recurrent bipolar disorder and major depressive disorder (Tondo et al 2003; Tondo, Hennen et al 2001; Tondo, Ghiani et al 2001; Baldessarini et al 2001, 2002, 2003). The antipsychotics clozapine, and perhaps olanzapine, have been shown to reduce suicide and suicide attempts in patients with schizophrenia (Meltzer and Okayli 1995; Meltzer et al 2003). Electroconvulsive therapy (ECT) has been used with selected patients who are acutely suicidal, and has been shown to decrease short-term suicidal ideation (Rich et al 1986; Prudic and Sackheim 1999; Kellner et al submitted). However, ECT has not been shown to decrease longerterm suicide attempt or suicide risk. There is no evidence from randomised controlled trials that antidepressant therapy is associated with reductions in suicide or suicide attempts (Baldessarini et al 2002; Khan et al 2000, 2001, 2003), although the numbers needed to demonstrate a reduction would be prohibitive, and people with suicidal ideation are often excluded from such trials on ethical grounds. Similarly, there is no evidence that treatment with mood-stabilising anti-convulsant drugs reduces suicidality in patients with mood disorders (Jacobs et al 2003), and no evidence that treatment with antianxiety agents reduces suicide or suicide attempts in patients with depression and anxiety (Khan et al 2002). Nevertheless, these treatments have all demonstrated efficacy in terms of treating the disorders in question. Behavioural therapies A series of behavioural therapies and approaches have been shown to reduce suicidal behaviour. Cognitive behavioural therapy (CBT) and interpersonal psychotherapy (IPT) have both been shown to reduce the likelihood of suicide attempt and of symptoms of depression in patients who had attended emergency departments for suicide attempts (Hawton et al 2000). Dialectical behavioural therapy (DBT) has been shown to reduce suicidal behaviour among patients with borderline personality disorder while they are in therapy (Linehan 1993). Provision of an emergency ‘ready access’ card suggests a trend to reduced suicidal behaviour among patients who have attended an emergency department for attempted suicide (Morgan et al 1993; Cotgrove et al 1995; Motto and Bostrom 2001; Postcards from the edge 2003). Other aspects of psychological intervention Having a full psychosocial assessment (which could result in appropriate follow-up after a suicide attempt) has been associated with reduced risk of repeated suicide attempt (Kapur et al 2004; Hickey et al 2001). An important aspect of these studies is that the intervention being tested was simply a standard thorough clinical assessment, which was not routinely being provided for these patients. There is also some evidence that seeing the same therapist after discharge is associated with higher rates of attendance at outpatient appointments, and with higher rates of taking medications (Hawton et al 2000). Suicide Prevention in New Zealand 63 7 Conclusion Recent research into suicide clearly and consistently shows that it is a complex phenomenon with multiple causes, which nevertheless seem mostly to have a common pathway via mental disorder. This evidence suggests there is no single programme for suicide prevention that in and of itself will achieve a significant reduction in suicide rates. Rather, it appears likely that a multisectoral approach is needed in which multiple programmes are developed in a number of different areas which contribute to suicide risk, with, perhaps, small gains in each of these areas aggregating to make a substantial overall impact on suicide rates. Although research into suicide has developed a relatively clear if by no means complete picture of the risk and protective factors that contribute to suicidal behaviours, less is known about translating this knowledge into effective prevention programmes. Furthermore, many of the suggested programmes have been less effective than expected, leading some authors to express considerable pessimism about the prospects of suicide prevention (Gunnell et al 1994). However, such an assessment may be overly pessimistic and that there are a number of areas that show promise as programmes for suicide prevention. The approaches that stand out include: population-based programmes that address depression and alcohol use promoting mental health and problem-solving skills, in the community at large and in school students community-level suicide prevention programmes using the USAF model educational programmes for professionals such as GPs to enhance their ability to identify, treat and manage depressed and suicidal individuals programmes that integrate and enhance community and primary care psychotherapeutic and pharmacotherapeutic treatments for mood disorders and other mental illnesses linked with suicidality. At the same time, rigorous and compelling evaluations of the efficacy, effectiveness and costeffectiveness of these programmes remain to be conducted. These considerations suggest that the major tasks for suicide prevention in the 21st century are: continuing development of the promising lines of suicide prevention greater investment in evaluating the efficacy and effectiveness of these programmes, with the acknowledgement that because of low base rates randomised controlled trials may not be feasible the development of innovative programmes at population levels addressing both high-risk groups and high risk in individuals, ensuring equitable outcomes for different population groups. These activities need to be conducted in parallel with further investigation into the mechanisms by which broader social factors may shape the more proximal risk factor profiles of those who subsequently die by suicide. Advances in behavioural genetics and in the methods employed by social epidemiology both have great potential to yield benefits in this area. It must not be 64 Suicide Prevention in New Zealand forgotten that risk factor profiles include resilience (Silverman 2004), and that both risk and resilience factors may be either fixed or modifiable, and either proximal or distal in the causal chain. Risk and resilience profiles also occur in the context of social and psychological development over the life span, and research in developmental psychopathology is rapidly increasing the available evidence on where it may be productive to target early interventions to prevent the development of mental illness in adolescence and adulthood. Rigorous studies of the effects of characteristics of society on health require large numbers of participants and the ability to collect data over long periods, both of which require significant commitment by research funding agencies and governments. Often natural experiments do occur, and researchers (and funders) need to be ready to take early advantage of these so that opportunities that cannot be replicated are not lost. Importantly, it seems likely that features of society that confer additional risk of one kind of health problem might also confer increased risk of other health problems. Although it may be difficult to draw direct links between such high-level factors and suicide rates, there may be beneficial effects on a range of health domains including mental health. In the area of social interventions to prevent suicide, it may be that suicide alone cannot be the only outcome measure. In developing models of suicide causation and prevention it is important not to confuse heuristic models with explanatory models. The latter can only be generated by evidence, while the former are a critical part of formulating and refining the enquiry process. In order for these tasks to be developed, it will be important for researchers, policy makers and those delivering suicide prevention programmes not to succumb to what has been described as ‘epistemological closure’ (Rogers and Pilgrim 2003:166), while still delivering prevention initiatives which balance the need for the wise investment of resources on the basis of a generally agreed type of acceptable evidence. Social epidemiology is an intellectual framework as well as an applied science. It applies traditional epidemiological methods combined with the increased power of innovations in statistical modelling to broad questions about the causes of health and disease. It considers the characteristics of individuals, but also the characteristics (especially the social characteristics) of the populations in which the individuals live. For these reasons it is a useful framework within which to consider questions about the aetiology and prevention of suicide. It provides an overarching perspective from which to view and integrate the various bodies of thought and knowledge about suicide causation and prevention. For New Zealand, this report provides important contextual information to allow the All Ages Suicide Prevention Strategy and its associated Action Plan to be delivered on the basis of the best existing evidence. It should be seen as complementary to existing evidence on interventions for individual-level risk factors. It is to be hoped that New Zealand suicide researchers and prevention workers will continue to cast a wide net in the search for increased understanding of the causal pathways to suicide, while maintaining a critical stance on what constitutes acceptable evidence for action. Suicide Prevention in New Zealand 65 References Ajwani S, Blakely T, Robson B, et al. 2002. Unlocking the Numerator-denominator Bias for the 1980s and 1990s. NZCMS Technical Report No. 4. Wellington: Department of Public Health, Wellington School of Medicine and Health Sciences, University of Otago. Ajwani S, Blakely T, Robson B, et al. 2003a. Decades of Disparity: Ethnic mortality trends in New Zealand 19801999. Wellington: Ministry of Health and University of Otago. Ajwani S, Blakely T, Robson B, et al. 2003b. Unlocking the numeratordenominator bias III: adjustment ratios by ethnicity for 19811999 mortality data: the New Zealand Census Mortality Study. New Zealand Medical Journal 116: U456. Althaus D, Schmidtke A, Niklewski G, et al. 2003. Preventing suicide by improving the care of patients suffering from depression: results of the ‘Nuremberg Alliance Against Depression’ (NAD). Paper presented at Crossing Borders in Suicide Prevention: From the Genes to the Human Soul, XXII World Congress of the International Association for Suicide Prevention (IASP), 1014 September, Stockholm, Sweden. Anderson J, Huppert F, Rose G. 1993. Normality, deviance and minor psychiatric morbidity in the community: a population-based approach to General Health Questionnaire data in the Health and Lifestyle Survey. Psychological Medicine 23(2): 47585. Andrews G. 2001. Should depression be managed as a chronic disease? British Medical Journal 322(7283): 41921. Anleu S. 1998. The medicalisation of deviance. In: J Germov (ed). Second Opinion: An introduction to health sociology. Oxford: Oxford University Press. Appleby L. 2000. Prevention of suicide in psychiatric patients. In: K Hawton, K van Heeringen (eds). The International Handbook of Suicide and Attempted Suicide. New York: John Wiley and Sons. Appleby L, Dennehy JA, Thomas CS, et al. 1999. Aftercare and clinical characteristics of people with mental illness who commit suicide: a case-control study. Lancet 353: 1397400. Appleby L, Shaw J. 1999. Suicide within 12 months of contact with mental health services: national clinical survey. British Medical Journal 318: 123539. Baldessarini RJ, Hennen J, Kwok KW, et al. 2002. Suicidal Risk and Assessment and Anti-depressant Treatment: A meta-analysis. Unpublished manuscript. Baldessarini RJ, Tondo L, Hennen J. 2001. Treating the suicidal patient with bipolar disorder: reducing suicide risk with lithium. Annals of the New York Academy of Sciences 932: 2438. Baldessarini RJ, Tondo L, Hennen J. 2003. Lithium treatment and suicide risk in major affective disorders: update and new findings. Journal of Clinical Psychiatry 64(suppl 5): S4452. Barber J. 2001. Relative misery and youth suicide. Australian and New Zealand Journal of Psychiatry 35(1): 4957. Baume P, Cantor C, McTaggert P. 1998. Suicides in Queensland: A comprehensive study. Brisbane: Australian Institute for Suicide Research and Prevention. Beaglehole R, Bonita R. 1997a. Evolution of epidemiology: ideas and methods. Chapter 4 in: Public Health at the Crossroads. Cambridge: Cambridge University Press. 66 Suicide Prevention in New Zealand Beaglehole R, Bonita R. 1997b. Public Health at the Crossroads. Cambridge: Cambridge University Press. Beautrais AL. 1996. Serious suicide attempts in young people: a case control study. PhD dissertation. University of Otago, Dunedin. Beautrais AL. 1998a. A Review of the Evidence: In our hands The New Zealand youth suicide prevention strategy. Wellington: Ministry of Health. Beautrais AL. 1998b. Risk factors for serious suicide attempts among young people: a case control study. In: RJ Kosky, HS Eshkevari, RD Goldney, et al (eds). Suicide Prevention: The global context. New York: Plenum Press. Beautrais AL. 1998c. Risk factors for suicide over the life course. Paper presented at American Association of Suicidology (ASS) Conference, Washington, DC. Beautrais AL. 1999. Risk Factors for Suicide and Attempted Suicide Among Young People. In Commonwealth Department of Health and Aged Care, National Youth Suicide Prevention Strategy – Setting the evidence-based research agenda for Australia (a Literature Review). Canberra: Commonwealth of Australia. URL: www.health.govt.au/nhmrc/publications/pdf/mh12.pdf Beautrais AL. 2000a. Methods of youth suicide in New Zealand: trends and implications for prevention. Australian and New Zealand Journal of Psychiatry 34(3): 41319. Beautrais AL. 2000b. Risk factors for suicide and attempted suicide among young people. Australian and New Zealand Journal of Psychiatry 34(3): 42036. Beautrais AL. 2000c. Risk Factors for Suicide and Attempted Suicide Amongst Young People. Report prepared for the National Health and Medical Research Council. Canberra, Australia: National Health and Medical Research Council Beautrais AL. 2001a. Effectiveness of barriers at suicide jumping sites: a case study. Australian and New Zealand Journal of Psychiatry 35: 55762. Beautrais AL. 2001b. Suicides and serious suicide attempts: two populations or one? Psychological Medicine 31(5): 83745. Beautrais AL. 2002. A case control study of suicide and attempted suicide in older adults. Suicide and Life-Threatening Behavior 32(1): 19. Beautrais AL. 2003a. Suicide in New Zealand I: time trends and epidemiology. New Zealand Medical Journal 116(1175). URL: www.NZMA.org.nz/journal/116-1175/460/ Beautrais AL. 2003b. Suicide in New Zealand II: a review of risk factors and prevention. New Zealand Medical Journal 116(1175). URL: www.NZMA.org.nz/jpurnal/116-1175/461 Beautrais AL. 2004a. Further suicidal behaviour amongst medically serious suicide attempters. Suicide and Life Threatening Behavior 34(1): 111. Beautrais AL. 2004b. Subsequent mortality in medically serious suicide attempts: a five-year follow-up. Australian and New Zealand Journal of Psychiatry 37(5): 5959. Beautrais AL, Horwood LJ, Fergusson DM. 2004. Knowledge and attitudes about suicide in 25-yearolds. Australian and New Zealand Journal of Psychiatry 38(4): 2605. Suicide Prevention in New Zealand 67 Beautrais AL, Joyce P, Mulder R, et al. 1996a. Prevalence and comorbidity of mental disorders in persons making serious suicide attempts: a case control study. American Journal of Psychiatry 153: 1009–14. Beautrais AL, Joyce PR, Mulder RT. 1996b. Risk factors for serious suicide attempts among youths aged 13 through 24 years. Journal of the American Academy of Child and Adolescent Psychiatry 35(9): 117482. Beautrais AL, Joyce PR, Mulder RT. 1997. Precipitating factors and life events in serious suicide attempts among youths aged 13 through 24 years. Journal of the American Academy of Child and Adolescent Psychiatry 36(11): 154351. Beautrais AL, Joyce PR, Mulder RT. 1998a. Psychiatric contacts among youths aged 13 through 24 years who made serious suicide attempts. Journal of the American Academy of Child and Adolescent Psychiatry 37(5): 50411. Beautrais AL, Joyce PR, Mulder RT. 1998b. Psychiatric illness in a New Zealand sample of young people making serious suicide attempts. New Zealand Medical Journal 111(1060): 448. Beautrais AL, Joyce PR, Mulder RT. 1998c. Youth suicide attempts: a social and demographic profile. Australian and New Zealand Journal of Psychiatry 32(3): 34957. Beautrais AL, Joyce PR, Mulder R. 2000. Unmet need following serious suicide attempt: follow-up of 302 subjects for 30 months. In: G Andrews, S Henderson (eds). Unmet Need in Psychiatry. Cambridge: Cambridge University Press. Beautrais AL, Joyce PR, Mulder RT, et al. 1996. Prevalence and comorbidity of mental disorders in persons making serious suicide attempts: a case-control study. American Journal of Psychiatry 153(8): 100914. Benichou J. 1991. Methods of adjustment for estimating the attributable risk in case-control studies: a review. Statistics in Medicine 10: 175373. Bennett S, Coggan C, Brewin M. 2003. Evidence for Student Focused School-based Suicide Prevention Programmes: Criteria for external providers. Auckland: Injury Prevention Research Centre (Te Puu Taki Aukati Whara). Berkman L, Glass T. 2000. Social integration, social networks, social support and health. In: L Berkman, I Kawachi (eds). Social Epidemiology. Oxford: Oxford University Press. Berkman L, Kawachi I. 2000. A historical framework for social epidemiology. In: L Berkman, I Kawachi (eds). Social Epidemiology. Oxford: Oxford University Press. Berrios G, Mohanna M. 1990. Durkheim and French psychiatric views on suicide during the 19th century: a conceptual history. British Journal of Psychiatry 156: 19. Bertolote J. 2000. Suicide in the world: an epidemiological overview, 19592000. In: D Wasserman (ed). An Unnecessary Death. London: Martin Dunitz. Bertolote JM, Fleischmann A, de Leo D, et al. 2003. Suicide and mental disorders: do we know enough? British Journal of Psychiatry 183(5): 3823. Bille-Brahe U. 2000. Sociology and suicidal behaviour. In: K Hawton, K van Heeringen (eds). The International Handbook of Suicide and Attempted Suicide. Chichester: John Wiley and Sons. Birckmayer J, Hemenway D. 1999. Minimum-age drinking laws and youth suicide, 19701990. American Journal of Public Health 89(9): 13658. 68 Suicide Prevention in New Zealand Bjarnason T, Sigurdardottir T. 2003. Psychological distress during unemployment and beyond: social support and material deprivation among youth in six northern European countries. Social Science and Medicine 56: 97385. Blakely T, Collings S, Atkinson J. 2003. Unemployment and suicide: evidence for a causal association? Journal of Epidemiology and Community Health 57: 594600. Bourke L. 2003. Toward understanding youth suicide in an Australian rural community. Social Science and Medicine 57(12): 235565. Bowles JR. 1995. Suicide in Western Samoa: an example of a suicide prevention programme in a developing country. In: R Diekstra, W Gulbinat, I Kienhorst, et al (eds). Preventive Strategies on Suicide. Leiden: EJ Brill. Breed W. 1963. Occupational mobility and suicide among white males. American Sociological Review 28: 17988. Brent D, Oqueno M, Birmaher B, et al. 2003. Prevention of familial transmission of early-onset suicidal behavior. Paper presented at Crossing Borders in Suicide Prevention: From the Genes to the Human Soul, XXII World Congress of the International Association for Suicide Prevention (IASP), 1014 September, Stockholm, Sweden. Brent DA, Bridge J. 2003. Firearms availability and suicide: evidence, interventions, and future directions. American Behavioural Scientist 46(9): 1192210. Brent DA, Johnson B, Bartle S, et al. 1993. Personality disorder, tendency to impulsive violence, and suicidal behavior in adolescents. Journal of the American Academy of Child and Adolescent Psychiatry 32(1): 6975. Brent DA, Perper JA, Moritz G, et al. 1993a. Psychiatric risk factors for adolescent suicide: a casecontrol study. Journal of the American Academy of Child and Adolescent Psychiatry 32(3): 5219. Brent DA, Perper JA, Moritz G, et al. 1993b. Stressful life events, psychopathology, and adolescent suicide: a case control study. Suicide and Life-Threatening Behavior 23(3): 17987. Brent DA, Perper J, Moritz G, et al. 1993c. Suicide in adolescents with no apparent psychopathology. Journal of the American Academy of Child and Adolescent Psychiatry 32(3): 494500. Bridgeman G, Dyall L. 1997. Ngā Ia o te Oranga Hinengaro Māori: Trends in Māori mental health: A discussion document. Wellington: Te Puni Kōkiri. Brody AL, Saxena S, Stoessel P, et al. 2001. Regional brain metabolic changes in patients with major depression treated with either paroxetine or interpersonal therapy: preliminary findings [see comment]. Archives of General Psychiatry 58(7): 63140. Bruce ML, Ten Have TR, Reynolds CF 3rd, et al. 2004. Reducing suicidal ideation and depressive symptoms in depressed older primary care patients: a randomized controlled trial. Journal of the American Medical Association 291(9): 108191. Brunner E, Marmot M. 1999. Social organisation, stress and health. In: M Marmot, RG Wilkinson (eds). Social Determinants of Health. Oxford: Oxford University Press. Bruzzi P, Green SB, Byar DP, et al. 1985. Estimating the population attributable risk for multiple risk factors using case-control data. American Journal of Epidemiology 122: 90414. Burns J, Patton G. 2000. Preventive interventions for youth suicide: a risk factor based approach. Australian and New Zealand Journal of Psychiatry 34: 388407. Suicide Prevention in New Zealand 69 Caine ED, Conwell Y. 2001. Suicide in the elderly. International Clinical Psychopharmacology 16(Suppl 2): S2530. Camus A. 1940. The Myth of Sisyphus. New York: Vintage. Cantor C. 2000. Suicide in the Western world. In: K Hawton, K van Heeringen (eds). The International Handbook of Suicide and Attempted Suicide. Chichester: John Wiley and Sons. Carson AJ, Best S, Warlow C, et al. 2000. Suicidal ideation among outpatients at general neurology clinics: prospective study. British Medical Journal 320: 131112. Carter G, Clover K, Whyte I, et al. 2003. Postcards from the edge: an RCT to reduce the repetition of hospital treated deliberate self-poisoning. Paper presented at Australasian Society for Psychiatric Research Annual Scientific Meeting, Christchurch, New Zealand. Caspi A, Sugden K, Moffitt TE, et al. 2003. Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science 301(5631): 2913. Cheng ATA. 1995. Mental illness and suicide: a case-control study in East Taiwan. Archives of General Psychiatry 52: 594603. Cheng ATA, Chen THH, Chen C-C, et al. 2000. Psychosocial and psychiatric risk factors for suicide: case-control psychological autopsy study. British Journal of Psychiatry 177: 3605. Cheng ATA, Lee C-S. 2000. Suicide in Asia and the Far East. In: K Hawton, K van Heeringen (eds). The International Handbook of Suicide and Attempted Suicide. Chichester: John Wiley and Sons. Ciffone J. 1993. Suicide prevention: a classroom presentation to adolescents. Social Work 38(2): 197203. Clarke RV, Lester D. 1987. Toxicity of car exhausts and opportunity for suicide: comparison between Britain and the United States. Journal of Epidemiology and Community Health 41(2): 11420. Clarke RV, Lester D. 1989. Suicide: Closing the exits. New York: Springer Verlag. Coggan C, Bennett S. 2002. Young people’s experience of recovery and wellbeing following a suicide attempt. Social Work Now (Dec): 1522. Coggan C, Fanslow J, Norton R. 1995. Intentional Injury in New Zealand . Wellington: Public Health Commission. Collings S, Blakely T, Atkinson J, et al. Suicide Trends and Social Factors: New Zealand 1981 to 1999: Analyses from the New Zealand CensusMortality Study. Wellington: Ministry of Health in press. Conner KR, Zhong Y. 2003. State firearm laws and rates of suicide in men and women. American Journal of Preventive Medicine 25(4): 3204. Conwell Y. 2001. Suicide in later life: a review and recommendations for prevention. Suicide and LifeThreatening Behavior 31(Suppl): S3247. Cotgrove A, Zirinsky L, Black D, et al. 1995. Secondary prevention of attempted suicide in adolescence. Journal of Adolescence 18(5): 56977. Crampton P, Howden-Chapman P (eds). 1997. Socioeconomic Inequalities and Health. Wellington: Institute of Policy Studies, Victoria University of Wellington. 70 Suicide Prevention in New Zealand de Leo D. 2002. Why are we not getting any closer to preventing suicide? British Journal of Psychiatry 181: 3724. de Leo D. 2004. Suicide prevention is far more than a psychiatric business. World Psychiatry 3(3): 1556. de Leo D, Buono MD, Dwyer J. 2002. Suicide among the elderly: the long-term impact of a telephone support and assessment intervention in Northern Italy. British Journal of Psychiatry 181: 2269. de Leo D, Evans R, Neulinger K. 2002. Hanging, firearm and non-domestic gas suicides among males: a comparative study. Australian and New Zealand Journal of Psychiatry 36: 1839. de Leo D, Hickey P, Neulinger K, et al. 2001. Ageing and Suicide. Canberra: Commonwealth Department of Health and Aged Care. Dean K. 2004. The role of methods in maintaining orthodox beliefs in health research. Social Science and Medicine 58(4): 67585. Dew MA, Bromet EJ, Brent D, et al. 1987. A quantitative literature review of the effectiveness of suicide prevention centers. Journal of Consulting and Clinical Psychology 55(2): 23944. Diekstra R, Gulbinat W, Kienhorst I, et al (eds). 1995. Preventive Strategies on Suicide. Leiden: EJ Brill. Durie M. 2001. Mauri Ora: the dynamics of Māori Health. Auckland: Oxford University Press. Durkheim E. 1897 (1951). Suicide: A study in sociology. Translated by JA Spaulding, G Simpson. New York: Free Press. Eaves L, Heath A, Martin N, et al. 1999. Comparing the biological and cultural inheritance of personality and social attitudes in the Virginia 30,000 study of twins and their relatives. Twin Research 2(2): 6280. Eckersley R, Dear K. 2002. Cultural correlates of youth suicide. Social Science and Medicine 55(11): 1891904. Eggert LL, Thompson EA, Herting JR, et al. 1995. Reducing suicide potential among high-risk youth: tests of a school-based prevention program. Suicide and Life-Threatening Behavior 25(2): 27696. Ellis P, Collings S. 1997. Public health solutions to mental health problems. In: P Ellis, S Collings (eds). Mental Health in New Zealand from the Public Health Perspective. Wellington: Public Health Group, Ministry of Health. Ferguson S, Blakely T, Allan B, et al. Suicide Rates in New Zealand: Exploring associations with social and economic factors. Wellington: Ministry of Health in press. Fergusson DM, Beautrais AL, Horwood LJ. 2003. Vulnerability and resiliency to suicidal behaviours in young people. Psychological Medicine 33(1): 6173. Fergusson DM, Lynskey MT. 1995. Childhood circumstances, adolescent adjustment, and suicide attempts in a New Zealand birth cohort. Journal of the American Academy of Child and Adolescent Psychiatry 34: 61222. Fergusson DM, Mullen PE. 1999. Childhood Sexual Abuse: An evidence based perspective. Thousand Oaks: Sage. Suicide Prevention in New Zealand 71 Fergusson DM, Woodward LJ, Horwood LJ. 2000. Risk factors and life processes associated with the onset of suicidal behaviour during adolescence and early adulthood. Psychological Medicine 30: 2339. Florio ER, Hendryx MS, Jensen JE, et al. 1997. A comparison of suicidal and non-suicidal elders referred to a community mental health center program. Suicide and Life-Threatening Behavior 27(2): 18293. Forbes A, Wainwright S. 2001. On the methodological, theoretical and philosophical context of health inequalities research: a critique. Social Science and Medicine 53: 80116. Freud S. 1917/1981. Mourning and Melancholia: The standard edition of the complete psychological works of Sigmund Freud. Translated and edited by SJ London. London: Hogarth Press. Gabbard GO. 2000. A neurobiologically informed perspective on psychotherapy. British Journal of Psychiatry 177: 11722. Gibbs JP, Martin WT. 1964. Status Integration and Suicide. Eugene, Oregon: University of Oregon Press. Gilman S, Kawachi I, Fitzmaurice G, et al. 2002. Socioeconomic status in childhood and the lifetime risk of major depression. International Journal of Epidemiology 31: 35967. Goldney R. 2001. The media and suicide: a cautionary view. Crisis 22(4): 1735. Goldney R. 2003. A novel integrated knowledge explanation of factors leading to suicide. New Ideas in Psychology 21: 1416. Goldney R. 2004. Enrico Morselli: a pioneer in suicide research. Crisis 2004(25): 39–40. Goldney RD, Fisher LJ, Wilson DH. 2001. Mental health literacy: an impediment to the optimum treatment of major depression in the community. Journal of Affective Disorders 64(2–3): 27784. Goldney R, Schioldann J. 2000. Pre-Durheim suicidology. Crisis 21(4): 1816. Goldney R, Schioldann J. 2001. A note concerning Durkheim’s precedence in the use of the terms egoistic and altruistic suicide [letter]. Suicide and Life Threatening Behaviour 31(1): 11314. Goldney R, Wilson D, Dal Grande E, et al. 2000. Suicidal ideation in a random community sample: attributable risk due to depression and psychosocial and traumatic events. Australian and New Zealand Journal of Psychiatry 34(1): 98106. Goldsmith H, Gottesman II, Lemery KS. 1997. Epigenetic approaches to developmental psychopathology. Development and Psychopathology 9(2): 36588. Gould M, Jamison KR, Romer D. 2003. Media contagion and suicide among the young. American Behavioural Scientist. 46: 1269–84. Gould MS, Fisher P, Shaffer D, et al. 1996. Psychosocial risk factors of child and adolescent completed suicide. Archives of General Psychiatry 53(12): 115562. Gould MS, Shaffer D, Fisher P, et al. 1998. Separation/divorce and child and adolescent complete suicide. Journal of the American Academy of Child and Adolescent Psychiatry 37(2): 15562. Guarnieri P. 1988. Between soma and psyche: Morselli and psychiatry in late 19th-century Italy. In: W Bynum, R Porter, M Shepherd (eds). The Anatomy of Madness. London: Routledge. 72 Suicide Prevention in New Zealand Gunnell D, Frankel S. 1994. Prevention of suicide: aspirations and evidence. British Medical Journal 308: 122733. Gunnell D, Harbord R, Singleton N, et al. Factors influencing the development and amelioration of suicidal thoughts in the general population. British Journal of Psychiatry 185: 38593. Guo B, Harstall C. 2002. Efficacy of Suicide Prevention Programs for Children and Youth. Alberta, Canada: Alberta Heritage Foundation for Medical Research. Hall WD, Mant A, Mitchell PB, et al. 2003. Association between antidepressant prescribing and suicide in Australia, 19912000: trend analysis. British Medical Journal 326(1008): 15. Harwood D, Jacoby R. 2000. Suicidal behaviour among the elderly. In: K Hawton, K van Heeringen (eds). The International Handbook of Suicide and Attempted Suicide. Chichester: John Wiley and Sons. Hassan R. 1998. One hundred years of Emile Durkheim’s Suicide: A study in sociology. Australian and New Zealand Journal of Psychiatry 32(2): 16871. Hawton K. 2002. United Kingdom legislation on pack sizes of analgesics: background, rationale, and effects on suicide and deliberate self-harm. Suicide and Life Threatening Behavior 32(3): 2239. Hawton K, Harriss L, Hall S, et al. 2003. Deliberate self-harm in Oxford, 19902000: a time of change in patient characteristics. Psychological Medicine 33: 98795. Hawton K, Townsend E, Arensman E, et al. 2000. Psychosocial versus pharmacological treatments for deliberate self harm. Cochrane Database of Systematic Reviews 2: CD001764. Hawton K, Townsend E, Deeks J, et al. 2001. Effects of legislation restricting pack sizes of paracetamol and salicylate on self poisoning in the United Kingdom: before and after study. British Medical Journal 322: 12037. Hawton K, van Heeringen K. 2000. Future perspectives. In: K Hawton, K van Heeringen (eds). International Handbook of Suicide and Suicide Prevention. Chichester: John Wiley and Sons. Hawton K, van Heeringen K (eds). 2000. The International Handbook of Suicide and Suicide Prevention. Chichester: John Wiley and Sons. Hawton K, Williams K. 2002. Influences of the media on suicide. British Medical Journal 325: 13745. Hazell P, King R. 1996. Arguments for and against teaching suicide prevention in schools. Australian and New Zealand Journal of Psychiatry 30: 63342. Heidegger M. 1962. Being and Time. Translated by J Macquarrie and E Robinson. New York: Harper and Row. Helman C. 1990. Culture, Health and Illness. Oxford: Butterworth-Heinemann. Henry AF, Short JF. 1954. Suicide and Homicide. Glenco, ILL: Free Press. Hickey L, Hawton K, Fagg J, et al. 2001. Deliberate self harm patients who leave the accident and emergency department without a psychiatric assessment: a neglected population at risk of suicide. Journal of Psychosomatic Research 50(2): 8793. Hirini P, Collings S. Whakamomori: He whakaaro, he korero noa: A collection of contemporary views on Māori and suicide. Wellington: Ministry of Health in press. Suicide Prevention in New Zealand 73 Hirschfeld RM, Keller MB, Panico S, et al. 1997. The National Depressive and Manic-Depressive Association consensus statement on the undertreatment of depression.[see comment]. Journal of the American Medical Association 277(4): 33340. Hollis M. 1994. The Philosophy of Social Science. Cambridge: Cambridge University Press. Howden-Chapman P, Cram F. 1998. Social, Economic and Cultural Determinants of Health. Wellington: National Health Committee. Howden-Chapman P, Hales S, Chapman R, et al. The Impact of Economic Recession on Youth Suicide: A comparison of New Zealand and Finland. Wellington: Ministry of Health, in press. Hulten A, Wasserman D. 1998. Lack of continuity: a problem in the care of young suicides. Acta Psychiatrica Scandinavica 97: 32633. Hume D. 1783. Essays on Suicide, and the Immortality of the Soul, Ascribed to the Late David Hume, Esq. Never before published. With remarks, intended as an antidote to the poison contained in these performances, by the editor. To which is added, two letters on suicide, from Rousseau’s [sic] Eloisa. Printed for M Smith; and sold by the booksellers in Piccadilly, Fleet -street, and Paternoster-row. Hunter R, Reser J, Baird M, et al. 1999. An Analysis of Suicide in Indigenous Communities of North Queensland: The historical, cultural and symbolic landscape. Canberra: Commonwealth Department of Health and Family Services. Hussey P, Anderson G, Osborn R, et al. 2004. How does the quality of care compare in five countries? Health Affairs 23(3): 8999. Isacsson G. 2000. Suicide prevention: a medical breakthrough? Acta Psychiatrica Scandinavica 102: 11317. Jacobs DG, Baldessarini RJ, Conwell Y, et al. 2003. Practice Guideline for the Assessment and Treatment of Patients with Suicidal Behaviors. New York: American Psychiatric Association. Jamieson PE. 2003. Changes in US popular culture portrayal of youth suicide 19502000. PhD thesis. University of Pennsylvania. Jane-Llopis E, Hosman C, Jenkins R, et al. 2003. Predictors of efficacy in depression prevention programmes. British Journal of Psychiatry 183: 38497. Jenkins R. 2002. Addressing suicide as a public health problem. Lancet 359(9309): 81314. Jenkins R, Singh B. 2000. General population strategies of suicide prevention. In: K Hawton, K van Heeringen (eds). The International Handbook of Suicide and Attempted Suicide. New York: John Wiley and Sons. Johnson JG, Cohen P, Gould MS, et al. 2002. Childhood adversities, interpersonal difficulties, and risk for suicide attempts during late adolescence and early adulthood. Archives of General Psychiatry 59(8): 7419. Johnston MV, Nishimura A, Harum K, et al. 2001. Sculpting the developing brain. Advances in Pediatrics 48: 138. Jorm A. 2000. Mental health literacy: public knowledge and beliefs about mental disorders. British Journal of Psychiatry 177: 396401. 74 Suicide Prevention in New Zealand Jorm AF, Angermeyer M, Katschnig H. 2000. Public knowledge of and attitudes to mental disorders: a limiting factor in the optimal use of treatment services. In: G Andrews, S Henderson (eds). Unmet Need in Psychiatry: Problems, resources, responses. Cambridge: Cambridge University Press. Jorm AF, Korten AE, Jacomb PA, et al. 1997. ‘Mental health literacy’: a survey of the public’s ability to recognise mental disorders and their beliefs about the effectiveness of treatment. Medical Journal of Australia 166(4): 1826. Joyce PR. 2001. Improvements in the recognition and treatment of depression and decreasing suicide rates. New Zealand Medical Journal 114(Dec 14): 5356. Kalafat J, Elias M. 1994. An evaluation of a school-based suicide awareness intervention. Suicide and Life-Threatening Behavior 24(3): 22433. Kant I. 1909. Groundwork of the Metaphysics of Morals. New York: Harper and Row. Kapur N, Cooper J, Hiroeh U, et al. 2004. Emergency department management and outcome for selfpoisoning: a cohort study. General Hospital Psychiatry 26(1): 3641. Katon W, Robinson P, Von Korff M, et al. 1996. A multifaceted intervention to improve treatment of depression in primary care. Archives of General Psychiatry 53(10): 92432. Katon W, Von Korff M, Lin E, et al. 1997. Population-based care of depression: effective disease management strategies to decrease prevalence. General Hospital Psychiatry 19(3): 16978. Kawachi I. 2000. Income inequality and health. In: L Berkman, I Kawachi (eds). Social Epidemiology. New York: Oxford University Press. Kawachi I, Berkman L. 2001. Social ties and mental health. Journal of Urban Health 78: 45867. Kellner CH, Fink M, Knapp R, et al. Bilateral ECT rapidly relieves suicidality: findings from phase 1 of the CORE ECT study. American Journal of Psychiatry (submitted). Kendler KS. 1996. Parenting: a genetic-epidemiologic perspective. American Journal of Psychiatry 153(1): 1120. Kendler KS. 1997. Social support: a genetic-epidemiologic analysis. American Journal of Psychiatry 154(10): 1398404. Kerkhof AJFM. 1999. The Finnish National Suicide Prevention Program evaluated. Crisis 20(2): 12. Kessler R, Kendler K, Heath A, et al. 1992. Social support, depressed mood and adjustment to stress: a genetic epidemiological investigation. Journal of Personal and Social Psychology 62: 25772. Khan A, Khan S, Kolts R, et al. 2003. Suicide rates in clinical trials of SSRIs, other antidepressants, and placebo: analysis of FDA reports [see comment]. American Journal of Psychiatry 160(4): 7902. Khan A, Khan SR, Leventhal RM, et al. 2001. Symptom reduction and suicide risk in patients treated with placebo in antidepressant clinical trials: a replication analysis of the Food and Drug Administration Database. American Journal of Psychiatry 158: 144954. Khan A, Leventhal RM, Khan S, et al. 2002. Suicide risk in patients with anxiety disorders: a metaanalysis of the FDA database. Journal of Affective Disorders 68: 18390. Khan A, Warner HA, Brown WA. 2000. Symptom reduction and suicide risk in patients treated with placebo in antidepressant clinical trials: an analysis of the food and drug administration database. Archives of General Psychiatry 57: 31117. Suicide Prevention in New Zealand 75 King M. 2003. The Penguin History of New Zealand. Auckland: Penguin Books. Knox KL, Conwell Y, Caine ED. 2004. If suicide is a public health problem, what are we doing to prevent it? American Journal of Public Health 94(1): 3745. Knox KL, Litts DA, Talcott GW, et al. 2003. Risk of suicide and related adverse outcomes after exposure to a suicide prevention programme in the US Air Force: cohort study. British Medical Journal 327: 15. Kotila L, Lonnqvist JK. 1987. Adolescents who make suicide attempts repeatedly. Acta Psychiatrica Scandinavica 76: 38693. Kotila L, Lonnqvist JK. 1988. Adolescent suicide attempts: sex differences predicting suicide. Acta Psychiatrica Scandinavica 77: 26470. Kreitman N. 1976. The coal gas story: United Kingdom suicide rates, 196071. British Journal of Preventive and Social Medicine 30: 8693. Kreitman N. 1990. Research issues in the epidemiological and public health aspects of parasuicide and suicide. In: D Goldberg, D Tantum (eds). The Public Health Impact of Mental Disorder. Toronto: Hogrefe and Huber Publishers. Kreitman N, Platt S. 1984. Suicide, unemployment, and domestic gas detoxification in Britain. Journal of Epidemiology and Community Health 38: 16. Kunz-Ebrecht S, Kirschbaum C, Marmot M, et al. 2004. Differences in cortisol awakening response on work days and weekends in women and men from the Whitehall II cohort. Psychoneuroendocrinology 29(4): 51628. Kunz-Ebrecht SR, Kirschbaum C, Steptoe A. 2004. Work stress, socioeconomic status and neuroendocrine activation over the working day. Social Science and Medicine 58(8): 152330. Lawson-Te Aho K. 1998. A Review of Evidence: A background document to support Kia Piki te Ora o te Taitamariki. Wellington: Ministry of Youth Affairs, Ministry of Health, Te Puni Kōkiri. Lester D. 1989. Changing rates of suicide by car exhaust in men and women in the United States after car exhaust was detoxified. Crisis 10(2): 1648. Lester D. 1997. The effectiveness of suicide prevention centers: a review. Suicide and Life-Threatening Behavior 27(3): 30410. Lester D. 2000. The epidemiology of suicide. In: D Lester (ed). Suicide Prevention: Resources for the millennium. Philadelphia: Brunner-Routledge. Lewis G, Hawton K, Jones P. 1997. Strategies for preventing suicide. British Journal of Psychiatry 171: 3514. Lin K, Von Korff M, Wagner EH. 1989. Identifying suicide potential in primary care. Journal of General Internal Medicine 4: 16. Linehan M. 1993. Cognitive Behavioral Treatment of Borderline Personality Disorder. New York: Guildford. Loftin C, McDowall D, Wiersema B, et al. 1991. Effects of restrictive licensing of handguns on homicide and suicide in the District of Columbia. New England Journal of Medicine 325: 161520. 76 Suicide Prevention in New Zealand MaGPIe Research Group. Mental disorders among Maori attending their general practitioner. Australian and New Zealand Journal of Psychiatry (in press) Mann JJ, Brent DA, Arango V. 2001. The neurobiology and genetics of suicide and attempted suicide: a focus on the serotonergic system. Neuropsychopharmacology 24(5): 46777. Maris RW. 1975. Sociology. In: S Perlin (ed). A Handbook for the Study of Suicide. New York: Oxford University Press. Marmot M. 1998. Improvement of the social environment to improve health. Lancet 351: 5760. Martikainen P, Valkonen T. 1996. Excess mortality of unemployed men and women during a period of rapidly increasingly unemployment. Lancet 348: 90912. Martin B. 2004. Dissent and heresy in medicine: models, methods, and strategies. Social Science and Medicine 58(4): 71325. Martin SD, Martin E, Rai SS, et al. 2001. Brain blood flow changes in depressed patients treated with interpersonal psychotherapy or venlafaxine hydrochloride: preliminary findings [see comment]. Archives of General Psychiatry 58(7): 6418. Marttunen M, Aro HM, Henriksson M, et al. 1991. Mental disorders in adolescent suicide: DSM II-R I and II diagnoses in suicide among 1319-year-olds in Finland. Archives of General Psychiatry 48: 8349. Marttunen MJ, Aro HM, Lonnqvist JK. 1992. Adolescent suicide: endpoint of long-term difficulties. Journal of the American Academy of Child and Adolescent Psychiatry 31(2): 64954. Marttunen MJ, Aro HM, Lonnqvist JK. 1993. Adolescence and suicide: a review of psychological autopsy studies. European Child and Adolescent Psychiatry 2(1): 1018. Maskill C, McClellan V, Hodges I, et al. Explaining Patterns of Suicide: A selective review of studies examining social, economic, cultural and other population-level influences. Wellington: Ministry of Health in press. McClure GM. 1984. Trends in suicide rate for England and Wales 197580. British Journal of Psychiatry 144: 11926. McKenzie K, Whitley R, Weich S. 2002. Social capital and mental health. British Journal of Psychiatry 181: 2803. Meltzer HY, Alphs L, Green AI, et al. 2003. Clozapine treatment for suicidality in schizophrenia: International Suicide Prevention Trial (InterSePT) [see comment] [erratum appears in Archives of General Psychiatry 2003 60(7): 735]. Archives of General Psychiatry 60(1): 8291. Meltzer HY, Okayli G. 1995. Reduction of suicidality during clozapine treatment of neurolepticresistant schizophrenia: impact on riskbenefit assessment. American Journal of Psychiatry 152(2): 18390. Menninger K. 1938. Man Against Himself. New York: Harcourt Brace World. Mental Health Branch Commonwealth Department of Health and Family Services. 1997. Youth Suicide in Australia: The national youth suicide prevention strategy. Canberra: Commonwealth Department of Health and Family Services. Michel K, Frey C, Wyss K, et al. 2000. An exercise in improving suicide reporting in print media. Crisis 21(2): 719. Suicide Prevention in New Zealand 77 Ministry of Health. 1998. Progress on Health Outcome Targets: The state of the public health in New Zealand in 1998. Wellington: Ministry of Health. Ministry of Health. 1999a. Our Health, Our Future: The health of New Zealanders. Wellington: Ministry of Health. Ministry of Health. 1999b. Suicide and the Media: The reporting and portrayal of suicide in the media. Wellington: Ministry of Health. Ministry of Health. 2000. New Zealand Health Strategy. Wellington: Ministry of Health. Ministry of Health. 2001. Suicide Trends in New Zealand 197898. Wellington: Ministry of Health. Ministry of Health. 2005. Like Minds, Like Mine National Plan 2003–2005: Project to counter stigma and discrimination associated with mental illness. Wellington: Ministry of Health. Ministry of Health. 2004. Suicide Facts: Provisional 2001 statistics (all ages). Wellington: Ministry of Health. Ministry of Youth Affairs, Ministry of Health, Te Puni Kōkiri. 1998. The New Zealand Youth Suicide Prevention Strategy. In our hands: Kia piki te ora o te taitamariki. Wellington: Ministry of Youth Affairs, Ministry of Health, Te Puni Kōkiri. Morgan HG, Jones EM, Owen JH. 1993. Secondary prevention of non-fatal deliberate self-harm: the green card study. British Journal of Psychiatry 163(July): 11112. Mortensen PB, Agerbo E, Erikson T, et al. 2000. Psychiatric illness and risk factors for suicide in Denmark. Lancet 355(9197): 912. Motto JA, Bostrom AG. 2001. A randomized controlled trial of postcrisis suicide prevention. Psychiatric Services 52(6): 82833. Mrazek PJ, Haggerty RJ (eds). 1994. Reducing Risks for Mental Disorders: Frontiers for preventive intervention research. Washington, DC: National Academy Press. Mulkay M. 1991. Three models of scientific development (1975). In: Sociology of Science. Buckingham: Open University Press. Mullen PE, Martin JL, Anderson JC, et al. 1993. Childhood sexual abuse and mental health in adult life. British Journal of Psychiatry 163: 72132. National Council for Suicide Prevention. 1995. Support in Suicidal Crises: The Swedish national programme to develop suicide prevention. Stockholm: The National Council for Suicide Prevention. National Health Committee. 1998. The Social, Cultural and Economic Determinants of Health in New Zealand: Action to improve health. Wellington: Ministry of Health. National Research and Development Centre for Welfare and Health. 1993. Suicide Can Be Prevented: Fundamentals of a target and action strategy. Helsinki: National Research and Development Centre for Welfare and Health. Nietzsche F. 1989. Beyond Good and Evil. Translated by Walter Kaufmann. New York: Random House. Northridge M. 1995. Annotation: public health methods, attributable risk as a link between causality and public health action. American Journal of Public Health 85:12024. 78 Suicide Prevention in New Zealand O’Carroll PW, Silverman MM. 1994. Community suicide prevention: the effectiveness of bridge barriers. Suicide and Life-Threatening Behavior 24(1): 8999. Olfson M, Shaffer D, Marcus SC, et al. 2003. Relationship between antidepressant medication treatment and suicide in adolescents. Archives of General Psychiatry 60(10): 97882. Ostamo A, Lonnqvist JK. 2001. Attempted suicide rates and trends during a period of severe economic recession in Helsinki, 19891997. Social Psychiatry and Psychiatric Epidemiology 36(7): 35460. Overholser JC, Hemstreet AH, Spirito A, et al. 1989. Suicide awareness programs in the schools: effects of gender and personal experience. Journal of the American Academy of Child and Adolescent Psychiatry 28: 92530. Owens D, Horrocks J, House A. 2002. Fatal and non-fatal repetition of self-harm: systematic review. British Journal of Psychiatry 181: 1939. Paquette V, Levesque J, Mensour B, et al. 2003. ‘Change the mind and you change the brain’: effects of cognitive-behavioral therapy on the neural correlates of spider phobia. Neuroimage 18(2): 4019. Paykel ES, Hart D, Priest RG. 1998. Changes in public attitudes to depression during the Defeat Depression campaign. British Journal of Psychiatry 173: 51922. Paykel ES, Tylee A, Wright A, et al. 1997. The Defeat Depression campaign: psychiatry in the public arena. American Journal of Psychiatry 154(6): 5965. Pearce N. 1996. Traditional epidemiology, modern epidemiology, and public health. American Journal of Public Health 86: 67883. Pearson J. 2003. Public awareness campaigns to prevent suicide. Paper presented at the International Association for Suicide Prevention: From the Genes to the Human Soul, XXII World Congress, 1014 September, Stockholm, Sweden. Pearson JL, Conwell Y. 1995. Suicide in late life: challenges and opportunities for research. International Psychogeriatrics 7(2): 1316. Perdiguero E, Bernabeu J, Huertas R, et al. 2001. History of health: a valuable tool in public health. Journal of Epidemiology and Community Health 55: 66773. Pfaff JJ, Acres JG, McKelvey RS. 2001. Training general practitioners to recognise and respond to psychological distress and suicidal ideation in young people. Medical Journal of Australia 174(5): 2226. Pirkis J, Blood RW. 2001. Suicide and the Media: A critical review. Canberra, Australia: Commonwealth of Australia. Pirkis J, Burgess P, Dunt D. 2000. Suicidal ideation and suicide attempts among Australian adults. Crisis 21(1): 1625. Platt S, Hawton K. 2000. Suicidal behaviour and the labour market. In: K Hawton, K van Heeringen (eds). The International Handbook of Suicide and Attempted Suicide. Chichester: John Wiley and Sons Ltd. Platt S, Micciolo R, Tansella M. 1992. Suicide and unemployment in Italy. Social Science and Medicine 34: 1191201. Platt SD. 1984. Unemployment and suicidal behaviour: a review of the literature. Social Science and Medicine 19(2): 93115. Suicide Prevention in New Zealand 79 Preti A, Miotto P. 1999a. Social and economic influence on suicide. Archives of Suicide Research 5: 14156. Preti A, Miotto P. 1999b. Suicide and unemployment in Italy, 19821994. Journal of Epidemiology and Community Health 53: 694701. Prudic J, Sackeim HA. 1999. Electroconvulsive therapy for suicide risk. Journal of Clinical Psychiatry 60(suppl 2): S10410. Public Health Commission. 1994. A Strategic Direction to Improve and Protect the Public Health. Wellington: Public Health Commission. Public Health Commission. 1995. Progress on Health Outcome Targets: The state of the public health in New Zealand in 1995. Wellington: Public Health Commission. Qin P, Agerbo E, Mortensen PB. 2003. Suicide risk in relation to socioeconomic, demographic, psychiatric, and familial factors: a national register-based study of all suicides in Denmark, 19811997. American Journal of Psychiatry 160: 6572. Quinnett P. 1995. Question Persuade Refer for suicide prevention: certified QPR gatekeeper instructions manual. Spokane WA: QPR Institute. Regier DA, Hirschfeld RMA, Goodwin FK, et al. 1988. The NIMH depression awareness, recognition, and treatment program: structure, aims, and scientific basis. American Journal of Psychiatry 145(11): 13517. Reynolds CFR, Degenholtz H, Parker LS, et al. Treatment as usual (TAU) control practices in the PROSPECT study: managing the interaction and tension between research design and ethics. International Journal of Geriatric Psychiatry 16(6): 6028. Rich CL, Fowler RC, Blenkush M. 1986. San Diego suicide study: comparison of gay to straight males. Suicide and Life-Threatening Behavior 16(4): 44857. Robson B, Reid P. 2000. Ethnicity Matters: Review of the measurement of ethnicity. Wellington: Te Rōpu Rangahau Hauora a Eru Pōmare, Department of Statistics. Rogers A, Pilgrim D. 2003. Mental Health and Inequality. Basingstoke: Palgrave Macmillan. Rose G. 1985. Sick individuals and sick populations. International Journal of Epidemiology 14: 328. Rose G. 1989. The mental health of populations. In: P Williams, G Wilkinson, K Rawnsley (eds). The Scope of Epidemiological Psychiatry. London: Routledge. Rose G. 1992. The Strategy of Preventive Medicine. Oxford, New York, Tokyo: Oxford University Press, p. 24. Rose G. 1993. Mental disorder and the strategies of prevention. Psychological Medicine 23(3): 5535. Rothman K, Greenland S. 1998. Modern Epidemiology. New York: Lippincott Williams and Wilkins. Rubenowitz E, Waern M, Wilhelmson K, et al. 2001. Life events and psychosocial factors in elderly suicides: a case-control study. Psychological Medicine 31: 1193202. Rutter M, Smith DJ. 1995. Psychosocial Disorders in Young People: Time trends and their causes. Chichester: John Wiley and Sons. 80 Suicide Prevention in New Zealand Rutz W, Carlsson P, von Knorring L, et al. 1992. Cost-benefit analysis of an educational program for general practitioners by the Swedish Committee for the Prevention and Treatment of Depression. Acta Psychiatrica Scandinavica 85: 45764. Rutz W, von Knorring L, Walinder J. 1992. Long-term effects of an educational program for general practitioners given by the Swedish Committee for the Prevention and Treatment of Depression. Acta Psychiatrica Scandinavica 85(1): 838. Sainsbury P. 2001. Beyond blue ... a leap into the blue beyond? RANZCP Congress, Sydney. Sakinofsky I. 2000. Repetition of suicidal behaviour. In: K Hawton, K van Heeringen (eds). International Handbook of Suicide and Attempted Suicide. Chichester: John Wiley and Sons. Sanddal ND, Sanddal TL, Berman AL, et al. 2003. A general systems approach to suicide prevention: lessons from cardiac prevention and control. Suicide and Life Threatening Behavior 33: 34152. Sartre J-P. 1956. Being and Nothingness: An essay on phenomenological ontology. Translated by HE Barnes. New York: Philosophical Library. Schmidtke A, Schaller S. 2000. The role of mass media in suicide prevention. In: K Hawton, K van Heeringen (eds). The International Handbook of Suicide and Attempted Suicide. New York: John Wiley and Sons. Seeley MF. 1997. The role of hotlines in the prevention of suicide. In: RW Maris, MM Silverman, SS Canetto (eds). Review of Suicidology. New York: Guilford. Shaffer D, Garland A, Fisher P, et al. 1988. Suicide crisis centers: a critical reappraisal with special reference to the prevention of youth suicide. In: FE Goldston, CM Heinick, RS Pynoos, et al (eds). Prevention of Mental Health Disturbance in Childhood. New York: APA Press. Shaffer D, Garland A, Vieland V, et al. 1991. The impact of curriculum-based suicide prevention programs for teenagers. Journal of the American Academy of Child and Adolescent Psychiatry 30(4): 58896. Shaffer D, Gould MS, Fisher P, et al. 1996. Psychiatric diagnosis in child and adolescent suicide. Archives of General Psychiatry 53: 33948. Shaffer S, Scott M, Wilcox H, et al. 2004. The Columbia Suicide Screen: Validity and reliability of a screen for youth suicide and depression. Journal of the American Academy of Child and Adolescent Psychiatry 43(1): 71–77. Shaw M, Dorling D, Davey-Smith G. 1999. Poverty, social exclusion and minorities. In: M Marmot, R Wilkinson (eds). Social Determinants of Health. Oxford: Oxford University Press. Sherbourne C, Schoenbaum M, Wells KB, et al. 2004. Characteristics, treatment patterns and outcomes of persistent depression despite treatment in primary care. General Hospital Psychiatry 26(2): 10614. Shneidman E. 1985. Definition of Suicide. New York: Wiley. Siegel D. 1999. Mind, brain and experience. Chapter 1 in: The Developing Mind. London: The Guilford Press. Silbert KL, Berry GL. 1991. Psychological effects of a suicide prevention unit on adolescents’ levels of stress, anxiety and hopelessness: implications for counselling psychologists. Counselling Psychology 4: 4558. Suicide Prevention in New Zealand 81 Silverman MM. 1997. Current controversies in suicidology. In: RW Maris, MM Silverman, SS Canetto (eds). Review of Suicidology. New York, NY: Guilford Press. Silverman MM. 2004. Preventing suicide: a call to action. World Psychiatry 3(3): 1523. Singh B, Judd F (eds). 1995. Social factors in suicide in Australia. Paper presented at the Ciba-Geigy Psychiatric Symposium, Melbourne, Australia. Skegg K. 1997. Suicide and parasuicide. In: P Ellis, S Collings (eds). Mental Health in New Zealand from a Public Health Perspective. Wellington: Ministry of Health. Skegg K, Cox B. 1991. Suicide in New Zealand 19571986: the influence of age, period and birthcohort. Australian and New Zealand Journal of Psychiatry 25: 18190. Skegg K, Cox B, Broughton J. 1995. Suicide among New Zealand Maori: is history repeating itself? Acta Psychiatrica Scandinavica: 92: 4539. Skegg K, Nada-Raja S, Dickson N, et al. 2003. Sexual orientation and self-harm in men and women. American Journal of Psychiatry 160: 5416. Stack S. 2000a. Suicide: a 15-year review of the sociological literature. Part I: Cultural and economic factors. Suicide and Life Threatening Behavior 30(2): 14562. Stack S. 2000b. Suicide: a 15-year review of the sociological literature. Part II: Modernization and social integration perspectives. Suicide and Life Threatening Behavior 30(2): 16375. Statham DJ, Heath AC, Madden PAF, et al. 1998. Suicide behaviour: an epidemiological and genetic study. Psychological Medicine 28: 83955. Statistics New Zealand. 1996. Demographic Trends 1996. Wellington: Statistics New Zealand. Statistics New Zealand. 2002. Census 2001. Wellington: Statistics New Zealand. Suokas J, Lonnqvist JK. 1991. Outcome of attempted suicide and psychiatric consultation: risk factors and suicide mortality during a five-year follow-up. Acta Psychiatrica Scandinavica 79: 4539. Susser M. 1996a. Choosing a future for epidemiology. I: Eras and paradigms. American Journal of Public Health 86(5): 66873. Susser M. 1996b. Choosing a future for epidemiology. II: From black box to Chinese boxes and ecoepidemiology. American Journal of Public Health 86(5): 6747. Szanto K. 2003. Suicidal behavior in the elderly. Psychiatric Times XX(13). URL: www.psychiatrictimes.com/p031252.html Szasz TS. 1961. The Myth of Mental Illness. London: Paladin. Szasz T. 1971. The Manufacture of Madness. London: Routledge. Thompson A, Dryden D, Borden K, et al. 2001. Return visits to the emergency department after a suicide attempt. American Society of Suicidology Annual Conference, April 2001. Thompson EA, Eggert LL, Herting JR. 2000. Mediating effects of an indicated prevention program for reducing youth depression and suicide risk behaviors. Suicide and Life-Threatening Behavior 30(3): 25271. Tondo L, Ghiani C, Albert M. 2001. Pharmacologic interventions in suicide prevention. Journal of Clinical Psychiatry 62: 515. 82 Suicide Prevention in New Zealand Tondo L, Hennen J, Baldessarini RJ. 2001. Lower suicide risk with long-term lithium treatment in major affective illness: a meta-analysis. Acta Psychiatrica Scandinavica 104(3): 16372. Tondo L, Isacsson G, Baldessarini R. 2003. Suicidal behaviour in bipolar disorder: risk and prevention. CNS Drugs 17(7): 491511. Traskman-Bendz L, Mann JJ. 2000. Biological aspects of suicidal behaviour. In: K Hawton, K van Heeringen (eds). The International Handbook of Suicide and Attempted Suicide. Chichester: John Wiley and Sons. University of Otago and Ministry of Health. 2005. Decades of Disparity II: Socioeconomic mortality trends in New Zealand, 19801999. Wellington: Ministry of Health. US Department of Health and Human Services. 2001. National Strategy for Suicide Prevention: Goals and objectives for action. Rockville, MD: National Library of Medicine Cataloging in Publication. van Heeringen K. 2003. The neurobiology of suicide and suicidality [comment]. Canadian Journal of Psychiatry Revue Canadienne de Psychiatrie 48(5): 292300. van Heeringen K, Hawton K, Williams JMG. 2000. Pathways to suicide: an integrative approach. In: K Hawton, K van Heeringen (eds). The International Handbook of Suicide and Attempted Suicide. Chichester: John Wiley and Sons. van Praag H. 2003. A stubborn behaviour: the failure of antidepressants to reduce suicide rates. World Journal of Biological Psychiatry 4: 18491. Velting DM, Gould MS. 1997. Suicide contagion. In: RW Maris, MM Silverman, SS Canetto (eds). Review of Suicidology, 1997. New York, NY: Guilford Press. Vieland V, Whittle B, Garland A, et al. 1991. The impact of curriculum-based suicide prevention programs for teenagers: an 18-month follow-up. Journal of the American Academy of Child and Adolescent Psychiatry 30(5): 81115. Waern M, Rubenowitz E, Runeson BS, et al. 2002. Burden of illness and suicide in elderly people: case-control study. British Medical Journal 324: 1355–7. Waern M, Rubenowitz E, Wilhelmson K. 2003. Predictors of suicide in the old elderly. Gerontology 49(5): 32834. Waern M, Runeson BS, Allebeck P, et al. 2002. Mental disorder in elderly suicides: a case-control study. American Journal of Psychiatry 159: 4505. Wasserman D. 2004. Evaluating suicide prevention: various approaches needed. World Psychiatry 3(3): 1534. Wasserman D, Varnik A. 1998. Suicide-preventive effects of perestroika in the former USSR: the role of alcohol restriction. Acta Psychiatrica Scandinavica 98(Suppl 394): S14. Wasserman D, Varnik A, Dankowicz M. 1998. Regional differences in the distribution of suicide in the former Soviet Union during perestroika, 19841990. Acta Psychiatrica Scandinavica 98(Suppl 394): S512. WHO. 1993. Guidelines for the Primary Prevention of Mental, Neurological and Psychosocial Disorders: 4: Suicide. Geneva: World Health Organization. WHO. 2000. Preventing Suicide: A resource for media professionals. Geneva: World Health Organization, Mental and Behavioural Disorders. Suicide Prevention in New Zealand 83 WHO. 2004a. Promoting Mental Health: Concepts, emerging evidence, practice. Summary report. Geneva: World Health Organization, Department of Mental Health and Substance Abuse in Collaboration with the Victorian Health Promotion Foundation and the University of Melbourne. WHO. 2004b. Suicide Prevention. Geneva: World Health Organization. WHO. 2004c. Suicide Rates (per 100,000) by Country, Year and Gender, 2004. Geneva: World Health Organization. WHO World Mental Health Survey Consortium. 2004. Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization world mental health surveys. Journal of the American Medical Association 291(21): 258190. Wilkinson R. 1999. Putting the picture together: prosperity, redistribution, health and welfare. In: M Marmot, G Wilkinson (eds). Social Determinants of Health. Oxford: Oxford University Press. Wilson J. 2001. Suicide and suicide prevention. Paper presented at the Royal Australian and New Zealand College of Psychiatrists Congress, May 2001, Canberra, Australia. Winefield AH, Tiggemann M. 1993. Psychological distress, work attitudes and intended year of leaving school. Journal of Adolescence 16(1): 5774. Wittgenstein L. 1953. Philosophical Investigations. New York: MacMillan. Wolff S. 1995. The concept of resilience. Australian and New Zealand Journal of Psychiatry 29: 56574. Yip PSF. 1996. Suicides in Hong Kong, Taiwan and Beijing. British Journal of Psychiatry 169: 495500. Zilboorg G. 1939. Differential diagnostic types of suicide. Archives of General Psychiatry 35: 27091. 84 Suicide Prevention in New Zealand